Introduction
Unhealthy diets are a major driver of non-communicable diseases and their related healthcare burdens (Benziger et al., Reference Benziger, Roth and Moran2016). In 2017, dietary risks were responsible for 11 million deaths and 255 million disability-adjusted life-years (DALYs) globally, with cardiovascular disease being the leading cause of diet-related deaths (GBD 2017 Diet Collaborators, 2019). In Singapore, poor dietary habit was the leading risk factor contributing to DALYs accounting for 10.1% of Singapore overall disease burden (Epidemiology & Disease Control Division, Ministry of Health Singapore and Institute for Health Metrics and Evaluation, 2019). Sub-optimal diet is an important preventable risk factor, and this highlights the importance of providing adequate nutrition care.
Nutrition care refers to any practice conducted by a health professional to support a patient to improve their dietary behaviours (Ball and Leveritt, Reference Ball and Leveritt2015) and includes nutrition assessment, education and counselling, and referral to nutrition-focused healthcare professionals and services. Nutrition care provided by primary care professionals has the potential to improve patients’ dietary behaviours (Ball et al., Reference Ball, Leveritt, Cass and Chaboyer2015), and a study showed that most patients with diet-related chronic diseases consider primary care physicians (PCPs) as their preferred provider of nutrition care because PCPs were able to provide trustworthy and personalised nutrition care (Ball et al., Reference Ball, Desbrow and Leveritt2014). Best practice guidelines also regard nutrition care as an important component of effective prevention and management of diet-related chronic diseases (Wharton et al., Reference Wharton2020).
Competency refers to the set of knowledge, skills, communication, and attitudes that facilitate a clinician’s ability to perform safe and effective healthcare practices (Verma et al., Reference Verma, Paterson and Medves2006). Studies have shown that there is a lack of nutrition competence among PCPs (Smith et al., Reference Smith, Seeholzer, Gullett, Jackson, Antognoli, Krejci and Flocke2015; Dumic et al., Reference Dumic, Miskulin, Pavlovic, Orkic, Bilic-Kirin and Miskulin2018; Keaver et al., Reference Keaver, O’Meara, Mukhtar and McHugh2018), resulting in inadequate nutrition care (Crowley et al., Reference Crowley, Ball and Hiddink2020a). To our knowledge, no study has been done in Singapore to evaluate the level of nutrition competence among PCPs. In order to better understand how to improve and support the provision of nutrition care to a growing population of patients with diet-related chronic disease, it is important that current nutrition competence among PCPs is measured and understood. This study aims to describe the self-perceived nutrition competence of PCPs in Singapore and to evaluate the factors affecting their self-perceived nutrition competence.
Methods
Study design and setting
This was a cross-sectional study involving PCPs from the National Healthcare Group Polyclinics (NHGP), which is a public primary care institution that delivers highly subsidized care, including outpatient, maternal, and child health services, to the community in Singapore. The study utilized an anonymous online survey platform Research Electronic Data Capture (REDCap®) to evaluate the physicians’ self-perceived competence in providing nutrition care to patients with chronic disease. Total population sampling was used, and all PCPs who worked in NHGP, excluding locums, were invited to participate in the study. An electronic invitation email with a secure link to the online survey was sent to all eligible participants and participation was voluntary. Weekly email reminders were sent out during the study period from 11 January 2022 to 12 February 2022.
A sample questionnaire for PCPs is available as online supplementary appendix.
NUTrition COMPetence (NUTCOMP) questionnaire
The NUTCOMP questionnaire (Ball and Leveritt Reference Ball and Leveritt2015) measures the self-perceived competence of healthcare professionals in providing nutrition care to patients with chronic diseases. Self-perceived competence has been shown to be an accepted indicator of actual competence (Davis et al., Reference Davis, Mazmanian, Fordis, Van Harrison, Thorpe and Perrier2006). NUTCOMP measures PCPs’ self-confidence across a few constructs: (1) nutrition knowledge, which refers to their understanding of food influences on the body systems, chronic diseases, and medication use; (2) nutrition skills, which refers to the assessment and management of the dietary needs of an individual; (3) nutrition communication and counselling, which refers to their understanding of the patients’ expectations and comprehension during dietary consultations, and their confidence in their ability to work with other healthcare professionals; and (4) attitudes towards nutrition care, which measures the level of agreement of PCPs in providing good nutrition care.
Each item in the questionnaire uses a 5-point Likert scale to rate confidence level (1 = not very confident at all to 5 = extremely confident) or degree of agreement (1 = completely disagree, to 5 = completely agree). To reflect the local context, ‘Australian Guide to Healthy Eating (National Health and Medical Research Council, 2013)’ found on two items (section 1, item 4 and section 2, item 4) was changed to ‘My Healthy Plate (Health Promotion Board, 2021)’. The mean score for each construct was calculated by adding up the scores for all items in that construct and then dividing the sum by the number of items to give a score from one to five. This represents the level of confidence or degree of agreement for that construct enabling comparisons between the different constructs. The NUTCOMP total score was calculated by taking the sum of scores for all the items in the four constructs.
Participant characteristics
Participant characteristics included age, gender, work experience in primary care setting, highest qualification, self-reported body mass index (BMI), previous formal education with nutrition content, and Continuing Medical Education (CME) engagement in nutrition. Participants were also asked on their perceived need for further nutrition education and the type of dietary counselling they were least confident with. PCPs’ highest qualification was classified into two categories: (1) basic medical degree such as Bachelor of Medicine and Bachelor of Surgery (MBBS) and/or Graduate Diploma in Family Medicine (GDFM) and (2) advanced training in family medicine, i.e. Master of Medicine in Family Medicine (MMED) and/or Fellow of the College of Family Physicians Singapore (FCFP). The GDFM is a two-year family medicine training programme that helps PCPs practice at an enhanced level, catering to the healthcare needs of the community. The MMED is designed for working doctors wishing to pursue further higher training in family medicine to function as a registrar family physician, and FCFP is designed to help PCPs function as a consultant family physician (College of Family Physicians Singapore, no date).
Personal dietary habits
This study used the NHGP Fat and Fibre questionnaire, which is a brief dietary assessment questionnaire used by dietitians in NHGP to help individuals identify unhealthy dietary habits. Brief dietary assessment tools offer a low-burden alternative for research studies (Reeves et al., Reference Reeves, Winkler and Eakin2015) to quickly identify dietary concerns (England et al., Reference England, Andrews, Jago and Thompson2015). The NHGP Fat and Fibre questionnaire uses the national dietary recommendations to assess the frequencies of food intake and food consumption behaviours for foods high in fat (fat construct) and fibre (fibre construct). The fat construct consists of 12 questions, and the total score ranges from 12 to 48, with a cut-off of ‘35 or less’ indicating undesirable or high-fat intake. The fibre construct consists of five questions, and the total score ranges from 5 to 20, with a cut-off score of ‘13 or less’ indicating undesirable or low fibre intake.
Statistical analysis
Data were extracted from the REDCap® database, and complete case analysis was utilized. Descriptive statistics were calculated for all measures. Means and standard deviations (SD) were presented for continuous variables, while frequency and percentage were used for categorical variables. Test for multicollinearity was conducted using variance inflation factors before proceeding to multivariable linear regression. This was used to investigate the association between each NUTCOMP construct and total score (outcome variable) with independent variables – highest qualification, gender, BMI, work experience, previous formal nutrition education, CME engagement in nutrition, fat, and fibre score. Internal consistency was measured using the Cronbach’s alpha. R version 4.1.2 was used for the analyses. A p-value of <0.05 was considered statistically significant.
Results
The study invitations were sent to 333 PCPs and 195 PCPs (58.6%) participated in the study, of which 153 PCPs (45.9%) completed the questionnaire in full and their data were included in the study. Table 1 shows the characteristics of the participants. The mean age was 35.9 ± 8.1 years old, and the proportion of male and female participants was fairly equal (50.3% male and 49.7% female). Only 50.3% of participants had ideal BMI (BMI <23 kg/m2). The majority of participants (79.7%) did not have any formal nutrition education program, and only 45.1% of participants had attended CME engagement in nutrition. Most participants (87.0%) agreed with the need for further nutrition education. Calorie counting and carbohydrate counting were the types of dietary counselling that most PCPs felt least confident with (54.6% and 53.0%, respectively).
With regards to the personal dietary habits of the participants, 64.7% and 69.9% of PCPs have undesirable fat and fibre scores, respectively.
Table 1. Characteristics of participating primary care physicians (n = 153)
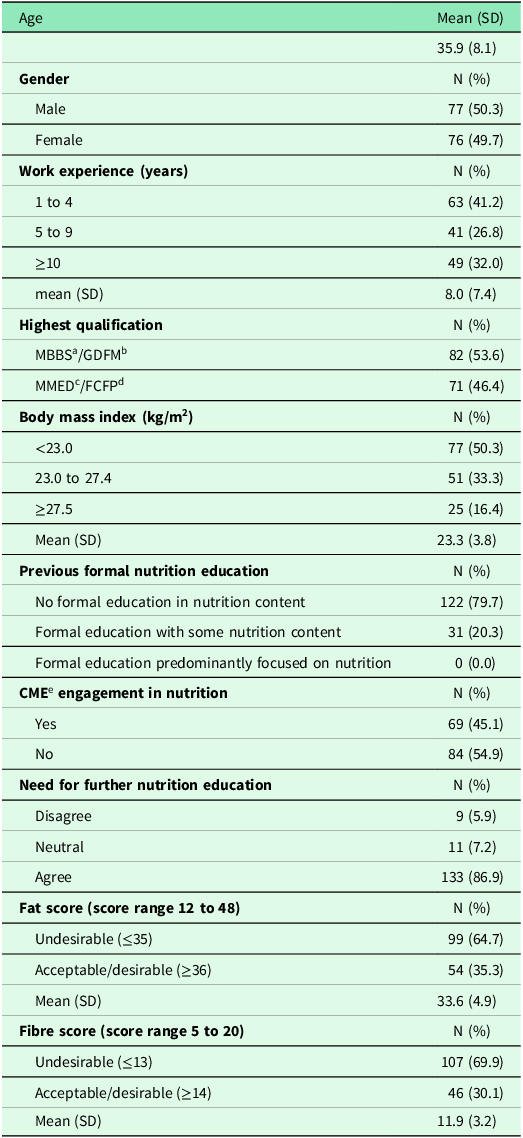
a MBBS: Bachelor of Medicine and Bachelor of Surgery
b GDFM: Graduate Diploma in Family Medicine
c MMED: Master of Medicine in Family Medicine
d FCFP: Fellow of the College of Family Physicians Singapore
e CME: continuing medical education
Table 2 shows the scores for the NUTCOMP constructs and the total score. PCPs had the lowest self-perceived confidence in nutrition knowledge and nutrition skills (mean scores 2.8 ± 0.6 and 2.9 ± 0.6, respectively), followed by self-perceived confidence in nutrition communication and counselling (mean score 3.1 ± 0.6). They scored highest in their attitudes towards nutrition care (mean score 4.3 ± 0.5).
Table 2. NUTCOMP constructs and total score
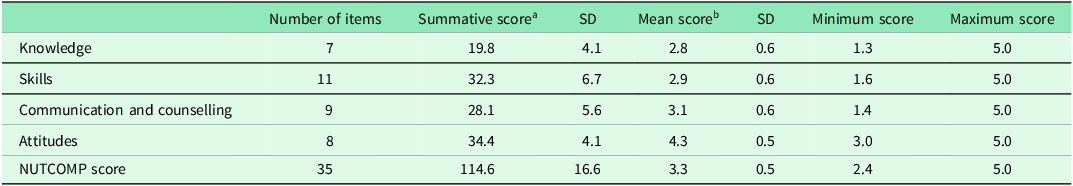
a Summative score for construct: summation of all scores for items in each construct
b Mean score for construct: summative scores divided by number of items in each construct (score range one to five)
The Cronbach’s alpha coefficients for the NUTCOMP questionnaire and its individual constructs were good (knowledge: 0.87, skills: 0.91, communication and counselling: 0.92, attitudes: 0.88, NUTCOMP: 0.95). For NHGP fat and fibre questionnaire, Cronbach’s alpha coefficients were 0.77 for fat and 0.71 for fibre.
There was significant collinearity between work experience and age, hence for multivariable regression analysis, we used work experience as an independent variable instead of age, as the former had more clinical significance.
After adjusting for PCPs’ characteristics (Table 3), physicians who had completed a formal education program with nutrition content had significantly higher scores in self-perceived nutrition knowledge (β = 2.27, 95% C.I: 4.57 to 16.94, p-value <0.01), self-perceived nutrition skills (β = 5.08, 95% C.I: 2.64 to 7.53, p-value <0.01), self-perceived nutrition communication and counselling (β =3.09, 95% C.I: 0.91 to 5.27, p-value <0.01), and NUTCOMP score (β = 10.76, 95% C.I: 4.57 to 16.94, p-value <0.01).
Table 3. Regression results between primary care physicians’ characteristics with NUTCOMP constructs and total score
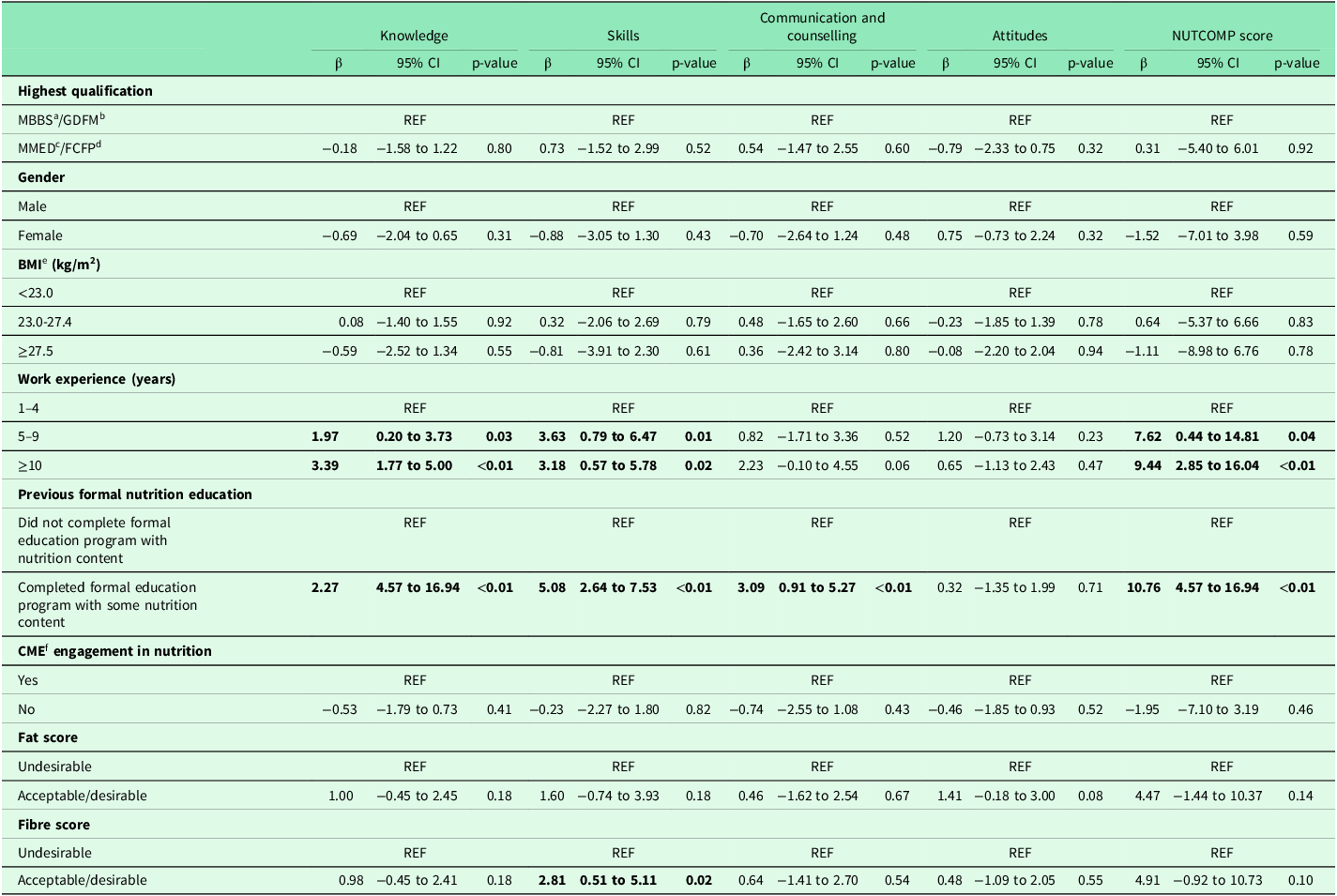
a MBBS: Bachelor of Medicine and Bachelor of Surgery
b GDFM: Graduate Diploma in Family Medicine
c MMED: Master of Medicine in Family Medicine
d FCFP: Fellow of the College of Family Physicians Singapore
e BMI: body mass index
f CME: continuing medical education
Compared to PCPs with ‘less than 5 years’ of work experience in primary care, those with ‘5 to 9 years’, and those with ‘more than 10 years’ of experience had significantly higher self-perceived nutrition knowledge [(β = 1.97, 95% C.I: 0.20 to 3.73, p-value 0.03) and (β = 3.39, 95% C.I: 1.77 to 5.00, p-value <0.01) respectively], self-perceived nutrition skills [(β = 3.63, 95% C.I: 0.79 to 6.47, p-value 0.01) and (β = 3.18, 95% C.I: 0.57 to 5.78, p-value 0.02) respectively] and NUTCOMP score [(β = 7.62, 95% C.I: 0.44 to 14.81, p-value 0.04) and (β = 9.44, 95% C.I: 2.85 to 16.04, p-value <0.01), respectively]. PCPs’ highest qualification, CME engagement in nutrition, BMI, and personal dietary habits were not significantly associated with their self-perceived nutrition competence.
Discussion
With the rise of non-communicable diseases related to poor dietary habits, there is increasing demand for PCPs to provide nutrition care. This is the first study to measure the self-perceived nutrition competence among PCPs in Singapore. Our findings showed that PCPs reported the highest scores in their attitudes towards nutrition care and the lowest scores in their self-perceived confidence in nutrition knowledge and nutrition skills. We also found that physicians with formal nutrition education and those with more work experience reported higher self-perceived nutrition competence.
Comparison of NUTCOMP constructs
Self-perceived nutrition knowledge and nutrition skills were the two constructs that PCPs had the lowest confidence in. This was similar to studies in Ireland (Keaver et al., Reference Keaver, O’Meara, Mukhtar and McHugh2018) and Saudi Arabia (Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020), which also used the NUTCOMP questionnaire. The findings also correlated with other studies that used quizzes and patient scenarios to objectively measure nutrition knowledge (Crowley et al., Reference Crowley, Ball and Wall2016b; Dumic et al., Reference Dumic, Miskulin, Pavlovic, Orkic, Bilic-Kirin and Miskulin2018). While the self-perceived nutrition knowledge and nutrition skills scores appeared to be low, it is important to acknowledge that the NUTCOMP tool does not provide a benchmark cut-off for what is high and low (Ball and Leveritt, Reference Ball and Leveritt2015). As such, further work is required to clarify what benchmark is acceptable for effective healthcare practice.
We also found that PCPs’ confidence in nutrition communication and counselling was low in comparison with other constructs, in keeping with similar studies (Smith et al., Reference Smith, Seeholzer, Gullett, Jackson, Antognoli, Krejci and Flocke2015; Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020). A focus group study on Australian PCPs reported that they needed further information to contextualize their nutrition counselling to patients’ cultural, social, and economic backgrounds (Crowley et al., Reference Crowley, Ball, McGill, Buetow, Arroll, Leveritt and Wall2016a). Low perceived confidence may be attributed to inadequate nutrition training, lack of time, and lack of compensation (Kolasa and Rickett, Reference Kolasa and Rickett2010). This lack of confidence may hinder PCPs’ efforts to improve patients’ dietary behaviours.
The PCPs in our study reported positive attitudes towards nutrition care, and this was also reflected in similar studies (Moore and Adamson, Reference Moore and Adamson2002; Crowley et al., Reference Crowley, Ball, Han, McGill, Arroll, Leveritt and Wall2015; Keaver et al., Reference Keaver, O’Meara, Mukhtar and McHugh2018; Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020) that used either the NUTCOMP questionnaire (Keaver et al., Reference Keaver, O’Meara, Mukhtar and McHugh2018; Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020) or self-reported questionnaire consisting of varying number of items (Moore and Adamson, Reference Moore and Adamson2002; Crowley et al., Reference Crowley, Ball, Han, McGill, Arroll, Leveritt and Wall2015). It is an encouraging sign that the majority of PCPs recognize the importance of nutrition care and agree that they have an essential role to play in providing nutrition care. Yet despite so, there exists a gap between the positive attitudes displayed by PCPs, and their low self-perceived confidence in knowledge, skills, communication, and counselling in providing nutrition care. This highlights the importance of strategies such as adequate nutrition training to bridge this gap (Crowley et al., Reference Crowley, Ball and Hiddink2020a).
PCPs’ characteristics and self-perceived nutrition competence
Our study showed that PCPs who completed a formal education program with nutrition content had significantly better self-perceived nutrition competence, but not those with higher qualifications and those with CME engagement in nutrition. Also, a large majority of PCPs felt that they needed further nutrition education. This may indicate a lack of adequate nutrition education in undergraduate (Danek et al., Reference Danek, Berlin, Waite and Geib2017; Mogre et al., Reference Mogre, Stevens, Aryee, Amalba and Scherpbier2018) and postgraduate medical training programmes (Devries et al., Reference Devries, Willett and Bonow2019) as well as in CME activities (Crowley et al., Reference Crowley, Ball and Hiddink2019), which are considered essential educational activities to maintain, develop, or increase the knowledge, skills, and professional performance of a doctor.
Previous studies have highlighted the lack of curriculum time for nutrition education (Adams et al., Reference Adams, Lindell, Kohlmeier and Zeisel2006), inadequate nutrition content coverage (Chung et al., Reference Chung, van Buul, Wilms, Nellessen and Brouns2014), poor collaboration with nutrition professionals, and poor application of nutrition science to clinical practice (Mogre et al., Reference Mogre, Stevens, Aryee, Amalba and Scherpbier2018) as obstacles to the integration of nutrition education into undergraduate and postgraduate medical training programmes worldwide. CME activities are also inconsistent in their delivery methods (Davis, Reference Davis1995) resulting in varying effectiveness on its learners (Marinopoulos et al., Reference Marinopoulos2007). In order to improve self-perceived nutrition competence among PCPs, there may be a need for more structured, comprehensive, competency-based education programmes. Competencies are key aspects of any educational model for medical training and having a focus on competency-based framework can help to guide medical education (Kris-Etherton et al., Reference Kris-Etherton2015).
Another important finding in our study was that PCPs with more work experience had significantly better self-perceived nutrition competence. This is also consistent with a national survey conducted among PCPs in the United States (Bleich et al., Reference Bleich, Bennett, Gudzune and Cooper2012b). More experienced PCPs may have gained nutrition knowledge and nutrition skills through other informal methods, such as interactions with patients and other allied healthcare workers, and thus felt more competent in providing nutrition care. Further studies using qualitative methods will be needed to better understand these informal methods, which may be helpful to improve nutrition competence training strategies targeted at our junior doctors.
Our study also showed that a significant number of PCPs had suboptimal BMI and undesirable personal dietary habits. While our study did not find significant associations between PCPs’ BMI, personal dietary habits, and self-perceived nutrition competence, the evidence in the literature is conflicting. Some studies suggested that PCPs who had healthy lifestyles (Hung et al., Reference Hung, Keenan and Fang2013) and normal BMI (Bleich et al., Reference Bleich, Bennett, Gudzune and Cooper2012a) displayed greater confidence in nutrition competence and were more likely to provide nutrition care. However, a systematic review showed that physicians’ own weight status was not significantly related to their knowledge, skills, or treatment behaviour of overweight or obese patients (Zhu et al., Reference Zhu, Norman and While2011).
Strengths and limitations
To our knowledge, this is the first study conducted in Singapore to evaluate self-perceived nutrition competence among PCPs. We used the NUTCOMP questionnaire that has been validated with good reliability to measure self-perceived nutrition competence. It has also been used among various healthcare professionals in many countries (Barnes et al., Reference Barnes, Desbrow and Ball2016;Keaver et al., Reference Keaver, O’Meara, Mukhtar and McHugh2018; Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020; Crowley et al., Reference Crowley, Ball and Wall2020b). Additionally, we explored important physician characteristics that could have influenced their self-perceived nutrition competence, such as their work experience, CME engagement in nutrition, personal dietary habits, and previous formal nutrition education.
Our study had a few limitations. First, the self-reported nature of data collection may have led participants to report socially desirable outcomes rather than a true reflection of their self-perceived nutrition competence. We chose to measure self-perceived nutrition competence, which is different from actual nutrition competence and actual provision of nutrition care, as direct measurement of actual competence is challenging and requires considerable resources to examine the care provided to the patient. Moreover, the measurement of self-perceived competence is reasonable as it has been shown to be an acceptable indictor of competence in health professionals (Davis et al., Reference Davis, Mazmanian, Fordis, Van Harrison, Thorpe and Perrier2006). Notably, studies have shown that PCPs with greater self-perceived nutrition competence were more likely to report providing nutrition care (van Dillen et al., Reference van Dillen, Hiddink and van Woerkum2013; Al-gassimi et al., Reference Al-gassimi, Shah, Sendi, Ezmeirlly, Ball and Bakarman2020).
Second, there may be non-response bias due to the suboptimal response rate.
Third, we sampled PCPs from the public primary care setting and did not include those from private clinics. Thus, our sample was not representative of all PCPs in Singapore, and caution is required in the generalizability of our results.
Conclusion
With increasing prevalence of metabolic diseases, of which poor diet is a major contributing risk factor, it is imperative that PCPs are competent to provide good nutrition care. Our study highlighted that PCPs had lowest self-perceived confidence in nutrition knowledge and nutrition skills, and formal nutrition education and more work experience were associated with better self-perceived nutrition competence. To improve self-perceived nutrition competence, more can be done to incorporate nutrition care into our formal medical education. Future research will be needed to first establish the required benchmark of nutrition competency for effective nutrition care provision by PCPs and second to study how nutrition competencies can be better integrated into the curriculum of formal education programmes.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1463423624000689
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Acknowledgements
The author will like to thank Associate Professor Lauren Ball for her kind permission to use the NUTCOMP questionnaire, as well as the Dietetic Service, Clinical Services of NHGP, for their kind permission to use the NHGP fat and fibre questionnaire.
Declarations
The study was approved by the institution review board.
The study was approved by the National Healthcare Group, Domain Specific Review Board, Singapore (DSRB Ref: 2021/00560).
The authors received no financial support for the research, authorship, and/or publication of this article.
All authors have no conflict of interest.






