Aims and definitions
The aim of this service model is to deliver responsive, individualised care, close to home, to adult patients with complex care needs in an acute health-care crisis. Proactive interventions aim to prevent unnecessary admissions to hospital and to facilitate early discharge from hospital when admission is necessary. The period of an individual’s case management is defined by the time required to resolve the crisis and institute a long-term care plan if appropriate. In the context of this service model, a patient with complex care needs is defined as any patient above 18 years of age needing support to access multiple medical and social services simultaneously and urgently.
Background
Upton Surgery is a six-partner, dispensing Personal Medical Services (PMS) Practice providing services for 10 700 patients in the market town of Upton-on-Severn and 48 surrounding villages over a geographical area of 60 square miles. The Surgery also provides medical care for 250 beds in local nursing and care homes. The Practice has a 5-year strategic plan (2008–13) that identifies the need for proactive intervention for patients with complex care needs to avoid unnecessary hospital admissions.
Some patients will have complex care needs for a limited period of time, such as serious trauma patients and orthopaedic patients. However, a significant proportion of patients with complex health-care needs will be people with long-term conditions (LTCs). Improving the well-being of individuals with LTCs, many of whom have complex health and social care needs, is currently high on the UK health service agenda (Department of Health (DH), 2005a; 2010). It is estimated that more than 15.4 million people in England suffer from one or more LTCs and this figure is likely to increase with the ageing population. Individuals with LTCs are more likely to visit their general practitioner (GP), with 80% of such consultations related to these LTCs (Crossland and Dobrzanska, Reference Crossland and Dobrzanska2007). The DH reported that 5% of hospital in-patients, many of whom have an LTC, account for 42% of emergency bed-days (DH, 2004). This population of patients are particularly vulnerable to poor standards of care, poor communication between health and social care agencies and difficult transitions between different care services (Coleman, Reference Coleman2003). The recent DH publication ‘Improving the health and well-being of people with long-term conditions’ identifies a number of ways in which care for people with LTCs can be improved. The document advocates proactive, planned care and services that meet wider holistic needs focusing on overall health and well-being. The use of assistive technologies such as exercise on prescription, holistic weight management programmes, access to psychological therapies, acupuncture and massage is suggested. The document suggest that proactive care planning (including provision of information and support for self-care) improves well-being in a number of ways, including slowing progression of disease and preventing emergency admissions (DH, 2010).
Individualised and proactive care planning is facilitated by collaborative working between health and social care and is of paramount importance in addressing patients’ health and social care needs effectively. It is also important in tackling health inequalities by facilitating a unified system of care and breaking down institutional barriers. This concept has become a central feature of the health and social care agenda, with the National Health Service (NHS) aiming to ‘work together with others to ensure a seamless service for patients’, emphasising the delivery of primary and community health services in partnership with local authorities, voluntary organisations and local communities (Secretary of State for Health, 2000). Although not all patients with complex care needs are older patients, the National Service Framework for older people (DH, 2001) endorses this approach to ensure that older people receive person-centred care, regardless of organisational and professional boundaries. Approaches that arose in response to these directives included locating social services teams in health centres, attaching social workers to general practices, appointing district nurse case managers to work in social services and joint primary health and social care teams (Davey et al., Reference Davey, Levin, Iliffe and Kharicha2005). The Partnership for Older People Projects provided DH funding to develop services for older people. The purpose of the funding was to promote health, well-being and independence and preventing or delaying the need for higher intensity or institutional care. The projects ranged from lunch clubs to more formal preventive initiatives, such as hospital discharge and rapid response services. Over a quarter of a million people used one or more of these services with a reduction in hospital emergency bed-days. The national evaluation of the projects, commissioned by the DH, concluded that the projects appear to have improved users’ quality of life. Projects providing services to individuals with complex needs were particularly successful (Personal Social Services Research Unit, 2010).
Many approaches to collaborative working rely on structural integration, creating teams within the same management structure to achieve a unified system of care. Collaborative working creates significant challenges related to professional identity, status and organisational structure. However, if sensitively and effectively managed, this way of working may facilitate closer working relationships (Huntington, Reference Huntington2003; Manthorpe and Iliffe, Reference Manthorpe and Iliffe2003; Merkeley Keith and Fraser Askin, Reference Merkeley Keith and Fraser Askin2008). Evidence to show that collaborative working has a beneficial impact is variable. In one study, the effect of advanced practice nurse case management on unplanned medical and geriatric hospital admission rates in patients aged 50 years and above, and on admission risk in a ‘higher-risk’ subgroup of patients in the UK showed a reduction in unplanned admission rates in the intervention practices, but this was only in part attributed directly to nurse case management; most of the reduction did not occur in case managed ‘multiple admitters’ (Huws et al., Reference Huws, Cashmore, Newcombe, Roberts, Vincent and Elwyn2008). The authors identified the need for further research to examine the complexity of potential outcomes in terms of the nature and necessity of admissions and most suitable lengths-of-stay in terms of acute care or rehabilitation need. A recent Australian study conducted a series of five systematic reviews of the literature from 1990 to 2006, sampling a spectrum of issues associated with LTCs and complex health-care needs, with a focus on planning and provision of multi-agency care. The study concluded that while multi-agency care planning improved functional outcomes, implementation was complex and testing of strategies for implementation was essential (Mitchell et al., Reference Mitchell, Tieman and Shelby-James2008).
Health-care purchasers are increasingly examining the strength of research evidence on clinical applications when allocating resources (Belsey and Snell, Reference Belsey and Snell1997). In order to develop effective service provision, the service should be based on the best available evidence, measuring the impact of health and social care interventions on outcomes (Hudson, Reference Hudson2002). Most studies evaluating outcomes of collaborative working approaches have focused on supporting or hindering factors or processes rather than on the outcomes for service users and carers (Johnson et al., Reference Johnson, Wistow, Schulz and Hardy2003; Kharicha et al., Reference Kharicha, Levin, Iliffe and Davey2004). Despite the emphasis on ‘evidence-based’ practice, showing statistically significant impact of health and social-care interventions on outcomes will be challenging when the collaborative working processes, as described here, are developed specifically to be relevant and appropriate to the local context rather than to be amenable to statistical evaluation.
The concept of case management has gained increasing precedence as an approach to managing the individualised care of patients with complex health and social care needs (Evans et al., Reference Evans, Drennan, Roberts, Evans, Drennan and Roberts2005; Morales-Asencio et al., Reference Morales-Asencio, Gonzalo-Jimenez, Martin-Santos, Morilla-Herrera, Celdraan-Manas, Carrasco, Garcia-Arrabal, Toral-Lopez and Carrasco2008). In 2005, the DH produced a strategy for caring for individuals with complex care needs using a case management approach. Case management is the process of planning, co-ordinating, managing and reviewing the provision of health and social care for individuals with complex needs (DH, 2005b). It is therefore dependent on effective collaborative working. Essentially, the aim of case management is to develop cost-effective mechanisms to coordinate services to improve the quality of life of patients (Crossland and Dobrzanska, Reference Crossland and Dobrzanska2007). Service delivery models that employ a case management approach often provide a service to one particular subgroup of patients with complex health-care needs, such as patients with mental health-care needs (Holmwood, Reference Holmwood1998), orthopaedic patients and older patients (Evans et al., Reference Evans, Drennan, Roberts, Evans, Drennan and Roberts2005) rather than providing a service for any patient with complex health-care needs in an acute health-care crisis.
The DH recognises that there are still significant challenges to achieving their objectives with respect to delivering care closer to home including appropriate infrastructure, leadership skills, workforce and technology (DH, 2008). The service model described in this paper relies on physical co-location of health and social care teams in a new purpose-built GP Practice and effective multi-agency collaborative working to deliver individual case management, rather than structural integration of individuals into dedicated health-care teams. Leadership skills within the Practice have enabled the use of a championed, project management approach to the development and delivery of this service. The service model is described here and includes an evaluation of patient-centred and financial outcomes.
Service model
The aims of this service model are to prevent patients with complex needs in acute health crisis being admitted unnecessarily to hospital and facilitating discharge in unavoidable admissions.
Initially, the partners at Upton Surgery were keen to provide additional local care for scheduled elective orthopaedic patients (eg, total hip or total knee replacement operations) to reduce hospital stays for these patients, using the model set up by the Royal Orthopaedic Hospital, Birmingham Royal Orthopaedic Community Scheme (ROCS; Closs, Reference Closs1995). A small team to develop and pilot an approach was envisaged and first appointments to this team were made in January 2008. The project was funded through Practice-Based Commissioning and PMS funding and championed within the Practice by a GP-lead and by the practice manager. The project was also supported by the South Worcestershire Commissioning Cluster as one of a series of pilots aimed at reducing hospital admissions and facilitating early discharge within the region.
The service model currently in place has developed significantly since the inception of the project. The initial case load of scheduled elective orthopaedic patients has been subsumed by a much broader remit including any patient with complex needs in acute health crisis. The prime objective of the service model is prevention of unnecessary hospital admission and the secondary objective is limiting in-hospital time.
The changes in case load and primary objective were in response to the local needs. The numbers of people having elective hip and knee replacement were not large and analysis of the average length of stay showed that this had already been significantly reduced by local changes in management. The ROCS model had been established in response to much longer periods, for example, 10–14 days, and was therefore not appropriate for the local needs. In contrast, there was an unmet need for reactive complex case management.
The team leader (the case manager), working with the project’s champions in the Practice, was instrumental in developing the concept into a successful working model. This evolution has required changes in the team, with respect to staffing and skill base, changes in line management responsibility and the recognition of the need for a specific budget for the project to be successful. The service model currently in use is described below but remains reactive and responsive to the local context.
The Complex Care Team
The Complex Care Team is led by the case manager who has line management responsibility for the team. Formal line management of the case manager is with the NHS Worcestershire. Informally, the GP lead for the project and practice manager provide advice and direction. The case manager has over 20 years of nursing experience in primary care and has some previous experience of service development. Although not recruited during the evaluation period, the case manager is now supported by the deputy case manager (Band 6). The deputy case manager is an occupational therapist. Initially, the case manager was supported by two health-care support assistants; the team is now supported by only one assistant. The support assistant has been given in-service training in intermediate care skills through the NHS Worcestershire’s competency-based training programmes. The team has access to physiotherapy through the community physiotherapy team based within the surgery. The complementary skill base of the members of the team is important, but the key skills are interpersonal skills, matrix management, clinical leadership and project management.
The manager holds an NHS Worcestershire team budget for the administration and management of the team. The role also holds a budget for spot purchasing of beds for periods of 1–2 weeks in local care homes (three in the local area) to prevent unnecessary admission to secondary care. Negotiated agreements are in place if vacancies are available. The budget is occasionally used for emergency private care in the home where this will contribute to admission prevention. Surgery GPs provide medical cover.
The team is physically co-located with the surgery-based social workers. The Complex Care Team works closely with the Practice GPs who have medical responsibility and provide guidance; with social workers who provide complex social support and longer-term support; with district nurses providing specialist nursing care (eg, intravenous therapy and end-of-life care); with the Surgery Team for administrative and information technology (IT) support; and with local voluntary and charity organisations (eg, Age UK, Friends of the Elderly). The physical co-location of the team with surgery-based social workers and the close proximity to the District Nurse Team and community physiotherapist enable effective communication, referral and planning that is patient-centred and facilitated by the Complex Care Team (Figure 1). The staff level within the team currently means that a service can only be provided on weekdays between 9am and 5pm.

Figure 1 Multi-agency patient-centred care
In addition to the relationships described above, the extended teams/services accessed include:
• Community hospitals (Pershore, Malvern and Evesham)
• Worcestershire Royal Hospital
• Local voluntary sector/charities
• Local housing teams
• Intermediate Care Centre
• Specialist Nursing Teams
• Palliative Care Services
• Continuing Health-care Team
• Local nursing and residential care homes
• County Council Admission Prevention Team and Reablement Team
• Falls coordinator
• Other hospitals outside the county.
Case identification
The Complex Care Team will consider any patient registered with the Practice, aged 18 years or above in acute health-care crisis with complex medical and social care needs. Many of these patients will be older patients with LTCs; however, advice and support is provided to clients with diverse problems and within all adult age groups. Patients who will benefit from support from the team are identified through:
• Other health-care professionals
• Community hospitals
• Secondary care discharge teams
• Relatives/friends/family
• Patients identified through the ‘patients at risk of re-hospitalisation’ assessment tool (The King’s Fund, 2009) and ‘frequent flyer’ (repeat admissions) information from NHS Worcestershire (formerly the Primary Care Trust (PCT))
• Analysis of long-stay data from the NHS Worcestershire
• Searching NHS Worcestershire and secondary care IT systems.
Awareness raising has been important in raising the profile and remit of the team within the local health-care community. The case manager chairs a multi-disciplinary review of the current caseload and patients at risk on a bi-monthly basis. GPs, specialist nurses, social services and local practitioners are invited to these review meetings. A traffic light system is used to indicate patients at risk. The team accepts referrals from any source outside those meetings.
The team’s caseload is very variable and patients have different levels of need. The team prioritises their cases with reference to the GP partners and usually admission prevention has first priority. The caseload may include 30–40 patients in the community and 10–20 patients in secondary care at any one time. Patients in acute need will constitute about 5–10 patients at any one point in time. Some patients may only have one visit from the team. For example, a patient had a phobia about visiting the GP, the case manager visited the patient and by working with the family facilitated a visit to the GP who was then able to resolve the problem. Signposting is also provided for patients and/or carers. In addition to acute health-care crises, the caseload has evolved to include end-of-life care. End-of-life would not normally be classed as an acute health-care crisis but requires similar multi-disciplinary facilitation.
Case management
By necessity this service should be rapid and responsive and requires co-ordination and mobilisation of the right services at the right time. The nature of each intervention is unique to the patient, as it is patient-centred and needs-led. The case manager or the deputy case manager will assess the patient’s needs in discussion with the patient and carers (where appropriate). The Complex Care Team identifies and oversees the delivery of appropriate services to support the patient. Two illustrative cases are described (Table 1). Where a patient’s condition changes dramatically or general circumstances change, the team rapidly and flexibly alters service provision accordingly. For example, if the medical condition deteriorates and acute hospital assessment is required then the patient will be admitted to hospital (and the team provides in-reach to monitor and support). If a patient is no longer safe to stay at home but does not require an acute admission the team will endeavour to secure an admission-prevention bed locally and input-relevant services, including therapy, as required. Collaborative discharge planning would commence almost on admission in these circumstances as beds are only available for a maximum of 1–2 weeks.
Table 1 Case management examples
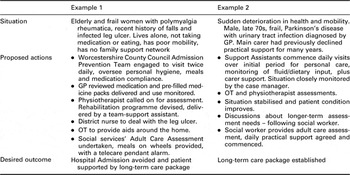
GP = general practitioner; OT = occupational therapist.
The Complex Care Team’s role in the end-of-life care is to work closely with patient and relatives to facilitate preferred place of care for end-of-life and to coordinate care collaboratively to achieve this. This includes fast-tracking patients for continuing healthcare and securing/coordinating appropriate services as required. As this service has evolved, calling on the multi-disciplinary facilitative skills of the team, they have undertaken more and more end-of-life care successfully. Where it is not possible to deliver care at home, care is provided as close to home as possible, for example, in a local care home. The team reflects on the care given in these circumstances and learn from each other at the monthly Multi-disciplinary Gold Standards Palliative Care meeting held at the surgery.
The following case indicates the breadth of the potential caseload and the diverse nature of service provision.
A 46-year-old female involved in a road traffic accident out of county, who had sustained multiple injuries including bilateral leg amputations, was referred to the Complex Care Team by the discharge team at Worcester Royal Hospital. An out-of-area hospital had contacted the Worcestershire Royal Hospital in an attempt to transfer the patient to an acute bed locally. The patient’s husband was very much stressed and exhausted with travelling to visit and the young daughter was having difficulties coping with the situation. On initial discussion with the local discharge team and out-of-area hospital, it was felt that an acute bed was no longer needed. The patient’s husband and young family had recently moved to Worcestershire and were living in rented accommodation unsuitable for the patient to return because of access problems so the patient was deemed homeless. There had been links with the local social services over the previous month, but this had not facilitated getting the patient closer to home. There was also concern about the significant transition from acute hospital to home after such significant trauma. Discussions were initiated with the patient, family and ward staff to ascertain their wishes and needs. It was suggested that finding a suitable rehabilitation bed within the county would be the first move so that it would be easier to access local services. This was agreed and a bed found on a dedicated rehabilitation ward in a community hospital with support from a nurse consultant in physical disabilities. The patient was transferred within 4 days. This was a positive move for the patient and her family and improved access to services to address discharge planning issues. Eight weeks later the patient was discharged to new, private accommodation requiring minimal practical support with on-going services in place, including GP, physical disabilities nurse consultant, social worker and Upton Complex Care Team. The patient is doing well, has been at home for many months and maintains intermittent contact with the Complex Care Team by phone.
Service evaluation
The service provided by the Complex Care Team over the period June 2008–June 2009 was independently evaluated by the University of Worcester in a pilot study to assess the impact of the service on hospital bed use, the ‘patient experience’ of the admission-prevention service and surgery work practices. The views and experiences of those involved in the project contributed significantly to the evaluation. The reduction in secondary-care costs associated with hospital admission was also evaluated.
Method
Design
Quantitative analysis was used to assess whether the introduction of the service model had an impact on hospital bed use. Both qualitative and quantitative methods were used to assess the impact of the admission-prevention service on the patient and carer experience and the staff experience.
This evaluation does not include data about patients for whom signposting was provided or patients who benefited from one-off visits from the team.
Participants
The sample consisted of patients, social workers, GPs, nurses, a practice manager and the capacity manager for Worcestershire Acute Hospitals NHS Trust.
Procedure
Data (Table 2) were obtained from the NHS Records of Admissions and a caseload database kept by the case manager. The caseload database recorded patient age, gender, diagnosis, care pathway, number of visits and length of stay in hospital where appropriate. Data from 251 patients were recorded in this database between inception of the project and the end of the evaluation period (January 2008–June 2009). Additional information on the quality of the service was sought from some patients (n = 21) who received admission-prevention support.
Table 2 Evaluation participants
GP = general practitioner.
aPatients supported to prevent hospital admission.
bThe response was the collated response from a team of nurses.
Questionnaires were made available to most patients who received significant care in the community setting to avoid hospital admission (n = 21). Patients (and their carers) who received end-of-life care (as opposed to care associated with an acute health crisis) were not given the questionnaires. The questionnaires (Table 3) used in this pilot study were developed specifically for this study and have not been validated in other studies. The questions related to the patient experience of the service model and sought suggestions for improvement. The questionnaires were designed to be completed by the patient and/or their carers. In order to evaluate the quality of care delivered and the patient experience, patients and carers were asked to rate various aspects of the service. The questionnaires also invited free-response comments about the service.
Table 3 Questionnaire
Some health-care professionals were approached to provide free-response comments about their experience of the service model.
Analysis
Hospital bed use (emergency admission and excess bed-days) was analysed quantitatively using the Wilcoxen signed-rank test (non-parametric, limited data set).
A financial evaluation was conducted to estimate the reduction in secondary care costs, over and above salary costs, for admission prevention, in agreement with the South Worcestershire Commissioning Cluster. Savings were estimated by comparison of the actual cost of treatment by the Complex Care Team, with the estimated cost of a hospital admission by assigning an appropriate HRG (Healthcare Resource Group) code and an HRG episode cost.
Both quantitative and qualitative methods were used to assess impact of the admission-prevention service on staff, patients and careers. Feedback from carers and patients was analysed collectively. Thematic analysis was carried out on the qualitative data obtained from the questionnaires, from free-response feedback from health professionals and from unsolicited feedback. Thematic analysis is a method for synthesising findings from a number of qualitative studies and includes identifying key themes in the included studies and then summarises the evidence within these themes or categories (Morse and Field, Reference Morse and Field1995; Buetow, Reference Buetow2010).
Ethics
The evaluation was conducted in accordance with the ethical guidelines of the British Psychological Society (British Psychological Society, 2009). Ethical approval for the evaluation was obtained from the ethics committee of the Institute of Health and Society at the University of Worcester.
All participants were made aware of their right to withdraw from the study at any time, without explanation. The anonymity and confidentiality of informants were assured at all times. All data generated by the evaluation were treated confidentially, reported anonymously and stored in accordance with the Data Protection Act (1998). Consent was obtained from patients providing case studies.
Results
Caseload
The main category of clinical diagnosis among patients requiring significant input and ongoing monitoring from the Complex Care Team during the evaluation period was musculoskeletal (n = 194); however, the primary clinical diagnoses were varied (see Figure 2). The patients ranged in age between 36 and 98 years with a mean age of 83 (SD = 10.6) years and included 71 men and 118 women (in five cases gender was not recorded).

Figure 2 Broad diagnostic categories of caseload
Table 4 gives details of patients supported through the Complex Care Team to prevent hospital admission (June 2008–June 2009). Table 5 provides data for patients for whom hospital stay was reduced by the Complex Care Team (December 2008–June 2009). Data from these tables show a higher proportion of female patients benefiting from the service provided by the Complex Care Team and that the age group benefiting most from hospital stay reduction is the older patient group (75–98 years).
Table 4 Patient data – hospital prevention

COPD = Chronic obstructive pulmonary disease; NOF = fractured neck of femur.
Table 5 Patient data – reduced hospital stay

HRG = Healthcare Resource Group.
Hospital bed use
There were no statistically significant changes in the number of non-elective emergency admissions per year over the financial years 2006–07 to 2008–09 (monthly means per year were 53, 49 and 51 patients for 2006–07, 2007–08 and 2008–09, respectively). The month-on-month data for both non-elective emergency admissions and excess bed-days was highly variable. The reduction in mean excess bed usage between before and after the introduction of the service provided by the Complex Care Team (monthly means are 35.3, 24.1 and 21.8, respectively) was not statistically significant by comparison of the month-on-month data; however, this translates to a reduction in excess bed-days from 520 per 1000 patients in 2007–08 to 232 in 2008–09.
Financial evaluation
During the evaluation period (June 2008–June 2009), the Complex Care Team identified 21 patients (Table 4) who were supported by deployment of the County Council/PCT-funded admission-prevention team with an overall estimated saving of £54 111 on hospital bed costs (using the methodology described above). In addition, PBC funds were used to spot purchase beds in local care homes rather than using hospital beds and the savings achieved by this approach was estimated as £33 200. The team also facilitates early discharge from hospital (Table 5). The reduction in excess bed-days equates to a saving, over and above salary costs, of £61 436 in 2008/09 on excess bed-days. The overall saving for June 2008–June 2009, over and above salary costs, is estimated to be around £148 000.
Quantitative questionnaire data evaluation
Service delivery to the 21 admission-prevention patients over the period of June 2008–June 2009 was evaluated with respect to the quality of care delivered, the patient experience and the reduction of secondary care costs. Seventeen feedback forms were received from this patient group. All feedback received from patients and carers rated the service ‘Good’ or ‘Excellent’ for overall quality, communications, information and advice, accessibility and helpfulness. (Figure 3) An ‘Average’ rating was received for flexibility and quality of service; however, this referred to an evening service not provided by the Complex Care Team.

Figure 3 Patient/carer assessment of service
Qualitative questionnaire data
Patients and carers were also asked more specific questions about the service provided (Figure 4). Patients felt supported, happy with the standard of care, had suitable equipment provided and felt that the staff were adequately trained. Most patients felt that the service had aided their recovery and of those at risk of going to hospital; most felt it was a better alternative. Three patients had reported an issue to the case manager, but were satisfied with the response that they received.

Figure 4 Patient/carer feedback on service and care provision
In addition to the formal questionnaires, 11 unsolicited notes of gratitude from patients (or their families) were received by the Practice expressing gratitude or praise for the service.
Analysis of qualitative data
Thematic analysis of the qualitative data from patient feedback forms, professional feedback and correspondence revealed four broad themes:
1) Collaborative working
2) Benefit to the patients, families and carers
3) Benefit to professional staff
4) New initiatives and future developments.
Collaborative working
This was the strongest theme. The team has created a more coherent service, allowing quicker assessment of patients and offering a more efficient and appropriate pathway through a greater understanding of the range of services available. Strong working relationships have been established with patients and families, Upton Surgery’s GPs, district nurses, social workers, care homes and NHS secondary services (especially Worcestershire Royal Hospital):
(The team are) ‘…often able to access services that I wasn’t even aware existed!’
(GP, Upton Surgery, male)
Benefits to patients, families and carers
Patients, family and professionals commented on the benefit that the service has had on patients taken on by the Complex Care Team.
Patients thought that the service had aided recovery. Several patients, families and staff mentioned the benefits of a reliable, knowledgeable team to guide patients and their families through a crisis. Several patients felt that the service had given them confidence by providing them with the skills to regain their mobility and independence, aiding their recovery. For example:
‘The care I received was just the ‘kick-start’ I needed to get me back to health and independence.’
(Patient A, female)
‘Without this service I am sure my husband would not have regained his mobility.’
(Carer A, female)
A social worker commented that the service allows a fairer assessment of longer-term needs while the patient recovers from the initial crisis. This long-term approach helps addresses repeated re-admissions, the ‘revolving door syndrome’.
Collaborative working was cited as providing a quicker service, continuity of care and a seamless service.
‘(Collaborative working) … inevitably enhances patient confidence and satisfaction which impacts positively on their recovery.’
(NHS Acute Trust Capacity Manager, female)
Benefits to professional staff
Collaborative working was identified as beneficial, avoiding unnecessary overlap or neglect with enhanced access to, and knowledge of, a wider range of services. ‘This service preempts national NHS initiatives towards an integrated team approach’ was one of the comments recorded. A GP commented that they could not imagine how they managed without the service. Staff felt that the impact of the team had engendered valued positive patient feedback.
Staff felt that there had been a significant drop in admissions and decrease in extra bed-days, confirmed by the evaluation. Two feedback statements suggested that the service was cost-effective.
‘The number of saved emergency admissions and facilitated early discharges has been huge.’
(GP, Upton Surgery, female)
‘Noticeable decrease in hospital admissions from local rest homes already seen in May 2009.’
(District Nurse Team Leader, female)
Although ‘benefit to professional staff’ was a prominent theme, not all the feedback was positive. A professional group at the Surgery felt that they had not been appropriately involved in the project. This issue has since been addressed by establishing weekly multi-agency team meetings.
New initiatives and future developments
Several sources suggested that it would be beneficial for the team to grow and develop and that the funding for the team should be maintained or increased. There was a desire for the team to take on more staff so that they could cover more hours (patient visits were only in weekday mornings during the evaluation period).
‘To whom it may concern please provide adequate long-term funding for this project – the service provided is excellent & takes immense pressure away from immediate family & friends in times of crisis.’
(Carer B, female)
The feedback forms welcomed new initiatives such as the postural stability classes, introduced in the past few months of the evaluation period. Increasing support for patients with LTCs and closer liaison with local nursing and care homes were mentioned as positive new steps forward as the team increased its outreach.
Evaluation limitations
The evaluation described here was a pilot study and the questionnaires were developed for this study. A greater depth of qualitative information may have been obtained by employing graded responses for all questions and the use of neutral questions, however, free response sections were provided on the questionnaires. In the evaluation period the number of patients receiving admission-prevention support from the Complex Care Team was relatively small and non-respondents were not followed up. Similarly, comments were received from both patients and carers and their views combined. It is possible, of course, that views may differ between these groups and further studies with larger numbers may help clarify this. The service model was evaluated during a period of significant development in response to the local context. Ideally, the value of a service model would be proven statistically using a non-randomised controlled intervention study and by comparison with other practices not using a similar service model. Such studies will still be confounded by small sample sizes and local issues.
Discussion
We have described a multi-agency collaborative service delivery model that has evolved to meet the local needs of a rural GP Practice. Although it was initially envisaged that it would provide support to minimise hospital care for elective orthopaedic patients, it now focuses on preventing patients with complex care needs in acute health crisis from unnecessarily being admitted to hospital. The remit is in reality much broader, providing support that ranges from signposting for ad-hoc health-care queries through to relocation of patients in out-of-area long-term health care.
Studies evaluating the effectiveness of case management approaches have reported an improvement in older people’s access to health and social care services, enhanced quality of life and cost effectiveness. However, evidence of the effectiveness of case management is arguably limited. Evans et al. (Reference Evans, Drennan, Roberts, Evans, Drennan and Roberts2005) identify that studies are often based in different care settings, have different drivers and lack a shared definition of case management, or the model is ill described. These limitations apply to the service model developed here, which is specific for the needs of the local community. In addition, the service model has been constantly evolving, therefore lacking even internal consistency. Despite this, the evaluation of the effect of the case management approach on both the patients and surgery team over a period of an year shows evidence of patient satisfaction, improved outcomes and value for money.
The leadership skills and working practices of the Complex Care Team have created a recognised and accepted central point of contact for all services involved in care of patients with complex needs, strengthening working relationships and shared knowledge between disciplines. Developing this service model has been a learning process for all those involved in its development. The learning points may be of interest to other practices developing similar models. In its initiation, developing the service was treated as a project and project champions identified. The case manager needed to challenge traditional roles and boundaries to establish an effective service delivery model and this was facilitated by the encouragement and support given by the Practice champions to challenge boundaries and to think and work in new ways.
At a management level, it was felt that the case manager, as team leader, should have line management responsibility for the team and should hold a budget. Direct line management of team members is essential for effective case-load management and for personal development and performance management of staff. Budgetary responsibility and autonomy were essential to establish agreements with local care providers and for spot purchasing of beds for admission prevention is required. The service model could not work without the Complex Care Team building effective working relationships that foster collaborative working. Issues that arose in developing this service are considered below.
Service development
The Complex Care Team negotiates with relatively senior staff in the health and social care sectors who may work with, but are not in the employ of, the Surgery. With only one member of the team with a skill-base and level of seniority appropriate for these tasks, the case manager was stretched too thinly to work effectively. Re-assessing the team structure and replacing one of the health assistants in the original team with a much more senior deputy case manager has enabled the team to work much more effectively. Therefore, the traditional pyramidal team structure, with a senior member of staff, the case manager, supported by two health-care assistants, turned out to be an ineffective team structure. The Complex Care Team needs senior staff with a varied skill base (clinical/nursing), creating a team that is ‘top-heavy’ rather than a traditional pyramid-shaped organisation.
The multi-agency working model requires staff in the team to have excellent interpersonal skills. The case manager, in particular, needs high-level leadership skills that enable her to motivate and lead a multi-agency team, that will be unique to each case, for whom she does not have line management responsibility and whose members are not necessarily employed by the same organisation. The case manager has challenged traditional boundaries by taking the initiative to create transient working partnerships where she is effectively the lead of staff, such as GP’s, who might be otherwise be considered her superior. This type of team working is common in other sectors.
Establishing a new service model that is highly collaborative in nature requires multi-agency working in novel partnerships. This requires some prior experience in service development or the flexibility to work effectively in an environment where established processes and procedures do not exist but need to be developed in partnership with other health-care services. As an example, working practices with local secondary care organisations were established to set up the secondary care in-reach programme. The ability to negotiate agreements both in working partnerships and in financial arrangements (eg, bed space in local care homes) is also essential.
Maintaining a large caseload of patients each with a unique care package requires the logistical and management skills used in project management. To be effective it also requires appropriate administrative and IT support. The development of appropriate IT support systems is ongoing, building on the initially ad hoc simple databases.
Important service factors
The physical co-location of many of the health and social care agencies used by the Complex Care Team in the Upton Surgery complex is seen as key to the success of the service model. The good relationships engendered between staff working physically in the same location and sharing social facilities enhances communication and effective working. Similarly, the easy accessibility of the Complex Care Team to other health-care services in the building means that referral to the service is much easier. Pre-negotiated agreements for access to services facilitate access in emergency scenarios.
Challenges
The small size of the Complex Care Team is a significant issue. For example, absence due to sickness or holidays compromises the ability of the team to respond rapidly. Similarly, the team is unable to offer a 24-h service and is unable to cover weekends, meaning that a truly urgent health-care crisis in the evening or at the weekend for a patient who would normally be referred to the team, will probably be admitted to hospital before being picked up by the team.
During the evaluation period the NHS Worcestershire did not have intermediate care services available to complement and interface with the Complex Care Team. Intermediate care services form an invaluable component of any care plan trying to deliver care closer to home. In addition, the nearest community hospital is 8 miles away. There is no automatic mechanism for identifying or monitoring patients admitted to secondary care outside of the county; however, in one case the team was able to facilitate the transfer of a patient from an out-of-county hospital back to a local hospital at the request of the family.
Some GP Practice staff felt that they were not adequately involved in and informed about the activities of the Complex Care Team and felt rather disenfranchised. This issue has been addressed by establishing the monthly review meeting with open invitations to all disciplines within the Practice. This has not entirely resolved the problem and provides an example of the challenges of new ways of working and challenging traditional boundaries not always being comfortable for all staff.
Service evaluation
The service evaluation aims were to assess the impact of the service on hospital bed use, the ‘patient experience’ of the admission-prevention service and Surgery work practices.
The Practice has reduced excess bed-days and reduced costs, saving £148 000 over and above salary costs between June 2008 and June 2009.
Qualitative analysis of feedback indicated a ‘seamless service’ had been achieved in the admission-prevention role, aiding patients smoothly through their crisis, a key objective of the NHS (Secretary of State for Health, 2000). The service allows people to be treated in, or close to their own home and this was identified as a crucial factor in the recovery process. Patients described gaining confidence and independence through support provided by the service. The evidence suggests that the consistency and quality of care provided to patients have been improved by the introduction of the Complex Care Team. Although the number of patients in the evaluation of the admission-prevention service was relatively low, the Practice also received unsolicited positive feedback within the evaluation period and has not received any unsolicited negative feedback.
The Practice has benefited from the introduction of the Complex Care Team by having a specialist team who can access the most appropriate pathways for the patients whose cases it manages. It has strengthened collaborative working, creating a more efficient service for patients and colleagues.
The Complex Care Team will continue to refine its service and has several new initiatives in progress or planned. These include: a pilot of a postural stability programme for people identified at high risk of falls, a pilot site for individual Level 1 and 2 Falls assessments (part of NHS Worcestershire Falls pathway programme-training underway), a local pulmonary rehabilitation programme for people with chronic respiratory problems and further Nurse-led Clinics developed within the practice for people with long-term conditions.
Conclusion
Upton Surgery, in developing its Complex Care Team has significantly strengthened local collaborative, multi-agency working, creating a more sophisticated and effective service for its patients and colleagues. Champions for the project, providing support and encouragement to challenge boundaries, both at inception and in its evolution have been critical to the success of the project, as have the inter-personal and leadership skills of the Complex Care Team staff. The Complex Care Team has sensitively challenged cultural and traditional roles and responsibilities and enabled effective and cohesive teams. The small team size means that absence has significant impact on the team but this is counterbalanced by the co-location of the team with other health-care agencies within the GP Practice premises. Evaluation of a service that is optimised for the local context is unlikely to provide statistically significant data that can categorically prove the value of the service; however the qualitative evaluation of the admission-prevention service described here has shown patient satisfaction with the service. The financial evaluation has shown the Complex Care Team has delivered savings to the NHS and the health-care staff has confidence in the service model. The development of this service model may provide learning points for other practices seeking to align themselves with current policy directives that promote collaborative working, for example, the recent DH publication ‘Improving the health and well-being of people with long-term conditions’.
Acknowledgement
No funding sources supported this work.











