Dementia is a relatively common diagnosis among the elderly population. The frequency is thought to be higher in hospitalised patients than in community dwellers (Royal College of Psychiatrists, 2005), and is often unrecognised in the former group (Reference Jorm and JolleyJorm & Jolley, 1998; Reference Laurila, Pitkala and StrandbergLaurila et al, 2004). Providing hospital care for the older person with dementia has implications for individual patient outcomes and broader financial costs.
Psychiatric assessment of older people in hospital may be an individual's first contact with mental health services, or may occur because specific review is required of a known patient. The aim of this study was to determine the proportion of elderly patients admitted to medical or geriatric wards thought to have a diagnosis of dementia, and their contact with local psychiatric services.
Method
An observational study of patients aged 65 years and over admitted to an acute medical unit or geriatric assessment unit generated 161 sets of patient details (80 acute medical admissions and 81 geriatric medical admissions). The patients were examined by the Department of Medicine for the Elderly (DoME) to determine potential diagnoses of dementia (using the DSM–IV checklist; see Appendix) (American Psychiatric Association, 1994) and delirium (using the Confusion Assessment Method; H. Hu, personal communication, 2006).
The demographic details of the 161 patients were then used by an assessor masked to patient diagnosis to enable a search of a computerised database, the Patient Information Management System, to determine those known to the local psychiatric services. Overall, 45 such patients were identified and the psychiatric case notes of 44 were examined by hand (one set of notes was missing). A further six patients had psychiatric case notes that were unavailable because they were outwith the catchment area.
Psychiatric diagnosis was sought along with relevant dates and follow-up where documented. Where data appeared incomplete, community psychiatric nurses were asked to confirm diagnosis using nursing notes. Once data had been collected from the psychiatric notes, psychiatric diagnoses given by the DoME were revealed. The diagnoses documented in the psychiatric case notes were compared with the diagnoses given by DoME staff. Dementia was the main diagnosis of interest, but other diagnoses were recorded.
Results
Of the 161 patients, 44 had available psychiatry case notes (Fig. 1). Of these 44 patients, 13 were men (30%) and 31 were women (70%). The mean age of the cohort was 80 years and the mean age of patients known to psychiatric services was also 80 years.
From the medical cohort of 161 patients, 111 had a likely diagnosis of dementia as defined by the DSM–IV checklist (69%). Of these 111, only 22 (20%) had locally available psychiatric case notes documenting a diagnosis of dementia. Of the 44 patients with psychiatric case notes, 20 were known to services prior to the index hospital admission and 19 were referred as new cases. Psychiatric diagnoses are given in Table 1.
Table 1. Psychiatric diagnoses in the sample
| Patients already known to psychiatric services (n=20) | Patients referred as new cases (n=19) | |
|---|---|---|
| Diagnosis | n | n |
| Dementia | 12 | 15 |
| Depression | 6 | 1 |
| Dementia with delirium | 0 | 2 |
| Psychotic depression | 1 | 0 |
| Hypomania secondary to steroid use | 1 | 1 |
Medical staff referred five patients for psychiatric review who were never seen by psychiatry and whose psychiatric case notes contained no information regarding follow-up. Proposed diagnoses by medical staff for these individuals were dementia in three cases. There was disagreement between the DoME proposed diagnosis of dementia and the diagnosis given by psychiatric staff in two cases: the psychiatric staff diagnosed depression in one case and hypomania secondary to steroid use in the other.
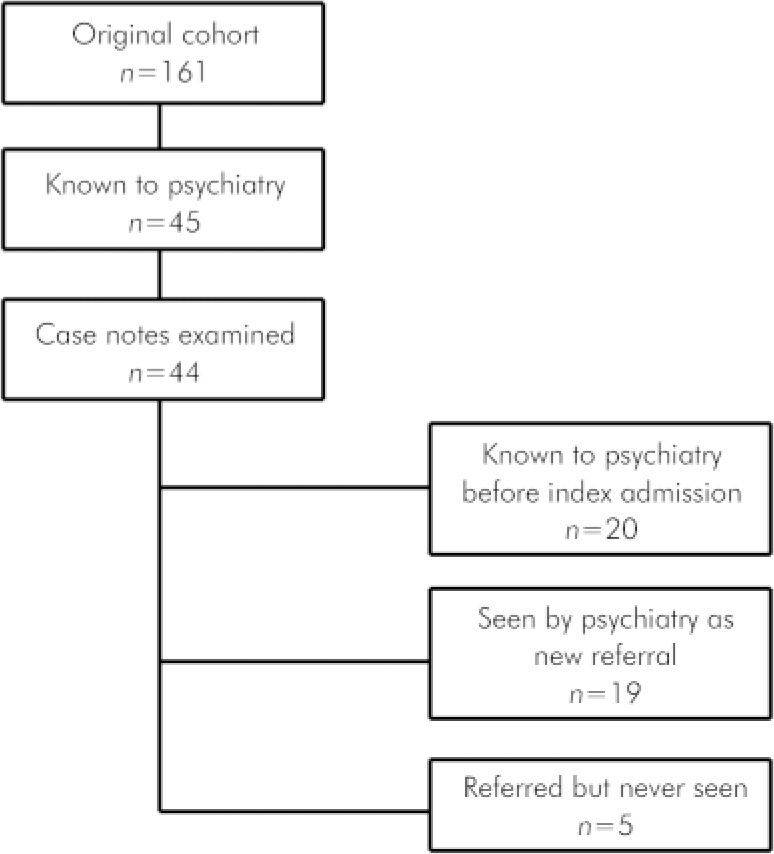
Fig. 1. Study profile.
Discussion
In this sample, 20% of patients considered by DoME staff to have dementia were known to psychiatric services as having dementia. A minority were referred during the study period as new cases. It would seem that the majority of individuals with dementia in our sample were being managed by primary care and other services without ever coming to the attention of mental health services. It is possible that some patients were not known to health or social services at all and that admission to a medical ward was the first time a diagnosis of dementia had been considered. There is potentially substantial unmet clinical need. It could be argued that involvement with psychiatric services is not always necessary when a person has dementia but only when particular problems arise. It seems likely that the diagnosis of dementia is not solely determined by psychiatrists and that sharing of this information between professionals is not universal.
The DoME and psychiatric staff might have used different screening tools with potentially different validity to reach diagnosis. The DSM–IV checklist was used by DoME staff to define cases, but psychiatric notes generally did not contain information as to how the diagnosis had been reached. It is likely that diagnoses by psychiatric staff were based on the Mini Mental State Examination (Reference Folstein, Folstein and McHUGHFolstein et al, 1975) and clinical presentation. There may be subtle differences in the way in which diagnosis was reached, as the psychiatric assessment could have been made by a liaison nurse, a consultant psychiatrist or a specialist registrar; it was not obvious from perusing the notes which professional had carried out the assessment.
There was disagreement about diagnosis in some cases. Dementia was diagnosed by DoME staff in one case in which psychiatric staff diagnosed depression and in one case thought to be an organic state secondary to steroid use. It would be difficult to be certain about these individuals’ diagnoses without accurate longitudinal information which is not yet available. Five patients were referred for psychiatric assessment but were never seen by psychiatric services; three of these patients were thought to have dementia. There are implications for patients who ‘slip through the net’. It was not possible from examining the notes to determine whether these individuals were later picked up by primary care or social work services.
The proportion of patients in medical and geriatric wards thought to have dementia in the original sample was high, with a point prevalence of 69%. This is greater than the prevalence of 5–45% (mean prevalence 31%) mentioned in the Who Cares Wins document from the Royal College of Psychiatrists (2005). This study population may, therefore, not be entirely typical of older people in hospital. It is also possible that there is over-diagnosis of dementia in this sample due to observational bias or reliance on the DSM–IV checklist.
Hospital care or DoME admission could represent a default pathway whereby older people with dementia come into hospital when a crisis arises at home. It is possible that the DoME is more accessible than psychogeriatric services, especially out of hours. Relatives and carers may be more familiar with the idea of being sent to the accident and emergency department with their loved one, rather than relying on the referrer contacting a community psychiatric nurse or psychiatrist for telephone advice.
This study may have limitations because of the small number of psychiatric case notes examined. The six out-of-area case notes were not examined for pragmatic reasons and it is not possible to comment how the final results might have been affected.
Future research could examine if these results are similar to findings in other geographical locations and whether the model of psychiatric liaison provided has any impact on numbers of patients seen. Longitudinal information on service use and individual outcomes would be interesting to determine if there is a key time when psychiatric input becomes most valuable. Follow-up information on the cases where there is disagreement on diagnosis may be of educational value.
The optimal balance between confidentiality and coordinated team working may be difficult to determine, but could offer benefits to individual patients by avoiding hospital admission, shortening length of stay and improving outcomes. Providing expert advice on diagnosis and management has scope to improve care for some of our most vulnerable elderly people.
Appendix
DSM–IV dementia checklist
For a diagnosis of dementia to be made according to DSM–IV all criteria A to D must be satisfied.
-
A. The presence of multiple cognitive deficits, one of which must include memory impairment.
-
B. At least one of the following cognitive disturbances:
-
• dysphasia
-
• dyspraxia
-
• agnosia
-
• disturbance of executive functioning.
-
-
C. The above symptoms must be sufficiently severe to cause significant impairment in the patient's social or occupational functioning and represent a decline from previous level of functioning.
-
D. Delirium must be excluded.
Declaration of interest
None.
Acknowledgements
Many thanks to the staff of the Glasgow Royal Infirmary academic department for providing the original data. We thank Professor Stott for his encouragement and advice on editing. Thanks are also due to the secretarial staff at Parkview Resource Centre and the records staff at Parkhead Hospital for sourcing case notes needed for the study.





eLetters
No eLetters have been published for this article.