Introduction
Hospital readmissions and timely outpatient follow-up after discharge are commonly used benchmarks for assessing the quality of psychiatric care (Byrne, Hooke, & Page, Reference Byrne, Hooke and Page2010; Durbin, Lin, Layne, & Teed, Reference Durbin, Lin, Layne and Teed2007; Hermann et al., Reference Hermann, Mattke, Somekh, Silfverhielm, Goldner, Glover and Chan2006; Katschnig et al., Reference Katschnig, Straßmayr, Endel, Berger, Zauner, Kalseth and Šprah2019; National Committee on Quality Assurance: HEDIS Measures and Technical Resources, 2021), especially for schizophrenia and other psychotic disorders (Patel et al., Reference Patel, Pilon, Gupta, Morrison, Lafeuille, Lefebvre and Benson2022). Extensive research has examined readmissions, identifying several risk and protective factors, albeit with occasionally conflicting evidence (Donisi, Tedeschi, Wahlbeck, Haaramo, & Amaddeo, Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016; Edgcomb, Sorter, Lorberg, & Zima, Reference Edgcomb, Sorter, Lorberg and Zima2020; Owusu, Oluwasina, Nkire, Lawal, & Agyapong, Reference Owusu, Oluwasina, Nkire, Lawal and Agyapong2022; Sfetcu et al., Reference Sfetcu, Musat, Haaramo, Ciutan, Scintee, Vladescu and Katschnig2017). For example, the number of prior hospitalizations consistently predicts subsequent ones, the influence of factors like the length of hospital stay has varied (Donisi et al., Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016).
Particularly, studies covering various periods of follow-up and readmission intervals have reported inconsistent results concerning the relationship between timely outpatient follow-up and readmissions (Beadles et al., Reference Beadles, Ellis, Lichstein, Farley, Jackson, Morrissey and Domino2015; Edgcomb et al., Reference Edgcomb, Sorter, Lorberg and Zima2020; Hermer, Nephew, & Southwell, Reference Hermer, Nephew and Southwell2022; Katschnig, Straßmayr, Endel, Posch, & Steiner, Reference Katschnig, Straßmayr, Endel, Posch and Steinern.d.; Kurdyak et al., Reference Kurdyak, Vigod, Newman, Giannakeas, Mulsant and Stukel2018; Lee et al., Reference Lee, Kim, Kim, Kim, Kim, Han and Paik2015; Marcus, Chuang, Ng-Mak, & Olfson, Reference Marcus, Chuang, Ng-Mak and Olfson2017; Sfetcu et al., Reference Sfetcu, Musat, Haaramo, Ciutan, Scintee, Vladescu and Katschnig2017). Indeed, factors linked to psychiatric readmissions may vary across different time segments following discharge, though there is currently a scarcity of comprehensive evidence in this area (Del Favero, Montemagni, Villari, & Rocca, Reference Del Favero, Montemagni, Villari and Rocca2020; Lee et al., Reference Lee, Kim, Kim, Kim, Kim, Han and Paik2015; Lin et al., Reference Lin, Chen, Lin, Lee, Ko and Li2010). In addition to timing, the type of the service may alter the association of follow-up and readmission. Previous studies have evaluated single or multiple contacts, different mean or content of contacts, primary or secondary care contacts or continuity of care, with mixed results (Sfetcu et al., Reference Sfetcu, Musat, Haaramo, Ciutan, Scintee, Vladescu and Katschnig2017). For example, in a Japanese study, a consultation by a psychiatrist for at least 5 min was defined as follow-up and was beneficial, and in an Australian study, having a discharge plan sent to the patient's GP was beneficial (Callaly, Trauer, Hyland, Coombs, & Berk, Reference Callaly, Trauer, Hyland, Coombs and Berk2011; Okumura, Sugiyama, & Noda, Reference Okumura, Sugiyama and Noda2018).
In Finland, national healthcare registers have comprehensive coverage and relatively good quality with all public services in primary and secondary care and supported housing services maintained by social services (Sund, Reference Sund2012). However, the exact content of a single outpatient contact cannot be determined from the registers and in some regions, mental health services may be integrated administratively to primary care and hence present in the primary care register. In addition, despite universal access to services in theory in Finland, long waiting times are a challenge for the system (Tynkkynen et al., Reference Tynkkynen, Alexandersen, Kaarbøe, Anell, Lehto and Vrangbӕk2018). For the purposes of this study, we focused on the first real-time contact to psychiatric services, supported housing services or primary healthcare as a measure reflecting the first step in continuation of care after discharge from psychiatric inpatient treatment.
We hypothesized that 1. timely outpatient follow-up associates with reduced readmissions and 2. the influence of different factors before and after discharge on the risk of readmission changes over time. By utilizing Finnish healthcare registers, we examined the risk of readmission in individuals diagnosed with a non-affective psychotic disorder (NAP) in a nationwide, representative patient cohort from the Finnish Quality of Psychosis Care Register.
Materials & methods
Data sources and study design
We used data from the Finnish Quality of Psychosis Care Register (FQPCR), which encompasses individuals diagnosed with a NAP. International Statistical Classification of Diseases and Related Health Problems (ICD-10) codes F20-F29 (schizophrenia, schizotypal and delusional disorders) or International Classification of Primary Care (ICPC-2) codes P72 (schizophrenia) or P98 (psychosis NOS) were included, and individuals were required to have any of these diagnoses at least once during the period 2010 to 2020. Excluded from both the FQPCR and our study were individuals not residing in Finland, those under the age of seven, or those diagnosed with dementia prior to their initial psychosis diagnosis. The data for this study were drawn from the Care Register for Health Care, the Register of Primary Health Care visits, and the Register of Social Services, with population statistics from Statistics Finland linked to the data at an individual level.
We conducted a register-based cohort study including all individuals within the FQPCR who had been discharged from a psychiatric hospital (regardless of their current discharge diagnosis) between 1 January 2017 and 31 December 2021. Participants were followed from their first discharge during the study period until readmission, death, up to 365 days, or the end of the study period, which ever came first. Each individual's cohort entry was determined by the first discharge event. Discharges from forensic psychiatric hospitals were excluded.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The quality registry project received permission to use the registry data from the Finnish Institute for Health and Welfare. Because the data is based on national registers only, a separate ethical review or informed consent is not required in Finland.
Response variable
The primary focus of investigation was the determination of whether patients were readmitted to a psychiatric hospital within a window of 1 to 365 days following their discharge from the index hospitalization.
Explanatory variables
The key explanatory variable was the time to the first outpatient follow-up contact after the index discharge during the follow-up period. Medical contacts with psychiatric outpatient clinics or primary care health centers, as well as with mental health housing units maintained by social services, were included. Both in-person and virtual real-time contacts were included.
Covariables were categorized as follows: Registered sex (man or woman), age group (7–12, 13–17, 18–29, 30–44, 45–64, 65–79, 80 years and over), calendar year, hospital district (20 administrative regions), length of stay (LOS) of the index hospitalization (1–3, 4–13, 14–27, 28–83, 84 days and over), and number of previous hospitalizations (0, 1–4, 5–9, 10 and over). Discharge diagnoses of the index hospitalizations were categorized into eight groups: schizophrenia (ICD-10: F20), schizoaffective disorders (F25), delusional disorders (F22 and F24), acute and transient psychotic disorders (F23), schizotypal disorder (F21), other nonorganic psychotic disorders (F28), unspecified nonorganic psychosis (F29), and other diagnoses (if the current hospitalization did not include a diagnosis from the ICD-10 group F20-29). The groups were mutually exclusive in the order presented above. The presence of substance use disorders (SUD, ICD-10: F10-F16, F18-F19) at the index discharge was recorded (present or not). In hospitals, only ICD-10 classification is used.
Data on residential status (living alone, with family or other, i.e. living in residential housing, institutions or homeless) and economic activity (employed, unemployed, under 15 years of age, student, retired, and others outside the labor force) were obtained from registers of Statistics Finland and represent the status on the last day of the year preceding the index discharge.
Analysis
Initially, linearity of the continuous covariables was assessed using penalized splines in Cox regression model and the covariables were categorized based on their associations and a prior knowledge on their nature. For example, according to Finnish law, individuals under 18 years of age must be treated in separate wards – those under 13 years in child and 13–17 years in adolescent psychiatric wards, and LOS of four days is the maximum length of so-called observational period after an involuntary admission. Subsequently, the Chi-square test was employed to assess the differences among groups based on occurrences or readmissions. Using the Kaplan–Meier method, we performed rehospitalization-free survival analysis based on the presence of outpatient follow-up and LOS of the index hospitalization.
To delve into the risk factors associated with readmission, we employed a time-dependent Cox's proportional hazard model. Each subject's follow-up time was split into the period before and after the first outpatient follow-up contact. Proportional hazards assumption was assessed using Schoenfeld residuals and by visual assessment of the Kaplan–Meier curves. Notably, the proportional hazards assumption was found to be unsuitable for the outpatient follow-up variable for the entire follow-up time. Consequently, the one-year follow-up period was divided into distinct intervals: week 1, weeks 2–4, weeks 5–13, weeks 14–25, and weeks 26–52. Subgroup analyses were conducted for each of these periods, yielding hazard ratios (HRs) with corresponding 95% confidence intervals (CIs) for the comparison of not having an outpatient follow-up contact v. attending the first follow-up contact. The following adjustments were included in the analysis: basic adjustments including sex, age group, year, and healthcare district; residential status, number of hospitalizations, diagnosis, presence of SUD, and economic activity. Bayesian information criteria were used for the model selection.
The sensitivity to definitions of the explanatory variable was investigated by alternative definitions in the following additional analyses: Secondary care, primary care and housing services were compared to no such follow-up (but possibly with other types of follow-ups), and the time interval for follow-up was restricted to the first 1, 4, 13, or 26 weeks (with later follow-up visits ignored). Finally, the main analysis was replicated using the Fine–Gray subdistribution hazard model with death as a competing event. Stata 17.1 (StataCorp LLC), and R 3.6.3 (R Project for Statistical Computing) were used for analyses and data management.
Results
Between 2017 and 2021, a total of 29 858 individuals (48.6% women, n = 14 521) were discharged from psychiatric inpatient care, of whom 10 623 (35.6%) were readmitted and 495 (1.7%) died within the study period. Outpatient follow-up occurred within a week in 16 155 individuals (54.1%) and within four weeks in 22 817 (76.4%), while 4 563 individuals (15.3%) had no outpatient contact within the year following the index discharge. Descriptive statistics are presented in Table 1. The median age at discharge was 40 (interquartile range [IQR]: 28–58) years, while the median LOS of the index hospitalization was 19 (IQR: 7–45) days. Roughly half of the population lived alone (50.9%, n = 15 185), and nearly half were retired (49.8%, n = 14 863). NAP (ICD-10: F20–F29) discharge diagnosis was not present in 5 553 (18.6%) individuals, although these individuals had received such a diagnosis earlier. Of those without present diagnosis of non-affective psychosis, diagnoses of mood disorder (F30–F39) were present in 3020 (10.1% of the whole sample), SUD (F10–F19) in 1603 (5.4%), anxiety disorders (F40–F48) in 1209 (4.1%), personality disorders (F60–F69) in 823 (2.8%), organic mental disorders (F00–F09) in 394 (1.3%), disorders with onset usually occurring in childhood and adolescence (F90–F98) in 309 (1.0%) and other diagnoses in less than 1% of cases. Diagnosis of mania or bipolar disorder (F30–F31) was present in 1352 (4.5%), and depression with psychotic features (F32.3 or F33.3) in 499 (1.7%) patients.
Table 1. Description of study and sample characteristics
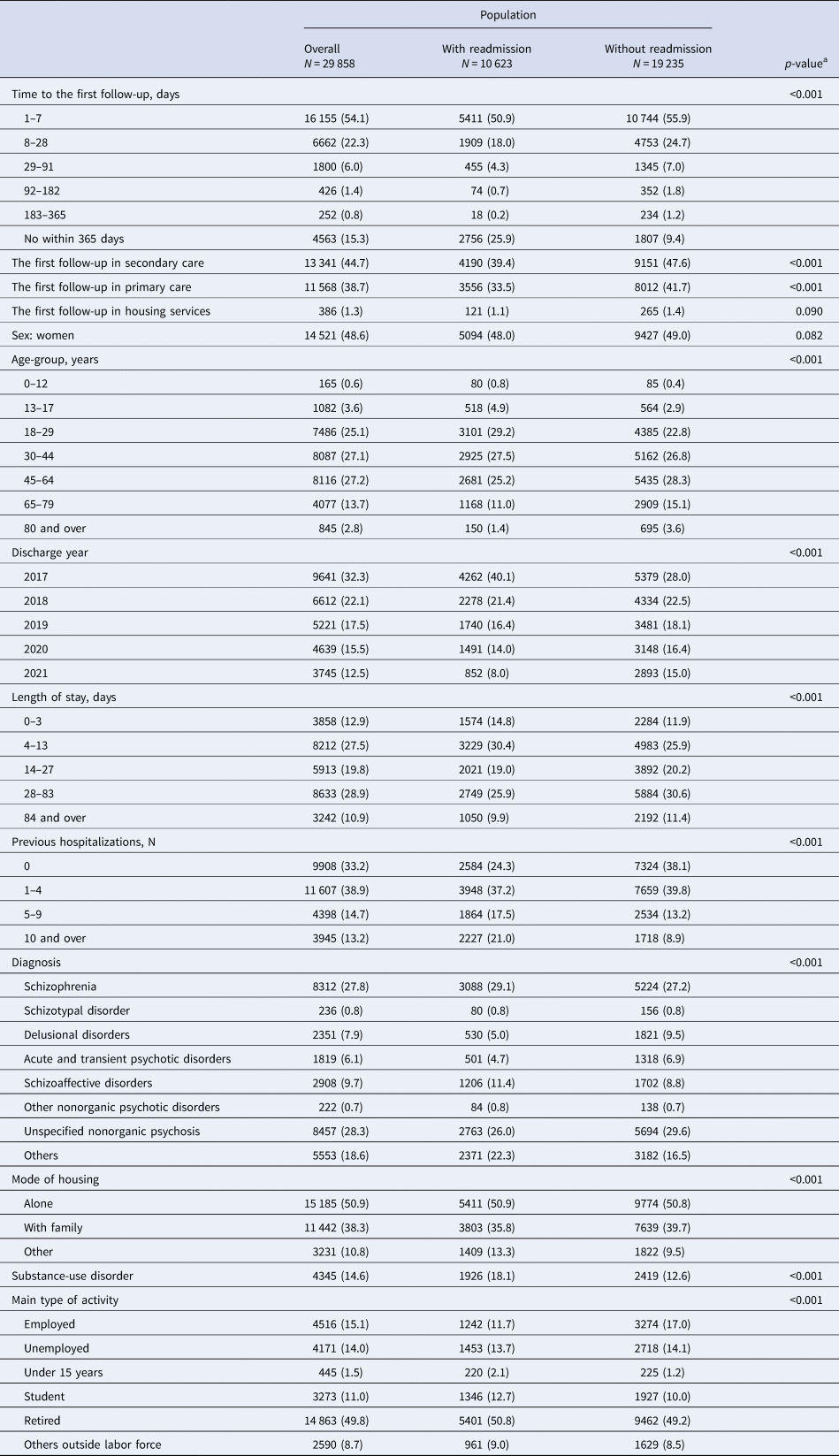
a Chi-square test to assess the differences among those with and without readmissions.
Association of outpatient follow-up and readmission
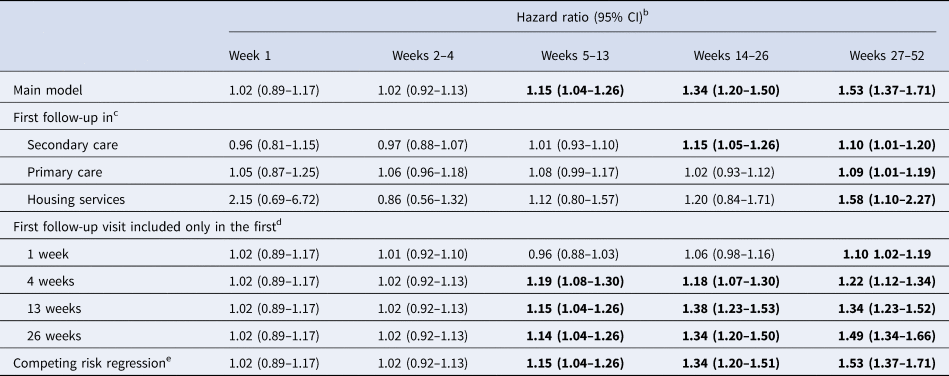
Kaplan–Meier analysis is shown in Fig. 1. In the first two follow-up intervals including the first four weeks after the index discharge, the presence of outpatient follow-up visit did not exhibit a statistically significant association with readmissions. However, during the subsequent periods of 5–13, 14–25, and 26–52 weeks after the index discharge, the absence of outpatient follow-up visits was associated with increased hazard of readmission. The HR ranged from 1.24 (95% CI 1.13–1.36) in weeks 5–13 to 1.58 (1.42–1.76) after basic adjustments and from 1.15 (1.04–1.26) to 1.53 (1.37–1.71) after all additional adjustments (Table 2).
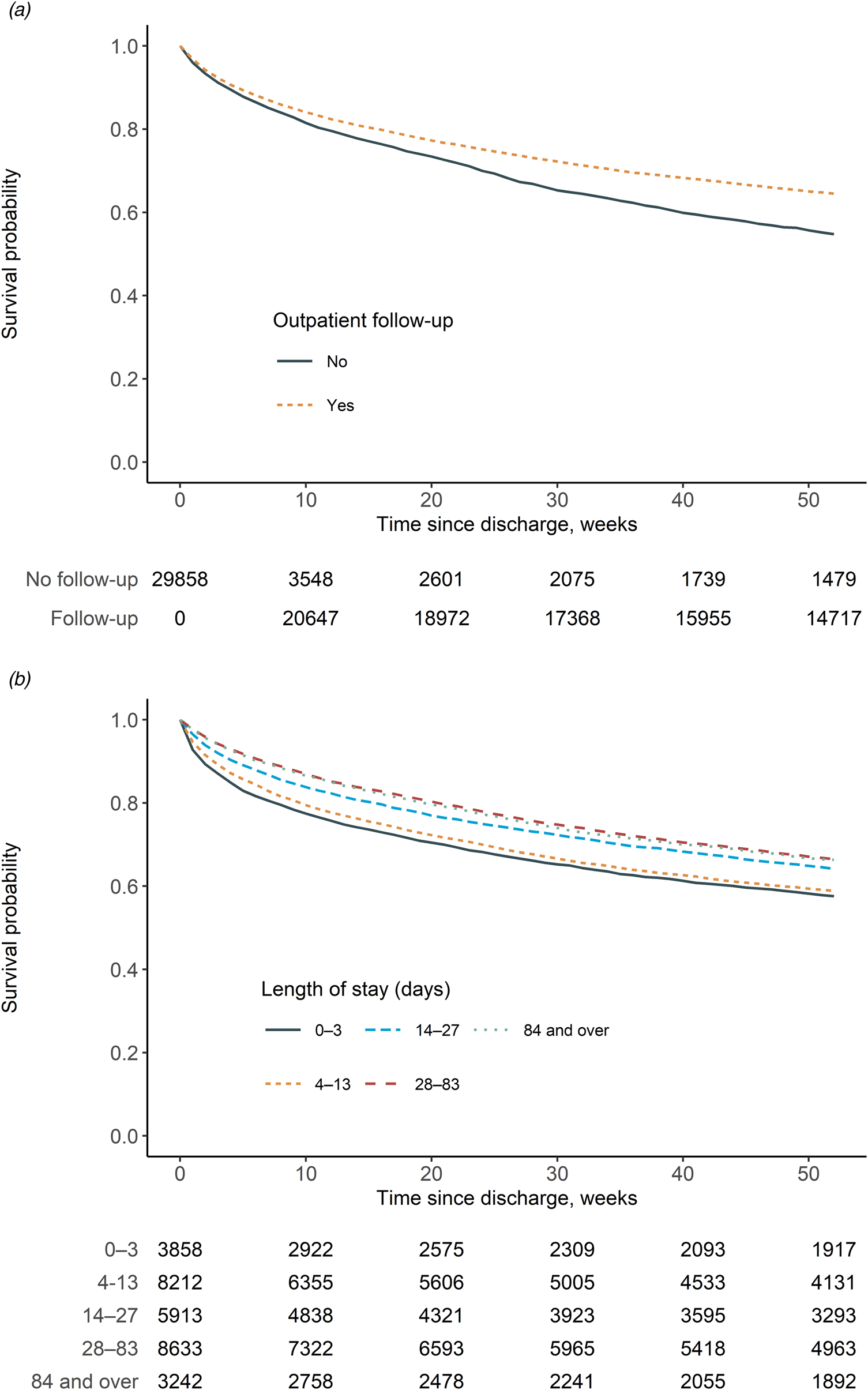
Figure 1. Kaplan–Meier curves for readmission. (a) For follow-up in outpatient care. (b) For length of preceding hospital stay.
Table 2. The unadjusted and adjusted risk of psychiatric readmission at different time intervals after discharge, among those without compared to those with follow-up in outpatient care after discharge
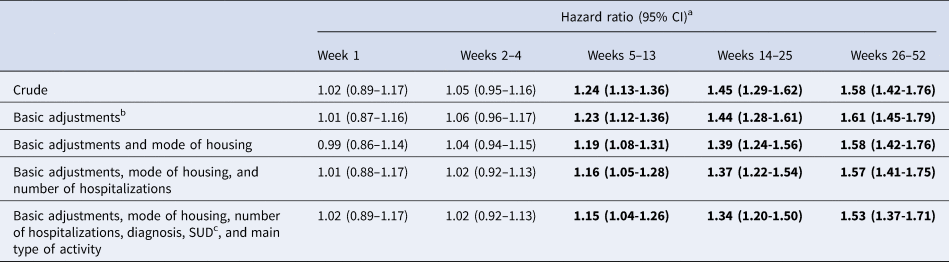
a Estimates with p < 0.05 are shown in bold.
b Basic adjustments included sex, age group, year, and healthcare district.
c SUD: substance use disorder.
Associations of other variables and readmission
Associations between other variables and readmission were observed. Notably, few variables exhibited consistent associations with readmission across all sub-periods; see Table 3. In models encompassing all additional adjustments, the number of previous hospitalizations consistently yielded heightened HRs and older age decreased HRs, while a diagnosis of delusional disorder was correlated with decreased HRs until 26 weeks. Other than delusional disorders, diagnostic categories had minimal impact across the sub-periods.
Table 3. The adjusted risk of psychiatric readmission at different time intervals after discharge by covariablesa
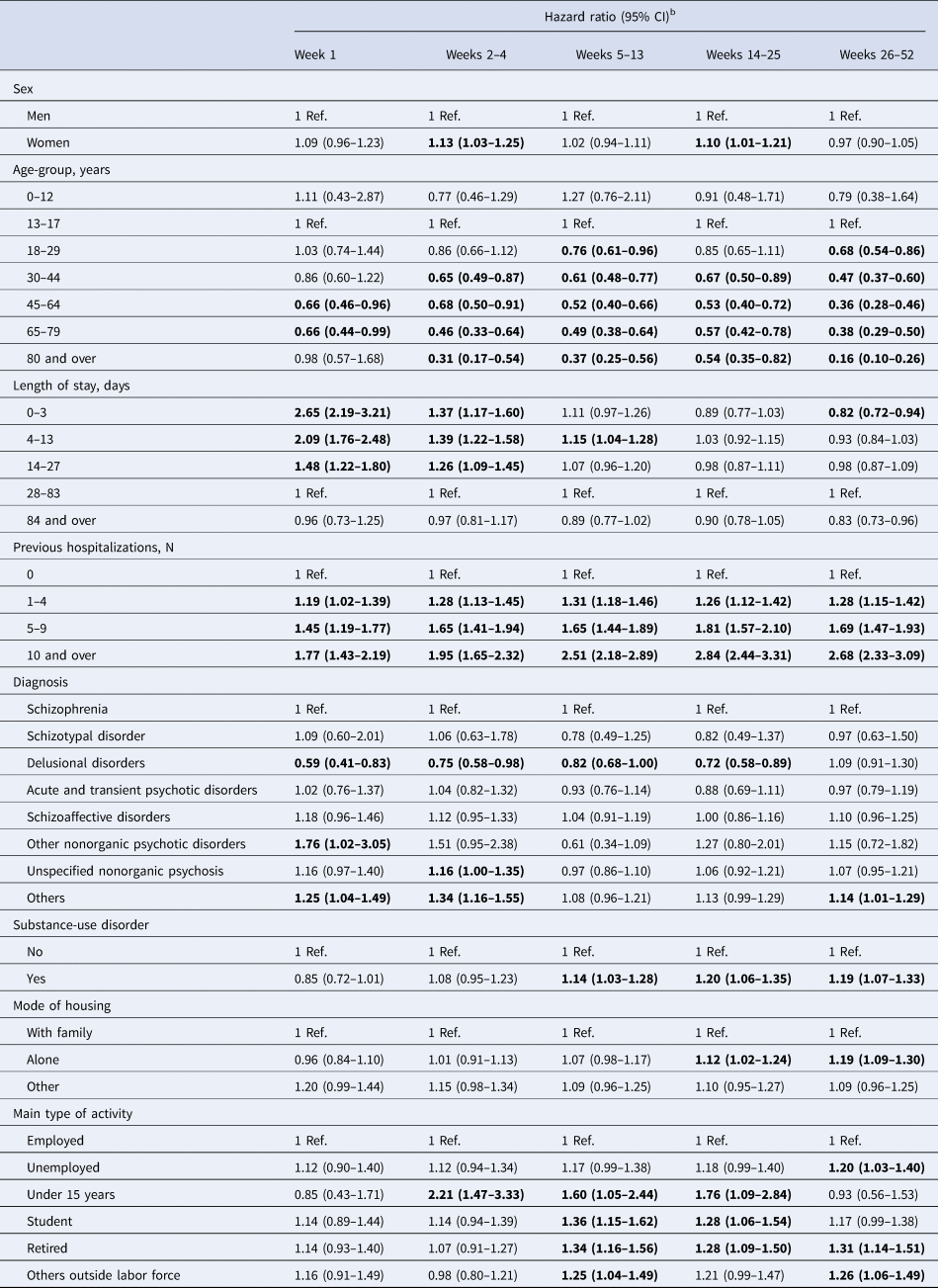
a The model included all covariables: sex, age group, year, healthcare district, outpatient follow-up, residential status, number of hospitalizations, diagnosis, substance use disorders, and economic activity.
b Estimates with p < 0.05 are shown in bold.
Furthermore, the relationships of several variables with the hazard of readmission varied over time. In the initial four weeks following the index discharge, LOS shorter than 28 days was associated with an increased likelihood of readmissions. However, after the first four weeks following the index discharge, this correlation with short LOS diminished. From the fifth week onwards after the index discharge, having a SUD, and from the 13th week onwards, not living with family, exhibited associations with increased readmissions. Main type of activity did not show constant associations with readmissions (Table 3).
Additional analysis
When follow-up only in secondary care, primary care, or housing services were considered, the association between first follow-up and readmission reduced suggesting that the association is not specific for certain types of follow-ups (Table 4). When the period of the first follow-up was restricted to the first 1, 4, 13, or 26 weeks after discharge, the observed HRs changed only a little. This suggests that the follow-up in outpatient care is associated with reduced readmissions, even if the first contact is later than in the first one or four weeks. Competing risk regression model did not alter the main findings compared to traditional Cox regression (Table 4).
Table 4. The adjusteda risk of psychiatric readmission at different time intervals after discharge, among those without compared to those with follow-up in outpatient care after discharge by different definitions for the explanatory variable and with competing risk regression model
a The models included all covariables: sex, age group, year, healthcare district, outpatient follow-up, residential status, number of hospitalizations, diagnosis, substance use disorders, and economic activity.
b Estimates with p < 0.05 are shown in bold.
c Only certain type of follow-up considered. For example, in the case of secondary care, those without secondary care follow-up (but possibly with primary or housing services) compared to those with secondary care follow-up.
d The interval from discharge to the first follow-up visit restricted to specific values. Later follow-up visits ignored.
e The Fine–Gray subdistribution hazard model with death as a competing event. The estimates provided are subhazard ratios and 95% CIs.
Discussion
In this population-based register study encompassing a nationally representative cohort of individuals with psychotic disorders, risk factors of readmission varied substantially over the first year after the index discharge. Lack of outpatient follow-up visits was associated with increased risk of readmission only after the first month following the index discharge. Shortly after discharge, only the number of previous hospitalizations and short hospital stays increased the risk of readmission. In addition, comorbid SUDs and social factors like living with family or being employed at the time of index admission associated with readmissions only later after the discharge. With time-varying analysis, this study provides new insight into the risk of readmission, and provides more detailed information on the importance of outpatient follow-up after discharge for clinical work and for interpretation on quality indicators of mental health services.
The current findings reveal a dynamic pattern in the risk factors associated with readmission among individuals with psychotic disorders. Specifically, our analysis demonstrates that a short LOS is linked to early readmissions, while the influence of a lack of outpatient follow-up is observable primarily after the initial month following discharge. This observed trajectory aligns with the premise that post-discharge symptom management is often tied to readmissions, and it is plausible that achieving symptom control in psychotic disorders may not be feasible during very brief hospital stays (Sfetcu et al., Reference Sfetcu, Musat, Haaramo, Ciutan, Scintee, Vladescu and Katschnig2017).
The present study contributes to previously limited literature on predictors of readmission at varying post-discharge time intervals. A study conducted in South Korea found that two or more outpatient visits within the first 60 days post-discharge in patients with schizophrenia reduced the risk of readmission in subsequent periods lasting 90 days or more. However, this study did not delve into early readmissions (Lee et al., Reference Lee, Kim, Kim, Kim, Kim, Han and Paik2015). Regarding LOS, a Taiwanese study demonstrated a risk reduction in readmissions within 14 days for LOS durations of 5–7 days, but not beyond this time frame in patients hospitalized with any mental disorder (Lin et al., Reference Lin, Chen, Lin, Lee, Ko and Li2010). Conversely, an Italian study reported an association between LOS and readmission after a six-month interval, but not within 30 days in patients hospitalized with any mental disorder (Del Favero et al., Reference Del Favero, Montemagni, Villari and Rocca2020). However, these two studies, which examined multiple time intervals, did not explore the role of post-discharge continuity of care as a contributing factor.
The findings of the present study contribute substantial evidence to affirming the advantages of outpatient follow-up in diminishing readmissions when the period is taken into account. Outpatient follow-up within 30 days has demonstrated a correlation with reduced readmissions in numerous, though not all, prior investigations (Sfetcu et al., Reference Sfetcu, Musat, Haaramo, Ciutan, Scintee, Vladescu and Katschnig2017). For instance, a recent study in the United States found that patients with schizophrenia who received outpatient follow-up within 30 days of discharge exhibited no significant decrease in the likelihood of readmission compared to those who did not receive such care (Hermer et al., Reference Hermer, Nephew and Southwell2022). Notably, this study observed that only 10% of patients received outpatient follow-up within the 30-day period. Another study conducted in the US identified a marginal association between follow-up and readmissions (Beadles et al., Reference Beadles, Ellis, Lichstein, Farley, Jackson, Morrissey and Domino2015). The authors argued that establishing a universal seven-day threshold for the first outpatient follow-up might lack significance for all adults with diverse psychiatric conditions. In contrast to the estimates from the US, for example, in the current study, more than half of the patients received outpatient follow-up within a week, highlighting differences in healthcare system as another source of variation in the risk factors regarding readmissions.
The implications of LOS on the risk of readmission have also yielded inconclusive results in prior studies; these have reported that higher LOS either increases or decreases the risk of readmission (Donisi et al., Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016; Katschnig et al., Reference Katschnig, Straßmayr, Endel, Posch and Steinern.d.). At the same time, the psychiatric bed numbers continue decreasing and LOS shortening (Mundt, Delhey Langerfeldt, Rozas Serri, Siebenförcher, & Priebe, Reference Mundt, Delhey Langerfeldt, Rozas Serri, Siebenförcher and Priebe2021). Many recent investigations exploring outpatient follow-up have incorporated LOS as a covariable. For instance, in South Korea, LOS had no independent effect (Lee et al., Reference Lee, Kim, Kim, Kim, Kim, Han and Paik2015), while in the USA, the impact of LOS varied across state hospitals and other institutions, possibly modifying the relationship between outpatient follow-up and readmission (Hermer et al., Reference Hermer, Nephew and Southwell2022). A cross-country comparison within certain European countries revealed that LOS correlated with reduced psychiatric readmissions, wherein longer stays were associated with decreased risk in Finland and Norway, but conversely linked to increased risk in Romania (Katschnig et al., Reference Katschnig, Straßmayr, Endel, Berger, Zauner, Kalseth and Šprah2019). Taken together, the body of evidence suggests that in Finland, short LOS is associated with psychiatric readmission.
The present findings align with prior research regarding many of the variables under study. For instance, the consistent association between the number of previous hospitalizations and readmission risk is in line with previous literature (Donisi et al., Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016). Similarly, the observations that older age, being married, or being employed is linked to a reduced risk of readmission mirrors findings from earlier investigations (Donisi et al., Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016). Furthermore, consistent with earlier research, the impact of diagnosis was found to be small, although those with delusional disorders had a reduced risk and those with SUDs had an elevated risk of readmission (Donisi et al., Reference Donisi, Tedeschi, Wahlbeck, Haaramo and Amaddeo2016). The current results indicate that the effects of these variables become evident primarily after the initial month following the index discharge, thereby suggesting that LOS and probably other clinical characteristics have an important role in shaping the risk of early readmission.
The variability of observed risk profiles in the readmission risks across studies suggest that contextual factors in the healthcare systems and psychiatric services may contribute substantially to the risk factors of readmissions. In Finland, readmission rates have demonstrated a rather average trend in European comparison (Katschnig et al., Reference Katschnig, Straßmayr, Endel, Berger, Zauner, Kalseth and Šprah2019). Subsequently, there has been an overall reduction in LOS, with 47% of all psychiatric hospitalizations lasting less than one week in 2021 (Kyrölä, Järvelin, & THL, Reference Kyrölä and Järvelin2022). Corresponding to global trends, the number of psychiatric beds has continued to decline in Finland in recent years, resulting in a count of 48 beds per 100 000 population by 2021 (Linnaranta, Reference Linnaranta2022). This evolution has spurred a spectrum of arguments both for and against such developments (Mundt et al., Reference Mundt, Delhey Langerfeldt, Rozas Serri, Siebenförcher and Priebe2021). For instance, a Danish study contended that the diminished number of hospital beds leading to high bed occupancy rates may have compromised the quality and duration of acute inpatient care (Jeppesen, Christensen, & Vestergaard, Reference Jeppesen, Christensen and Vestergaard2016). Notably, in Finland, the increased emphasis on outpatient care has not resulted in subsequent reduction in the rates of first psychiatric hospital admissions, raising questions about the overall performance of the psychiatric health care system (Suokas et al., Reference Suokas, Koivisto, Hakulinen, Kaltiala, Sund, Lumme and Pirkola2020).
Follow-up after discharge and continuity of care frequently emerge as significant indicators of the quality of psychiatric services. However, timely follow-up protocol may have beneficial outcomes other than reduced readmission, such as a reduction of symptoms and prevention of post-discharge suicides (Madsen, Egilsdottir, Damgaard, Erlangsen, & Nordentoft, Reference Madsen, Egilsdottir, Damgaard, Erlangsen and Nordentoft2021). In addition, it is possible that timely follow-ups may potentially result in an elevated number of readmissions, especially if LOS is brought down to a minimum or patients are discharged prematurely. Furthermore, established frameworks such as the Institute of Medicine's conceptualization of quality of care encompass six dimensions: safety, timeliness, effectiveness, efficiency, equity, and patient-centeredness (Institute of Medicine (US) Committee on Quality of Health Care in America, 2001). Within this framework, it becomes apparent that appropriate follow-up after discharge has value of its own regarding the spectrum of quality of care attributes.
Limitations
The present study has some limitations. It is important to note that nationwide register data lack information on important clinical factors that could mediate the association between continuity of care and readmissions. For example, poor insight is associated with outpatient treatment disengagement (Myers, Bhatty, Broussard, & Compton, Reference Myers, Bhatty, Broussard and Compton2017) and may lead to medication nonadherence, which in turn predict rehospitalizations (van Dee, Schnack, & Cahn, Reference van Dee, Schnack and Cahn2023). More severe symptoms at discharge, associated with rehospitalization in previous studies (Schennach et al., Reference Schennach, Obermeier, Meyer, Jäger, Schmauss, Laux and Riedel2012), may explain the association between short LOS and increased risk of rehospitalization. Nevertheless, our results point out to actionable targets to reduce readmissions: avoiding premature discharge, promoting continuity of care and improving treatment of patients with a dual diagnosis.
In addition, there was no data pertaining to the nature of readmissions, such as whether they were planned or unplanned. Furthermore, the scope of follow-up was defined in broad terms as any contact with healthcare services, without specific information on the nature or content of these interactions. The original motivation for booking any medical appointments cannot be determined from the administrative registers in detail. Here we consider that the first real-time follow-up contact in psychiatric services, primary care of housing services serves as a proxy for continuation of care. In any case, however, follow-up contacts offer means for healthcare personnel to evaluate the patient's clinical situation and react accordingly. Furthermore, the actual content or intensity of the psychiatric outpatient care at and after the first contact is outside the scope of this study and would be better accounted with data sources other than administrative register alone.
The evaluation was based on a single discharge per individual, thus excluding the assessment of multiple events or the so-called revolving door phenomenon, which could potentially impact the interpretation of the findings. In addition, no data was available on severity of illness or attitudes towards treatment.
Conclusions
The quality of psychiatric hospital care remains a continuous concern. This study underscores the potential benefits of outpatient follow-up after discharge for individuals with psychotic disorders, although these advantages only become evident after a certain period. On the other hand, the link between a short hospital stay and the need for another hospital admission after a short period seems strong, at least in the Finnish context, suggesting the role of the adequacy of hospital care in the risk of readmission. This finding emphasizes the significance of evaluating quality indicators holistically, taking into account the intricate complexities and contextual factors that shape mental health services.
Data availability statement
The data that support the findings of this study are available from the Finnish Institute for Health and Welfare. Restrictions apply to the availability of these data, which were used under license for this study. Data can be requested from the Finnish Social and Health Data Permit Authority Findata.
Funding statement
The study was funded by a grant from the Academy of Finland (#310295, MH) and the Finnish Cultural Foundation (MH).
Competing interests
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The quality registry project received permission to use the registry data from the Finnish Institute for Health and Welfare. Because the data is based on national registers only, a separate ethical review or informed consent is not required in Finland.








