Brief psychotic disorder (BPD) and acute and transient psychotic disorder (ATPD) are two related but different concepts used to define psychotic disorders with acute onset and early remission by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) and the International Classification of Diseases, tenth edition (ICD-10), correspondingly (Gaebel & Reed, Reference Gaebel and Reed2012). ATPD is a broad category which integrated various concepts including bouffée délirante (Pichot, Reference Pichot1986), cycloid psychosis (Perris, Reference Perris, Marneros and Tsuang1986) and the reactive and schizophreniform psychoses (Stromgren, Reference Stromgren, Marneros and Tsuang1986), while BPD is a diagnosis with duration of symptoms of 1 month or less and eventual full return to pre-morbid functioning. Studies in ATPD suggest that patients with ATPD are a higher proportion of females, more likely to have stressful life events before onset of illness and full recovery (Pillmann, et al. Reference Pillmann, Wustmann and Marneros2012; Rusaka & Rancāns, Reference Rusaka and Rancāns2014; Castagnini et al. Reference Castagnini, Munk-Jørgensen and Bertelsen2016). Research in ATPD has grown in recent years, but many of the studies were retrospective in nature and of in-patient records, and there have been only a few studies in BPD (Pillmann et al. Reference Pillmann, Haring, Balzuweit, Blöink and Marneros2002a , Reference Pillmann, Haring, Balzuweit and Marneros b ). There was only moderate concordance between BPD and the polymorphic subtype (F23.0) of ATPD, while the schizophrenia-like subtype (F23.2) of ATPD was in concordance with schizophreniform disorder (Pillmann et al. Reference Pillmann, Haring, Balzuweit, Blöink and Marneros2002 a) and little is known about the cognitive functions and pre-morbid condition in this population. The present study was designed to compare the pre-morbid condition, cognitive function, and demographic and clinical characteristics between patients with BPD and patients with schizophrenia in a prospective study with an out-patient sample.
A total of 42 patients with BPD (16 men and 26 women, mean age 36.02 years) and 157 patients with schizophrenia (75 men and 82 women, mean age 37.61 years) out of 360 patients were consecutively recruited between June 2009 and August 2011 from a population-based territory-wide study of early psychosis in Hong Kong targeting adult-onset first-episode patients [the Jockey Club Early Psychosis (JCEP) Project; Hui et al. Reference Hui, Chang, Chan, Lee, Tam, Lai, Wong, Tang, Li, Leung, McGhee, Sham and Chen2014, Reference Hui, Lau, Leung, Chang, Tang, Wong, Chan, Lee and Chen2015]. Written informed consent was obtained from all patients. The study was approved by the Institutional Review Boards and conducted in accordance with Good Clinical Practice and the Declaration of Helsinki.
Basic demographic information including age, gender, years of education and marital status were recorded. Diagnosis was made according to DSM-IV criteria and reconfirmed at 6 months following the first episode by two experienced psychiatrists based on a best-estimate consensus using all available information, including the validated Chinese version of the Structured Clinical Interview for DSM-IV (So et al. Reference So, Kam, Leung, Chung, Liu and Fong2003), medical records, history from informants, and case workers of the JCEP Project. Age of onset, presence of life events in the prior 6 months, psychiatric hospitalization at entry and family history of mental illness were evaluated.
Pre-morbid functioning during childhood, adolescence and adulthood were evaluated using the Premorbid Adjustment Scale (PAS; Cannon-Spoor et al. Reference Cannon-Spoor, Potkin and Wyatt1982). Pre-morbid schizoid and schizotypal traits were assessed by the assessment of Premorbid Schizoid and Schizotypal Traits (PSST; Foerster et al. Reference Foerster, Lewis, Owen and Murray1991). Positive and negative symptoms were assessed using the Positive and Negative Syndrome Scale (PANSS; Kay et al. Reference Kay, Fiszbein and Opler1987). Cognitive functions were assessed using a comprehensive battery of neurocognitive tests, which included digit span (forward and backward), visual patterns test, logical memory (immediate and delay recall), verbal fluency test and digit symbol substitution test. Functioning level was assessed using the Social Occupational Functioning Assessment Scale (SOFAS; Goldman et al. Reference Goldman, Skodol and Lave1992).
All statistical analyses were performed using IBM SPSS version 23.0 (IBM Corp., USA). Differences in the basic demographic, clinical, functional and neurocognitive characteristics were determined using independent t tests for parametric continuous variables, and χ2 tests for categorical variables. The level of statistical significance for all analyses was set at p < 0.05.
There were 35.7% (n = 15) of patients with BPD and 24.8% (n = 39) of patients with schizophrenia who were married. Family history of mental illness was present in 31.0% (n = 13) of patients with BPD and 29.3% (n = 46) of patients with schizophrenia. A life event was present in 47.6% (n = 20) of patients with BPD and 48.4% (n = 76) of patients with schizophrenia. All of these were not statistically different between the two groups. The other demographic and clinical characteristics are listed in Table 1.
Table 1. Clinical characteristics
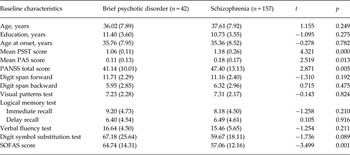
Data are given as mean (standard deviation).
PSST, Premorbid Schizoid and Schizotypal Traits; PAS, Premorbid Adjustment Scale; PANSS, Positive and Negative Syndrome Scale; SOFAS, Social and Occupational Functioning Assessment Scale.
The mean PSST score, mean PAS score and PANSS total score were lower in patients with BPD than patients with schizophrenia. Patients with BPD had a significantly higher SOFAS score and a higher proportion of psychiatric admission than patients with schizophrenia (81.0% v. 55.4%; χ2 = 9.068, p = 0.003).
To the best of our knowledge, this is the first study to examine the cognitive functions and pre-morbid conditions in patients with BPD. We found that patients with BPD are different from patients with schizophrenia prior to onset of illness with fewer schizoid and schizotypal traits and better pre-morbid functioning. This is in consistent with the concept that BPD is a psychotic disorder which has an acute onset in contrast to schizophrenia which has personality predisposition and functional decline in the prodromal period. Patients with BPD also had a higher proportion of psychiatric admission than patients with schizophrenia. This may be explained by the acute change in condition which the carer and health care professionals found difficult to manage in the community. Although patients with BPD had milder severity of psychopathology, and better social and occupational functioning than patients with schizophrenia, a considerable degree of residual symptoms was still observed even after stabilization of the first episode of psychotic illness. Furthermore, we did not find any difference in cognitive functions including attention, memory and executive function between patients with BPD and patients with schizophrenia. The lack of difference may suggest that patients with BPD may not have recovered faster than patients with schizophrenia in terms of cognitive functions after a psychotic episode. Our previous finding in first-episode psychosis patients suggests that there may be a time lag between improvement in cognitive functions and symptoms (Hui et al. Reference Hui, Longenecker, Wong, Tang, Chang, Chan, Lee, Dunn, Miao, Yeung, Wong, Chan, Tang and Chen2012). These findings warrant future studies to examine if patients with BPD can achieve full remission after a psychotic episode, especially for a subgroup of BPD with repeated brief psychotic episodes (Pillmann et al. Reference Pillmann, Haring, Balzuweit and Marneros2002b ). In contrast to some previous findings in ATPD, we found no significant difference in gender ratio, marital status, family history of mental illness and presence of life events between patients with BPD and schizophrenia (Castagnini & Berrios, Reference Castagnini and Berrios2009). This suggests that findings in ATPD may not be applied directly to BPD and more studies in BPD are needed.
Our study suggests that BPD is different from schizophrenia in terms of patients’ pre-morbid conditions, severity of psychopathology and social functioning. Future studies using a longitudinal design examining the change in cognitive functions in comparison with normal controls and its importance in prediction of relapse and diagnostic transition may help to identify a subgroup of patients for more intensive care. Major change in the subtyping of ATPD has been proposed in the coming ICD-11; we hope that more research in BPD can help to understand the characteristics of acute psychotic disorders to facilitate future refinement of the classification system.
Acknowledgements
This work was supported by funding from the Hong Kong Jockey Club Charities Trust (grant number 21009144).
Declaration of Interest
E.Y.H.C. has served on the advisory board for Otsuka; and has received research funding from AstraZeneca, Janssen-Cilag, Pfizer, Eli Lilly, Sanofi-Aventis and Otsuka, and an educational grant from Janssen-Cilag. The other authors declare no conflict of interest in this study.



