Nearly 46 000 Americanmes died by suicide in 2020, making it the 12th leading cause of death in the USA (Centers for Disease Control and Prevention, 2022). In the US Army, the substantial increase in suicidal behavior that began during the Iraq and Afghanistan wars has persisted for more than a decade (Black, Gallaway, Bell, & Ritchie, Reference Black, Gallaway, Bell and Ritchie2011; Gibson, Corrigan, Kateley, Youmans Watkins, & Pecko, Reference Gibson, Corrigan, Kateley, Youmans Watkins and Pecko2017; Pruitt et al., Reference Pruitt, Smolenski, Tucker, Issa, Chodacki, McGraw and Kennedy2018; Tucker, Smolenski, & Kennedy, Reference Tucker, Smolenski and Kennedy2019; Ursano et al., Reference Ursano, Kessler, Heeringa, Cox, Naifeh, Fullerton and Stein2015b). Given the importance of interpersonal difficulties in suicide risk (Chu et al., Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker, Hagan and Joiner2017; Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010), identifying fundamental processes that may have negative consequences for one's present and future interpersonal relationships may aid in identifying and treating those at risk of suicide. Specifically, adult attachment style is associated with both mental disorders and suicidal behavior (Miniati, Callari, & Pini, Reference Miniati, Callari and Pini2017; Palitsky, Mota, Afifi, Downs, & Sareen, Reference Palitsky, Mota, Afifi, Downs and Sareen2013).
Attachment styles were derived from initial work by Bowlby (Reference Bowlby1969) in the context of early childhood and later conceptualized and extended to describe emotional ties in adult relationships (Hazan & Shaver, Reference Hazan and Shaver1987). Secure attachment (valuing both intimate friendships and personal autonomy) is often contrasted with three types of insecure attachment: preoccupied (overly dependent on acceptance by others), fearful (avoiding relationships due to fear of rejection, fear of being hurt, or distrust of others), and dismissing (dismissing the value of relationships and emphasizing self-reliance) (Bartholomew & Horowitz, Reference Bartholomew and Horowitz1991). Consistent with studies of adolescent and clinical samples (Adam, Sheldon-Keller, & West, Reference Adam, Sheldon-Keller and West1996; Lessard & Moretti, Reference Lessard and Moretti1998; Stepp et al., Reference Stepp, Morse, Yaggi, Reynolds, Reed and Pilkonis2008; Wright, Briggs, & Behringer, Reference Wright, Briggs and Behringer2005), a representative survey of US adults found that risk of suicide ideation and suicide attempt (SA) is higher among individuals endorsing insecure attachment styles and lower among those reporting secure attachment (Palitsky et al., Reference Palitsky, Mota, Afifi, Downs and Sareen2013). Similarly, a recent study of new soldiers found that insecure attachment styles were associated with self-reported pre-enlistment SAs (Wang et al., Reference Wang, Naifeh, Herberman Mash, Morganstein, Fullerton, Cozza and Ursano2022).
Here, we use data from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) New Soldier Study (NSS) (Ursano et al., Reference Ursano, Colpe, Heeringa, Kessler, Schoenbaum and Stein2014) to prospectively examine attachment style as a predictor of medically documented SAs among US Army enlisted soldiers during their first 4 years of service. The vast majority of SAs occur among enlisted soldiers, and the first 4 years of service, which is generally equivalent to the first term of enlistment, is the Army career phase with the highest SA risk (Ursano et al., Reference Ursano, Kessler, Stein, Naifeh, Aliaga, Fullerton and Heeringa2015c). Using a representative sample of soldiers surveyed during their first week of Army service and followed over time via their Army and Department of Defense administrative records, we examine the association of attachment style (preoccupied, fearful, dismissing, and secure), assessed at baseline, with future SAs before and after adjusting for socio-demographic, service-related, and mental health diagnosis (MH-Dx) variables. We then examine interactions of attachment style with sex and MH-Dx to determine whether the association of attachment style with SA differs for women and men, or for those with and without a MH-Dx. Approximately one-third of soldiers who attempt suicide do not receive a MH-Dx, and are therefore not identified with mental health problems, before their attempt (Naifeh et al., Reference Naifeh, Ursano, Stein, Herberman Mash, Aliaga, Fullerton and Kessler2022; Ursano et al., Reference Ursano, Kessler, Naifeh, Herberman Mash, Nock, Aliaga and Stein2018).
Method
Sample
The NSS surveyed representative samples of US Army soldiers entering service and beginning Basic Combat Training between April 2011 and November 2012. Soldiers were recruited within 48 h of reporting for duty and, following informed consent, completed a computerized self-administered questionnaire (SAQ) (see online Supplementary material for additional details). Recruitment and consent procedures were approved by Human Subjects Committees of all Army STARRS collaborating organizations. The 21 772 NSS respondents considered here represent all Regular Army enlisted soldiers who completed the SAQ and agreed to administrative data linkage (77.1% response rate). Data were doubly weighted to adjust for differences in survey responses among respondents who did v. did not agree to administrative record linkage and differences in administrative data profiles between the latter subsample and the population of all new soldiers. More details on NSS weighting are reported elsewhere (Kessler et al., Reference Kessler, Heeringa, Colpe, Fullerton, Gebler, Hwang and Ursano2013). Using the survey-linked administrative data, person-month records were created by coding each month of a soldier's career for each administrative variable and allowing values to change over time (Singer & Willett, Reference Singer and Willett2003; Willett & Singer, Reference Willett and Singer1993). Respondents were followed via administrative data throughout their time on active duty during their first 4 years of service (up to 48 months).
Measures
Administrative variables
SA. Medically documented non-fatal SAs were identified using: DoD Suicide Event Report (DoDSER) (Gahm et al., Reference Gahm, Reger, Kinn, Luxton, Skopp and Bush2012) records; and codes from ICD-9-CM (E950–E958; indicating self-inflicted poisoning/injury with suicidal intent) (Centers for Disease Control and Prevention, 2013) and ICD-10-CM (X71–X83, indicating intentional self-harm; and T36–T65 and T71, where the 5th or 6th character indicates intentional self-harm; and T14.91, indicating SA, not otherwise specified) (Centers for Disease Control and Prevention, 2019; Hedegaard et al., Reference Hedegaard, Schoenbaum, Claassen, Crosby, Holland and Proescholdbell2018) in data systems capturing healthcare encounter information from military and civilian treatment facilities, combat operations, and aeromedical evacuations (online Supplementary eTable 1).
Socio-demographic, service-related, and MH-Dx variables. Administrative personnel records (online Supplementary eTable 1) were used to identify socio-demographic (sex, current age, race, education, marital status) and service-related [rank, deployment status (never deployed, currently deployed, previously deployed)] characteristics. Administrative medical records were used to create an indicator variable for MH-Dx received during Army service based on ICD-9-CM and ICD-10-CM mental health diagnostic codes and mental health-related V-codes and Z-codes (e.g. stressors/adversities, marital problems), excluding postconcussion syndrome and tobacco use disorder (online Supplementary eTable 2). Person-months were coded such that when a MH-Dx was recorded in an individual's records, that month and all subsequent months were coded as positive for MH-Dx.
Self-reported baseline survey variables
Attachment style. Attachment style was assessed with four items adapted from the Relationship Questionnaire (RQ) (Bartholomew & Horowitz, Reference Bartholomew and Horowitz1991). Respondents used a five-point Likert scale (‘not at all like me,’ ‘a little like me,’ ‘somewhat like me,’ ‘a lot like me,’ and ‘exactly like me’) to rate each of the following attachment styles: preoccupied (‘People I care about sometimes don't want to be as close to me as I want. I worry they might leave me. This sometimes makes me too clingy.’); fearful (‘I want to have relationships, but have a hard time letting people get close. I worry I will be hurt if I let people get too close.’); dismissing (‘It is very important to me to feel independent. I don't need close relationships. I prefer not to depend on other people.’); and secure (‘I am pretty comfortable with emotional closeness, but I am also fine being alone. I don't worry much about being accepted or rejected.’). The four-item RQ has acceptable reliability and validity (Bartholomew & Shaver, Reference Bartholomew, Shaver, Simpson and Rholes1998; Scharfe & Bartholomew, Reference Scharfe and Bartholomew1994). Item-level missingness (3.7–4.4%) was imputed using the sample-wide median. The four items were dichotomized, with responses of ‘a lot like me’ or ‘exactly like me’ considered positive endorsement of a given attachment style.
Analysis methods
Analyses were conducted using SAS version 9.4 (SAS Institute Inc., 2013). Person-month data were analyzed using discrete-time survival analysis with a logistic link function (Singer & Willett, Reference Singer and Willett2003; Willett & Singer, Reference Willett and Singer1993). A series of logistic regression analyses separately examined the association of each attachment style with first documented SA during the first 4 years of Army service, before and after adjusting for socio-demographic variables, service-related variables, and MH-Dx. All four attachment styles were then examined simultaneously in a model adjusting for all other covariates. Two-way interactions of each attachment style with sex and MH-Dx were examined separately in a model adjusting for the main effects of the other three attachment styles and the other covariates. Significant interactions were explored by stratifying the sample and examining attachment style as a multivariable predictor within each stratum. All models accounted for changes in SA risk across time in service using splines (piecewise linear functions) identified in previous analyses (Naifeh et al., Reference Naifeh, Ursano, Stein, Herberman Mash, Aliaga, Fullerton and Kessler2022).
Logistic regression coefficients and confidence limits were exponentiated to obtain estimated odds ratios (OR) and 95% confidence intervals (95% CI). Standard errors were estimated using the Taylor series method (Wolter, Reference Wolter1985) to adjust for the weighting and clustering of NSS data. Multivariable significance tests in the logistic regression analyses were made using Wald χ2 tests based on coefficient variance–covariance matrices adjusted for design effects using the Taylor series method. Statistical significance was evaluated using two-sided design-based tests and the .05 level of significance.
In order to examine patterns of SA risk as a function of attachment style and time in service, we used discrete-time survival models to estimate risk (suicide attempters per 100 000 person-months) during each month of service for soldiers endorsing each attachment style.
Results
Sample characteristics
In the total cohort, weighted person-months were mostly male (87.6%), White non-Hispanic (60.9%), had at least a high school education (91.0%), not married (61.8%), at least 21-years-old (72.9%), E4 or higher rank (50.2%), and never deployed (74.0%). Person-months in which a SA occurred (n = 253) were mostly male (75.4%), White non-Hispanic (59.9%), at least high school-educated (84.4%), not married (60.8%), age 21 or older (61.6%), E3 or lower rank (71.0%), and never deployed (74.5%) (Table 1).
Table 1. Distribution of sample characteristics among a cohort of Regular Army enlisted soldiers over their first four years of servicea

a The survey respondents considered here were Regular Army enlisted soldiers (n = 21 772). Survey-linked administrative person-month records were examined through 48 months of service. The number of available person-month records for a given soldier varied because of attrition from service.
b <High school includes General Educational Development credential (GED), home study diploma, occupational program certificate, correspondence school diploma, high school certificate of attendance, adult education diploma, and other non-traditional high school credentials.
Of the 21 772 unique soldiers at baseline, the estimated prevalence of preoccupied, fearful, dismissing, and secure attachment was 9.1, 15.7, 19.2, and 46.8%, respectively. The proportion of subsequent person-months associated with each attachment style was as follows: preoccupied (8.2%), fearful (14.9%), dismissing (19.1%), and secure (47.5%). Bivariate correlations among the dichotomized attachment variables ranged from r = −0.13 (p < 0.0001) for dismissing–secure to r = 0.31 (p < 0.0001) for preoccupied–fearful (for additional correlation results, see online Supplementary eTables 3 and 4).
Association of attachment style with future SA
Examined separately in models adjusting only for time in service, all three insecure attachment styles were associated with increased odds of future SA, ranging from preoccupied [OR 2.5 (95% CI 1.7–3.4)] to fearful [OR 1.6 (95% CI 1.1–2.3)], whereas secure attachment was not associated with SA. Associations persisted after adjusting for socio-demographic and service-related variables. When MH-Dx was included, preoccupied and dismissing remained significant (Table 2).
Table 2. Separate associations of attachment style with documented suicide attempts among a cohort of Regular Army enlisted soldiers over their first 4 years of servicea
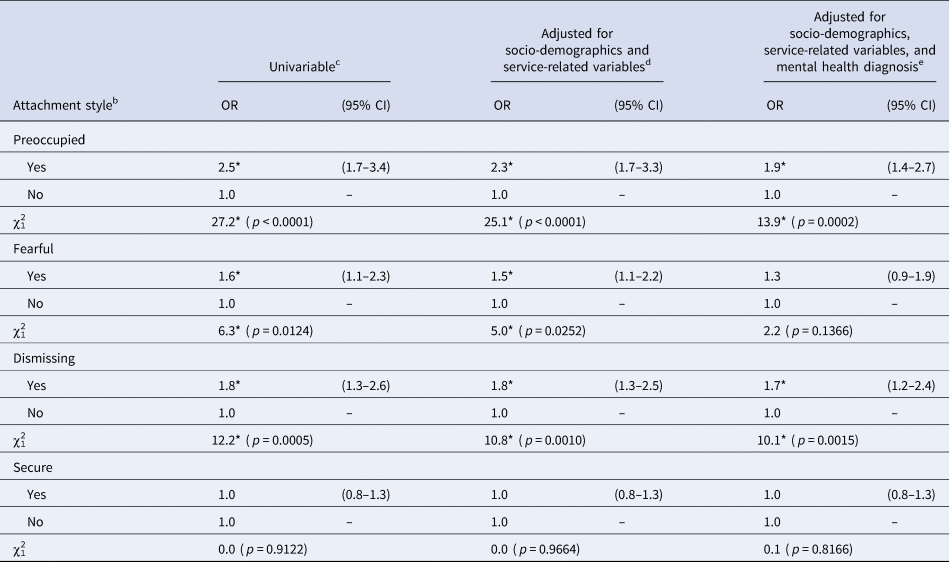
a The survey respondents considered here were Regular Army enlisted soldiers (n = 21 772). Survey-linked administrative person-month records were examined through 48 months of service. The number of available person-month records for a given soldier varied because of attrition from service.
b Each attachment style was examined in separate models.
c Adjusted only for time in service (spline variables).
d Adjusted for time in service (spline variables), socio-demographic variables (sex, race/ethnicity, education, marital status), and service-related variables (rank, deployment status).
e Adjusted for time in service (spline variables), socio-demographic variables (sex, race/ethnicity, education, marital status), service-related variables (rank, deployment status), and administratively documented mental health diagnosis.
*p < .05.
When all attachment styles were examined simultaneously in a model, preoccupied [OR 2.2 (95% CI 1.5–3.2)] and dismissing [OR 1.7 (95% CI 1.2–2.5)] were associated with future SA, whereas fearful and secure attachment were not. Associations persisted after adjusting for socio-demographic variables, service-related variables, and MH-Dx (Table 3).
Table 3. Simultaneous associations of attachment style with documented suicide attempts among a cohort of Regular Army enlisted soldiers over their first four years of servicea

a The survey respondents considered here were Regular Army enlisted soldiers (n = 21 772). Survey-linked administrative person-month records were examined through 48 months of service. The number of available person-month records for a given soldier varied because of attrition from service.
b All four attachment styles were included in each model.
c Adjusted only for time in service (spline variables).
d Adjusted for time in service (spline variables), socio-demographic variables (sex, race/ethnicity, education, marital status), and service-related variables (rank, deployment status).
e Adjusted for time in service (spline variables), socio-demographic variables (sex, race/ethnicity, education, marital status), service-related variables (rank, deployment status), and administratively documented mental health diagnosis.
*p < .05.
Two-way interactions between each attachment style and sex were all non-significant. The two-way interaction between dismissing attachment style and MH-Dx was significant (χ21 = 4.5, p = 0.0347), and the preoccupied attachment × MH-Dx interaction trended toward significance (χ21 = 3.5, p = 0.0621). Other attachment style × MH-Dx interactions were non-significant. After stratifying the sample by MH-Dx, dismissing attachment style was significantly associated with future SA among soldiers without MH-Dx [OR 2.5 (95% CI 1.3–4.6)], but not among those with MH-Dx [OR 1.4 (95% CI 0.9–2.0)]. Similarly, preoccupied attachment was significant among those without [OR 3.2 (95% CI 1.6–6.5)], but not with [OR = 1.4 (95% CI 0.8–2.3)] MH-Dx.
Population-attributable risk proportions
Using the total sample and the full multivariable model (all four attachment styles and covariates), we calculated multivariable population-attributable risk proportions (PARPs) for preoccupied attachment (6.4%) and dismissing attachment (11.5%), the two styles that remained significant.
SA risk as a function of attachment style and time in service
Using discrete-time survival models, we estimated SA risk in each month since entering service for soldiers endorsing any of the three insecure attachment styles v. soldiers endorsing none (Fig. 1). Due to the limited number of monthly SA cases, risk estimates were averaged over 6-month intervals. Risk was consistently higher among soldiers with v. without an insecure attachment style over the first 48 months of service, with the largest differences occurring during the first year. Specifically, SA risk over the first 6 months of service was 53/100 000 person-months among soldiers with insecure attachment v. 12/100 000 person-months for those without insecure attachment. During 7–12 months of service, risk was 79/100 000 v. 37/100 000 person-months in soldiers with v. without insecure attachment.

Figure 1. Risk of suicide attempt by time in service among Regular Army enlisted soldiers reporting an insecure attachment style.
Discussion
Using novel longitudinal data, the current study found that US soldiers' self-reported attachment style upon entering the Army was associated with future risk of medically documented SA during the first 48 months of service. Examined separately, the three insecure attachment styles (preoccupied, fearful, and dismissing) were associated with increased odds of SA, even after adjusting for socio-demographic and service-related characteristics. When all four attachment styles were examined simultaneously, preoccupied and dismissing were positively associated with future SA, even after adjusting for all other covariates, including MH-Dx. The association of dismissing attachment style with SA differed for soldiers who did v. did not receive MH-Dx during service. Among soldiers who did not receive MH-Dx, and therefore were not identified as having mental health problems, odds of SA were 2.5 times higher for those with v. without dismissing attachment. Dismissing attachment was not associated with SA among soldiers with MH-Dx. Interestingly, although insecure attachment styles were associated with higher SA risk overall, the item assessing secure attachment was non-significant, suggesting that endorsement of secure attachment is not necessarily protective in military populations.
Examination of SA risk as function of attachment and time in service revealed that risk during the first 48 months was consistently elevated in soldiers who reported one of the three insecure attachment styles, particularly during the first year of service. Dismissing attachment had the largest multivariable PARP at 11.5%, indicating that nearly 12% of SAs could be prevented if the risk associated with dismissing could be reduced, through appropriate intervention or treatment, to the risk level among those without dismissing attachment. Overall, findings indicate that soldiers entering the Army with an insecure attachment style are at increased SA risk during the first 48 months of service. These findings are broadly consistent with contemporary theoretical and empirical work highlighting the importance of interpersonal relationships in suicide (Chu et al., Reference Chu, Buchman-Schmitt, Stanley, Hom, Tucker, Hagan and Joiner2017; Joiner, Reference Joiner2005; Van Orden et al., Reference Van Orden, Witte, Cukrowicz, Braithwaite, Selby and Joiner2010).
The overall finding that insecure attachment styles are prospectively associated with increased SA risk extends cross-sectional findings from military (Wang et al., Reference Wang, Naifeh, Herberman Mash, Morganstein, Fullerton, Cozza and Ursano2022) and civilian (Palitsky et al., Reference Palitsky, Mota, Afifi, Downs and Sareen2013) samples. A previous study of NSS respondents found that when all four attachment styles were examined simultaneously, new soldiers with preoccupied or fearful attachment were more likely to report pre-enlistment SA (Wang et al., Reference Wang, Naifeh, Herberman Mash, Morganstein, Fullerton, Cozza and Ursano2022). Generally, those retrospectively reported attempts would have occurred during adolescence (Ursano et al., Reference Ursano, Heeringa, Stein, Jain, Raman, Sun and Kessler2015a), given that most NSS respondents were ⩽20-years-old at the time of survey (Rosellini et al., Reference Rosellini, Heeringa, Stein, Ursano, Chiu, Colpe and Kessler2015). In contrast, SAs in the current study were documented during the first 4 years of Army service, thus likely occurring during early adulthood. Our findings therefore provide even stronger support for the importance of preoccupied attachment as a consistent indicator of SA risk, whether examined retrospectively in the context of adolescence or prospectively during early adulthood.
The discrepancies are interesting as well: whereas the prior NSS study found fearful attachment was associated with SAs in adolescence, but dismissing attachment was not (Wang et al., Reference Wang, Naifeh, Herberman Mash, Morganstein, Fullerton, Cozza and Ursano2022), our study found dismissing attachment was associated with documented SAs in early adulthood, but fearful attachment was not. Although it is possible that these discrepancies are attributable to methodological differences (e.g. retrospective v. prospective, self-reported v. documented attempts), it is worth considering whether particular attachment styles have stronger associations with SA risk during particular developmental phases. It is also important to recognize the environmental changes that differentiate SAs before v. during military service. Individuals entering the Army are separated from many of the relationships formed during adolescence (e.g. in school) and must form new relationships with fellow soldiers in the context of Army training and acculturation. Interestingly, fearful and dismissing attachment are both forms of avoidant attachment, with fearful attachment reflecting avoidance rooted in a negative view of self and feelings of vulnerability, and dismissing attachment reflecting avoidance rooted in a positive view of self and valuing of independence (Bartholomew & Horowitz, Reference Bartholomew and Horowitz1991). It may be that avoiding relationships out of fear of rejection and/or being hurt (fearful attachment) is more detrimental in the context of adolescence and secondary school, whereas avoiding relationships out of a desire for independence (dismissing attachment) is more detrimental in the context of early adulthood and a military unit.
Importantly, dismissing attachment was associated with SA in soldiers without MH-Dx (but not in those with MH-Dx), suggesting it is specifically a risk factor for SA among soldiers who have not yet been identified by the mental healthcare system. It may be that those with a MH-Dx are more likely to receive mental health services (e.g. psychotherapy) that help to buffer against the SA risk associated with a dismissing attachment style. Preventing suicidal behavior in the one-third of suicide attempters who do not receive a MH-Dx prior to their attempt is a significant and important challenge (Naifeh et al., Reference Naifeh, Ursano, Stein, Herberman Mash, Aliaga, Fullerton and Kessler2022; Ursano et al., Reference Ursano, Kessler, Naifeh, Herberman Mash, Nock, Aliaga and Stein2018), and identifying soldiers with a dismissing attachment style might be part of future intervention strategies to assist this group.
Examination of SA risk by time in service identified periods of increased risk and may suggest that specific aspects of Army life interact with soldiers' attachment styles to create risk. The risk associated with insecure attachment was consistently elevated across all 4 years of service. However, the difference was most pronounced during the first year, an Army career phase during which SA risk is especially high (Naifeh et al., Reference Naifeh, Ursano, Stein, Herberman Mash, Aliaga, Fullerton and Kessler2022; Smith, Schaughency, Christopher, Watkins, & Anke, Reference Smith, Schaughency, Christopher, Watkins and Anke2021; Ursano et al., Reference Ursano, Kessler, Stein, Naifeh, Aliaga, Fullerton and Heeringa2015c). It may be that formation of positive interpersonal relationships with other unit members is particularly important for managing stressors during this period of initial training and Army acculturation, and those with an insecure attachment style may have greater difficulty forming, maintaining, and/or fully benefitting from such relationships. Higher unit cohesion and peer support has been found to protect against suicidal thoughts and behaviors (Anderson et al., Reference Anderson, Campbell-Sills, Ursano, Kessler, Sun, Heeringa and Stein2019; Rugo et al., Reference Rugo, Leifker, Drake-Brooks, Snell, Bryan and Bryan2020), and recent evidence suggests that interventions designed to build unit cohesion during initial military training may decrease suicide risk (Wyman et al., Reference Wyman, Pisani, Brown, Yates, Morgan-DeVelder, Schmeelk-Cone and Pflanz2020, Reference Wyman, Pickering, Pisani, Cero, Yates, Schmeelk-Cone and Pflanz2022). It is not known whether service members with insecure attachment benefit from such interventions to the same degree as those with secure attachment.
There are a number of additional important questions to address in future research. Additional work is needed to understand if and how the association between attachment style and SA risk changes across different developmental phases and life stressors/environments. Associations between attachment style and SA should also be examined within the context of soldiers' current interpersonal relationships (e.g. size of social network, perceived support from others). It is particularly important for future studies to examine whether insecure attachment is prospectively associated with the clinically important but difficult to predict (Nock, Kessler, & Franklin, Reference Nock, Kessler and Franklin2016) transition from suicide ideation to SA, as suggested by previous retrospective findings (Wang et al., Reference Wang, Naifeh, Herberman Mash, Morganstein, Fullerton, Cozza and Ursano2022). Studies should also consider whether attachment style modifies the effectiveness of interventions designed to increase unit cohesion and peer support among service members.
This study has several limitations: First, administrative data may be incomplete and/or inaccurate. Medical records are unlikely to capture all SAs and mental disorders due to factors such as underreporting, and they are subject to errors in clinician diagnosis and coding. Second, each attachment style was assessed with a single item. Multi-item attachment instruments, such as the Experiences in Close Relationships Scale (Brennan, Clark, & Shaver, Reference Brennan, Clark, Shaver, Simpson and Rholes1998), may improve precision, reliability, and validity; however, brief assessments (e.g. Lafontaine et al., Reference Lafontaine, Brassard, Lussier, Valois, Shaver and Johnson2015) are ultimately needed for large-scale population screening, such as surveying all soldiers beginning initial military training. Third, results are specific to enlisted soldiers in their first 4 years of service during the study period; therefore, the findings may not generalize to other populations.
Within the context of those limitations, the current study indicates that an insecure attachment style, particularly preoccupied or dismissing, is associated with increased risk of future SA among US Army soldiers. This elevated risk, though most substantial during the first year of service, persists for at least the first 48 months of an enlisted soldier's career. In addition, the SA risk associated with a dismissing attachment style is specific to soldiers without MH-Dx, suggesting it may be useful as a risk indicator among those not yet identified by the mental healthcare system. Future research is needed to understand whether and how the association between attachment style and SA changes across developmental phases and environmental contexts, as well as whether individuals with insecure attachment styles benefit sufficiently from emerging interventions designed to, among other things, increase peer support and unit cohesion.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291723002489
Acknowledgements
Team acknowledgements: The Army STARRS Team consists of Co-Principal Investigators: Robert J. Ursano, MD (Uniformed Services University) and Murray B. Stein, MD, MPH (University of California San Diego and VA San Diego Healthcare System). Site principal investigators: James Wagner, PhD (University of Michigan) and Ronald C. Kessler, PhD (Harvard Medical School). Army scientific consultant/liaison: Kenneth Cox, MD, MPH [Office of the Assistant Secretary of the Army (Manpower and Reserve Affairs)]. Other team members: Pablo A. Aliaga, MS (Uniformed Services University); David M. Benedek, MD (Uniformed Services University); Laura Campbell-Sills, PhD (University of California San Diego); Carol S. Fullerton, PhD (Uniformed Services University); Nancy Gebler, MA (University of Michigan); Meredith House, BA (University of Michigan); Paul E. Hurwitz, MPH (Uniformed Services University); Sonia Jain, PhD (University of California San Diego); Tzu-Cheg Kao, PhD (Uniformed Services University); Lisa Lewandowski-Romps, PhD (University of Michigan); Alex Luedtke, PhD (University of Washington and Fred Hutchinson Cancer Research Center); Holly Herberman Mash, PhD (Uniformed Services University); James A. Naifeh, PhD (Uniformed Services University); Matthew K. Nock, PhD (Harvard University); Nur Hani Zainal, PhD (Harvard Medical School); Nancy A. Sampson, BA (Harvard Medical School); and Alan M. Zaslavsky, PhD (Harvard Medical School).
Financial support
Army STARRS was sponsored by the Department of the Army and funded under cooperative agreement number U01MH087981 with the US Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health (NIH/NIMH). Subsequently, STARRS-LS was sponsored and funded by the Department of Defense (USUHS grant numbers HU00011520004 and HU0001202003). The grants were administered by the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc. (HJF).
Competing interest
In the past 3 years, Dr Kessler was a consultant for Datastat, Inc., Holmusk, RallyPoint Networks, Inc., and Sage Therapeutics. He has stock options in Mirah, PYM, and Roga Sciences. In the past 3 years Dr Stein received consulting income from Actelion, Acadia Pharmaceuticals, Aptinyx, atai Life Sciences, Boehringer Ingelheim, Bionomics, BioXcel Therapeutics, Clexio, EmpowerPharm, Engrail Therapeutics, GW Pharmaceuticals, Janssen, Jazz Pharmaceuticals, and Roche/Genentech. Dr Stein has stock options in Oxeia Biopharmaceuticals and EpiVario. He is paid for his editorial work on Depression and Anxiety (Editor-in-Chief), Biological Psychiatry (Deputy Editor), and UpToDate (Co-Editor-in-Chief for Psychiatry).
Disclaimers
The contents are solely the responsibility of the authors and do not necessarily represent the views of the Department of Health and Human Services, NIMH, or the Department of the Army. The opinions and assertions expressed herein are those of the author(s) and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences or the Department of Defense. The contents of this publication are the sole responsibility of the author(s) and do not necessarily reflect the views, opinions or policies of The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







