The increasing burden of childhood obesity together with ongoing issues of undernutrition is a public health threat to low- and middle-income countries(1). This double burden of malnutrition has been in part attributed to unhealthy diets and related behaviours. Consumption of energy-dense (high fat and sugar) foods and beverages has shown positive associations with risk of overweight and obesity in preschool children(Reference Gubbels, Kremers and Goldbohm2–Reference Yu, Chen and Zhao4). Moreover, lower intake of fruits and vegetables has been associated with undernutrition and micronutrient deficiencies in Indian young children(Reference Semba, de Pee and Sun5). Given childhood dietary behaviours track into adulthood(Reference Craigie, Lake and Kelly6,Reference Mikkilä, Räsänen and Raitakari7) and preschool age is the critical period in the formation of food preferences and choices(Reference Nicklas, Baranowski and Baranowski8,Reference Cashdan9) , cultivating healthy food choices in preschool children via age-appropriate interventions is essential.
Dietary behaviour is an outcome of multiple interactive factors within and around a child. Exploring factors that influence children’s dietary behaviour using an ecological approach is required to design effective interventions(Reference Bronfenbrenner, Husen and Postlethwaite10,Reference Moore, de Silva-Sanigorski and Moore11) . A recent systematic review of interventions targeted at improving eating behaviours of preschool children found that nutritional knowledge of family/caregivers, household food availability and family income can be modified to change the food choices of preschool children in low- and middle-income countries(Reference Sirasa, Mitchell and Rigby12). Therefore, improving family nutritional knowledge and creating a supportive family environment for the child to promote healthy eating should be targeted in healthy eating interventions for children of low- and middle-income countries(13).
Throughout the literature, child nutrition education interventions were used to improve children’s healthy food choices with some including parental education(Reference Başkale and Bahar14–Reference Céspedes, Briceño and Farkouh18). However, a recent study conducted with a group of Australian preschool children found that nutrition education and minimal parental involvement (nutrition education via brochures) increased their nutritional knowledge, but not their healthy food preferences/choices(Reference Wiseman, Harris and Lee19). Although preschool children have the ability to distinguish foods as either healthy or unhealthy(Reference Sigman-Grant, Byington and Lindsay20–Reference Wiseman, Harris and Lee22), this may not translate into healthier food choices(Reference Wiseman, Harris and Lee19). This may, at least in part, be explained by the parental belief that their preschool child’s food preferences are shaped by sensory cues of taste and appearance of the food(Reference Sirasa, Mitchell and Silva23). Therefore, a comprehensive approach beyond nutritional education to children and caregivers is required to modify children’s food preferences.
Multicomponent interventions (MCI) including parental/caregiver engagement have shown promising results in promoting healthy eating(Reference Murimi, Moyeda-Carabaza and Nguyen24–Reference Matwiejczyk, Mehta and Scott26). As parents are the key decision-makers on children’s food intake and are foremost role models for young children to imitate in their eating behaviours(Reference Østbye, Malhotra and Stroo27), involving parents in interventions is logical(Reference Sirikulchayanonta, Iedsee and Shuaytong28–Reference Peñalvo, Sotos-Prieto and Santos-Beneit31). In addition to nutrition education sessions for parents, engaging parents and children in joint interactive food activities has been shown to be more beneficial(Reference De Bock, Breitenstein and Fischer29–Reference Peñalvo, Sotos-Prieto and Santos-Beneit31) than distributing educational materials to parents via preschools(Reference Wiseman, Harris and Lee19). The study by De Bock et al. (Reference De Bock, Breitenstein and Fischer29) included meal preparation and eating meals together in groups of children, teachers and parents as an interactive activity. Moreover, incorporation of food tasting experiences and role modelling of eating by parents, teachers and peers promote healthy food preferences in preschool children(Reference Sirikulchayanonta, Iedsee and Shuaytong28,Reference Nekitsing, Hetherington and Blundell-Birtill32) .
Sri Lanka is a middle-income country, experiencing a rapid increase in childhood overnutrition with existing prevalence of undernutrition and micronutrient deficiencies. Prevalence of overweight and obesity among Sri Lankan children under 5 years has increased in urban locations by 87·5 % from 2006 to 2016 (from 0·8 % to 1·5 %)(33,34) . A recent study reported that on average, urban Sri Lankan children do not consume adequate servings of fruits (1·02) and vegetables (0·84) daily with the daily recommendations of ≥2 servings for fruits as well as vegetables met by <20 % of children(Reference Sirasa, Mitchell and Harris35). Conversely, more than one-third of children consumed sugary snacks and confectionaries daily with one in ten having them twice a day(Reference Sirasa, Mitchell and Harris35). A qualitative investigation conducted among Sri Lankan urban parents/caregivers has reported food preferences of the child as the core factor that drives food choices of preschool children(Reference Sirasa, Mitchell and Silva23). Family income, nutritional knowledge of the family, maternal control of food choices and household food preparation facilities were also selected by these parents as most influential. This highlights the need for effective eating interventions using a comprehensive approach to modify food preferences of the child and family characteristics in Sri Lanka(Reference Sirasa, Mitchell and Silva23).
The current study was designed to evaluate the effectiveness of a MCI comprising child nutrition education plus family engagement to improve the dietary diversity of urban Sri Lankan preschool children. The effect of MCI was compared with two arms: a single component intervention (SCI) involving child nutrition education and a control (no intervention). Dietary diversity as a proxy measure for nutrient adequacy and dietary quality(Reference Kennedy36) was included to assess the healthfulness of diet. Through the intervention, changes in children’s food knowledge and food preferences were expected and considered as impact pathways to improve dietary diversity. Therefore, in addition to the main effect of the intervention, dietary diversity changes, effects on these impact pathways (children’s food knowledge and food preferences) were included for assessment. We hypothesised that the MCI would be more effective than the SCI and control in increasing food knowledge, healthy food preferences and thereby dietary diversity of preschool children.
Methods
Study area
Sri Lanka is a South Asian country with a population of 21·2 million. Approximately 8 % of the population are children aged 5 years or younger, and one-third of them live in urban locations(34). In accordance with the Human Development Report 2019, Sri Lanka has been placed in the high human development category ranking the Human Development Index to seventy-one out of 189 countries and territories, which is above the average for countries in South Asia(37). The growing issue of overnutrition in children aged 5 years or younger is more striking in urban locations. The current study area includes the administrative areas of ‘Kurunegala and Mawathagama’ District Secretariats, which are local government authorities of North-western province of Sri Lanka. These locations were selected as Kurunegala is the capital of North-western province and both locations were mostly urban.
Study design and intervention description
A MCI was conducted for a 6-week period, with preschool children during February to July 2018. The MCI, underpinned by Bronfenbrenner’s Ecological System Theory(Reference Bronfenbrenner, Husen and Postlethwaite10), focused on improving the dietary diversity of children by developing food preferences of the child towards healthy food (individual characteristics), improving the nutritional knowledge of parent/caregiver and creating a supportive food environment for the child. Selection of these factors was based on a systematic review conducted in low- and middle-income countries as well as Sri Lankan parents and caregivers’ perception of factors influencing their preschool children’s food intake(Reference Sirasa, Mitchell and Rigby12,Reference Sirasa, Mitchell and Silva23) . Therefore, the MCI arm included child nutrition education plus family engagement as nutrition education for parents via group sessions; family participation in meal preparation; and tasting exposure for children with parents, teachers and peers at the preschool centres guided by the research team.
The child nutrition education intervention was designed as six 30–45-min weekly sessions with the content matched to participant characteristics and learning patterns. The sessions involved introducing food groups, awareness on importance of healthy eating for a healthy body and the differences between ‘everyday foods’ and ‘sometimes foods’ (classified according to the Sri Lankan Food Based Dietary Guidelines)(38). Foods recommended to consume are categorised as ‘everyday foods’, and those restricted are categorised as ‘sometimes foods’. The contents of the parents’ educational sessions were decided based on Sri Lankan urban parents’ perceptions of factors most influencing their preschool children’s food choices(Reference Sirasa, Mitchell and Silva23). Based on the effect of parental engagement emphasised in previous studies, the components of meal preparation(Reference De Bock, Breitenstein and Fischer29) and tasting exposure were included(Reference Sirikulchayanonta, Iedsee and Shuaytong28,Reference Nekitsing, Hetherington and Blundell-Birtill32) . An activity of washing hands before meals and during meal preparation was included due to the role of hand hygiene in reducing respiratory and gastrointestinal infections in children(Reference Willmott, Nicholson and Busse39,Reference Azor-Martinez, Yui-Hifume and Muñoz-Vico40) recognised as an immediate causative factor for child undernutrition in South-East Asia(41).
The MCI was evaluated employing a cluster randomised controlled trial with two comparison groups: SCI arm and control arm. Participating preschool centres of SCI arm received a child nutrition education intervention, where control arm received no intervention. Parents of children belonging to SCI arm received a brochure on child nutrition post-intervention. Those assigned to the control arm received a partial delayed intervention including a single nutrition education session (covering SCI session topics 1 & 2) for preschool children and a brochure on child nutrition for parents; all provided post-intervention. Detailed description of the MCI, SCI and control arms are provided in Table 1.
Table 1 Outline of the intervention components of multicomponent intervention (MCI), single component intervention (SCI) and control arm over a period of 6 weeks

Study participants
Fifteen preschool centres (known as Early Childhood Development centres in Sri Lanka) were randomly selected from a list of preschool centres (both government and privately owned) registered under the local government authorities, Kurunegala and Mawathagama District Secretariats. Preschool centre in-charges were approached in person and invited to take part in the trial, with 14 (93 %) agreeing and subsequently informing parents of children aged 4–6 years attending their centre about the opportunity to participate in the study. Children–parent dyads were recruited after obtaining written consent from parents. Consenting preschool centres were randomly assigned to one of three arms stratified by the size of the preschool centre (number of children) to promote equal numbers in all arms. Preschool centres were considered as the unit of randomisation and intervention to avoid the possibility of exchange of intervention information among parents and children between intervention and comparison arms. Participant recruitment and the study process are presented in Fig. 1. The ethical approval for this study was obtained from the Human Research Ethics Committee of Griffith University, Australia (GU Ref No: 2017/812) and Ethics Review Committee of Wayamba University of Sri Lanka (ERC No: 201810HI01).
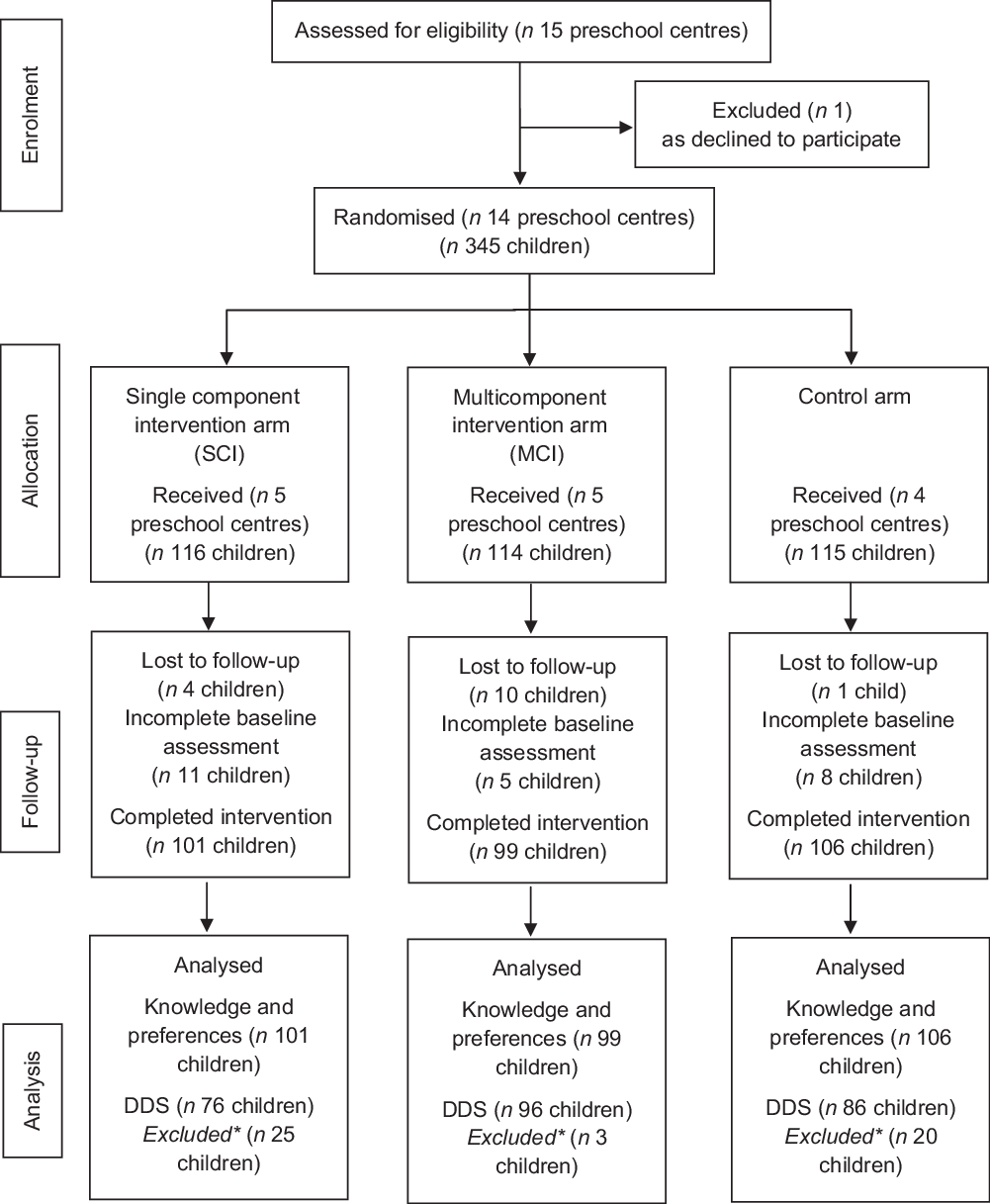
Fig. 1 CONSORT flow chart of the study process of healthy eating intervention to improve urban preschool children’s food knowledge, healthy food preferences and dietary diversity, North-western Sri Lanka
DDS, Dietary diversity score.
*Missing post DDS measures.
Given the limited evidence on impact assessment of children’s dietary diversity using difference-in-difference (DID) method and the identified link between children’s food preferences and their food choices or intake(Reference Sirasa, Mitchell and Silva23), sample size was based on a previous pre-post study design on healthy food preferences of preschool children with an effect size of 0·29 (Cohen’s d) (sd 2·41)(Reference Wiseman, Harris and Lee19). Based on the previous study(Reference Wiseman, Harris and Lee19), a minimum of ninety-five child–parent dyads per arm was required which identified a difference in preferences score of 0·69 with a power of 80 % (where α = 0·05; β = 20 %). Anticipating a dropout rate of 30 %, 125 child–parent dyads per arm were recruited in the trial. Due to time, finance and human resource limitations, all 345 child–parent dyads who consented to participate were included and were blinded to intervention conditions at recruitment and baseline assessment.
Intervention delivery/procedure
Interventions were delivered at participating preschool centres by a nutritionist-led five-member research team (final year food and nutrition undergraduate students). The research team was trained by the nutritionist on intervention delivery with mock sessions. Every child was given a stationery pack valued at AUD$5 as a token of appreciation for their participation after post-intervention assessment. All children attending the preschool centres participated in the intervention, but data were only collected from the 4–6-year-old children with parent consent.
Measures
The outcome variables were scores of children’s: (i) food knowledge; (ii) healthy food preferences and (iii) dietary diversity, assessed at both baseline (pre-intervention) and post-intervention time points. Outcomes (i) and (ii) were collected using an online desktop computer activity with children, and the main outcome variable, dietary diversity, was assessed using a 7-d food checklist via a self-administered questionnaire from parents/caregivers. Additionally at baseline, demographic and socio-economic information of children and parents/caregivers were collected through the self-administered questionnaire from parents/caregivers. Post-intervention assessment was completed within 1 week after the intervention.
Food knowledge and healthy food preference
Preschool child food knowledge and healthy food preferences were assessed using an online desktop computer activity adapted from the iPad activity titled ‘Preschool Food and Play Questionnaire’(Reference Wiseman, Harris and Downes42). The original iPad activity has ten food photo pairs, and adaptation of this tool was conducted by replacing the existing food photo pairs with similar food photos in terms of food category and local availability in Sri Lanka. As such two food photo pairs were removed due to non-availability in Sri Lanka and three new food photo pairs were included with the purpose of testing children’s knowledge regarding the unhealthiness of deep-fried fast foods and the healthiness of vegetables and green leaves. The adapted questionnaire consisted of eleven food photo pairs, one representing healthy and the other representing a relatively less healthy/unhealthy food choice. Healthy food choices were sultanas (raisins), rice, yoghurt, green gram (mung bean), drinking water, banana, milk, guava, ‘Pittu’ (made by rice flour and scraped coconut), bean curry and ‘Gotukola leaf sambal’ (green leafy vegetable salad with scraped coconut). The paired less healthy/unhealthy food choice were jujubes (candy), ‘Kottu’ (chopped flatbread meal with high-fat and salt content, prepared with refined wheat flour and oil mixed with some vegetables, egg and/meat and spices), doughnut, bun, juice (processed), biscuits, soft drink, piece of icing cake, rolls (deep-fried fast food), potato chips and chilli paste (grounded chilli flakes with high-fat content). All foods were locally photographed on a plain background. This data collection tool was implemented with each child individually in a separate room at their preschool centre and took approximately 6–8 min/child.
At the beginning of the activity, each child was asked a question ‘What do you mean by healthy?’ Then, they were provided with an age-appropriate explanation, such as, ‘Being healthy means that you can play outside, you don’t get sick and you feel good’. Thereafter, each child was asked to choose a doll and pretend that he/she was taking care of the doll and needed to help the doll to be healthy. The usage of the doll positioned the child in a caretaker role and thus makes it less likely they make choices based on personal preferences(Reference Wiseman, Harris and Downes42,Reference Calfas, Sallis and Nader43) . To test knowledge, the activity with eleven pairs of food photographs was presented to the child in random order on the desktop computer with the child asked to ‘point to the food that will make the doll healthy’. To test food preferences, the same activity was repeated (without the doll), asking the child to ‘point to food that he/she likes most’. The computer application of the activity was set up to assign the photo pair display order randomly for the assessment of each child. Choices of each child were scored as one (1) point for healthy choice and zero (0) point for relatively less healthy/unhealthy choice and summed to obtain the scores in the range of 0–11 for measures of food knowledge and food preferences separately. This assessment was performed by the nutritionist involved in this study.
Dietary Diversity Score
Dietary Diversity Scores (DDS) were calculated for each child using a 7-d food checklist, which includes nine food groups: rice, lentils, green leafy vegetables (green salads and ‘Mellum’), yellow/orange fruits, eggs, fish (including seafoods), chicken, meat other than chicken and milk (including all dairy-based food products and excluding breast milk). A DDS assessment using nine food groups was decided based on Rah et al. (Reference Rah, Akhter and Semba44), as their research was conducted with children aged <5 years which is comparable to the age group of our study population. The number of days children consumed items from the nine food groups during the previous week was obtained from parents/caregivers to determine the DDS(Reference Rah, Akhter and Semba44). The total DDS was in the range of 0–63 (nine food groups × 7 d), with the average daily DDS for each child calculated by dividing the total by seven, ranging from 0 to 9.
Demographic and socio-economic data
Demographic and socio-economic information of the parent/caregiver (age, sex, years of education, occupation and monthly family income) and the child (age and sex) were collected prior to the randomisation at baseline, from parents/caregivers of the preschool children using a paper-based self-administered questionnaire.
Data analysis
Differences between baseline child and parent/caregiver characteristics (demographic and socio-economic) of intervention and comparison arms were examined using χ 2 tests (categorical variables). Normality of the outcome variables was assessed and established by visual inspection of Q-Q plots and histograms.
Although we recruited preformed clusters of preschool centres with children, these clusters were selected from a single urban location (Kurunegala District) within a 20 km radius from the Kurunegala city, North-western Sri Lanka, allowing us to assume there is no influence of clustering. However, despite the differences in cluster sizes (number of participants at each preschool centre), intra-cluster correlation coefficient (ICC) was calculated using ANOVA(Reference Killip, Mahfoud and Pearce45) for the outcome variables of food knowledge score, healthy food preferences score and dietary diversity score at baseline and was 0·103, 0·057 and 0·057, respectively. The calculated design effect (DE) did not exceed two for main outcome variable, dietary diversity score as well as healthy food preferences score (DE = 1 + (average cluster size – 1) × ICC, where average cluster size was assumed to be the harmonic mean of the group sizes (18·8))(Reference De Bock, Breitenstein and Fischer29). Therefore, the effect of clustering was not taken into account for our analyses(Reference De Bock, Breitenstein and Fischer29).
A regression-based DID model was used to evaluate the effect of intervention arm compared with the other two arms on children’s food knowledge, preference and dietary diversity scores between the baseline and post-intervention assessment. DID was employed to control the baseline differences confounding the treatment outcomes. The estimation followed the model of:
where y is the outcome variable of interest, T i is the ‘dummy’ variable for the timeline of assessment (baseline = 0, post-intervention = 1), A i is the ‘dummy’ variable for the intervention arm (control = 0, intervention = 1) and X i is the covariate (confounders).
Parent/caregiver characteristics were considered as potential covariates except for age, gender and occupation. These characteristics were not included in the model as covariates, as they were representing the participating parent/caregiver who completed the demographic and socio-economic questionnaire, and not the primary caregiver influencing child’s dietary intake. Suitable ‘dummy’ variables were created for potential covariates, although they are time-invariant confounders.
The treatment effect (DID) is estimated as the coefficient of the interaction variable of ‘Time (T i ) and Intervention arm (A i )’, which is calculated as the difference of the mean score change in the exposed (intervention) group minus the change in the unexposed (control) group. Three combinations of exposed v. unexposed groups were tested: MCI v. Control; SCI v. Control and MCI v. SCI. The null hypothesis was based on the usual counterfactual assumption that without exposure (intervention), outcome variables of the exposed group and unexposed group followed a parallel trend over time. Analyses were performed using SPSS version 25.0(46) and Statistical software package Stata 16.0(47) with only complete data of baseline and post-intervention participants included. The type I error rate was set at 0·05 for all analyses.
Results
Characteristics of participants
Of the 345 participants recruited, 321 (93·0 %) completed all assessment at baseline (including demographic and socio-economic information), 306 (88·7 %) completed two outcome variables (food knowledge score and healthy food preference score) and 258 (74·8 %) completed the third outcome variable (DDS) at the post-intervention assessment. Analyses were based on 306 child–parent dyads except for DDS. The majority of children belonged to the age category of 48–59 months (84·6 %), with similar sex distribution at all three arms. There were significant baseline differences between the intervention and comparison arms for parent/caregiver characteristics including gender, ethnicity, years of school education, occupation and monthly household income (Table 2). The participating parents/caregivers in MCI arm (with family engagement) included comparatively more females (95·0 %), housewives (75·8 %), fewer years of education (<12 years) (62·6 %) and had lower monthly household income of <45 000 LKR (<USD 241·18) (85·9 %) as well as fewer belonging to Sinhalese ethnicity (63·6 %) compared with those in the SCI and control arms.
Table 2 Demographic and socio-economic characteristics of the participants (n 306); 4–6-year-old children and their parent/caregivers, at baseline by intervention and control arm, and comparison of difference between arms, North-western Sri Lanka, February–July 2018

MCI, Multicomponent intervention; SCI, Single component intervention.
Significant P values are indicated in bold font.
* Missing value from one participant.
† Statistics using χ 2 test.
Children’s food knowledge score
Children’s food knowledge (mean) scores increased significantly from baseline to post-intervention for both MCI and SCI arms (Table 3). Table 3 presents the effects of intervention using DID estimation with three outcome variables adjusted with three covariates (parents/caregivers’ ethnicity, years of education and household monthly income). As an impact pathway effect, significant positive intervention effects were observed in MCI and SCI arms compared with control arm with mean knowledge score changes (DID) of 3·76 and 2·66, respectively (Table 3). Children who received the MCI showed comparatively greater food knowledge score than that of children who received SCI (DID = 1·10).
Table 3 Intervention effects on mean scores of 4–6-year-old children’s healthy food knowledge, healthy food preferences and dietary diversity compared with control/single component intervention (SCI) arm: difference-in-difference (DID) estimation, North-western Sri Lanka, February–July 2018

MCI, Multicomponent intervention.
Significant P values are indicated in bold font.
* Comparing value of pre- and post-intervention assessment in each arm using regression model.
† Intervention effect was compared with control, and different comparison has been specified as MCI v. SCI under each outcome variable.
‡ Difference-in-difference was estimated using linear regression model adjusting for covariates including caregivers’ ethnicity, caregivers’ years of school education and caregivers’ household monthly income. Ethnicity of Sinhalese ethnic group = 0 and other ethnic groups = 1, since majority of the study population were Sinhalese. Parent/caregiver years of education of <12 years = 0 and ≥12 years = 1, as completing 11 years of education (General Certificate of Examination Ordinary Level – senior secondary education) is the milestone achieved by most (70 %) Sri Lankans(Reference Dundar, Millot and Riboud48). Parent/caregivers’ monthly family income of <45 000 LKR = 0 and ≥45 000 LKR = 1, since the median monthly income of households in Kurunegala District was around 45 000 LKR(49).
§ Robust Standard Error.
Children’s healthy food preferences score
Mean scores for healthy food preferences significantly increased in MCI and SCI from baseline to post-intervention (Table 3). According to DID estimation, positive significant intervention effects were reported in MCI arm (DID = 2·79) and SCI arm (DID = 2·15) (Table 3) compared with control arm. Non-significant positive effects were observed in MCI v. SCI arm (with v. without family engagement) (DID = 0·64, P = 0·220) (Table 3).
Children’s dietary diversity score
Neither of the MCI nor SCI showed significant differences in average dietary diversity score of children between baseline and post-intervention (Table 3). Although minor positive intervention effects were reported in MCI compared with control arm (DID = 0·09) and SCI arm (with v. without family engagement) (DID = 0·16), the effect was not significant (Table 3).
Discussion
Multicomponent (involving parents and family engagement), population-specific eating interventions, which address underlying factors driving children’s food choices, are proven to be effective in establishing healthy food choices in preschool children(Reference Murimi, Moyeda-Carabaza and Nguyen24–Reference Matwiejczyk, Mehta and Scott26). The present study shows that MCI (with family engagement) in Sri Lankan urban children influences the impact pathways for children’s dietary diversity positively but does not improve the dietary diversity. The MCI significantly increased children’s food knowledge and healthy food preferences scores by around 3·76 and 2·79, respectively, on an eleven-point scale compared with the control arm. Children’s dietary diversity score showed a non-significant slight increase of 0·09 on a nine-point scale after receiving MCI. Compared with SCI (without family engagement), MCI increased all three outcome variables, but significant effect was only found in children’s healthy food knowledge score.
Intervention effects were estimated using DID method, and MCI showed a significant positive effect on children’s mean food knowledge and healthy food preferences scores compared with the control group. This is consistent with previous research that assessed children’s food knowledge, attitudes and habits after a MCI(Reference Peñalvo, Sotos-Prieto and Santos-Beneit31). In the current study, interactive meal preparation sessions with parents at preschool centres combined with eating the prepared meals together facilitate taste exposure to foods and modelling of food behaviour. This is consistent with the findings of Sirikulchayanonta et al. (Reference Sirikulchayanonta, Iedsee and Shuaytong28) study conducted among Bangkok kindergarten children that showed cooking, tasting and eating together increased the intake of fruits and vegetables as well as a review that reported taste exposure interventions yielded successful outcomes in healthy food (vegetables) choices and consumption(Reference Nekitsing, Hetherington and Blundell-Birtill32). The present study found that meal preparation sessions and provision of a recipe book with easy to prepare healthy recipes for kids supported parents cooking skills and confidence to prepare healthy meals for their children. Evidence confirms that cooking programmes have improved the cooking confidence in parents and thereby promote healthy food choices in parents and their children(Reference Izumi50,Reference Robson, Stough and Stark51) .
In this study, SCI showed positive effects for children’s mean food knowledge and healthy food preferences scores compared with the control arm. While the MCI revealed greater effects on children’s food knowledge and healthy food preferences, when compared with the SCI outcomes, there was not a statistical difference in children’s healthy food preferences score. At face value, this finding suggests that an SCI oriented on nutrition education for children could be a more cost-effective and feasible intervention which offers similar positive outcomes to a MCI. It is evident that preschool centre-based nutrition education alone can improve the nutritional knowledge of children, which can positively influence their food preferences and support healthy food consumption(Reference Sigman-Grant, Byington and Lindsay20,Reference Cason52) . However, it is unknown whether the acquired food knowledge and healthy food preferences by children who received the SCI would be sustained in the medium term compared with an MCI that also engaged parents. Sustained effects have been observed in children’s nutrition education interventions that include some involvement of primary caregivers such as nutrition education sessions, workshops, provision of nutrition information pamphlets/brochures, menu samples and weekly positive health messages to primary caregivers(Reference Başkale and Bahar14–Reference Céspedes, Briceño and Farkouh18). A recent review reported that allowing an adequate duration (at least 6 months) to observe intervention effects is an important undertaking to evidence the success of an intervention(Reference Murimi, Moyeda-Carabaza and Nguyen24). Future research should include a third data collection point 6 months post-intervention to examine whether the improved knowledge and preferences are sustained at a similar level in both groups (SCI and MCI).
The current study found no significant differences in children’s dietary diversity score between children who participated in either MCI or SCI arms when compared with those in the control arm. MCI impacted more positively on children’s dietary diversity score than that of SCI, though the difference was not significant. This might be due to the short duration (6 weeks) of the intervention programme in our study being not adequate to generate positive changes in the home food environment. Home environment with healthy food availability and role modelling of healthy eating behaviours by parents have been shown to increase healthy food intake of US children aged 2–5 years(Reference Østbye, Malhotra and Stroo27). In this regard, the home food environment is associated with socio-economic characteristics of parents such as employment, education and income(Reference Sirasa, Mitchell and Silva23,Reference Fernández-Alvira, Mouratidou and Bammann53) . A recent study with Sri Lankan urban parents of preschool children identified that family income is a most important factor in a child’s food choices, especially healthy foods, which can be more costly(Reference Sirasa, Mitchell and Silva23). The modifying effect of socio-economic characteristics on the impact of healthy eating intervention warrants attention for future studies.
The current study has focused on the role of parents’ nutrition knowledge and the home food environment in children’s food knowledge, preferences and dietary diversity. However, it is important to acknowledge that the general food environment constraints the home environment through factors such as food availability in the market, food prices, accessibility to food and food promotions via mass media(Reference Story, Kaphingst and Robinson-O’Brien54,Reference Andreyeva, Kelly and Harris55) . In Sri Lanka, there is a wide availability of unhealthy foods in the market(Reference Townsend, Williams and Wickramasinghe56) and extensive advertisement of unhealthy food items through television(Reference Prathapan, Wijewardena and Low57). Modifying the general food environment is a long-term strategy which will require substantial changes in government policies(Reference Story, Kaphingst and Robinson-O’Brien54).
Previous MCI studies that have reported positive effects on dietary intake were conducted over a longer timeframe ranging from 10 weeks(Reference Aktaç, Kızıltan and Avcı58) to 1 year(Reference Hu, Ye and Li15,Reference De Bock, Breitenstein and Fischer29,Reference Yongqing, Chunsheng and Jian30) . Either a delayed post-intervention assessment or repeating the intervention for an extended period, to provide greater time for changes in the home food environment (e.g. household food availability, number of family meals/week) to be implemented, could be required to identify the intervention’s impacts on dietary diversity of children. Additionally, a mediation analysis could be conducted to assess the magnitude of changes in dietary diversity that is accounted for by changes in children’s food knowledge or healthy food preferences to evidence positive changes with time.
Strengths of the present study include inclusion of adequate sample size in each arm and usage of age-appropriate evaluation methods to collect data from the population of interest. Evaluating children’s responses using an age-appropriate visual food photograph activity increases the engagement of children in the research and the credibility of our findings(Reference Wiseman, Harris and Lee19). Additionally, usage of the DID estimation method to evaluate the impact of the intervention/exposed arm compared with the control/unexposed arm is also considered a strength of this study, as the confounding effects of the baseline characteristics were adjusted, thus supporting the generalisability of the findings to other urban locations in Sri Lanka.
The present study has several limitations. First, although the intervention was assigned randomly, which reduced selection bias, the randomisation was made at the preschool centre level rather than at the individual level. As Sri Lankan preschools are mostly conducted in any of two local languages (Sinhala and Tamil), language-bound ethnic groups are predominant in each preschool centre and due to time and financial restrains, selection of all consenting children from invited preschools ended up creating unequal cluster sizes. Although the cluster effect on outcome variables was ignored based on the design effect, unequal cluster sizes and specific ethnicity-dominated preschool clusters might have accounted for the differences between the baseline demographic and socio-economic characteristics of the participants among the three arms. However, DID estimation allowed adjustment for all observed and unobserved confounders during intervention effect/impact calculation. Second, only data from the consenting child–parent dyads were included for analysis, which means there is potential for selection bias in the study sample as parents more concerned about health may be over-represented. Third, this study did not employ a delayed post-intervention assessment to assess longer-term impacts. Allowing a transition period is important for parents to apply their newly acquired knowledge and resources and encourage children for healthy eating. This could be addressed by lengthening the intervention duration or including a third data collection point. Finally, sub-analyses to examine the effects of family socio-economic characteristics on the intervention could not be considered due to sample size limitations. Future studies with a larger sample size should consider the inclusion of socio-economic factors.
Conclusion
Overall, our findings suggest that the MCI, comprising nutrition education with children and parents together with family participation in meal preparation and tasting, positively influenced the food knowledge and healthy food preferences of Sri Lankan urban preschool children, but not the dietary diversity score. For all intervention outcomes, comparatively greater effects were reported in MCI over SCI (though not significant). Increased food knowledge and preferences did not change eating behaviour. While a longer intervention may see positive changes in the home food environment, moderated by family socio-economic factors, meaningful community change will remain difficult unless the context of the broader food environment is addressed. Future research should examine whether a longer intervention or delayed post-intervention assessment would see positive changes in the home food environment and why increased knowledge and preferences do not translate into improved dietary diversity. Findings suggest that there could be merit in the inclusion of activity-based nutrition education in the preschool curriculum for both children and caregivers in middle-income countries.
Acknowledgements
Acknowledgements: We would like to thank the Kurunegala and Mawathagama District Secretariats (local government authorities) and preschool centre in-charges for granting permission to carry out the study. We would like to give recognition to the undergraduate research team of Wayamba University of Sri Lanka (Maduwanthi Wathsala, Randika Vishwanath, Lahiru Sandaruwan, Asnaka Weudage, Naseeha Nasneen) for their support in intervention preparation and delivery. We also thank the preschool centres and teachers for their time and support offered to deliver interventions and evaluation, and the parents/caregivers and children for their participation. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. F.S. was supported by a PhD scholarship from Griffith University, Australia. Conflict of interest: There are no conflicts of interest. Authorship: F.S. conceptualised and designed the study, collected data, analysed the data and drafted the manuscript; L.M. and N.H. contributed to study design, supervised the study and critically reviewed the manuscript. A.C. supervised the study on-site and critically reviewed the manuscript. A.A. was involved in data collection, analysis and interpretation. All authors contributed substantially to revisions of the manuscript, read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Human Research Ethics Committee of Griffith University, Australia (GU Ref No: 2017/812) and Ethics Review Committee of Wayamba University of Sri Lanka (ERC No: 201810HI01). Written informed consent was obtained from all participants before commencement of the study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001877






