Food insecurity and malnutrition, which are common consequences of conflict and long-term socio-economic hardship, have emerged in the Occupied Palestinian Territory (oPt) since the year 2000(1). According to the 2002 Nutritional Assessment of the West Bank and Gaza Strip, escalation of the Palestine–Israel conflict has led to ‘a deterioration of the household economies, interfered with food availability and accessibility, and raised the probability of a significant problem of undernutrition’(Reference Abdeen, Greenough, Shahin and Tayback2).
As observed in previous studies(Reference Yip3), anaemia among Palestinian refugees is due essentially to the poor availability of dietary Fe, and children and women are disproportionally affected. They are therefore the best group to monitor. Anaemia is a slow-onset consequence of micronutrient deficiency(Reference Seal, Creeke, Mirghani, Abdalla, McBurney, Pratt, Brookes, Ruth and Marchand4, Reference Dunbar5); thus its prevalence might be linked to socio-economic conditions in the oPt in previous years.
The estimated anaemia prevalence among pregnant Palestinian refugee women in 1990 was 67·4 % in the Gaza Strip and 47·6 % in the West Bank(Reference Madi6). In 1999 the rates had decreased to 44·7 % in the Gaza Strip and 35·5 % in the West Bank(7). The aim of the present paper is to describe the current prevalence of anaemia among pregnant women in the oPt, correlating the findings with social and biological determinants.
Experimental methods
Study setting
The study was conducted in September and October 2006 among registered pregnant Palestinian refugee women who attended UNRWA (United Nations Relief and Works Agency for Palestine Refugees in the Near East) antenatal clinics in the Gaza Strip and West Bank.
Subjects
UNRWA is the main health-care provider for the Palestine refugee population. It provides primary health care in 134 primary health-care facilities in Lebanon, Syria, the West Bank, the Gaza Strip and Jordan. Through its comprehensive antenatal and postnatal programme, it offers prevention and treatment of Fe-deficiency anaemia comprising supplementation and treatment with Fe and folic acid preparations, food supplementation, and fortification of wheat flour with Fe, folic acid and vitamins.
All pregnant women attending the UNRWA antenatal services were targeted for Hb testing and enrolled in the study from September 2006 until the sample size was reached. The catchment area comprised fifty-five UNRWA health centres in the oPt (eighteen in the Gaza Strip and thirty-seven in the West Bank).
Data collection
A data collection sheet was designed. Background information collected included age, education level, parity, trimester of gestation and interfamily marriage. Data were collected at the health centre level by staff nurses and compiled and validated by the Chief of the UNRWA Health Protection and Promotion Programme.
Biochemical analysis
Hb levels were determined using the cyanmethaemoglobin method. The cut-off point for anaemia was defined as Hb level below 11·0 g/dl. Anaemia was further categorized as mild (Hb = 9·0–10·9 g/dl), moderate (Hb = 7·0–8·9 g/dl) and severe (Hb < 7·0 g/dl)(Reference Reveiz, Gyte and Cuervo8).
The study protocol was approved by the UNRWA Health Department Ethical Review Committee.
Statistical methods
Sample size was calculated using expected prevalence rates from an identically designed survey conducted by UNRWA in 2004 and defining a confidence level of 95 %, power of 80 % and precision to the nearest 3 %.
The statistical significance of the association between anaemia and social and biological determinants was calculated using the χ 2 test. P values less than 0·05 were considered statistically significant.
Data were entered and analysed with the Epi Info™ for Windows statistical software package version 3·4·1 (distributed by Centers for Disease Control and Prevention, Atlanta, GA, USA).
Results
The sampling frame consisted of 1740 pregnant women, randomly selected among those attending UNRWA antenatal services in the oPt. Mean age was 27·1 (sd 6·0) years, mean parity was 2·7 (sd 2·3) live births and mean number of years of education was 10·9 (sd 3·1).
Anaemia prevalence in the oPt in 2006 was found to be 38·6 % (95 % CI 36·3, 40·9 %). Most women (92·4 %) suffered from mild anaemia; the prevalence of moderate-to-severe anaemia was 3 % (1·9 % in the West Bank and 4·1 % in the Gaza Strip).
The present survey showed a significant (χ 2 = 12·9, P < 0·01) overall increase in anaemia prevalence compared with 33·2 % reported in 2004. However, once stratified by geographical area, the increase was statistically significant only for the Gaza Strip (χ 2 = 16·8, P < 0·01; Table 1).
Table 1 Anaemia prevalence among pregnant Palestinian women, 2004 and 2006

Anaemia prevalence was found to increase with age, parity and trimester of pregnancy. The latter showed the strongest correlation with anaemia, with a threefold risk of developing the disease in the second and third trimesters of gestation as opposed to the first (second trimester v. first: OR = 3·2, 95 % CI 2·2, 4·6; third trimester v. first: OR = 3·3, 95 % CI 2·2, 4·8). No statistical correlation was found between anaemia and level of education, interfamily marriage and residence in a camp, in both West Bank and Gaza Strip (Table 2).
Table 2 Association between anaemia and social and biological determinants among pregnant Palestinian women, 2006

*Statistically significant correlation.
†‘Relative’ indicates any other person related by blood excluding first cousins (sons of siblings of the mother/father) or second cousins (sons of a first cousin of the woman’s parent).
Discussion
Anaemia among pregnant women in the oPt (38·6 % prevalence) is a public health problem that can be classified as moderate in the West Bank (31·1 %) and severe in the Gaza Strip (44·9 %)(9).
The global prevalence of anaemia among pregnant women reported in the WHO 2007 survey among pre-school children, pregnant women and non-pregnant women of reproductive age was 41·8 % (95 % CI 39·9, 43·8)(Reference McLean, Cogswell, Egli, Wojdyla and De Benoist10). Analysing the global data disaggregated by UN region (Fig. 1) shows our surveyed population to have a prevalence of anaemia between the rates of Asia and Latin America and the Caribbean, with the highest rates observed in the Gaza Strip. Considering Europe as the standard comparator, the prevalence of anaemia among pregnant Palestinian women is more than double.

Fig. 1 Anaemia prevalence (95 % CI) among pregnant women (LAC, Latin America and the Caribbean; NA, North America): comparison of data from the 2007 WHO global review(Reference McLean, Cogswell, Egli, Wojdyla and De Benoist10) and the present 2006 UNRWA (United Nations Relief and Works Agency for Palestine Refugees in the Near East) study in the Gaza Strip and the West Bank
Conversely, if we consider the prevalence rates of anaemia among pregnant women in countries of the Eastern Mediterranean Region as published by WHO in 2004(Reference Bagchi11), only the West Bank has a prevalence rate that is in line with those observed in neighbouring countries. The Gaza Strip has a much higher prevalence (Fig. 2).
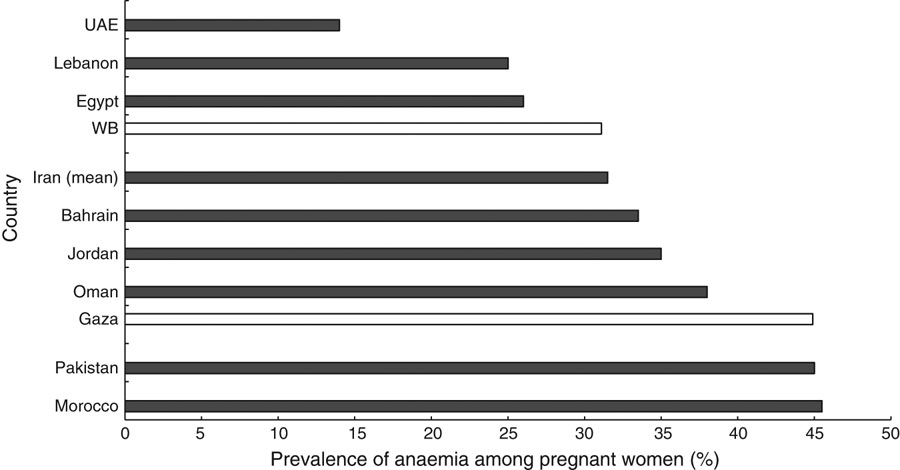
Fig. 2 Anaemia prevalence among pregnant women (UAE, United Arab Emirates): comparison of data from the 2004 survey of the WHO Eastern Mediterranean Region(Reference Bagchi11) (█) and the present 2006 UNRWA (United Nations Relief and Works Agency for Palestine Refugees in the Near East) study in the Gaza Strip and the West Bank (WB) (□)
This might correlate with the worsening of socio-economic conditions in the Gaza Strip in spite of UNRWA interventions. What can be inferred from the data presented is that if the social and economic situation in the oPt does not improve, anaemia rates among Palestine refugees could be subjected to future worsening(Reference Bocco, Brunner, El Haj, Al Husseini, De Martino, Khalidi and Lapeyre12).
Although low intake of dietary Fe has been indicated as the main cause of anaemia and the rationale for supplementation programmes, there is currently no scientific evidence that aid programmes comprising flour fortification or food supplementation have improved Fe status of targeted population groups(13).
UNRWA has a long-standing Fe supplementation programme targeting pregnant Palestinian refugee women in the oPt. Coverage has been over 90 % in the past 10 years. Although studies on patient compliance have not been carried out, data from UNRWA pharmacies indicate that on average 90 % of enrolled women regularly receive Fe supplementation as prescribed by UNRWA physicians.
The present study revealed a persistently high prevalence of anaemia despite the existing long-term supplementation programme. The lack of improvement in anaemia prevalence notwithstanding Fe supplementation programmes shows that anaemia cannot be attributed to one cause. It is now accepted that anaemia is not determined by the presence of a single risk factor but by interactions between groups of risk factors, such as poor Fe absorption due to inhibiting dietary substances such as tannins and phytates, high birth rates, short birth intervals, concurrent infections and genetic diseases(Reference Bagchi11).
There is still debate on the relationship between birth interval and anaemia(Reference Dewey and Cohen14, Reference Conde-Agudelo, Rosas Bermudez and Kafury-Goeta15), although relevant correlations between anaemia and inter-pregnancy intervals shorter than 6 months(13, Reference Conde-Agudelo and Belizan16) have been described. This is consistent with the findings of the present survey, where frequent pregnancy was correlated with increased anaemia prevalence.
As expected, the lowest rate of anaemia was observed during the first trimester of pregnancy in both settings and anaemia levels almost doubled in the second and third trimesters of gestation. This variable was the strongest determinant found in the present study: the risk of developing anaemia was threefold higher in the second and third trimesters. Pre-existing anaemia is a risk factor for haemorrhage-related maternal deaths that are one of the main causes of maternal mortality among UNRWA Palestinian refugees(17).
Although Fe metabolism was not studied, the high anaemia prevalence observed combined with epidemiological evidence from previous studies(Reference Yip3) supports Fe deficiency as the most relevant aetiological factor among pregnant Palestinian refugee women in the oPt. The present survey demonstrated a statistical correlation between anaemia, trimester of pregnancy and parity, with a particularly high risk of developing anaemia in the later stages of pregnancy. This suggests a condition triggered by a pregnancy-induced increased metabolic requirement rather than the consequence of chronically severe micronutrient deficiency. However, the high prevalence rates observed support the hypothesis that concurrent factors such as subclinical micronutrient deficiency, genetic traits and exposure to toxic agents could play a role in making women more prone to developing clinical anaemia during pregnancy.
Although the survey offers enlightening hints on the correlation between biological/social determinants and anaemia prevalence, a study on aetiology including Fe metabolism was not conducted and therefore causal relationships in this setting cannot be found. Further studies are necessary to examine the relative risk of developing anaemia by cause (toxic, nutritional or genetic).
Acknowledgements
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sector. Each author has seen and approved the contents of the submitted manuscript and declares that there are no conflicts of interest. G.S. revised the paper and analysis; F.R. carried out the analysis; A.K. and H.M. designed the study, supervised data collection and entry, and drafted the paper. We would like to acknowledge the support provided by the chiefs of the Field Health Programmes in the Gaza Strip and the West Bank, the field laboratory services officers, the field nursing officers, medical officers, senior staff nurses, midwives, professional nurses, laboratory technicians and clerks, who played a major role in blood testing and the process of referral and data collection. Special thanks to Dr Mohammed Maqadmeh, Field Family Health Officer in the Gaza Strip, and to Dr Elias Habash, Field Family Health Officer in the West Bank, for supervising the process of data collection and entry. We would also like to thank Dr Yousef Shahin, Head of the Health Information System, and Ms Wafa’a Zeidan, Assistant Statistician, for their help with data compilation and analysis; and Mr Ahmad Al-Natour, Senior Laboratory Services Officer at the HQ.






