In recent years, it has become overwhelmingly clear that regularly eating foods that are high in energy, such as saturated fats, with added sugar and salt, is among the key risk factors for developing weight problems, metabolic disorders and related diseases(Reference Hooper, Abdelhamid and Bunn1–Reference Te Morenga, Howatson and Jones3). In this regard, the WHO has produced specific recommendations on the appropriate dietary intake of the above-mentioned elements to prevent the rise of non-communicable diseases(4). In particular, total fat should not exceed 30 % of the total energy intake, saturated fat should be <10 % of the total energy intake and trans-fat <1 %. Fat consumption should shift away from saturated fats and trans-fats to unsaturated fats and towards the goal of eliminating industrially produced trans-fats. As regards the intake of free sugars, this should be limited to <10 % of the total energy intake, and <5 % is suggested for additional health benefits. Keeping salt intake to <5 g a day (corresponding to Na intake of <2 g a day) helps to prevent hypertension and reduces the risk of heart disease and stroke in the adult population(4).
By the mid-1900s, this trio of ingredients – salt, sugar and fat – had taken on a new psychosensory dimension because the processed food industry had discovered that they could be formulated to generate a sense of satiety and pleasure in consumers(Reference Rao, Rodriguez and Shoemaker5). Palatable food activates brain reward circuitry through fast sensory inputs and slow post-ingestive consequences (such as raising glucose concentration in the blood and brain). The repeated supraphysiological stimulation of reward pathways may make people’s behaviour increasingly compulsive and lead to further loss of control over food intake and ultimately to obesity(Reference Volkow and Wise6,Reference Yeomans and Gray7) . It is well known that the foods that are more palatable and that induce more cravings are typically processed foods or foods with a high salt, sugar and/or fat content(Reference Rao, Rodriguez and Shoemaker5). Today, crave-inducing foods and soft drinks are sold and consumed worldwide, creating an unfavourable food environment that has led to higher rates of obesity and its co-morbidities, diabetes and CVD(Reference Traill, Mazzocchi and Shankar8,Reference French, Story and Jeffery9) .
From the above considerations, there is an abundantly clear need to implement all useful strategies to induce people to lower their consumption of sugar, salt and fat in an effort to improve the population’s general health and prevent the non-communicable diseases that are currently the main causes of death. Providing the population with appropriate dietary information and promoting a healthy eating behaviour are certainly essential to efforts in this sense.
One factor that has gained importance in recent years, as evidence has emerged of its association with health-related behaviours (such as diet), is health literacy (HL)(Reference von Wagner, Knight and Steptoe10), or an individual’s ability to access and understand health-related information and consequently make appropriate health-related decisions. HL empowers individuals, enabling them to take responsibility for their health(Reference Kickbusch11,Reference Nutbeam12) . A limited HL has an adverse impact on health-related behaviour and disease-preventing strategies, such as participation in screening programmes(Reference Davis, Williams and Marin13–Reference Pappas, Siozopoulou and Saplaoura16). In addition, people with a limited HL tend to make more use of healthcare services, including hospitalisations and emergency services, partly as a consequence of their often adopting unhealthy lifestyles(Reference Lynn Nielsen-Bohlman and Kindig17–Reference Cho, Lee and Arozullah19). HL can thus play a fundamental part in health promotion and prevention strategies(Reference Nutbeam20), and its importance was emphasised at the Ninth Global Conference on Health Promotion (Shanghai, 2016)(21). Moreover, the theoretical model of health promotion indicated that improving HL is a way to improve people’s control and thereby change intermediate health outcomes such as dietary habits. However, no syntheses of empirical evidence have yet been provided. Concerning nutrition and dietary behaviour, it was recognised that higher levels of literacy, numeracy and HL are predictors of food label use, good portion-size estimation skills, lower BMI and better dietary quality(Reference Malloy-Weir and Cooper22–Reference Cha, Kim and Lerner25). However, there are still several aspects that remain to be clarified, for example, if HL affects the intake of specific nutrients.
The first aim of this systematic review was to shed more light on the link between HL and dietary intake of sugar, salt and fat. The second aim was to discover the role of baseline HL levels in influencing the effectiveness of health promotion programmes aiming to encourage appropriate sugar, salt and fat intake. To achieve the first aim, we collected and summarised all currently available data emerging from observational studies generating evidence of the association between HL and dietary intake of sugar, salt and fat. To assess the second aim, we considered intervention studies promoting a healthy diet that referred specifically to an appropriate sugar, salt and fat intake, and we analysed their outcomes to see whether HL moderated the efficacy of such intervention.
Methods
Search strategy
For the current study, a comprehensive and systematic literature search was conducted in the Medline and Scopus databases to identify:
-
1. observational studies (cross-sectional, cohort and case–control studies) investigating the association between HL and dietary intake of sugar, fat and salt;
-
2. intervention studies aiming to promote an appropriate intake of these three ingredients to see whether HL influences the efficacy of the intervention.
The search process involved the use of three different search strings obtained by combining the terms ‘health literacy’ or ‘literacy’ with the terms ‘sugar*’ or ‘sweet*’ or ‘sport drink’, and ‘salt*’ or ‘salty’ or ‘sodium’, and ‘fat*’ or ‘fatty’ using Boolean operators. Three different search strings were used (one for each of the nutrients considered), so the search yielded three different lists of papers. The search strings were defined as explained in online supplementary material, Appendix 1.
The records retrieved from the databases were imported in Endnote and duplicates were removed. Two reviewers (G.G. and L.M.) checked the search hits by reading the article titles and abstracts. If the results of a study were published more than once, only the most complete article was considered in the analysis. The authors also checked the reference lists of the papers included in the review for any articles not already considered.
Data extraction
The following data were extracted from each study: first author’s name, year of publication, journal, study design, sampling method, characteristics of the study sample (e.g., age range), measures of outcome and exposure, results, confounding factors, interactions and the author’s conclusions.
Eligibility criteria
The studies included in the review had to meet the following inclusion criteria: HL had to be measured using validated questionnaires; dietary intake of sugar, fat and salt had to be measured quantitatively; a measure of the association between HL and dietary sugar/fat/salt intake had to be reported and the paper had to have been published from January 2000 up until January 2019 (for sugar) or March 2019 (for salt and fat) and written in English. Studies involving patients with a specific disease and previous systematic reviews were ignored. For the intervention studies, only explicit interventions aimed at reducing salt, sugar or fat intake were considered in this systematic review.
Quality assessment criteria
Two different authors (G.G. and L.M.) independently judged the methodological quality of the studies using the Strengthening the Reporting of Observational Studies in Epidemiology approach(21) for observational studies and the Consolidated Standards of Reporting Trials approach(Reference Malloy-Weir and Cooper22) for randomised controlled trials. Total Strengthening the Reporting of Observational Studies in Epidemiology and Consolidated Standards of Reporting Trials scores were calculated for each study. A larger percentage of items conforming to the guidelines indicated a higher methodological quality: ≥80 % excellent quality, 60–79 % good quality, 50–59 % sufficient quality and <50 % poor quality. A Cohen’s kappa score was calculated to establish the level of agreement between the two reviewers’ assessments.
Results
The reference lists of the nine selected articles yielded no additional papers meeting our inclusion and exclusion criteria. The review was thus conducted on nine papers in all (one paper assessed the association between HL and both sugar and salt intake). Among these, eight were observational studies, while one was a randomised controlled trial.
Considering these nine articles, the number of participants enroled in each observational study ranged from 100 to 3165. Seven studies(Reference Huizinga, Carlisle and Cavanaugh23–Reference Persoskie, Hennessy and Nelson29) were conducted on adults (one of them(Reference Huizinga, Carlisle and Cavanaugh23) only enroled participants over 60 years old), while one study sample(Reference Naghibi Sistani, Virtanen and Yazdani30) consisted of dyads involving a female caregiver and a 3- to 5-year-old child, and one study was conducted on adolescents aged 13–15 years(Reference Zoellner, You and Connell31).
The studies were conducted in various parts of the world, including the USA (five studies), Iran (two studies), Switzerland (one study) and Indonesia (one study), and they were published between 2012 and 2018.
HL was measured with the Newest Vital Sign tool in three studies (one of them considered only three of the six items in the test) and with the Rapid Estimate of Adult Literacy in Medicine – Short Form(Reference Zoellner, Hedrick and You32) in two studies. Other tools used in single studies were the Rapid Estimate of Adult Literacy in Dentistry-30(Reference Luta, Hayoz and Gréa Krause33), the Nutrition Literacy Questionnaire (NLQ-20)(Reference Guntzviller, King and Jensen34), the Oral Health Literacy – Adults Questionnaire(Reference Divaris, Lee and Baker35) and the Test of Functional Health Literacy in Adults – Shortened version. Two tests were administered in one study: a Short Food Literacy Questionnaire for adults(Reference Joulaei, Keshani and Kaveh36) and the sixteen items concerning the health promotion domain in the European Health Literacy questionnaire (HLS-EU-Q47, German version)(Reference Arozullah, Yarnold and Bennett37).
The studies varied in their approach to measuring the outcomes and relied mostly on self-reported information. In the majority of cases, participants answered questionnaires about their nutritional habits; only one study estimated Na intake (in g/d) from urinary excretion. Tables 1 and 2 provide details of the observational studies identified and included in the review.
Table 1 Overview of studies reviewed. Material and methods
OHL, oral health literacy; REALM-SF, Rapid Estimate of Adult Literacy in Medicine, Short Form; HL, health literacy; NVS, Newest Vital Sign; OHLAQ, Oral Health Literacy − Adults Questionnaire; SSB, sugar-sweetened beverage; FL, food literacy; HEI, Healthy Eating Index; DGA, Dietary Guidelines for Americans; BEVQ, Beverage Intake Questionnaire; MHC, monthly health checkups.
Table 2 Overview of studies reviewed. Results

HL, health literacy; OHL, oral health literacy; FNL, functional nutrition literacy; NFP, Nutrition Facts panel; SSB, sugar-sweetened beverage; FL, food literacy; SNAP, Supplemental Nutrition Assistance Program.
Health literacy and sugar intake
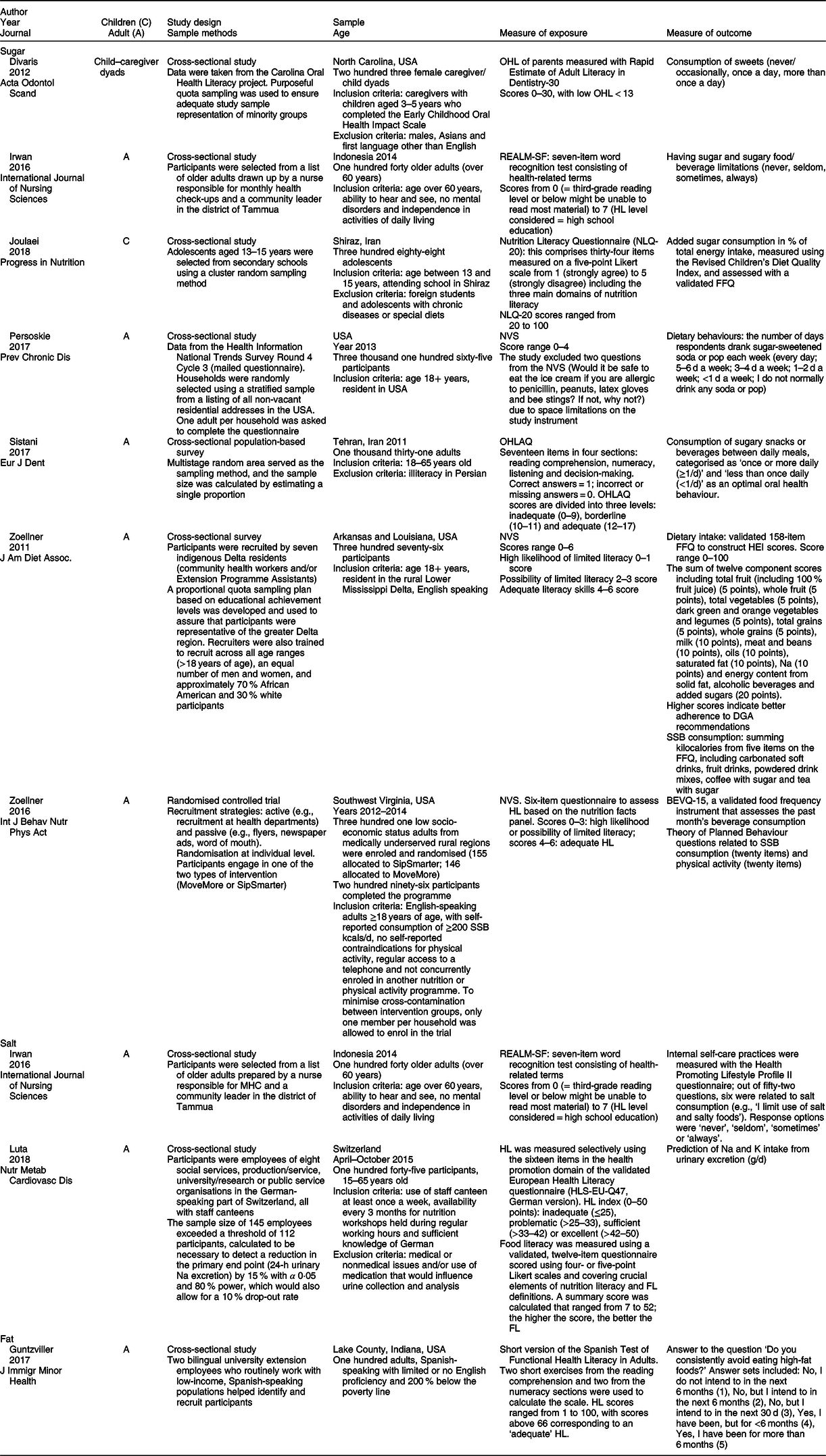
Figure 1 shows the flow chart of the article selection process for the association between sugar intake and HL. Seven articles met our inclusion criteria and were included in this review: three studies found that participants with a higher HL had a lower sugar intake, one found the same association only for boys and two found no evidence of any association.
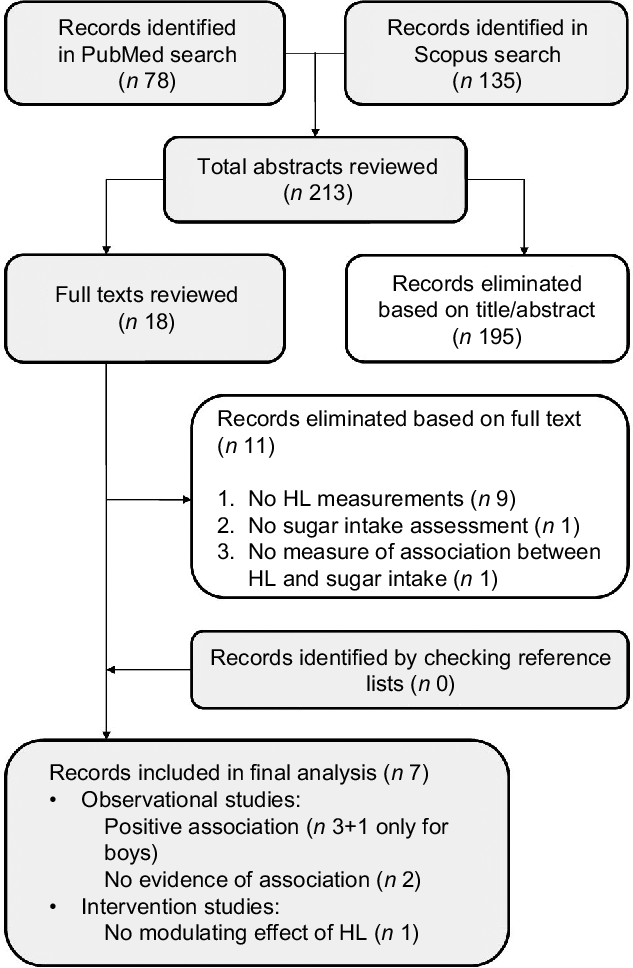
Fig. 1 Article selection process (sugar), flow chart. HL, health literacy
All three studies finding an association were conducted on adults. Two of these studies were conducted in the USA and focused specifically on sugar-sweetened beverage (SSB) consumption, using the Newest Vital Sign tool to measure participants’ HL. Using nationally representative data, Huizinga et al. (Reference Huizinga, Beech and Cavanaugh24) found that participants with a better understanding of panels reporting nutritional facts reported consuming sugar-sweetened soda fewer times a week. Their findings were consistent with those of von Elm et al. (Reference von Elm, Altman and Egger26), who reported that participants in the lowest HL category (as measured with the Newest Vital Sign tool, which measures understanding of food labels) ingested just over 100 kcal/d more from SSB than participants with an adequate HL. Each additional point in participants’ HL scores (0–6) was associated with a 34 kcal/d lower intake from SSB. The third study showing an association between a higher HL and a more limited consumption of sugar was conducted by Cha et al. (Reference Cha, Kim and Lerner25), who investigated the association between oral health-related behaviour and oral HL among Iranian adults. They considered the consumption of sugary snacks or beverages between meals, finding that higher oral HL scores correlated significantly with a lower consumption of these foods (less than once a day).
Oral HL was assessed by Naghibi Sistani et al. too(Reference Naghibi Sistani, Virtanen and Yazdani30), who investigated the association between caregivers’ oral HL and their children’s oral health-related quality of life. The authors explored whether HL modified the association between children’s oral health status and oral health-related quality of life. The study was based on data from structured interviews with female caregivers of 3- to 5-year-old children to examine deleterious oral health practices in children. Although a trend emerged, the frequency of the children’s sweet consumption was not found significantly associated with the caregivers’ level of oral HL (only bivariate distribution was performed). The only study that we found concerning adolescents (13–15 years old) estimated their eating behaviour using a validated FFQ and examined its association with nutritional literacy(Reference Zoellner, You and Connell31). This construct was investigated specifically in three aspects – functional nutrition literacy, interactive nutrition literacy and critical nutrition literacy – using the Nutrition Literacy Questionnaire (NLQ-20)(Reference Guntzviller, King and Jensen34). It emerged that a higher functional nutrition literacy was associated with a lower sugar intake in boys, while there was no evidence of such an association in girls. Sugar intake was not associated with either of the other aspects of nutritional literacy (interactive nutrition literacy or critical nutrition literacy) in either sex.
A single cross-sectional study aimed to examine self-care practices and health-seeking behaviours of older adults (over 60 years)(Reference Huizinga, Carlisle and Cavanaugh23). Various self-care practices were investigated, including the dietary intake of sugar and salt. No evidence of any association emerged between HL and a limited consumption of these elements.
The only intervention study we found was a randomised and controlled trial aiming to examine the effects of a behavioural intervention to reduce SSB intake among adults in medically underserved rural communities(Reference Schulz, Altman and Moher27). It emerged that baseline HL status did not moderate any outcomes.
Health literacy and salt intake
Figure 2 shows the flow chart of the article selection process for the association between salt intake and HL. Two cross-sectional studies were selected. Neither found any significant association between salt intake and HL. Irwan et al. (Reference Irwan, Kato and Kitaoka28) sought associations between HL, food literacy (FL) and salt awareness, on the one hand, and salt intake, K intake and Na:K ratio, on the other hand, using baseline data from a workplace intervention trial conducted in Switzerland. Na and K intakes were estimated from a single 24-h urine collection. The authors found a tendency towards a lower salt intake among the more health-literate and food-literate participants, but on multiple regression analysis, neither HL nor FL was significantly associated with salt intake, K intake or Na:K ratio. The only variable significantly associated with salt intake was food salt awareness when it came to the choice of foods.
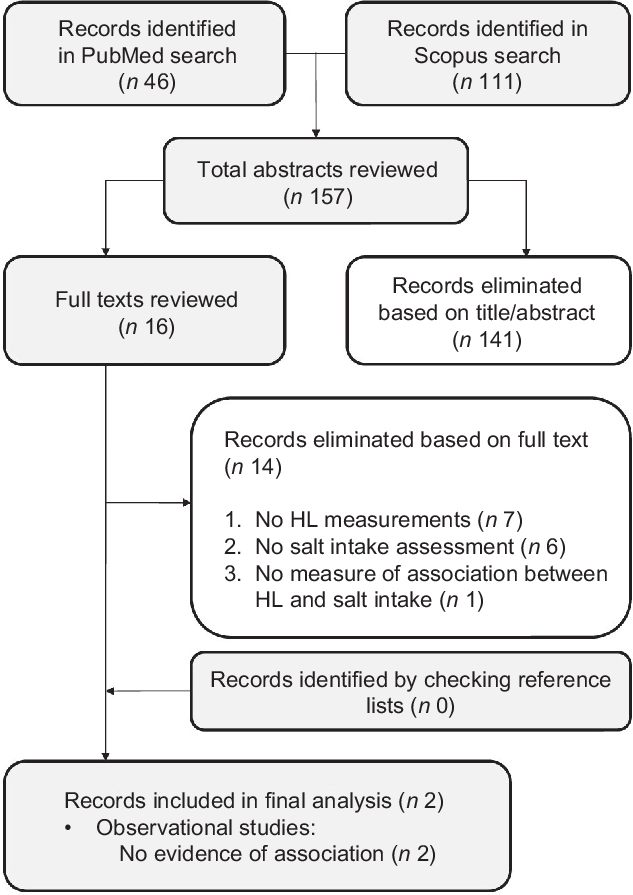
Fig. 2 Article selection process (salt), flow chart. HL, health literacy
Health literacy and fat intake
Figure 3 shows the flow chart of the article selection process for the association between fat intake and HL. The only study investigating this issue aimed to examine HL, self-efficacy and eating and exercising behaviour in a low-income Hispanic population in the USA(Reference Persoskie, Hennessy and Nelson29). The results produced no evidence of any statistically significant association between HL and the intake of fatty foods. Self-efficacy interacted with HL as regards to the three types of behaviour investigated (eating fruits and vegetables, avoiding fatty foods and exercising), but the interaction was only marginally significant for avoiding fatty foods.
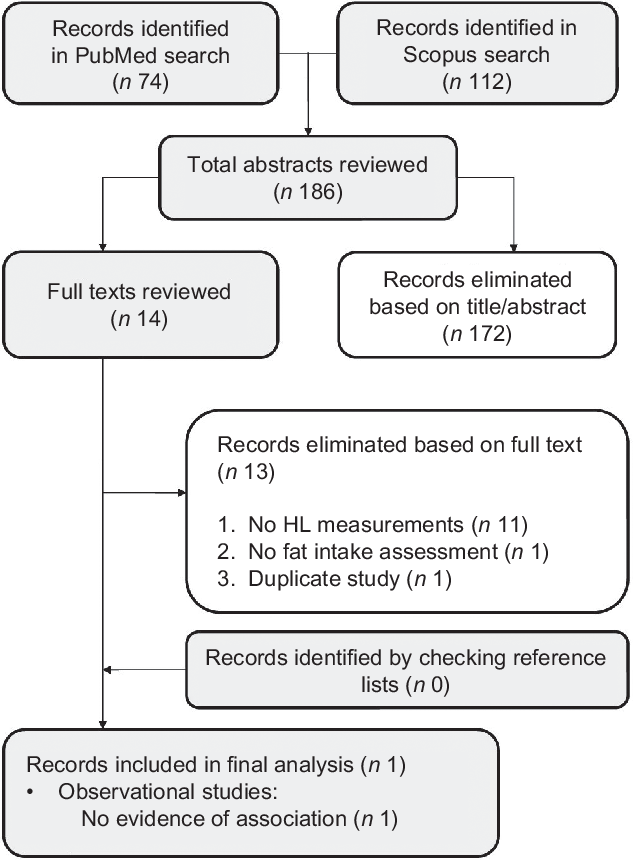
Fig. 3 Article selection process (fat), flow chart. HL, health literacy
Appendix 2 in the online supplementary material outlines the methodological quality of the studies. Overall, of the eight observational studies considered, three were of good, three of moderate and two of poor methodological quality. The single randomised controlled trial was compliant for 77 % of the items. A Cohen’s kappa of 0·66 reflected a good agreement between the two reviewers.
Discussion
Three of the six observational studies that considered sugar intake found that a greater HL coincided with a lower sugar intake, providing weak evidence of HL being a determinant of sugar intake, mainly in adults. As for salt and fat intake, our review goes to show that the evidence to support any empirical associations between HL and salt and fat is still very scanty, and no studies have found an association between HL and these nutrients to date.
Returning to the association between HL and sugar intake, the three studies revealing an association between a greater HL and a lower sugar intake (especially in the form of SSB) were conducted on adults. These findings indicate that healthier dietary practices are associated with a better understanding of food labels and suggest that HL might have a role in improving adult people’s diet. Given that SSB consumption has doubled over the past three decades in the USA(Reference Lee, Rozier and Lee38–Reference Naghibi Sistani, Montazeri and Yazdani40), the relationship between these drinks and obesity(Reference Krause, Beer-Borst and Sommerhalder41–Reference Brownell, Farley and Willett43), and the evidence of their consumption being inversely related to the level of schooling(Reference Malik, Willett and Hu44), and to HL, would warrant major targeted intervention to reverse the trends of their consumption(Reference von Elm, Altman and Egger26). This consideration would not apply to elderly people, as the only study on this age group found no association between HL and sugar intake.
While children and young adults are a core target group for HL research and practice, there are limited knowledge and academic consensus regarding the abilities and knowledge a child or young person should possess in order to make sound health-related decisions. The only study that investigated the link between nutritional literacy and eating behaviour in adolescents found that a higher nutritional literacy is associated with a lower sugar intake in boys, but not in girls(Reference Joulaei, Keshani and Kaveh36).
Only one randomised and controlled trial examined the effects of a behavioural intervention to reduce SSB intake and see if HL influenced retention, engagement or outcomes(Reference Schulz, Altman and Moher27). It emerged that baseline HL status did not moderate any of the primary or secondary outcomes, suggesting that the intervention strategies achieved much the same benefits irrespective of participants’ level of HL. In other words, health promotion interventions to improve the population’s knowledge of health-related topics can apparently overcome inequalities relating to participants’ baseline HL levels. In one systematic review of health promotion interventions targeting disease self-management conducted in 2010, only eight of the twenty-four trials analysed the modifying effect of different levels of HL, and findings were mixed regarding how much people’s level of HL influenced the effectiveness of such interventions(Reference Duffey and Popkin45).
Studies assessing HL and salt intake found no evidence of any association between the two variables(Reference Huizinga, Carlisle and Cavanaugh23,Reference Irwan, Kato and Kitaoka28) . As for HL, FL and salt awareness vis-à-vis salt intake, the only variable significantly associated with the salt intake (in one study) was food salt awareness, when it came to the choice of foods. This might seem paradoxical because applying a knowledge of salt content when choosing what food to eat is considered an advanced form of (interactive and critical) FL behaviour. It demands the ability to judge whether a food contributes to healthy nutrition and to distinguish between more healthy and less healthy options(Reference Malik, Schulze and Hu46). This requires a good functional FL, such as knowing the recommendations and being able to read and understand food labels(Reference Malik, Schulze and Hu46). The authors nevertheless conclude that, whatever the potential of HL, FL and specific salt awareness, the high Na content in processed foods may hamper consumers’ efforts to reduce their overall Na intake(Reference Irwan, Kato and Kitaoka28). In fact, previous studies have demonstrated that hedonic response to salt preference depends on a complex interplay of physiological, genetic, psychological and developmental factors and that high salt intake could be the expression of sensory and behavioural factors(Reference Beauchamp and Engelman47,Reference Leshem48) . On the other hand, an experimental study(Reference Lee, Cho and Bae49) found salt taste sensitivity unrelated to the real salt intake, whereas self-reported eating habits were associated with the actual salt intake. This would support the feasibility of limiting individuals’ salt intake effectively through education and training.
The only study based on social cognitive theory hypothesised that self-efficacy and capability (e.g., HL) may interact in influencing preventive health behaviours, such as fat intake, but found no such association. Previous studies had found that overeaters feature a strong liking or preference for fat and a strong attraction to more palatable food, the palatability consequently overriding any satiety signal being triggered by the fat(Reference Erlanson-Albertsson50). Such a scenario suggests a weak satiety response to fat. It was also demonstrated that high-fat eaters had higher levels of diet-induced thermogenesis and higher leptin levels, suggesting that some individuals stay lean on high-fat diets due to a particular genotype(Reference Blundell and Cooling51). Both these studies suggest that physiological mechanisms could explain dietary fat intake, but also in a complex interplay with psychological aspects. For instance, fat addiction could have important psychological determinants relating to motivation, depression, anxiety and reasoning that need to be carefully examined(Reference Sarkar, Kochhar and Khan52). These considerations and complex relationships should have important implications in how we interpret the influence of HL on dietary behaviour and how we devise intervention to address eating problems and promote healthy lifestyles, especially in adults(Reference Smilowitz, German, Zivkovic, Montmayeur and le Coutre53,Reference Meule54) .
Strengths and limitations
While a low HL has been linked to numerous unhealthy behaviours and poor health outcomes, this is the first study (to our knowledge) to systematically review the evidence of the association between people’s HL and their dietary intake of sugar, salt and fat – the three main elements considered in recommendations for a proper diet to prevent non-communicable diseases.
Our systematic review has a few limitations. First, the various studies adopted different tools to measure both HL and dietary intake of the elements considered, making the results difficult to compare and preventing any meta-analysis. The use of a limited number of standardised measuring tools in future studies would facilitate comparisons between international scenarios. Second, some of the samples considered in our review were drawn from particular categories of the population that might be seen as vulnerable (i.e., ethnic minorities) and may not be representative of the general population. The characteristics of the target population could influence the level of association between the variables analysed. Further studies could try to clarify the possible influence of different socio-demographic characteristics, such as age, in mediating the association between HL and health-related behaviour. We also found only one publication describing an intervention programme that enabled us to examine whether HL mediated the efficacy of a health-promoting intervention. Further studies on HL and health-related behaviour would be useful to shed more light on these topics.
Conclusion
This systematic review concerning the association between HL and the dietary intake of sugar, salt and fat revealed no evidence of any such association for salt and fat, while for sugar, the results are mixed: only about half of the studies considered found an association between a higher level of HL and a more limited sugar consumption. The hypothesised link between health promotion and education strategies and an improvement in HL – with a view to influencing intermediate outcomes such as eating habits – should be tested in further research because this first attempt to summarise the early empirical evidence is inconclusive. More work is also needed to better understand the moderating effects of HL on the outcomes of health promotion interventions.
Acknowledgements
Acknowledgements: None. Financial support: The current research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: There are no conflicts of interest. Authorship: A.B. conceptualised the study and approved the final manuscript as submitted. M.S. designed the data collection tools and approved the final manuscript as submitted. A.B., G.G., E.D. and L.M. drafted the manuscript and approved the final manuscript as submitted. V.B., C.B., S.C. and T.B. critically reviewed the interpretation of the data, revised the manuscript and approved the final manuscript as submitted. Ethics of human subject participation: Not applicable.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020002311.








