Oxidative stress is a shift in the balance of oxidants and antioxidants in favour of the former, and an increase in the intracellular levels of reactive oxidative species or inadequate levels of antioxidants can cause damage to lipids, proteins and DNA(Reference Birben, Sahiner and Sackesen1,Reference Schieber and Chandel2) . Strong evidence supports the role of oxidative stress and chronic inflammation in the development of chronic diseases(Reference Cooney, Chai and Franke3) including CVD(Reference Cervantes Gracia, Llanas-Cornejo and Husi4) and cancer(Reference Reuter, Gupta and Chaturvedi5), as well as increased risk of all-cause and cause-specific mortality(Reference Schottker, Saum and Jansen6). Dietary factors with anti-inflammatory and antioxidant properties may aid in lowering the risk of chronic diseases and mortality.
Lipid-soluble micronutrients such as vitamin A (retinol), vitamin E (tocopherols) and carotenoids are potent antioxidants with anti-inflammatory properties, with broad effects on immune function providing protection against oxidative damage(Reference Lobo, Patil and Phatak7). Several observational studies have shown that higher serum levels and/or dietary intake of carotenoids, α-tocopherol (the predominate form of vitamin E) and β-carotene were associated with reduced risk of chronic disease as well as cause-specific and all-cause mortality(Reference Aune, Giovannucci and Boffetta8–Reference Block10). However, clinical trials report no benefit of vitamins A, E or β-carotene against incidence of chronic disease or mortality(Reference Steinhubl11). A comprehensive systematic review found that higher levels of antioxidants, including β-carotene, and vitamins E and A may increase the risk of mortality(Reference Bjelakovic, Nikolova and Gluud12), suggesting the presence of non-linear relationships with a threshold of efficacy and toxicity on disease or mortality risk. To date, optimal levels of serum antioxidants for protection against disease incidence and mortality have not been fully elucidated.
The burden of chronic diseases varies by race/ethnicity in the USA, with minority populations having a generally greater burden than non-Hispanic White population, although trends are not universal(Reference Weinstein, Geller and Negussie13). As such, minority racial/ethnic groups have shorter life expectancies, higher incidence of chronic diseases and less favourable mortality outcomes than their non-Hispanic White counterparts(Reference Weinstein, Geller and Negussie13). Differential chronic inflammation and oxidative stress may contribute to these disparities. One study reported that chronic inflammatory markers such as C-reactive protein (CRP) and IL-6 were significantly higher in African Americans(Reference Morimoto, Conroy and Ollberding14), while adiponectin levels were lower when compared with their White counterparts(Reference Morimoto, Conroy and Ollberding14), suggesting increased exposure to oxidative stress and chronic inflammation in African American populations. Furthermore, ethnicity has been independently correlated with dietary micronutrient intake and serum levels, including key antioxidants in the US population(Reference Kant and Graubard15). One study found that dietary intake of vitamin C, carotenes, vitamin E, folate and iron differed by race/ethnicity, with lower intakes of vitamin E, folate and iron in non-Hispanic Blacks than in non-Hispanic Whites, and higher vitamin C and carotene intake in Mexican Americans than in non-Hispanic Whites(Reference Kant and Graubard15). A recent study reported differential use of dietary supplements across racial/ethnic groups, among non-Hispanic Whites (61 %), non-Hispanic Blacks (40 %) and Hispanics (36 %)(Reference Blumberg, Frei and Fulgoni16). Differences in chronic inflammation and oxidative stress(Reference Morimoto, Conroy and Ollberding14), dietary intake of micronutrients(Reference Rehm, Penalvo and Afshin17) and use of dietary supplements across racial/ethnic groups(Reference Blumberg, Frei and Fulgoni16) may contribute to the observed racial/ethnic disparity in mortality in the USA. Little research, however, has been conducted to assess the non-linear effects of serum lipid-soluble antioxidant levels on mortality, and even less has been done to assess the associations across racial/ethnic groups.
Using data from the National Health and Nutrition Examination Survey (NHANES) 1999–2002, we examined the hypothesis that high serum levels of lipid-soluble antioxidants may be non-linearly associated with lower risk of all-cause, cancer and CVD mortality, and the associations may vary across racial/ethnic groups.
Materials and methods
Study population and outcomes
The current study utilised data from two continuous cycles of the NHANES between 1999 and 2002, in which serum antioxidant levels were analysed. The NHANES is a cross-sectional survey under the purview of the Centers for Disease Control and Prevention, designed to assess health and nutritional status in a nationally representative sample of the non-institutionalised US population, described previously in detail(Reference Curtin, Mohadjer and Dohrmann18). In total, 10 282 adults were aged 20 years or older at the time of blood collection. Of these, 1524 participants were excluded due to pregnancy or lactation at baseline, as well as missing serum antioxidant levels. Finally, a total of 8758 participants were included in the current analysis (Fig. 1). All participants provided written informed consent, and the Institutional Review Board of the National Center for Health Statistics approved the study protocol(19).
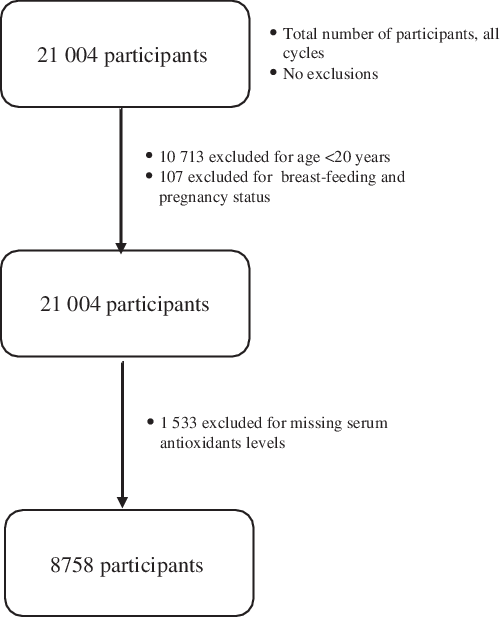
Fig. 1 Study participants flow chart
Participants were followed for mortality status from the date of Mobile Examination Center (MEC) visit until 31 December 2015. Mortality outcomes were determined using matching methods between NHANES and the National Death Index death certificate records described previously(20). Additionally, Social Security Administration, Centers for Medicare and Medicaid Services or death certificate review were used for confirmation of mortality status(20). The ninth and tenth revision of the International Statistical Classifications of Diseases, Injuries and Causes of Death (ICD-9 and ICD-10) were utilised to classify deaths from CVD (I00-I78) and cancer (C00-C97)(Reference Bramer21). All-cause mortality was classified as death from any cause.
Assessment of serum lipid-soluble antioxidants/micronutrients
Blood was drawn from participants in the MEC by phlebotomists. Serum levels of vitamin A (measured here as retinol), vitamin E (measured here as α-tocopherol and γ-tocopherol) and the six major carotenoids (α-carotene, trans-β-carotene, cis β-carotene, β-cryptoxanthin, combined lutein/zeaxanthin and trans-lycopene) were assessed by isocratic HPLC, and spectrophotometric methods were used for quantitative analysis(22). Total carotenoid levels were calculated by summing values for the six major carotenoids as described in a previous report(Reference Shardell, Alley and Hicks23). β-Carotene was calculated by summing levels of the two major components of the nutrient: cis and trans β-carotene. α-Tocopherol was calculated by subtracting γ-tocopherol from total vitamin E levels. Isoforms of the tocopherols (α and γ) were assessed independently due to their different physiological properties(Reference Cook-Mills and McCary24). Serum carotenoid levels were only assessed for the 1999–2000 cycle. Therefore, sample size for each assessed antioxidant ranged from 4633 to 8758. All serum antioxidant nutrient levels were captured in microgram per deciliter (µg/dl).
Statistical analysis
Due to the complex nature of the NHANES multistage clustered probability sampling, the ‘Survey’ procedure in SAS 9.4 software (SAS Institute) was used to estimate variance with incorporation of sampling weights in the study design. Hazards ratios (HR) and 95 % CI for the associations between serum antioxidant levels and all-cause, cancer or cardiovascular mortality were estimated from Cox proportional hazards regression models. Participants were followed until an event (death) or the end of the study period. Those without an event were censored at the conclusion of the study period (31 December 2015). Serum antioxidant nutrient levels were categorised into quartiles based upon their concentrations in the study population, using the lowest category as the reference for all antioxidants except vitamin A. Because previous studies have reported normal range of vitamin A for normal dark adaptation(Reference Ansari, Sahni and Etherington25) and a possible threshold effect of vitamin A on mortality(Reference Goyal, Terry and Siegel26), we utilised the second quartile as the reference in our analyses.
Potential confounders included in multivariable modelling were age, sex and race/ethnicity, BMI, history of CVD, cancer and diabetes, as well as alcohol use, smoking status and physical activity. Alcohol use was defined dichotomously as used within the past 12 months from time of MEC exam, yes or no. Physical activity was categorised into two strata: no and low level, and moderate and high level, defined as no vigorous or moderate physical activity in the past 30 d, and at least 10 min of sustained moderate or vigorous physical activity, respectively. Diabetes status was defined as having Hb A1C ≥ 6·5 % at the time of the MEC visit, as per the WHO guidelines(Reference Forouhi and Wareham27). Prior studies showed a relationship between CRP and mortality(Reference Zacho, Tybjaerg-Hansen and Nordestgaard28), and γ-tocopherol has been associated with CRP(Reference Saboori, Shab-Bidar and Speakman29). We examined associations with adjustment for log-transformed CRP (since it was not normally distributed in the current study); results were similar to those without adjustment for CRP. Therefore, log-transformed CRP was ultimately not included in final models. Because α-tocopherol and γ-tocopherol are lipophilic compounds transported in lipoprotein fractions in the blood, their concentration depends on total lipid serum levels(Reference Ford, Schleicher and Mokdad30). Therefore, total cholesterol to total tocopherol ratio was calculated and categorised into quartiles. Similar associations were observed when examining total cholesterol to total tocopherol ratio (data not shown) and total tocopherol levels (Vitamin E) with cause-specific and all-cause mortality; thus, the ratio was not included in final analysis. The temporal association between serum antioxidants and disease history (including CVD, cancer, liver problems and diabetes) cannot be determined due to the cross-sectional nature of the survey. In order to assess whether disease history was a mediator of the association between antioxidant serum status and mortality, separate analyses were run excluding disease history. Results were not materially changed; therefore, the history of diseases was included in final models. Supplement use was defined as a participant reporting use of a multivitamin at the time of the MEC exam. In order to avoid over adjustment of the potential association of antioxidant serum status with mortality, and because inclusion of this covariate did not alter our findings, we did not include supplement use in our final models. Because total daily energetic intake and season of MEC visit did not alter our findings, we chose not to retain them in our final models. Serum antioxidant levels were compared with characteristics using the non-parametric Wilcoxon rank sum test. To test our hypothesis that the associations of serum antioxidants on mortality may vary by race/ethnicity, we analysed these associations within strata of race/ethnicity. Interaction between serum antioxidant nutrients and race/ethnicity was tested in the Cox regression model by evaluating a multiplicative term using the Wald test (data not shown). Sensitivity analyses were conducted after excluding participants who died within 2 years of blood collection; however, results did not change materially (data not shown). Tests for dose–response relationship were estimated by fitting models with exposure variables included as continuous variables for all serum antioxidants in the overall study population and stratified by race/ethnicity (data not shown). All reported P-values were two-tailed, and statistical significance was set at 0·05. R-Studio was used to visualise relationships of serum antioxidants and all-cause mortality stratified by race/ethnicity.
Results
Of the 8758 subjects included in the study, 2083 died (1151 men and 932 women) during a median follow-up time of 14·2 years. Three hundred and forty-five deaths were due to CVD, and 429 deaths were due to cancer. Table 1 presents the baseline serum antioxidants levels by demographic and selected lifestyle factors.
Table 1 Serum antioxidant nutrient levels among adults ≥ 20 years, NHANES 1999–2002
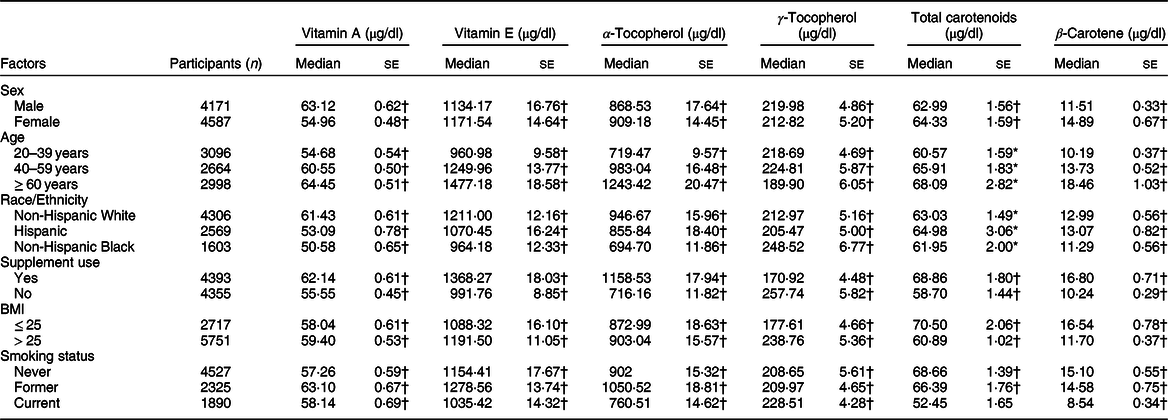
NHANES, National Health and Nutrition Examination Survey.
Participant column total reflects total number of possible participants which varies by antioxidant nutrient level availability.
Wilcoxon rank test revealed significance at *P < 0·05 or †P < 0·01.
Associations of serum levels of lipid-soluble antioxidant micronutrient levels with all-cause, CVD and cancer mortality after adjustment for age at blood collection, race/ethnicity and other potential confounders are presented in Table 2. For total vitamin E, compared with participants in the lowest quartile, those in the highest quartile had an increased risk of all-cause mortality (HR = 1·22, 95 % CI 1·04, 1·43), and those in the second quartile were also associated with an increased risk of all-cause mortality (HR = 1·22, 95 % CI 1·00, 1·49). Similarly, there was a suggestion of a positive association between high α-tocopherol level and all-cause mortality; however, results were not statistically significant. Compared with the first quartile, the second and highest quartile of serum total carotenoid levels tended to be associated with lower risk of all-cause mortality, but none of these associations were statistically significant. There were no associations of serum vitamin A, γ-tocopherol and β-carotene levels with all-cause mortality. Furthermore, no associations between the antioxidants analysed and risk of CVD or cancer mortality were observed for the overall study population. Additionally, no linear trends were observed in the overall study population.
Table 2 All-cause and cause-specific mortality and serum antioxidant level, NHANES 1999–2002*
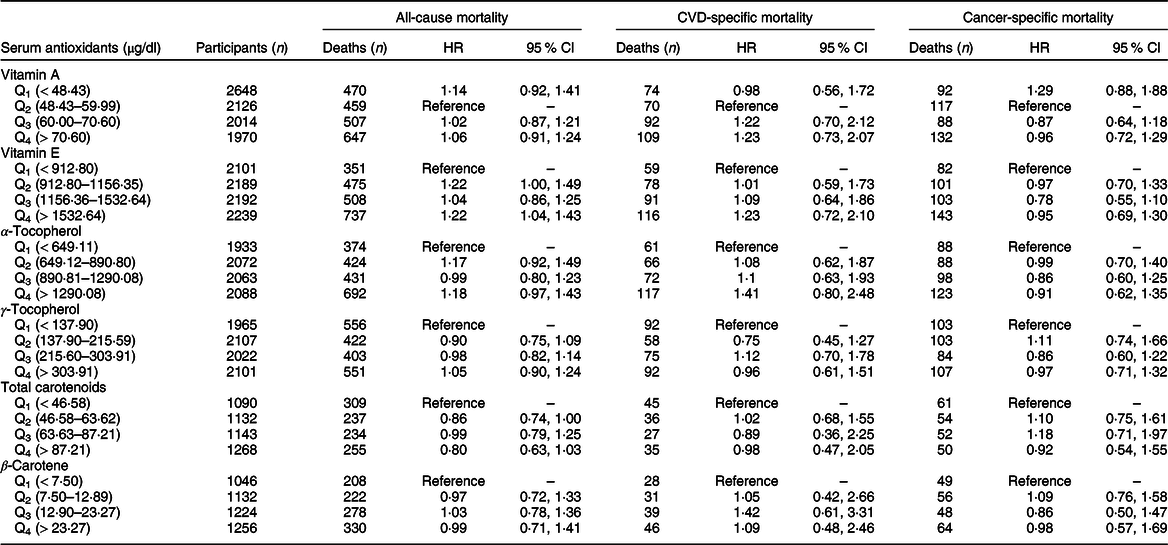
NHANES, National Health and Nutrition Examination Survey.
* All analyses were adjusted for age, sex, race/ethnicity, smoking status, alcohol use, physical activity level, BMI, history of CVD, cancer, liver problems and diabetes.
We further conducted stratified analyses for associations of serum antioxidants with all-cause mortality by race/ethnicity (Table 3). For total vitamin E, the positive association with all-cause mortality remained significant among non-Hispanic Whites (HR = 1·37, 95 % CI 1·15, 1·63, highest v. lowest quartile, P trend < 0·01), while non-Hispanic Blacks with total vitamin E concentrations in the third quartile showed suggestions of reduced risk (HR = 0·71, 95 % CI 0·48, 1·07). Similar patterns of association were observed for serum α-tocopherol levels (HR = 0·66, 95 % CI 0·42, 1·03, third v. lowest quartile) among non-Hispanic Blacks. Serum levels of antioxidants were not associated with risk of all-cause mortality among Hispanics. Figure 2 showed U-shaped associations between serum levels of vitamin E, α-tocopherol and all-cause mortality among non-Hispanic Blacks, with significant reduction in risk in the third quartile. Additionally, although suggestions of linear associations with all-cause mortality were observed among non-Hispanic Blacks, tests for trend revealed no significance for serum total carotenoids (P trend = 0·08) and γ-tocopherol levels (P trend = 0·08). No linear associations were observed for other antioxidants and all-cause mortality in race/ethnicity stratified analysis.
Table 3 All-cause mortality and serum antioxidant level by race/ethnicity, NHANES 1999–2002*
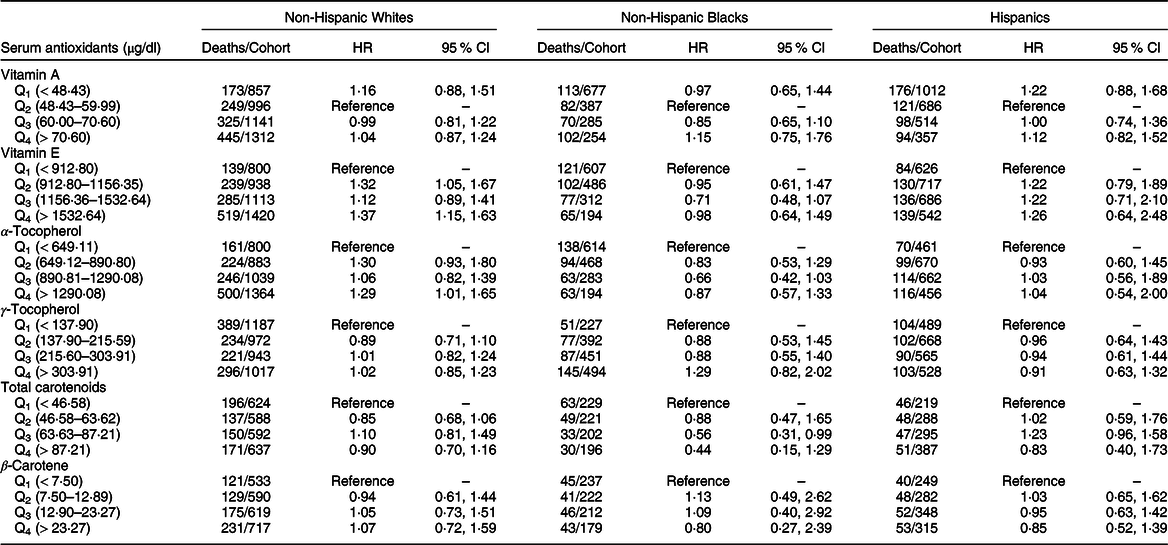
NHANES, National Health and Nutrition Examination Survey.
* All analyses were adjusted for age, sex, smoking status, alcohol use, physical activity level, BMI, history of CVD, cancer, liver problems and diabetes.
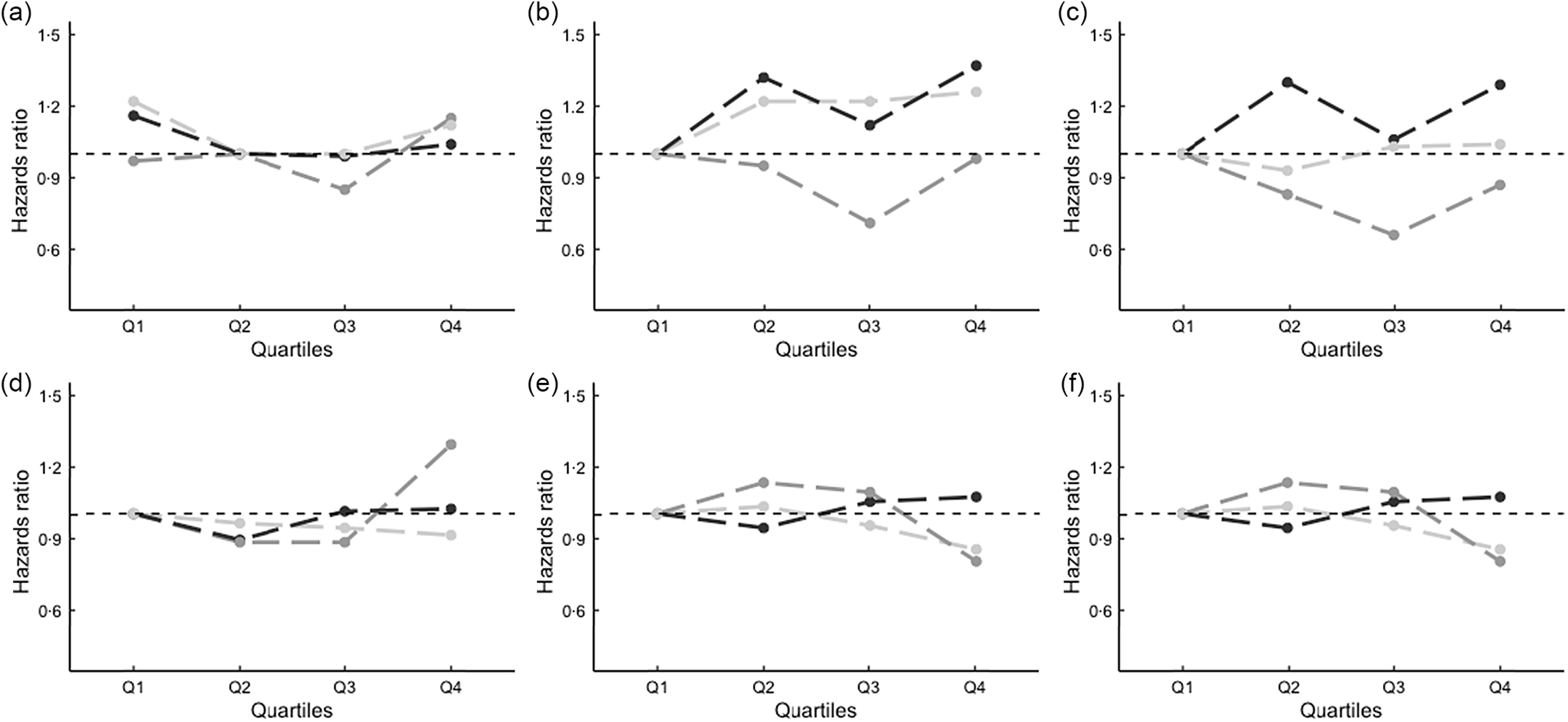
Fig. 2 Lipid-soluble antioxidants serum levels and all-cause mortality by race/ethnicity*.*Interaction tests were performed evaluating a multiplicative term using the Wald test. (a) Vitamin A, (b) vitamin E, (c) α-Tocopherol, (d) γ-Tocopherol, (e) total carotenoids, (f) β-carotene. NH, non-Hispanic; ![]() , NH White;
, NH White; ![]() , NH Black;
, NH Black; ![]() , Hispanic
, Hispanic
Results for cancer and CVD mortality, stratified by race/ethnicity, are presented in online supplementary material, Supplemental Tables 1 and 2, respectively. Among non-Hispanic Blacks, the highest quartile of serum total vitamin E and third quartile of serum α-tocopherol levels were inversely associated with cancer mortality, when compared with the lowest quartiles (total vitamin E: HR = 0·46, 95 % CI 0·21, 1·00, P trend < 0·01, and α-tocopherol: HR = 0·30, 95 % CI 0·12, 0·75, P trend < 0·01). There was suggestion of an inverse association between high total carotenoid levels and cancer mortality among non-Hispanic Blacks; meanwhile; for CVD mortality, the pattern of association was similar, with the second quartile of total carotenoids showing an inverse association with CVD mortality (HR = 0·26; 95 % CI 0·07, 0·97). The second and highest quartiles of serum β-carotene were associated with lower risk of CVD mortality (HR = 0·38; 95 % CI 0·16, 0·88; HR = 0·05; 95 % CI 0·01, 0·38, respectively) among Hispanics when compared with the lowest quartile, and the test for trend was statistically significant (P trend < 0·01). There were no significant differences in the risk of cancer or CVD mortality for different levels of serum antioxidants among non-Hispanic Whites. There were no significant interactions between serum antioxidant levels and race/ethnicity in relation to all-cause mortality, CVD mortality or cancer mortality.
Discussion
Utilising a representative sample of US adults, we found that serum antioxidant levels related to mortality, but the associations differed by race/ethnicity, and were non-linear for all-cause and cause-specific mortality. To our knowledge, few studies have examined the associations of serum antioxidant levels with mortality by race/ethnicity, and limited research has examined non-linear associations with mortality(Reference Goyal, Terry and Siegel26).
Vitamin E is a chain-breaking antioxidant with the function of preventing propagation of free radical reactions; it is primarily composed of α- and γ-tocopherol, with higher concentrations of α-tocopherol than any other tocopherol in serum(Reference Wright, Lawson and Weinstein31). Furthermore, γ-tocopherol inhibits cancer cell progression and proliferation(Reference Wright, Lawson and Weinstein31) and may play a role in CVD prevention through the decrease of lipid peroxidation, platelet accumulation and monocyte proatherogenic effects, to name a few(Reference Kaul, Devaraj and Jialal32). The mechanisms through which vitamin E acts to prevent disease remain to be fully elucidated. The Institute of Medicine has identified a concentration of 5·16 µg/ml (516 µg/dl) of α-tocopherol as sufficient to prevent acute vitamin E deficiency, while pointing out the need for more research to determine the levels and types of tocopherols important for optimal nutritional status and their mechanisms in chronic disease prevention(33). In our population, which consisted of over 50 % non-Hispanic Whites, we found that high total vitamin E or α-tocopherol concentration was associated with increased risk of all-cause mortality, although no dose–response relationships were observed. These patterns of association were similar only among non-Hispanic Whites. A recent Mendelian randomisation of subject of predominantly European ancestry found non-linear associations of circulating vitamin E levels with risk of coronary artery disease and myocardial infarction and reported significant increase in the risk of coronary artery disease and myocardial infarction for those with higher circulating levels of vitamin E(Reference Wang and Xu34), which may support our findings among non-Hispanic Whites. Consistent with previous studies(Reference Goyal, Terry and Siegel26,Reference Ford, Schleicher and Mokdad30) , we observed U-shaped curves in the association of total vitamin E or α-tocopherol levels with all-cause mortality among non-Hispanic Blacks, with greatest reductions in mortality risk with serum vitamin E at 1156·35–1532·64 µg/dl or α-tocopherol at 890·81–1290·08 µg/dl, comparable to previously reported optimal ranges(Reference Ford, Schleicher and Mokdad30). Additionally, total vitamin E concentrations were inversely associated with cancer mortality in the linear dose–response analysis among non-Hispanic Blacks.
Variations in associations of total vitamin E and α-tocopherol with risk of mortality across different racial/ethnic groups may be explained, partially, by differences in serum concentrations of these micronutrients. In our study, serum total vitamin E and α-tocopherol levels were considerably higher among non-Hispanic Whites than non-Hispanic Blacks and Hispanics, and the prevalence of vitamin E deficiency was higher in the two minority groups. Differences in dietary intake of vitamin E might contribute to the observed variations in serum vitamin E levels between non-Hispanic Whites, non-Hispanic Blacks and Hispanics(Reference Kant and Graubard15). Supplement use also mirrored serum α-tocopherol deficiency, with highest use among non-Hispanic Whites (62 %) followed by Hispanics (38 %) and non-Hispanic Blacks (37 %), suggesting that use of dietary supplements may be necessary in inadequate populations to prevent mortality. It is possible that over-supplementation may have contributed, at least partially, to the observed positive association between vitamin E or α-tocopherol and all-cause mortality among non-Hispanic Whites in our study, suggesting the potential harms of over-supplementation(Reference Miller, Pastor-Barriuso and Dalal35). Future studies are warranted to confirm these findings and to elucidate the underlying mechanisms for racial/ethnic differences in the relationships between total vitamin E levels, α-tocopherol and mortality.
With respect to γ-tocopherol, a recent report found positive associations for serum γ-tocopherol with all-cause, cancer and CVD-specific mortality in the overall population and among all-cause mortality in Whites, with suggestions of a positive association among non-Hispanic Blacks(Reference Chai, Maskarinec and Franke36). Similar patterns of association among non-Hispanic Whites and non-Hispanic Blacks were observed in our study, although associations were not statistically significant. This inconsistency could be the result of overall higher γ-tocopherol levels in our study population, possibly due to significant age differences between the two populations considering that serum γ-tocopherol levels may decrease with older age(Reference Chai, Novotny and Maskarinec37). Potential differences in physiological properties and functions of α- and γ-tocopherol could further complicate the interpretation of our observed results.
Blood carotenoids are a reliable biomarker of usual intake of fruits and vegetables(33,Reference Burrows, Rollo and Williams38) . Carotenoids can reduce damage from reactive oxidative species, inhibit lipid peroxidation and are involved in cellular communications that regulate proliferation and apoptosis(Reference Dutta, Surapaneni and Bansal39,Reference Tapiero, Townsend and Tew40) . Inverse associations between dietary or circulating levels of carotenoids and mortality have been previously observed(Reference Shardell, Alley and Hicks23,Reference Agudo, Cabrera and Amiano41) , suggesting the potential benefits of carotenoids for optimal health and prevention of disease. In our study, we did not observe a strong protective association for serum carotenoid levels with all-cause mortality. However, there appeared to be threshold effects in the non-Hispanic Black population, in which reduced risk of CVD mortality was observed for total carotenoid levels between 46·58 and 63·62 µg/dl. This observation is in concordance with a study(Reference Shardell, Alley and Hicks23) that reported incremental benefits of serum total carotenoid levels in relation to mortality that plateaued at 1·0 mmol/l (~53·73 µg/dl). Furthermore, our results were similar to another study that found non-linear relationships for serum carotenoid levels with risk of mortality among colorectal cancer patients(Reference Cooney, Chai and Franke3). In our study, among Hispanics, an inverse association between the second and highest quartiles of serum β-carotene level with CVD mortality was observed. However, carotenoid levels were only assessed in one cycle; thus, cause-specific mortality was low in stratified analysis and results should be interpreted cautiously. Future studies with larger representation of minority populations are necessary to validate our findings. Finally, other factors likely influence the absorption, transportation, storage and utilisation of carotenoids. Lower levels of serum carotenoids have been observed among smokers(Reference Chow, Thacker and Changchit42) and obese individuals(Reference Chai, Conroy and Maskarinec43), both of which increase chronic inflammation and oxidative stress(Reference van der Vaart, Postma and Timens44,Reference Keaney, Larson and Vasan45) , and may lead to increased mobilisation of these antioxidants. Physiological relationships between inflammation, oxidative stress, carotenoids and mortality risk, as well as differences between racial/ethnic populations must be investigated in future studies, particularly minority populations.
The strengths of the current study include a nationally representative sample of the USA, large sample size and long follow-up time, which enabled us the power to detect relatively weak associations and further assess associations by race/ethnicity. Rigorous methods utilised by the NHANES for obtaining mortality status reduce the chances of information bias influencing results. Several limitations must be mentioned. The use of one serum sample limited our ability to assess the impact of long-term antioxidant levels on mortality. Furthermore, the use of a single measurement for serum antioxidant level may have misclassified exposures for some participants, attenuating risk estimates; however, serum levels of tocopherol, total carotenoids and β-carotene measured 2–4 weeks apart showed good stability (correlation ranging from 0·79 to 0·84)(Reference Block, Dietrich and Norkus46). Another limitation secondary data analysis is that cause-specific events were defined broadly in the study population. These cause-specific outcomes (e.g., CVD, cancer) possess heterogeneous mechanisms which we were unable to assess in the current study. In addition, the distribution of all-cause and cause-specific mortality likely differs across racial/ethnic groups for reasons other than inflammation, and race/ethnicity specific analysis may have masked relationships linking antioxidant serum status to inflammation-related cause of death. Furthermore, our population was younger than most cohorts assessing these associations; thus, average follow-up of 14 years may have been insufficient to detect effects if the primary benefit of antioxidants is to extend life expectancy or slow progression of disease in its earliest stages. Additionally, we have baseline information for potential confounders but no information on those factors over the follow-up period. We cannot rule out that we did not have enough power to detect weak associations in some strata. Further, the imbalanced and relatively small number of participants in each racial/ethnic group likely influenced the subgroup specific findings.
In summary, we found that over a certain level, there was no additional benefit of higher serum concentrations of certain lipid-soluble antioxidants on overall survival. We found that the associations of serum antioxidant levels and mortality may differ between racial/ethnic groups, suggesting race/ethnicity-specific thresholds. In the current study, particularly, for total vitamin E, α-tocopherol and total carotenoids, there were different thresholds for the associations with all-cause or cause-specific mortality across racial/ethnic groups. Studies with greater representation of minority populations and longer follow-up are warranted to confirm these findings.
Acknowledgements
Acknowledgements: The authors thank the investigators, the staff and the participants of NHANES for their valuable contribution. Financial support: Dr. Tao’s effort was partially supported by the National Institute on Minority Health and Health Disparities of the National Institute of Health under Award U54MD006882. Conflict of interests: No potential conflicts of interests were disclosed. Authorship: N.C.P. conducted statistical analyses and wrote the manuscript; W.C. and R.V.C. contributed to data interpretation and the critical review of the manuscript and M.-H.T. designed the study, supervised the study process and wrote the manuscript. Ethics of human subject participation: The current study was conducted according to the guideline laid down in the Declaration of Helsinki, and all procedures involving research study participants were approved by the Institutional Review Board of the National Center for Health Statistics (NCHS). All participants provided written informed consent.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020004619








