The increasing prevalence of obesity worldwide is a major public health concern(1, 2). Longitudinal studies show a direct association between increase in BMI and changes in most of the established risk factors for CVD(Reference Jousilahti, Tuomilehto and Vartiainen3, Reference Lamon-Fava, Wilson and Schaefer4). It has also been shown that weight gain, as a risk factor for other disease development, is a characteristic not only of adults but also of children and adolescents(2). The tendency of overweight children and adolescents to remain overweight throughout adulthood renders them a population more vulnerable to earlier onset of cardiovascular problems.
To reverse the ongoing obesity epidemic, it is important to access lifestyle determinants of BMI and its increase over time. Some cross-sectional(Reference Jeffery, Forster and Folsom5–Reference Jacobsen and Thelle8) and a few longitudinal(Reference Sundquist and Johansson9, Reference Wilsgaard, Jacobsen and Arnesen10) studies have addressed the association between BMI and lifestyle factors. Among them, breakfast consumption habits have been shown to be strongly related to overweight and obesity(Reference Cho, Dietrich and Brown6, Reference Ma, Bertone and Stanek11–Reference Van der Heijden, Hu and Rimm13). In addition, persons who consume low-energy breakfast or no breakfast at all have been shown to have higher cholesterol levels, and this applies to both adults and children(Reference Resnicow14). Moreover, a few studies have shown that breakfast skipping could be part of a constellation of other health-compromising behaviours that compound the many deleterious effects of obesity on health(Reference Revicki, Sobal and Deforge15–Reference Burke, Milligan and Beilin19).
Eating patterns, as well as smoking, physical activity and alcohol consumption habits, develop during adolescence and follow through to adulthood, when changing deeply ingrained habits becomes increasingly difficult. Adolescence, therefore, is a critical time to encourage the development of health-promoting behaviours.
On these grounds, our objective was to determine (i) the percentage of Greek adolescents who skip breakfast, (ii) the relationship between breakfast consumption and BMI in Greek adolescents and (iii) the interrelationship between breakfast skipping and other health-compromising behaviours, such as smoking, alcohol consumption and leading a sedentary life, in Greek adolescent boys and girls.
Materials and methods
The present study was part of a nationwide, cross-sectional, epidemiological study designed to estimate the prevalence of obesity in the entire Greek population. The survey was conducted from February to June 2003 by physical training instructors of the school who were trained in how to take body measurements by experienced doctors, all members of the Hellenic Medical Association of Obesity, with the approval and collaboration of the Greek Ministry of Education(Reference Kapantais, Tzotzas and Ioannidis20).
Sample selection
The methodology for the study was previously described(Reference Kapantais, Tzotzas and Ioannidis20, Reference Tzotzas, Kapantais and Tziomalos21). The population studied consisted of adolescent pupils aged 13–19 years from public schools throughout Greece, including the islands. Secondary schools representing various social classes were included in the selected sample. The selection method used was proportionate stratified random sampling (SRS).
From among the 3514 public secondary schools, a sample of 332 (9·45 %) was randomly selected. In each school, according to SRS, all the pupils from four out of six classes participated in the study. All adolescents in the survey were measured and completed a questionnaire at their respective schools(Reference Tzotzas, Kapantais and Tziomalos21).
Procedure
Study approval was obtained from local and state school authorities. Student and parental consent was obtained based on whether the questionnaires were completed. Physical training instructors of the school were responsible for conducting the survey after being given training and standardised criteria by doctors of the Hellenic Medical Association for Obesity. Adolescents aged 13–19 years who were living in the same household but not attending the same schools as other participants were invited to their siblings’ school to have measurements taken with the aid of gym instructors. This group comprised < 3 % of all adolescents.
The initial sample included 16 578 adolescents, and from this sample 14 454 (6676 boys and 7778 girls) entered the study. Reasons for exclusion from the study were missing values or reporting of aberrant values in measurements, incomplete questionnaires or unreliable answers.
Adolescents had direct measurements taken for height and weight and completed a self-reported paper questionnaire. The questionnaire consisted of questions regarding breakfast consumption, both qualitative and quantitative, as well as questions regarding their ethnic origin (Greek, non-Greek), their smoking and drinking habits and their physical activity during leisure time, which was estimated through the hours spent walking, exercising and watching television (TV) each week. The questionnaire was pre-tested in a large school in Athens.
Regarding drinking habits, grams of ethanol consumed per week were calculated from the reported number of glasses of wine, beer and spirits per week, according to the alcoholic degree of each beverage (12 % for wine, 5 % for beer and 40 % for spirits).
Participants who reported that they did not eat anything for breakfast (or only reported occasionally eating breakfast, i.e. less than two times a week) constituted the ‘breakfast skipping’ group. All the remaining participants constituted the ‘breakfast consumption’ group. Participants were asked whether they classed themselves as smokers (yes/no). Adolescents who responded with ‘no’ to this question were defined as non-smokers, compared with those responding with ‘yes’ who were defined as smokers. They were also asked individually (i) whether they watched TV; (ii) whether they exercised; (iii) whether they walked; and (iv) whether they played computer games. All these questions could be answered with a ‘yes’ or ‘no’. If participants answered ‘yes’ to any of the aforementioned activities, they were also required to report how many hours per week they engaged in that activity.
Measurements
Weight was measured to the nearest 0·1 kg using the same kind of portable weight scale (Terraillon T 715; Terraillon France, Chatou, France) and with the participants in minimal clothing. Height was measured to the nearest 0·1 cm, without shoes, using a stadiometer (Seca 220; Seca, Columbia, SC, USA).
Statistical analysis
Age and BMI are expressed as mean and sd. The χ 2 test was used to analyse the differences in behaviours. To compare quantitative characteristics, we used a t test, where applicable, or a non-parametric (Wilcoxon) test. In addition, a logistic regression was used to test which behaviours can predict breakfast skipping. All P values were two-tailed. Results were considered significant at P < 0·05. Statistical analyses were carried out using the Statistical Package for the Social Sciences statistical software package version 11·5 (SPSS Inc., Chicago, IL, USA).
Results
Mean BMI values for adolescent boys and girls were 22·1 (sd 3·9) kg/m2 and 21·1 (sd 3·4) kg/m2, respectively. Table 1 describes in more detail the demographic values for each group, as well as the ethnicity of the two groups (males v. females). A t test was conducted and significant differences in BMI were found between boys and girls, t (2,14 452) = −16·653 (P < 0·001), with boys having higher BMI.
Table 1 Characteristics of the adolescents studied
Further findings showed significant differences between genders in the percentage of smokers (χ 2(2,1) = 20·18, P < 0·001; Fig. 1) and consumption of alcohol (χ 2(1,1) = 205·05, P < 0·001; Fig. 1). Furthermore, some minor, not statistically significant, gender differences were found in the following behaviours: walking habitually (71·1 % boys v. 72·3 % girls, P > 0·05), exercising systematically (37·9 % boys v. 35·8 % girls, P > 0·05) and watching TV regularly (97·7 % boys v. 97·8 % girls, P > 0·05).
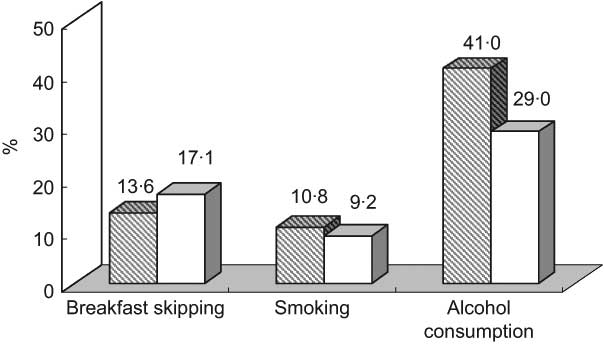
Fig. 1 Health-influencing habits among Greek adolescents (![]() , boys;
, boys; ![]() , girls)
, girls)
As shown in Table 2, breakfast consumers had a lower BMI than breakfast skippers in Greek adolescent boys (t (2,6498) = 9·273, P < 0·001). Analogous significant results were found in female breakfast consumers; they had lower BMI than breakfast skippers (t (2,7776) = 9·369, P < 0·001).
Table 2 BMI and lifestyle parameters of both breakfast consumers and skippers among Greek adolescent boys and girls

There were significant gender differences in breakfast skipping, with boys being more likely to consume breakfast than girls (χ 2 = 33·8, P < 0·001). The rate of breakfast skipping was also found to be higher in older ages in both sexes: 14·1 % of girls at 13–14 years old skip breakfast v. 18·8 % and 18·7 % of girls at 15–16 and 17–19 years old, respectively (χ 2 = 27·74, P < 0·001). In boys, the breakfast skipping rate was found to be 9·8 % in the younger ones (13–14 years old), 14·3 % in the middle age group (15–16 years old) and 17·2 % in the older age group (17–19 years old; χ 2 = 50·29, P < 0·001). The difference in the breakfast skipping rate between boys and girls was most obvious in the younger adolescents and decreased from the younger to the older ages: 14·1 % of girls v. 9·8 % of boys in the younger age group skipped breakfast (χ 2 = 21·78, P < 0·001). This difference remained in the middle age group: 18·8 % of girls v. 14·3 % of boys at the age of 15–16 years skipped breakfast (χ 2 = 17·31, P < 0·001). In the older adolescents, however, no statistically significant difference was found in the breakfast skipping rate between the sexes: 18·7 % of girls v. 17·2 % of boys were breakfast skippers.
Regarding the impact of ethnicity on BMI and breakfast habits (Table 3), it was found that Greek boys had significantly higher BMI than non-Greek boys (t (2,6465) = −3·317, P < 0·001), although they did not differ in breakfast consumption (χ 2 = 0·186, P > 0·05). Contrary to boys, no difference was found in BMI between Greek and non-Greek girls (t (2,237*552) = −1·170, P > 0·05), and no significant difference was found in breakfast consumption (χ 2 = 2·511, P > 0·05).
Table 3 Nationality, BMI and breakfast habits of adolescent boys and girls

Focusing on our initial target, the relationship between breakfast consumption habits and health-compromising behaviours in Greek adolescents, we found that among boys, breakfast skippers were significantly more likely to smoke than breakfast eaters (χ 2 = 29·71, P < 0·001; Table 2, Fig. 2). Moreover, the number of cigarettes smoked per day in male smokers was significantly higher among those who skipped breakfast than in breakfast consumers (t = 5·815, P < 0·001; Table 3). Similarly, among girls, breakfast skippers were significantly more likely to admit to smoking compared with breakfast eaters (χ 2 = 15·16, P < 0·001; Table 2, Fig. 1). In contrast to boys, however, there was no significant difference in the severity of smoking among female smokers who consumed breakfast regularly v. those who skipped breakfast (Table 4).
Table 4 Intensity of lifestyle parameters of both breakfast consumers and skippers among Greek adolescents
As already mentioned, another important health-compromising behaviour studied was alcohol consumption. It was found that male breakfast skippers were significantly more likely to admit to drinking alcohol compared with breakfast consumers (χ 2 = 10·7, P < 0·001; Table 2, Fig. 2). Moreover, weekly alcohol consumption (ethanol in grams per week) in adolescent boys who admitted to drinking was significantly higher among those who skipped breakfast compared with those who ate breakfast (Table 3). Among adolescent girls, there was no significant difference in alcohol consumption between breakfast consumers and breakfast skippers (χ 2 = 3·29, P < 0·071; Table 2, Fig. 2). However, weekly alcohol consumption in girls who admitted to drinking was significantly higher among those who skipped breakfast compared with those who ate breakfast (t = 2·575, P < 0·05; Table 3).
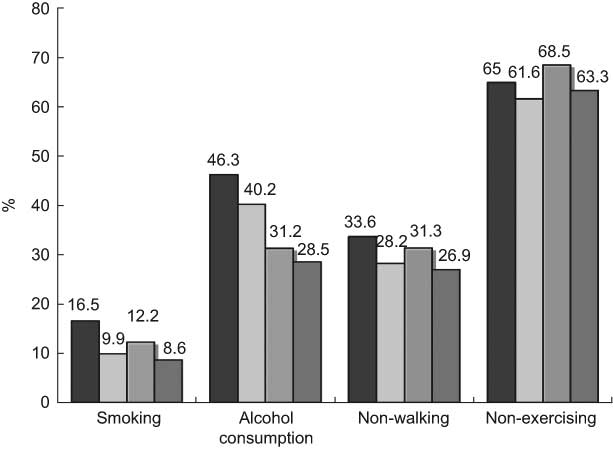
Fig. 2 Health-compromising behaviours in Greek adolescents according to breakfast habits (![]() , skipping boys;
, skipping boys; ![]() , consuming boys;
, consuming boys; ![]() , skipping girls;
, skipping girls; ![]() , consuming girls)
, consuming girls)
To further investigate the relationship between breakfast consumption and lifestyle (sedentary or more active), we analysed the answers to questions regarding leisure-time activity as this could be estimated through walking, exercising and TV watching habits, and the results were as follows. Regarding habitual walking, boys who ate breakfast were significantly more likely to give a positive answer to walking than breakfast skippers (χ 2 = 10·93, P = 0·001; Table 2). Hours spent walking per week, however, did not differ significantly between breakfast consumers and breakfast skippers in the subgroup of boys who answered positively in this respect (Table 4). Adolescent girls who ate breakfast were significantly more likely to report a positive answer to habitual walking in leisure time than those who skipped breakfast (χ 2 = 10·66. P < 0·001; Table 2). As was the case with boys, hours spent walking per week did not differ significantly between breakfast eaters and breakfast skippers in the subgroup of girls who answered positively to walking (Table 4).
Regarding the habit of regular exercise, although there were no significant differences between boys who ate breakfast v. breakfast skippers, boys who ate breakfast reported that they exercised more than those who skipped breakfast (χ 2 = 3·79, P < 0·05; Table 2). Furthermore, there was no significant difference in the hours spent per week on exercise between breakfast consumers and breakfast skippers in boys who answered positively to exercising (Table 4). In contrast, adolescent girls who ate breakfast regularly exercised more than did breakfast skippers (χ 2 = 12·84, P < 0·001; Table 2). However, there was no significant difference in hours of gym attendance per week between breakfast consumers and breakfast skippers in the subgroup of girls who answered positively to exercising (Table 4).
When it came to TV watching habits, there was no significant difference with respect to breakfast consumption in adolescent boys (Table 2). Likewise, a majority of adolescent girls watched TV regularly irrespective of breakfast habits (χ 2 = 2·12, P > 0·05; Table 2). However, in the subgroup of girls who watched TV, the number of hours spent in watching TV per week differed significantly between breakfast eaters and breakfast skippers (t = 4·506, P < 0·001; Table 4).
Many Greek adolescent boys and even more girls felt the need to control their weight through dieting; 21 % of adolescent boys and 44 % of adolescent girls had already experienced at least one dieting effort in the past, while 11 % of boys and 23 % of girls were on a diet at the time of the study. Regarding the relationship between dieting and breakfast consumption, it was found that 87 % of adolescent boys who had never been on a diet in the past ate breakfast significantly more regularly compared with 82 % of those who had gone on a diet previously (χ 2 = 22·75, P < 0·00; Fig. 3). The results for adolescent girls were analogous, since 85 % of those who had never been on a diet ate breakfast more regularly than only 79 % of those who had been on a diet (χ 2 = 47·99, P < 0·001; Fig. 3).
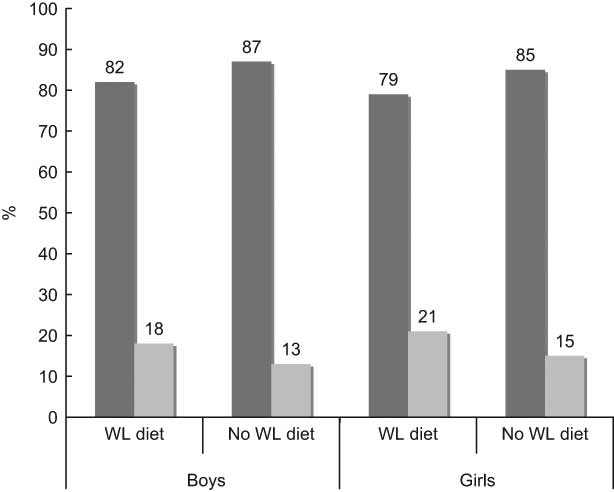
Fig. 3 Greek adolescents’ breakfast habits according to weight loss (WL) diets in the past (![]() , breakfast consuming;
, breakfast consuming; ![]() , breakfast skipping)
, breakfast skipping)
Finally, a logistic regression was conducted for both boys and girls; a cluster of behaviours that were examined earlier (e.g. smoking, TV, walking, exercise, alcohol consumption, diet attempts) was entered to predict breakfast skipping. In girls, after an initial analysis was performed, all the non-significant predictors were removed from the model. Four predictors remained in the second analysis. These were the hours spent in the gym (Wald = 5·16, P < 0·05), the hours of TV watched (Wald = 21·563, P < 0·001), the number of diets attempted in the past (Wald = 45·928, P < 0·001) and weekly ethanol consumption (Wald = 6·8, P < 0·05). The model was significant with χ 2 = 82·19, df = 4, P < 0·001. The −2 log likelihood (LL) was 6742·72 and the Cox and Snell R 2 was 0·011, which means that 1·1 % of the variance was explained. This means that spending more hours in the gym, fewer hours of watching TV, fewer previous dieting attempts and lower alcohol consumption are significant predictors of breakfast eaters in adolescent girls.
In boys, a similar approach was followed. After the initial analysis, all the non-significant predictors were removed from the model and the logistic regression was performed again. This time the significant predictors of breakfast skippers were the hours spent in the gym (Wald = 4·225, P < 0·05) and the number of diets attempted in the past (Wald = 21·377, P < 0·001). The model was statistically significant (χ 2 = 24·73, P < 0·001) and the −2 LL = 5074·43 (the Cox and Snell R 2 = 0·004). This means that it explained 0·4 % of the variance, which is really low. In adolescent boys, spending more hours in the gym and fewer previous dieting attempts are significant predictors of breakfast eaters. Both logistic regressions provide some evidence that breakfast skipping is associated with unhealthy behaviours such as watching TV for a long time, not exercising, a lot of attempts in dieting and drinking a lot of alcohol.
Discussion
Many studies have shown a decline in the rate of breakfast consumption over the years, which is the case mainly with American adolescents(Reference Siega-Riz, Popkin and Carson22, Reference Cohen, Evers and Manske23). In Europe, the extent of breakfast skipping varies from 12 % to 28 %(Reference Vanelli, Iovane and Bernardini24, Reference Croezen, Visscher and Ter Bogt25) (12 % in North Italian pubertal boys, 28 % in North Italian pubertal girls, 13·8 % in 15–16-year-old Dutch boys, 18·2 % in 15–16-year-old Dutch girls). Another Greek study(Reference Dialektakou and Vranas26), which was conducted in a limited sample of Greek students from the city of Piraeus, came up with analogous results on breakfast skipping (13·7 % of boys ate very rarely and 2·9 % never ate breakfast on weekdays, while 14·8 % of girls ate very rarely and 5·2 % never ate breakfast on weekdays). The present study, however, has limitations in that it was conducted in older adolescents and young adults within the limits of a certain city.
Our results are more consistent with the findings of an Australian survey conducted among 13-year-olds concerning the extent of skipping breakfast. Moreover, as was the case in Australia and in the above-mentioned studies, Greek adolescent girls seem to skip breakfast more often than do boys(Reference Shaw27).
In our study, breakfast skipping rates were found to be higher in older than in younger ages in both sexes, which could have two possible explanations: (i) the parental influence is more obvious in younger adolescents who are either forced or persuaded by their parents to have breakfast, or simply tend to mimic their parents, while older adolescents tend to differentiate themselves from the rest of the family and to follow the habits of their friends of waking up late and leaving for school on an empty stomach. (ii) As the adolescents get older, they are more and more concerned about their image and falsely believe that by skipping breakfast they may reduce their energy intake. This hypothesis may also explain why young women, even from very early adolescence, skip breakfast more often than do boys, since it is generally known that girls tend to be more obsessed about their weight at an earlier age.
Furthermore, several studies among children and adults have shown an inverse association between breakfast consumption and BMI(Reference Jeffery, Forster and Folsom5–Reference Wilsgaard, Jacobsen and Arnesen10). To our knowledge, this is the first national analysis of breakfast habits in adolescents in Greece and its findings are consistent with studies conducted in other countries.
Several mechanisms to explain this putative effect of breakfast consumption on BMI have been postulated. Breakfast consumption could contribute to a greater meal frequency per day, which could lead to less efficient energy use by increasing dietary-induced thermogenesis, and hence result in a lower BMI(Reference Drummond, Crombie and Kirk28). Moreover, breakfast consumption may prevent overeating during the day. Ghrelin levels rise(Reference Cummings, Purnell and Frayo29) and insulin levels decline during prolonged fasting(Reference Boyle, Shah and Cryer30), which may trigger hunger and stimulate eating. It has also been shown that persons who consume a high-energy breakfast derive more daily energy from carbohydrates and less from fat than those who consume either a low-energy breakfast or no breakfast at all. This could lead to better weight control for breakfast consumers(Reference Preziosi, Galan and Deheeger31).
On the other hand, one could propose a different point of view concerning breakfast-eating habits. It could be hypothesised that adolescents who already have problems controlling their weight skip breakfast in order to limit their total daily energy intake.
On these grounds, one could propose two different explanations for our finding concerning the relationship between breakfast consumption habits and past dieting experience. Specifically, in both boys and girls who have been in need of a diet in the past, breakfast consumption was lower than in those who had never been on a diet. This could reflect either (i) the positive impact of breakfast consumption on weight control, thus reducing the need for dieting, or (ii) the conscious effort of adolescents with weight problems to limit their total daily energy intake by skipping breakfast in an attempt to lose weight.
In our study, we also found that skipping breakfast can be part of a constellation of several unhealthy lifestyle parameters, namely smoking, alcohol drinking and a more sedentary lifestyle, as can be estimated from leisure-time activities. This finding is consistent with other studies in which breakfast skipping in adolescents has also been associated with various health-compromising behaviours and unhealthy lifestyles(Reference Kapantais, Tzotzas and Ioannidis20–Reference Cohen, Evers and Manske23). Other studies have also shown that breakfast skippers, even after controlling for age, gender and BMI, have significantly higher total cholesterol levels than breakfast consumers. If that is verified by further study, then the constellation of higher BMI together with higher total cholesterol levels and the above-mentioned health-compromising behaviours in breakfast skippers could be detrimental to the health of adolescents(Reference Drummond, Crombie and Kirk28).
Thus, it seems that skipping breakfast reflects more than just meal timing preferences; it appears to be, in fact, one component of frequently co-occurring health-compromising behaviours. Adolescents who skip breakfast may care less about their health than those who eat breakfast regularly. On these grounds, we could propose a different approach to the detection of dangerous behaviours in adolescents through questioning about their breakfast habits. Breakfast skipping is easily admitted, while alcohol consumption or smoking could be more difficult to assess since adolescents may feel ashamed about them. However, further evidence is needed to show that this is possible, as the present study’s results cannot be generalised due to the low R 2 in the logistic regressions.
Moreover, smoking is sometimes used to augment dieting, since it has been shown to increase energy expenditure slightly. Furthermore, smoking, which was more common in our study among breakfast skippers than breakfast consumers, may either suppress one’s appetite in the morning or reduce the time available for a healthy first meal. Even if smoking were to be used in that sense, it would not prove fruitful according to our findings. As was shown by multiple regression analysis, there was no influence of smoking on BMI among boys, while among girls, smokers actually had a greater BMI than non-smokers.
Simple nutritional interventions concerning breakfast eating may fail to address these more complex issues. The most effective strategy for influencing the breakfast habits of adolescents is probably to create family atmospheres that endorse generally health-conscious lifestyles. This healthy family environment should be present even during the early years of life, since, as we have previously proposed, parental influence on the eating habits of offspring is likely to be age-specific and the eating habits of teenagers are less likely to be under parental control than those of young children.
Acknowledgements
The study was funded by the pharmaceutical companies Abbott Laboratories Hellas and Roche Hellas. There is no conflict of interest to declare. E.K. wrote the introduction and discussion sections. E.C. wrote the introduction and methods sections. D.K. wrote the results section and helped with the discussion. The rest of the authors helped in data collection, distributing questionnaires, etc. The authors would like to extend their sincere gratitude to the Hellenic Ministry of Education for approval of the project and their collaboration, as well as to the directors and gym instructors of the various schools for their active participation in the survey.









