The Middle Eastern countries are experiencing a nutrition transition that is shifting from traditional diets high in fibre, fruits and vegetables towards Western diets high in fat, sugar and salt(Reference Amuna and Zotor1). This has resulted in noticeable increases in the prevalence of obesity and its related co-morbidities(Reference Popkin and Gordon-Larsen2). It has been reported that 25–45 % of total deaths in these countries are due to CVD(Reference Yusuf, Reddy and Ounpuu3). Besides being the leading cause of death(Reference Naghavi, Abolhassani and Pourmalek4), CVD represents a different picture in this part of the world. Unlike the situation in most developed countries, cardiovascular risk factors are more prevalent among Middle Eastern women than men(Reference Azizi, Esmaillzadeh and Mirmiran5). Furthermore, due to high consumption of refined carbohydrates, low HDL cholesterol (HDL-C) and high TAG are the most prevalent cardiovascular risk factors in this part of the world(Reference Esmaillzadeh and Azadbakht6). Additionally more than two-thirds of the adult population has dyslipidaemia(Reference Mirmiran, Esmaillzadeh and Azizi7). Furthermore, in contrast to trends observed in northern Europe and the USA, mortality from CVD has risen in the Middle East(Reference Yusuf, Hawken and Ounpuu8). On the other hand, the majority of available data on dietary determinants of CVD, particularly diet–CVD relationships, has mainly been confined to Western populations with their own dietary characteristics and it is unclear to what extent these findings might apply to the Middle Eastern population taking into account that dietary intakes in this region are totally different from those in Europe, the USA or even other parts of Asia(Reference Esmaillzadeh and Azadbakht9). Therefore, identification of diet–CVD relationships is of great importance in these countries.
Obesity is a major underlying factor contributing to CVD. Recently, great attention has been paid to dietary energy density (DED) in the aetiology of obesity(Reference Iqbal, Helge and Heitmann10–Reference Howarth, Murphy and Wilkens12). DED (kJ/g, kcal/g) has been defined as the amount of energy in a given weight of food(Reference Ello-Martin, Ledikwe and Rolls13). It has frequently been reported that consumption of energy-dense diets is significantly associated with greater risk of overweight, obesity or weight gain; not only in cross-sectional(Reference Howarth, Murphy and Wilkens12, Reference Ledikwe, Blanck and Kahn14) and prospective studies(Reference Savage, Marini and Birch15, Reference Bes-Rastrollo, van Dam and Martinez-Gonzalez16), but also in clinical trials, where reducing DED has been associated with significant weight loss(Reference Ello-Martin, Roe and Ledikwe17, Reference Saquib, Natarajan and Rock18). Obesity has been placed at the centre of studies focusing on DED; however, obesity-related co-morbidities have not received the attention they deserve in this field. Energy-dense diets have been reported to be high in refined grains, processed foods, added sugars and added fats, and low in fruits, vegetables and whole grains – all of these items have been associated with greater risk of CVD. Furthermore, such diets could raise CVD risk through their effects on obesity and weight gain. There are just three reports(Reference Wang, Luben and Khaw19–Reference Murakami, Sasaki and Takahashi21) available discussing DED in relation to metabolic risk factors: one has assessed incident diabetes as an outcome(Reference Wang, Luben and Khaw19) among adults in Norfolk, UK; the second(Reference Mendoza, Drewnowski and Christakis20) found an independent positive association between DED and the metabolic syndrome among US adults; and the third by Japanese investigators failed to find a significant relationship between DED and metabolic risk factors(Reference Murakami, Sasaki and Takahashi21). These three studies have their own limitations: the study by Wang et al.(Reference Wang, Luben and Khaw19) just considered diabetes, not other cardiovascular risk factors; Mendoza et al.(Reference Mendoza, Drewnowski and Christakis20) used a single day's 24 h dietary recall for collecting dietary data whereas 24 h dietary recall cannot reflect participants’ habitual dietary intakes(Reference Willett22); and Murakami et al.'s(Reference Murakami, Sasaki and Takahashi21) study participants were lean young women. To better understand the association between DED and cardiovascular risk factors, we designed the current study in a non-Western population whose dietary intakes have their own unique characteristics(Reference Esmaillzadeh and Azadbakht9, Reference Esmaillzadeh and Azadbakht23). Therefore, the main aim of the present study was to assess the association between DED and cardiovascular risk factors among Iranian women. The second aim was to examine if the associations between DED and metabolic risk factors are mediated through obesity.
Materials and methods
Participants
Detailed information about the present cross-sectional study, its participants and measurements has been published earlier(Reference Azadbakht and Esmaillzadeh24–Reference Esmaillzadeh, Kimiagar and Mehrabi26). Briefly, by the use of multistage cluster random sampling method, 583 Tehrani female teachers from different socio-economic categories were invited to participate and 521 women (response rate: 89 %) agreed and gave informed written consent. Exclusion criteria for the current analysis were the existence of a prior history of chronic diseases, leaving more than seventy items blank on the FFQ, under- or over-reporting of energy intake (<3347 or >17 573 kJ (<800 or >4200 kcal), respectively) and taking medications (propranolol, lovastatin, furosemide, metformin). Therefore, 486 women with full relevant data remained for the current study. The current project was approved by the Research Council of the Food Security and Nutrition Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Assessment of dietary intake
We used a validated 168-item semi-quantitative FFQ for collecting dietary data(Reference Esmaillzadeh, Kimiagar and Mehrabi27, Reference Esmaillzadeh, Kimiagar and Mehrabi28). Participants were asked to report the frequency of food items they consumed in the previous year considering a given serving of food items in the questionnaire. They were asked to report on a daily, weekly or monthly basis. We then calculated grams per day of the consumed foods using standard protocols. Total energy intake was calculated by summing up energy intakes from all 168 food items in the questionnaire.
Our validation study(Reference Esmaillzadeh, Kimiagar and Mehrabi27, Reference Esmaillzadeh, Kimiagar and Mehrabi28) with the use of biomarkers and also twelve 24 h dietary recalls as gold standard indicated that the FFQ provided a reasonably valid and reliable measure of intake for most food and nutrient intakes. Although we did not assess the correlation coefficients for DED per se, the correlations for fruits, vegetables and fats (the most influential factors on DED) were reasonable. For instance, comparing two FFQ completed 1 year apart, we reached the correlation coefficients of 0·71 for reproducibility of fruits, 0·74 for vegetables, 0·59 for partially hydrogenated and 0·69 for non-hydrogenated vegetable oils. The validity of the FFQ for assessing consumption of fruits, vegetables, partially hydrogenated and non-hydrogenated vegetable oils was also good, such that between the FFQ and detailed dietary recalls, corresponding correlation coefficients were 0·61, 0·57, 0·55 and 0·44, respectively.
Calculation of dietary energy density
To calculate DED, we divided each individual's reported daily energy intake from foods only (kJ/d, kcal/d) into total weight of foods consumed (g/d). Total weight of foods consumed by participants was calculated by summing up the weight of foods only (154 out of 168 food items in the FFQ). We did not consider energy and weight of drinks consumed because a recent systematic review has shown that calculating DED by including drinks results in a variable that biases associations between DED and weight gain towards the null(Reference Johnson, Wilks and Lindroos29). Earlier studies have shown that calculating DED based on foods only would provide a variable with the best associations with obesity and weight gain(Reference Kant and Graubard30).
Assessment of other variables
Anthropometric variables including weight, height and waist circumference were measured(Reference Esmaillzadeh and Azadbakht9) and BMI was calculated as weight in kilograms divided by the square of height in metres. Plasma glucose concentrations and serum lipid levels were measured on a fasting blood sample by the use of a Selectra 2 auto-analyser (Vital Scientific, Spankeren, Netherlands)(Reference Esmaillzadeh, Kimiagar and Mehrabi28). Fasting plasma glucose (FPG) was measured on the day of blood collection by the enzymatic colorimetric method using glucose oxidase (Pars Azmoon Inc., Tehran, Iran). Serum TAG concentrations were assayed using TAG kits (Pars Azmoon Inc.) by enzymatic colorimetric tests with glycerol phosphate oxidase. Serum HDL-C was measured after precipitation of the apo-B-containing lipoproteins with phosphotungstic acid. Serum LDL cholesterol (LDL-C) was calculated from serum total cholesterol (TC), TAG and HDL-C, except when TAG concentration was greater than 4·4 mmol/l (400 mg/dl)(Reference Friedwald, Levy and Fredrickson31). The inter- and intra-assay CV of this method were <10 %. Blood pressure was measured three times after the participants sat for 15 min, as reported earlier(Reference Esmaillzadeh, Kimiagar and Mehrabi26). We used the International Physical Activity Questionnaire for obtaining data on physical activity(Reference Craig, Marshall and Sjostrom32). Using standard guidelines(Reference Ainsworth, Haskell and Whitt33), these data were expressed as metabolic equivalent hours per week (MET-h/week). Additional information regarding age, smoking habits, socio-economic status (defined based on educational level, income, family size, being owner of the house or renting the house, house area), medical history and current use of medications was obtained using questionnaires.
Definition of terms
Hypertriacylglycerolaemia was defined as serum TAG ≥2·2 mmol/l (200 mg/dl), hypercholesterolaemia as serum TC ≥6·24 mmol/l (240 mg/dl), high serum LDL-C as ≥4·1 mmol/l (160 mg/dl) and low serum HDL-C as <1·29 mmol/l (50 mg/dl)(35). Dyslipidaemia was defined based on the third report of the National Cholesterol Education Program Adult Treatment Panel III(34) as having hypertriacylglycerolaemia or hypercholesterolaemia or high LDL-C or low HDL-C. Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg based on the sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure(35). Diabetes mellitus was defined as FPG ≥6·93 mmol/l(36). The presence of ‘at least one risk factor’ and ‘at least two risk factors’ of the three major risk factors for CVD (hypertension, dyslipidaemia and diabetes) was also evaluated.
Statistical methods
Quartile cut-off points of DED were used for categorizing participants. General characteristics and dietary intakes of participants were compared across quartiles of DED by the use of ANOVA, χ 2 and analysis of covariance (ANCOVA) where appropriate. All dietary intakes were obtained by the use of General Linear Models with age and total energy intake as covariates. Multivariate-adjusted means for metabolic risk factors were compared across quartiles of DED by the use of ANCOVA. Selection of variables to be included in the models was done using the change-in-estimate method. This method has been shown to produce more reliable models than the methods based on statistical significance(Reference Maldonado and Greenland37). Therefore, a potential confounder is included in the model if it changed the coefficient by 10 %. This approach is consistent with the definition of confounding, where confounding is said to be present if the unadjusted effect differs from the effect adjusted for putative confounders(Reference Maldonado and Greenland37). Adjustments were made for age, cigarette smoking, physical activity, socio-economic status, current oestrogen use, menopausal status, family history of diabetes and stroke, and BMI. To explore the associations between DED and cardiometabolic risk factors, we obtained prevalence ratios in different models. First, we adjusted for age (years), cigarette smoking (yes or no), physical activity (MET-h/week), socio-economic status (categorical), current oestrogen use (yes or no), menopausal status (yes or no) and family history of diabetes and stroke (yes or no). Then adjustments were made for BMI. All models were done by treating DED as quartile categories with the first quartile as a reference. The overall trend across quartiles of DED was examined through the use of the Mantel–Haenszel extension χ 2 test. The SPSS statistical software package version 10·0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. P ≤ 0·05 was taken to indicate statistical significance.
Results
Mean DED was 7·41 (sd 1·46) kJ/g (1·77 (sd 0·35) kcal/g). General characteristics and dietary intakes of women across quartiles of DED are shown in Table 1. Individuals in the top quartile of DED were younger, less physically active, less likely to be postmenopausal and had higher BMI compared with those in the lowest quartile. Consumption of energy-dense diets was associated with higher intakes of energy, dietary fat, cholesterol, vegetable oils, refined grains and high-fat dairy products, along with lower intakes of dietary carbohydrates, fruits, vegetables, and meat and fish.
Table 1 General characteristics and dietary intakes of 486 Tehrani females by quartile of dietary energy density (DED)*
%E, percentage of total energy intake.
*Data are means and standard deviations unless indicated otherwise.
†By using linear regression.
‡Obesity: BMI ≥ 30 kg/m2.
Multivariate-adjusted means for metabolic risk factors across quartiles of DED are provided in Table 2. After control for potential confounders, participants in the highest quartile of energy density had elevated levels of serum TAG, TC and LDL-C and lower levels of serum HDL-C compared with those in the lowest quartile. Higher DED was not associated with FPG levels, systolic and diastolic blood pressure.
Table 2 Multivariate-adjusted means of cardiovascular risk factors across quartiles of dietary energy density (DED) among 486 Tehrani females*
FPG, fasting plasma glucose; TC, total cholesterol; HDL-C, HDL cholesterol; LDL-C, LDL cholesterol; SBP, systolic blood pressure; DBP diastolic blood pressure.
*Data are means with their standard errors adjusted for age, cigarette smoking, physical activity, socio-economic status, current oestrogen use, menopausal status, family history of diabetes and stroke, and BMI.
†By using linear regression.
The prevalences of cardiometabolic risk factors across quartiles of DED are shown in Fig. 1. Women in the top quartile of DED were more likely to have dyslipidaemia, at least one and at least two cardiometabolic risk factors. No overall significant association was found between DED and prevalence of diabetes and hypertension.
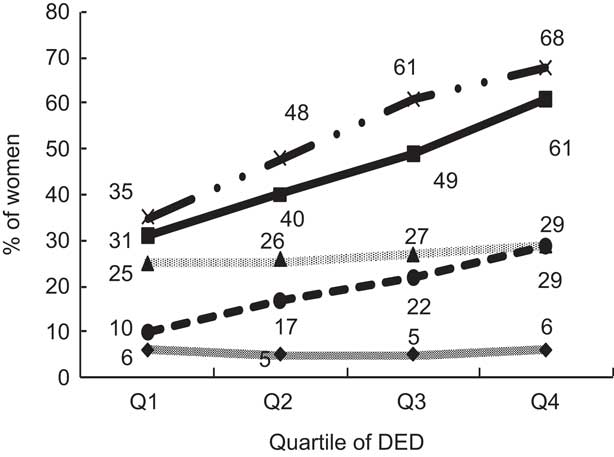
Fig. 1 Prevalence of cardiovascular risk factors (![]() , diabetes;
, diabetes; ![]() , dyslipidaemia;
, dyslipidaemia; ![]() , hypertension;
, hypertension; ![]() , at least one risk factor (ALORF);
, at least one risk factor (ALORF); ![]() , at least two risk factors (ALTRF)) across quartiles of dietary energy density (DED) among 486 Tehrani females. Diabetes was defined as fasting plasma glucose ≥126 mg/dl. Dyslipidaemia was defined as having hypertriacylglycerolaemia (serum TAG ≥200 mg/dl) or hypercholesterolaemia (serum total cholesterol ≥240 mg/dl) or high LDL cholesterol (≥160 mg/dl) or low HDL cholesterol (<50 mg/dl). Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg based on sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. ALORF and ALTRF were defined as having at least one and two cardiometabolic risk factors, respectively, from among the three major risk factors of hypertension, dyslipidaemia and diabetes. Women in the top quartile of DED were more likely to have dyslipidaemia, at least one and at least two cardiometabolic risk factors
, at least two risk factors (ALTRF)) across quartiles of dietary energy density (DED) among 486 Tehrani females. Diabetes was defined as fasting plasma glucose ≥126 mg/dl. Dyslipidaemia was defined as having hypertriacylglycerolaemia (serum TAG ≥200 mg/dl) or hypercholesterolaemia (serum total cholesterol ≥240 mg/dl) or high LDL cholesterol (≥160 mg/dl) or low HDL cholesterol (<50 mg/dl). Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg based on sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. ALORF and ALTRF were defined as having at least one and two cardiometabolic risk factors, respectively, from among the three major risk factors of hypertension, dyslipidaemia and diabetes. Women in the top quartile of DED were more likely to have dyslipidaemia, at least one and at least two cardiometabolic risk factors
Multivariate-adjusted prevalence ratios for cardiometabolic abnormalities across quartiles of DED are presented in Table 3. After controlling for age and other potential confounders, consumption of energy-dense diets was significantly associated with greater chance of having dyslipidaemia (prevalence ratio in top quartile v. bottom quartile: 1·78; 95 % CI 1·33, 2·58), at least one (1·81; 1·44, 2·49) and at least two cardiometabolic risk factors (2·81; 1·51, 5·24). Additional control for BMI slightly attenuated the associations but all were still significant. Even after further adjustment for total energy intake the associations remained significant. No overall significant associations were found between consumption of energy-dense diets and risk of having diabetes or hypertension either before or after adjustment for confounders.
Table 3 Multivariate-adjusted prevalence ratios and 95% confidence intervals for cardiovascular risk factors across quartiles of dietary energy density (DED) among 486 Tehrani females*†
PR, prevalence ratio; ALORF, at least one risk factor; ALTRF, at least two risk factors.
*Diabetes was defined as fasting plasma glucose ≥126 mg/dl. Dyslipidaemia was defined as having hypertriacylglycerolaemia (serum TAG ≥200 mg/dl) or hypercholesterolaemia (serum total cholesterol ≥240 mg/dl) or high LDL cholesterol (≥160 mg/dl) or low HDL cholesterol (<50 mg/dl). Hypertension was defined as systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg based on sixth report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. ALORF and ALTRF were defined as having at least one and two cardiometabolic risk factors, respectively, from among three major risk factors of hypertension, dyslipidaemia and diabetes.
†Model I: adjusted for age, cigarette smoking, physical activity, socio-economic status, current oestrogen use, menopausal status and family history of diabetes and stroke. Model II: additionally adjusted for BMI.
‡By the use of Mantel–Haenszel extension χ 2 test.
Discussion
We found that consumption of energy-dense diets was associated with higher risk of having dyslipidaemia, at least one and at least two cardiometabolic risk factors. No overall significant associations were found between DED and the prevalence of hypertension and diabetes. To the best of our knowledge, the present study is among the first to examine DED in relation to cardiometabolic abnormalities in a Middle Eastern population.
Several controversial methods have been proposed for calculating DED. Some investigators have suggested the use of drinks in DED calculation, others disagree(Reference Cox and Mela38, Reference Ledikwe, Blanck and Kettel-Kahn39). In a recent systematic review(Reference Johnson, Wilks and Lindroos29), it was suggested that drinks must be excluded from the calculation of DED and including ‘foods only’ would better reflect the meaning of DED. This conclusion was based on findings from cross-sectional or prospective studies indicating the effect of DED on body weight(Reference Ledikwe, Blanck and Kahn14, Reference Mendoza, Drewnowski and Christakis20, Reference Ledikwe, Rolls and Smiciklas-Wright40). In the current study, only foods, not drinks, were considered for calculating DED. Such method of calculation would not bias the associations towards the null(Reference Johnson, Wilks and Lindroos29). However, when we considered beverages in the calculation of DED, the associations were slightly attenuated but their significance did not alter. Mean DED obtained in the present study is slightly higher than that in other investigations using the same method.
We found that high DED is associated with unhealthy food choices. This finding is in agreement with other studies where DED has been related to poor diet quality(Reference Ello-Martin, Roe and Ledikwe17, Reference Malik, Schulze and Hu41). Energy-dense diets are often high in refined grains, processed foods, added sugars and added fats, and low in fruits, vegetables and whole grains. The main characteristic of energy-dense diets, as shown by Bes-Rastrollo et al.(Reference Bes-Rastrollo, van Dam and Martinez-Gonzalez16), is that they contain higher amounts of saturated and trans fats and a higher glycaemic load. It must be kept in mind that high-fat diets do not necessarily contain higher energy density. A prominent example in this case is the traditional Mediterranean dietary pattern. Despite the higher content of fat, this dietary pattern is also popular for its higher content of fruits and vegetables. In Japan, low-energy-dense diets have been reported to be high in boiled rice and noodles(Reference Murakami, Sasaki and Takahashi21). In the 1994–1996 Continuing Survey of Food Intakes by Individuals, Ledikwe et al.(Reference Ledikwe, Blanck and Khan42) have shown that consumption of a low-energy-dense diet is associated with higher intakes of micronutrient-rich foods high in water and low in fat, lower intakes of total dietary fat and carbonated beverages, and higher intakes of vitamins A, C and B6, folate, Fe, Ca and K. It seems that low-energy-dense diets in different parts of the world have their own characteristics: in some Asian populations they contain foods high in water, whereas in Western populations they contain a lower content of fat. The diet in Middle Eastern countries is totally different from that in the USA, Europe and also other parts of Asia. However, it seems that the characteristics of energy-dense diets in Iran are similar to those in Western populations. Characteristics of energy-dense diets are particularly important when reducing DED is chosen as a strategy for weight management. What is the best way to reach reduced DED is still under investigation. Some have suggested reduced intakes of foods rich in saturated fats and refined carbohydrates and a simultaneous increase in fruit and vegetable intakes(Reference Bes-Rastrollo, van Dam and Martinez-Gonzalez16). Others believe that reducing the consumption of soft drinks is the case(Reference Malik, Schulze and Hu41).
We found a significant positive association between DED and the prevalence of dyslipidaemia. However no significant association was found with DED, hypertension and diabetes. Although previous studies have found a positive association between DED and the metabolic syndrome(Reference Mendoza, Drewnowski and Christakis20), no one has reported such an association with dyslipidaemia. In a cross-sectional study among young Japanese women aged 18–22 years, Murakami et al.(Reference Murakami, Sasaki and Takahashi21) failed to find a significant relationship between DED and metabolic variables such as plasma glucose levels, blood lipid profiles and blood pressure. The difference between our findings and those of Murakami et al.(Reference Murakami, Sasaki and Takahashi21) might be explained by the characteristics of the study population. In the Japanese study lean young women were studied, while ours was an overweight population. In contrast to our findings about diabetes, Wang et al.(Reference Wang, Luben and Khaw19) found a positive significant association between DED and incident diabetes. The lack of an association between DED and diabetes in our study needs further investigations. Possible reasons for this finding might be the lower prevalence of diabetes compared with the other cardiovascular risks, inadequate sample size and the cross-sectional design of the study. It must also be kept in mind that in our study type 2 diabetes was determined only by the use of FPG, which clearly underestimates the prevalence. To further explore the association of DED and diabetes, one would need to use the 2 h post-challenge plasma glucose measure as well. Another explanation might be the quantity and quality of dietary fibre, which plays different roles in glucose metabolism(Reference Sartorelli, Freire and Ferreira43). It has previously been shown that considering the quantity of total dietary fibre intake without taking into account its food sources might fail to explain its association with the development of impaired glucose disturbance(Reference Sartorelli, Freire and Ferreira43). It was shown previously that consumption of energy-dense diets is associated with overweight and obesity(Reference Ello-Martin, Roe and Ledikwe17, Reference Kant and Graubard30) – these conditions play an important role in developing diabetes and hypertension.
Our findings must be interpreted in the light of some study strengths and limitations. The strengths include the coverage of a broad range of dietary intakes from different socio-economic categories in Tehran, adjustment for important confounders between DED and cardiometabolic abnormalities, and finally the use of a validated FFQ. Limitations of the current study are the cross-sectional design of the study, probable misclassification of participants due to the use of semi-quantitative FFQ for dietary data collection and confining the participants to women. It must be kept in mind that our sample is representative of Tehran female teachers only, due to the sampling procedure we used. It cannot be regarded as a representative sample of the whole Iranian women or even Tehrani women.
It is concluded that consumption of energy-dense diets is significantly associated with a high prevalence of dyslipidaemia, at least one and at least two cardiometabolic risk factors among Iranian women. Further investigations on larger samples with prospective designs are warranted.
Acknowledgements
The data collection phase of the study was supported by a grant (P. 25/47/2337) from the National Nutrition and Food Technology Research Institute of the Islamic Republic of Iran and Shaheed Beheshti University of Medical Sciences, Tehran, Iran. Financial support for the conception, design, data analysis and manuscript drafting came from the School of Public Health, Isfahan University of Medical Sciences, Isfahan, Iran. A.E., H.K.B. and L.A. have no personal or financial conflicts of interest. A.E., H.K.B. and L.A. participated in the collection of data, conception and design, statistical analysis and data interpretation, manuscript drafting and approval of the final manuscript for submission. The authors would like to express their grateful appreciation to the Research Council of the Food Security Research Center, Isfahan University of Medical Sciences, for their support.






