The WHO described childhood obesity as ‘one of the most serious public health challenges of the 21st century’(1). This is due to the increasing prevalence of childhood obesity and associated physical and psychological health decrements. In response, national governments and healthcare organisations have developed initiatives to monitor the prevalence and develop interventions. For instance, the UK Government’s ‘Childhood Obesity; a plan of action chapter 2’ stated that there is a national ambition to halve childhood obesity and to significantly reduce the gap in prevalence between children in the most and least deprived areas by 2030(2).
An initiative developed in England is the National Child Measurement Programme (NCMP) which is a mandatory programme delivered to all children in the first and final year of primary school (aged 4–5 and 10–11 years) whose parents/guardians have not opted out(3). The programme was originally developed as a method of monitoring children’s weight status and has been delivered predominantly in primary school settings in England. Where schools opt out from delivering the NCMP on their premises, nearby locations such as village halls are utilised. The programme has three phases: pre-measurement, where parents are contacted by their Local Government Authority (LGA) to inform parents/guardians about the programme including an opportunity to opt out; the measurement, where children are measured for their height and weight which is translated into BMI z-scores and recorded in a national database (this provides national statistics for childhood overweight and obesity); and post-measurement, where parents/guardians are contacted by their LGA, typically providing an overview and relevant information (a feedback/the result letter) about their child’s weight status. Nationally, the programme has 95 % uptake equating to over 1 million children measured each year(4). Out of the three phases, only the pre-measurement phase is mandated and LGA are required to inform parents according to The Local Authority (Public Health, Health and Wellbeing Boards and Health Scrutiny) Regulations 2013(5) The provision of the results is voluntary but recommended by the British Government(6) who also ensured that the legislative changes enabled to issue results to parents from 2008 to 2009(Reference Nnyanzi, Summerbell and Ells7–9). These changes have evolved the programme from monitoring to a screening initiative(Reference Grimmett, Croker and Carnell10–Reference Ames, Mosdøl and Blaasvær12). Lastly, proactive follow-up of children who fall into the extremely low and high BMI centiles is recommended by the operational guidelines developed at the Public Health England (PHE)(3).
Previous research regarding the NCMP has predominantly focused on the aspects related to the results feedback. For example, Nnyanzi et al. (Reference Nnyanzi, Summerbell and Ells7) interviewed parents of children in the Reception and Year 6 who received the Overweight results and identified a range of behaviours (16 parents; female = 13, low socio-economic status = 8) such as being shocked, denying the results, or fear or help-seeking. Gainsbury and Dowling(Reference Gainsbury and Dowling13) described parental experience regarding the feedback for children in the Reception year using four focus groups (18 parents). Their results showed that parents commonly rejected the results letter for children identified as Overweight as they have felt the result was intended primarily for parents other than themselves and perceived the feedback as patronising and offensive(Reference Gainsbury and Dowling13).
In 2019, Sallis and Colleagues(Reference Sallis, Porter and Tan14) conducted a cluster-randomised controlled trial to investigate whether the uptake to children’s weight management services can be increased by modifying the result letters. They have found a small effect between the intervention (4·33 % chance of uptake) and control group (2·19 % chance of uptake) among 2642 parents(Reference Sallis, Porter and Tan14). In other work examining the impact of behaviour change from the parent feedback from the NCMP, Viner et al. reported that feedback has a positive effect on parental intentions to change behaviour; however, it often does not translate into the actual behaviour change(Reference Viner, Kinra and Christie15). Additionally, in their study, they have found that parents consult the results not only with various professionals such as GP (general practitioner) and school nurses but also use informal sources from the internet.
To our knowledge, there is no published data or research on the methods used to deliver the NCMP across the 152 LGA in England, and the PHE guidance to LGA regarding the delivery of the NCMP allows for a varied approach, meaning schools, parents and families are likely to have varied experiences(3,16,17) . Thus, this study aimed to explore the delivery and implementation of the NCMP in England.
Method
Design
An online survey to explore the delivery of the NCMP was developed, comprising 59 questions. Most included an option to select ‘I don’t know’ or ‘Other’. Where ‘Other’ was selected, LGA representatives were asked to provide further details in an open-ended question.
The survey consisted of five blocks of questions: (1) opt out of NCMP; (2) parents’ result feedback; (3) proactive follow-up; (4) available services and (5) sociodemographic and supplementary information. Where appropriate, LGA representatives were able to skip questions. Three versions of the survey were piloted with a convenience sample (n 35) of LGA Health and Wellbeing Board Commissioners from across England, representatives of PHE and university researchers before releasing the final version.
The final survey questions were selected as part of in-depth consultations with the NCMP team at PHE and representatives of selected LGA who volunteered to peer-review each survey iteration. The most significant change was reducing the number of questions from 122 to 59. Additionally, the selected experts had practical experience with the NCMP which helped to modify the survey terminology. For example, initially, we have used the term ‘routine feedback’ but after the consultation was replaced with ‘parents results letter’.
As part of the survey, LGA representatives were asked to upload their most recent NCMP documentation, that is, pre-measurement letters, result letters and any additional attachments sent with the letters. To increase the participation rate, all representatives were entered into a prize draw to attend an international conference or one of two £100 amazon gift vouchers.
Sampling
Conventional sample size estimations for finite population was used where the margin of error was z × se ≤ 0·05 (up to 5 %)(Reference Ramachandran and Tsokos18). The finite population correction formula was applied on calculated sample size from infinite population formula based on the margin of error formula(Reference Diez, Barr and Cetinkaya-Rundel19). This has yielded the required sample size of 110 after rounding. Non-probability convenience sampling(Reference Etikan, Musa and Alkassim20,Reference Levy and Lemeshow21) was used, which was facilitated throughout PHE regional centres. As shown in online supplementary material, Supplemental Figure 5, we have achieved response rates between 53 and 69 % across four geographical regions (London, Midlands and the East, the South, and the North) of England (see online supplementary material, Supplemental Figures 6–8 for additional demographic details).
Procedure
After institutional ethics clearance, LGA were contacted via emails to complete the survey between February 2018 and May 2018. In agreement with PHE’s NCMP team, emails were delivered to LGA with the assistance of PHE Regional Offices. The email asked for a representative from each LGA who has a good understanding of the operational delivery and access to the NCMP documentation to complete the survey. Freedom of Information requests was sent to 60 LGA in June 2018 who did not upload the NCMP documentation within the survey; 55 LGA provided the documents.
Data analysis
Descriptive analysis of the survey data was produced to represent LGA delivery of the NCMP. Results are presented as frequencies and percentages, with supplementary visual representations using R software environment for statistical computing version 4.0.0 (2020–04–24), R Studio 1.3.959 and the Grammar of Graphics 2 (ggplot2)(Reference Wickham22).
Results
Descriptives
Ninety-two (out of 152; 61 %) LGA representatives completed the survey (assumed margin of error was z × se ≤ 0·10 or 10 %). Each LGA selected their representative; see Supplemental Figure 1. A further 23 LGA provided NCMP documentation after Freedom of Information requests (i.e. 115 LGA). For the majority of sampled (n 92) LGA, the NCMP delivery is commissioned to a provider organisation (The provider is any organisation supporting the NCMP that has been commissioned by an LGA and is not the LGA itself.) (88 %), then in-house (11 %), other (4 %) and I don’t know (0 %).
Figure 1 provides an overview of the tasks and responsibilities for NCMP delivery. Panel A represents those that are managed by LGA, Panel B shows the responsibilities managed by a commissioned provider and Panel C indicates what responsibilities are shared amongst the two. The graphs are set visualisations and are analogous to Venn diagrams where the upper section of the visualisation indicates the number of responses (NR) for a given combination of (sets) responsibilities(Reference Conway, Lex and Gehlenborg23,Reference Lex, Gehlenborg and Strobelt24) .
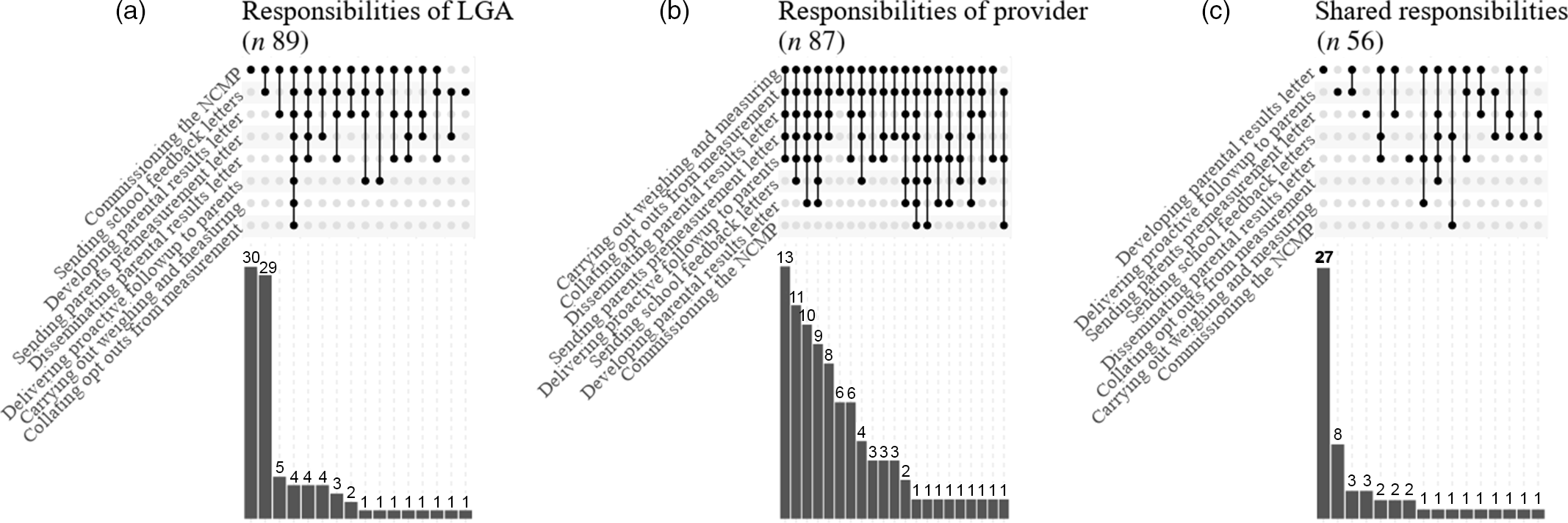
Fig. 1 Responsibilities: (a) responsibilities of LGA (n 89), (b) responsibilities of provider (n 87) and (c) shared responsibilities (n 57). LGA, Local Government Authority
The two most common responsibilities (sets) were commissioning the NCMP (NR = 30) and sending school feedback letters (NR = 29) (Panel A, Fig. 1).
In comparison, commissioned providers were tasked to manage various responsibilities with the dominant set including all responsibilities except for commissioning the NCMP, sending school feedback letters and developing result letters for parents (NR = 13) (Panel B, Fig. 1).
By far, the most common shared responsibility was developing result letters for parents (NR = 27), and thus, LGA and providers co-author the NCMP result letters which are delivered to parents (Panel C, Fig. 1).
Pre-measurement information
Legally, all LGA must inform parents and offer them an opportunity to opt their child out of the NCMP. Therefore, it was assumed that all LGA perform this duty.
The most common method of informing parents about the NCMP measurements among the participating LGA was via children’s school bags (n 64; 70 %), followed by postal services (n 23; 13 %); see Fig. 2 – right-hand side. However, LGA often facilitated the delivery of information using multiple methods as per Fig. 2 – left-hand side. The letters and postal services were the most common combination of sets indicating that these are the preferred methods of delivering the pre-measurement information (NR = 39 and NR = 14, respectively); Fig. 2 – left-hand side.

Fig. 2 Methods of informing about NCMP
LGA primarily use the PHE specimen; however, the majority (n 55; 60 %) modify it. Five representatives indicated they had never seen the specimen. Inductive content analysis(Reference Braun and Clarke25) of the reasons LGA change the PHE pre-measurement specimen letter indicated four themes – clarifications, language, localisation and user-driven; see Supplemental Table 1.
Finally, LGA were asked whether they provide attachments alongside the opt-out letter: 45 (49 %) included attachments, 33 (36 %) did not and 14 (15 %) did not provide an answer.
Result feedback to parents
Seventy-nine (86 %) of sampled LGA provide result feedback to parents. Fig. 3, Panel B shows that of those LGA most (NR = 55) delivered results to all weight categories; however, 14 LGA indicated that they prioritise children outside Healthy Weight category and 4 indicated they only target the upper weight category with the rest of the representatives indicating mixed response pattern.

Fig. 3 (a) How do you share results with parents? (n 79) and (b) Do you share results with all parents? (n 79)
The most common option from the sum of all options (i.e. sum of all distinct options in sets) describing the methods for delivering the result feedback to parents was postal services (i.e. letters, n 69, 75 %), followed by phone calls (n 20, 22 %). Additionally, 84 % (66) of LGA provide an attachment (e.g. Change4Life Leaflet) alongside result.
The most common set of delivery methods (see Fig. 3, Panel A) were postal services (NR = 45), followed by postal services combined with phone calls (NR = 15). Four LGA indicated that they only deliver via children’s school bags. In terms of alternative delivery methods for parents’ results feedback, the following responses were recorded: * ‘Coffee mornings’ (LGA from London),
‘Home visits’ (LGA from Midlands and the East),
‘We will be starting to utilise Parents ‘Chat Health’ which is an anonymous texting system for parents to raise concerns with the school nursing service’ (LGA from the Midlands and East), ‘We highly recommend that the school texts the parents of Year 6 children to inform them to come and collect their child’s letters by a certain date. If they do not get collected, they will then go out in the children’s school bag.’ (LGA from the North)
The final comment by one of the representatives indicates that children’s school bags may be a viable method if LGA do not regularly use postal services. In this case, parents are encouraged to gather the result feedback (i.e. letters) themselves from their school but if they do not, the LGA will use the child’s school bag method. This may also be rationalised by cost-effectiveness, despite PHE discouraging this delivery method.
Some LGA do not provide the result feedback to all parents; these reasons included prioritising children perceived to be of most need (21; 47 %), staff capacity to implement this mechanism (6; 13 %) and lack of service provision (2; 4 %):
‘We only send letters to underweight, overweight and very overweight. We had altered the letter a few times but still receive negative feedback from parents regarding the wording of the letter.’ (LGA from the North)
‘Parents have to request through a website for the height and weight of the child and that only appears on the letter sent to them. Some people loose [sic] these letters and struggle to find the information they need.’ (LGA from the South)
‘Parents are advised that they can call the Public Health Commissioner for Children and Young People to find out their child’s results.’ (LGA from London)
Fifty-one (65 %) of sampled LGA use PHE’s specimen result letter but tailor it to their needs; 23 % (n 18) use it and do not alter it and 11 % do not use it (n 9). Reasons for changing the PHE specimen result letter centred on five main themes – clarifications, design, language, localisations and user-driven, see Supplemental Table 2.
Finally, we asked the representatives how parents can contact them after receiving the results, see Supplemental Figure 2. Most of the representatives indicated that the two most common methods are phone number (NR = 30) and a combination of phone number with email (NR = 17). These contact options are listed within the result feedback (i.e. letters) parents receive.
Proactive follow-up
Sixty-five (71 %) of the participating LGA proactively follow up (i.e. proactive follow-up involves contacting a parent or carer to offer them personalised advice and services) with parents, 21 (23 %) do not and 6 (7 %) did not know. LGA were asked who receives the follow-up, what delivery methods they use and their reasons for targeting weight categories that they indicated. Sixty-five LGA who indicated that they deliver proactive follow-up indicated that they target parents of children identified within the Overweight and Very Overweight (n 19, 21 %); Underweight, Overweight and Very Overweight (n 19, 21 %); and Underweight and Very Overweight (n 11; 12 %) ranges (see Fig. 4, Panel B). Thus, proactive follow-up is focused primarily on groups excluding Healthy Weight; see Fig. 4, Panel B.

Fig. 4 (a) How do you proactively follow up with parents? (b) Do you proactively follow up with all parents? and (c) Why do you not proactively follow up with all parents?
The most common set of methods for proactive follow-up were phone calls (n 28) or phone calls and postal services (n 14); see Fig. 4, Panel A. Where proactive follow-up was not delivered to all parents of children participating in the NCMP, the most common set of reasons was the combination of cost-funding and staff capacity to implement (n 16); see Fig. 4, Panel C.
Services
Seventy-four (80 %) of the participating LGA reported having any services (as part of healthy weight care pathways; Tier 1, 2, 3 and universal) available for parents or carers and their Reception year and Year 6 children. Only four LGA representatives reported that there is no service available, which was primarily due to cost implications (one representative was not sure). The available services were offered to children with various NCMP weight classification and the classifications were often combined. Of the 74 LGA that reported available services, 32 (35 %) indicated they offered combined access for children identified within the Overweight and Very Overweight ranges, while 20 (22 %) offer combined access to all weight groups; see Fig. 5. Eleven (12 %) LGA offered services to combination of all weight classifications except for children identified within the Healthy Weight range.

Fig. 5 Which children are eligible to attend available services?
LGA who provide services but do not target all weight groups (n 54) were asked for the reasons they restrict service access. Supplemental Figure 3, Panel A shows that the most common reason was lack of funding (NR = 6) and other (NR = 11), for example, ‘Underweight children are supported through their GP and not our Healthy Lifestyle service’. Supplemental Figure 3, Panel B extends to LGA which indicated they do not provide any services at all. This was relevant to four out of five LGA and the cost of funding was indicated three times.
Comparing the PHE regions
Finally, we show the selection of the key plots across all phases of the NCMP; however, this time we also add a split between PHE regions (London, Midlands and the East, the South, and the North) to allow comparison between parts of England in the participating LGA. Supplemental Figure 4 shows how is the measurement information with opt-out and the result feedback delivered (A and B), and which children are usually targeted in proactive follow-up and eligible for services (C and E). There are no remarkable regional differences in how the NCMP is delivered in the regions.
Discussion
The current study aimed to explore the delivery of the NCMP by LGA across England. The study has highlighted the varied practice, responsibilities, and ultimately, experiences that parents and families have who participate in the NCMP.
The current study identified a high proportion of LGA commission the NCMP to provider organisations, modify the PHE specimen result letter and include further information about local services. This, as well as the varied modes of delivering the NCMP, and in some instances not performing some of the recommended NCMP mechanisms (e.g. proactive follow-up) due to factors such as cost, raises questions about the comparable nature of the NCMP and the ability to highlight good practice that can be translated to other LGA(3).
Furthermore, methods of delivering the pre-measurement information varied; the most common was in children’s school bag. Most LGA alter the PHE specimen letter, with a very small percentage reporting that they had never seen it.
Most result feedback is posted as letters to parents, with few sending the letter via children’s school bag which does not adhere to PHE guidance(3). Alongside the result feedback, most LGA include attachments such as healthy eating guides, information about local services and Change4Life leaflets. Many LGA do not provide result feedback to all children, and in most cases, parents of children identified within the Healthy Weight range do not receive the feedback.
The most common reason that LGA do not provide proactive follow-up and do not have child weight management services was cost. Regrettably, the provision of the NCMP relies on printed materials and electronic delivery methods remain underutilised, as evidenced by our results. We believe that additional support and guidance need to be available for LGA to help them implement electronic delivery methods and thus reduce the cost of the NCMP.
Future work should explore the impact of the varied practice including the modifications to the NCMP result feedback. The feedback element of the NCMP has been criticised as a cause of distress to parents(Reference Nnyanzi, Summerbell and Ells7,Reference Gainsbury and Dowling13,Reference Gillison, Beck and Lewitt26) . A paucity of research has explored parents’ experiences to the varied feedback content and given the potential impact of this NCMP element, further work is warranted. One study that has explored the impact of NCMP feedback reported that the letters can be used to nudge parents, leading to a small increase in service uptake(Reference Sallis, Porter and Tan14).
Research suggests that parents have various preferences regarding the feedback and these should be considered within NCMP feedback (e.g., timing, terminology, literacy level or tone)(Reference Ames, Mosdøl and Blaasvær12). Since LGA are free to modify the feedback information, there should be a discussion about how to best share the feedback. Unfortunately, this topic appears to be underestimated in the available guidelines(3,Reference Chadwick, Clark and Gahagan27) . For example, the conversational framework guidelines state that ‘A parent’s beliefs and culture will influence how they respond to NCMP feedback’(Reference Chadwick, Clark and Gahagan27) (p. 13). While the guidelines acknowledge that parents may experience distress, it does not recognise that the content of the letters or the way the feedback is shared may be the cause of this and thus does not provide support to LGA on the best practice that could be followed taking local arrangements into account(Reference Chadwick, Clark and Gahagan27).
This study is not without limitations. The current sample of LGA does not cover all potential variations of the NCMP implementation. From all possible LGA (152), 92 agreed to participate in the survey. While we believe the study brings representative findings given the response rates across the four PHE regions varied from 53 to 69 %, the non-probability sampling technique is a limitation that should be considered when interpreting the study findings. Additionally, some LGA may not have been comfortable sharing their data or were experiencing changes which meant they were unable to provide data at the time of the study. Finally, the survey focused on the perspective of LGA representatives; we did not explore the perspectives of other stakeholders such as schools, providers or parents in this survey.
The study collected data between February 2018 and May 2018. On 14 February 2018, PHE introduced the new version of the result feedback (i.e. letters) which replaced the version primarily used between years 2014 and 2017, but not all LGA have been able to use the latest version(3). Additional updates to the operational guidelines were introduced in the same year; therefore, some of the practical and local changes may have happened in the following year due to the introduced changes(3).
The study findings highlight that NCMP delivery is varied, and that further guidance regarding standards of best practice would help LGA to find the most suitable localisation from the various options that exist. Additionally, since the majority of LGA work with external providers, further guidance should be available to support these collaborations. We believe that each part of the NCMP process should be treated as a longer-term relationship building between parents, LGA and potential service providers. After all, the relationship between provider and parents is one of the key elements of addressing childhood obesity(Reference Sjunnestrand, Nordin and Eli28). Finally, only a limited number of LGA currently benefit from electronic delivery of the NCMP, which may support with funding challenges.
In conclusion, this study provides the first insights into the design implementation and delivery of the NCMP in England. Key findings show that there is varied practice, and therefore experiences, for parents and children who participate.
Acknowledgements
Acknowledgements: The NCMP team at Public Health England for their support with data collection. Financial support: Not applicable. Conflict of interest: None. Authorship: MČ, principal investigator, writing, data collection and analysis. SWF, writing and reviewing. RT, writing and reviewing. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Leeds Beckett University ethics committee. Written informed consent was obtained from all participants.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020004991








