At present, obesity is a major public health concern. According to recent reports, at least 400 million adults are obese and 1·6 billion are overweight worldwide(1). Although the prevalence of obesity has reached 50 % in developed countries, many developing countries face this health problem, especially among women(Reference Low, Chin and Deurenberg-Yap2). The prevalence of obesity among Iranian women has increased dramatically to 20·8 % from 16·5 % over 3 years (from 1998 to 2001, according to a national study)(Reference Azizi, Azadbakht and Mirmiran3). However, the pattern of body fat distribution is a more important determinant of chronic diseases than general obesity(Reference Wei, Gaskill and Haffner4, Reference Esmaillzadeh, Mirmiran and Azadbakht5). In Iran, it has been reported that 67 % of women and 33 % of men above 20 years of age are centrally obese(Reference Azadbakht, Mirmiran and Azizi6, Reference Azadbakht, Mirmiran and Shiva7). A study of secular trends in central fat accumulation in Iran showed a 6 % increase among men and a 9 % increase among women in central adiposity between 1998 and 2002(Reference Azizi, Azadbakht and Mirmiran3).
Various dietary and non-dietary factors are related to obesity and abdominal adiposity(Reference Azadbakht and Esmaillzadeh8–Reference Jaffiol10). Among dietary factors, the consumption of many nutrients, foods and food groups is reported to be associated with this health problem(Reference Wang and Beydoun11–Reference Azizi, Mirmiran and Azadbakht14). Although paying attention to diet components is important, there are many undiscovered compounds in foods, and possible interactions among nutrients, which suggest using indices of the whole diet and not only a single component(Reference Hu15–Reference Kant17).
To our knowledge, there is little emphasis on overall diet characteristics and obesity in literature in the field of nutrition. Dietary diversity score (DDS) is an indicator for assessing overall diet(Reference Hatloy, Torheim and Oshaug18). Eating a more varied diet is associated with higher intake of macro- and micronutrients, as well as higher nutritional adequacy and diet quality(Reference Azadbakht, Mirmiran and Azizi19–Reference Steyn, Nel and Nantel22). Furthermore, DDS might be associated with the prevalence of chronic diseases such as metabolic syndrome(Reference Azadbakht, Mirmiran and Azizi23), cancers(Reference McCollough, Feskanich and Stampfer24) and CVD(Reference Azadbakht, Mirmiran and Esmaillzadeh25, Reference Wahlqvist, Lo and Myers26). Some earlier studies reported protective effects against non-communicable diseases in more varied diets(Reference Azadbakht, Mirmiran and Azizi23–Reference Miller, Crabtree and Evans27). Although higher variety score of a diet is associated with increased fibre intake, vitamin C and calcium, which are inversely correlated to obesity(Reference Mirmiran, Azadbakht and Azizi21), eating a more varied diet is usually associated with higher energy intake(Reference Azadbakht, Mirmiran and Azizi19, Reference Raynor and Epstein28–Reference Raynor, Jeffery and Tate30). Hence, the main question regarding the association between DDS, obesity and abdominal adiposity still remains, and it will be interesting to be assessed. Therefore, we conducted a cross-sectional study on female youth to determine the association between DDS, obesity, overweight and abdominal adiposity. We also found an association between the diversity of each food group and overweight, obesity and abdominal adiposity.
Materials and methods
Subjects
This cross-sectional study was conducted for a representative sample of female students, aged 18–28 years, from Isfahan University of Medical Sciences in Iran, selected by the multi-stage cluster random sampling method. When choosing the sample for the study, we first considered all the schools at Isfahan University of Medical Sciences, and departments were randomly chosen from each school. From each department some students were chosen randomly from the list of students in the records. In order to select the students in this way, we considered all the students in different stages of socio-economic status. Using this stratified multi-stage cluster random sampling method, both students who were living in dormitories and those who were living with their families were considered in the sample.
A total of 344 female students were invited to participate in the present study, of whom 308 agreed to participate. The response rate was 89 %. Nineteen students were excluded because of having consumed medications that affected their weight or because they reported their energy intake outside the range of 3347–17 573 kJ/d (800–4200 kcal/d). Therefore, the final analysis has been conducted on 289 students. Written informed consent was obtained from each participant. The study was approved by the research council of the School of Health, Isfahan University of Medical Sciences.
Assessment of dietary intake
Dietary intake was evaluated by a 168-item semi-quantitative FFQ. All the questionnaires were administered by trained dietitians. The FFQ consisted of a list of foods with a standard serving size. Participants were asked to report their frequency of consumption of each food item during the previous year on a daily (e.g. bread), weekly (e.g. rice and meat) or monthly (e.g. fish) basis. Portion sizes of consumed foods were converted to grams using household measures(Reference Ghaffarpour, Houshiar-Rad and Kianfar31). Each food and beverage was then coded according to the prescribed protocol and analysed for content of energy and the other nutrients using Nutritionist III software (version 7·0; N-Squared Computing, Salem, OR, USA), which was designed for Iranian foods. The reported frequency for each food item was then converted to a daily intake. Validity and reliability of the FFQ have been assessed previously(Reference Azadbakht, Mirmiran and Esmaillzadeh32).
Assessment of anthropometric measures
Weight was measured by using digital scales, with the participants wearing minimal clothing and no shoes, and was recorded to the nearest 100 g. Height was measured by using a tape measure while the participants were standing in a normal position with no shoes. BMI was calculated as weight divided by the square of height (kg/m2). To measure waist circumference (WC), the narrowest level was considered and the hip circumference was measured at the maximum level over light clothing. Both of these procedures were carried out by using non-stretchable tape, without any pressure applied to the surface of the body; measurements were recorded to the nearest 0·1 cm. Whenever we could not define the narrowest area of the waist, because of a large amount of abdominal fat or extreme thinness, WC was measured immediately below the end of the lowest rib(Reference Wang, Thornton and Bari33). All the measurements were taken by the same person to reduce chances of error.
Assessment of other variables
Sociodemographic and physical status information was obtained from the questionnaires. Data on physical activity were collected based on the interviews and expressed as metabolic equivalent hours per week (MET-h/week)(Reference Ainsworth, Haskell and Whitt34).
Definition of terms
Obesity and overweight were defined(Reference Stunkard and Wadden35) as BMI ≥ 30 kg/m2 and BMI = 25 to <30 kg/m2, respectively. Abdominal adiposity was defined as WC > 88 cm(36).
Dietary diversity score
We used the method described by Kant et al.(Reference Kant, Schatzkin and Ziegler37, Reference Kant, Schatzkin and Ziegler38) for scoring dietary diversity. This procedure was based on five groups, bread-grains, vegetables, fruits, meats and dairy, based on the food groups introduced by the US Department of Agriculture (USDA) Food Guide Pyramid(39). We considered this food group category because the USDA Food Guide Pyramid provides a balanced healthy diet(39). Furthermore, adherence to this guideline is associated with higher diet quality and mean adequacy of nutrient intake(Reference Mirmiran, Azadbakht and Azizi40). The main groups mentioned were divided into twenty-three subgroups. These subgroups show the dietary diversity across the groups of the Food Guide Pyramid(39). The bread-grain group was divided into seven subgroups (refined bread, biscuits, macaroni, whole grain bread, corn flakes, rice and refined flour). Fruit was divided into two subgroups (fruit and fruit juice, berries and citrus), and vegetables was divided into seven subgroups (vegetables, potato, tomato, other starchy vegetables, legumes, yellow vegetables and green vegetables). There were three subgroups of meat (red meat, poultry, fish and eggs) and also for dairy (milk, yoghurt and cheese). To be counted as a ‘consumer’ for any of the food group categories, a respondent had to consume at least one-half of the serving in a day as defined by the Food Pyramid quantity criteria. Each of the five broad food categories receive a maximum diversity score of 2 out of the 10 possible score points. Total score was the sum of the scores of the five main groups. The maximum and minimum scores of total dietary diversity were between 0 and 10. To calculate the diversity score of each food group, the abovementioned method was used and the subgroups were the same. The maximum and minimum scores of diversity were 0–2 within each food group. To calculate the diversity score of each food group, we considered a participant a consumer of a food group if he or she consumed at least one-half of the serving of any subgroup in a day as defined by the Food Pyramid quantity criteria. For example, in the bread-grain group, if a person consumed whole grain and macaroni and biscuits, his or her score was calculated as (3 ÷ 7) × 2 = 0·85. Therefore, the diversity score of the bread-grain group is 0·85.
Statistical methods
The Statistical Package for Social Science statistical software package version 9·05 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Cut-off points for quartiles of DDS were calculated and participants were categorised based on quartile cut-off points: first, <3; second, 3–<5·5; third, 5·5–<8·5; and fourth, ≥ 8·5. Significant differences in general characteristics across quartile categories of DDS were investigated using the ANOVA test. If there was a significant main effect, the Bonferroni test was used to detect pairwise differences. The χ 2 test was used to detect any significant differences in the distribution of participants across quartile categories of DDS with regard to qualitative variables. All correlation coefficients reported were calculated as Pearson correlation coefficients. To determine the association of DDS with obesity and abdominal adiposity, we used multivariable logistic regression. The model was controlled for age (years), energy intake (kJ/d) and physical activity. For abdominal adiposity risk assessment, a second model was also provided in which BMI was further adjusted in addition to the mentioned variables. In all multivariate models, the first quartile of DDS was considered as a reference. The Mantel–Haenszel extension χ 2 test was performed to assess the overall trend of an increasing quartile of DDS associated with an increasing or decreasing likelihood of being classified as high risk. To evaluate the association between energy intake and DDS, the linear regression model was used, and multivariable logistic regression was used to determine the association of the diversity of each food group, obesity, overweight and abdominal adiposity.
Results
Mean and standard deviation of DDS were 6·78 and 1·12, respectively (minimum: 4·08 (sd 1·25); maximum: 8·31 (sd 1·55)). When we calculated each group diversity score separately, the maximum and minimum scores of diversity were related to the fruit (1·78 (sd 0·68)) and bread-grain (0·76 (sd 0·33)) groups, respectively. Mean and standard deviation of age, physical activity status and anthropometric measures, as well as the distribution of participants with regard to obesity and abdominal adiposity across quartile categories of DDS, is shown in Table 1. Participants in the lower category of DDS were younger and had higher values of anthropometric measures than those in the upper category. The prevalence of obesity was lower among those in the upper category of DDS than those in the lower category. Age and energy-adjusted means for dietary variables across quartile categories of dietary diversity score are presented in Table 2. A higher DDS was associated with a healthier diet, with those in the upper category also consuming less fatty food, and refined grain and more fruit, vegetables and whole grain. The higher DDS was positively associated with total intake of dietary fibre (r = 0·33), calcium (r = 0·41) and vitamin C (r = 0·38).
Table 1 Characteristics of the female youths by quartiles of dietary diversity score
WHR, waist-to-hip ratio; MET-h/week, metabolic equivalent hours per week.
*Quartile cut-points of DDS are as follows: first, <3; second, 3 to <5·5; third, 5·5 to <8·5; fourth, ≥ 8·5.
†P < 0·01 compared to the first quartile.
Table 2 Dietary intakes of female students in Isfahan University of Medical Sciences by DDS quartile categoriesFootnote *
DDs, dietary diversity score.
* Quartile cut-points of DDS are as follows: first, <3; second, 3 to <5·5; third, 5·5 to <8·5; fourth, ≥ 8·5.
† Reported food intakes were adjusted for age and total energy intake.
‡ Includes apples, oranges, bananas, peaches, grapes, strawberries, pears, watermelon, grapefruit, prunes, pomegranates, kiwi, persimmons, raisins, figs, coconuts, apricots and sweet lemon.
§ P < 0·05 compared to the first quartile.
∥ Includes onions, cucumbers, lettuces, carrots, cauliflower, Brussels sprouts, kale, cabbage, spinach, mixed vegetables, corn, green beans, green peas, peppers, beets, potatoes, tomatoes, broccoli and celery.
¶ Includes beef, liver, chicken hearts and kidneys, meat, poultry, tuna fish and other fishes.
** Includes dark breads (sangak, barbari and taftoon), barley bread, cornflakes, bulgur and germs.
†† Includes white breads (lavash and baguette), noodle, pasta, rice, toasted bread, milled barley, sweet bread, white flour, starch and biscuits.
‡‡ Includes milk, yoghurt and cheeses.
§§ Includes hamburger, sousages, processed meats and pizza.
Multivariate-adjusted OR and 95 % CI for having obesity and abdominal adiposity across quartile categories of dietary diversity score are presented in Table 3. The probability of overweight and obesity, as well as abdominal adiposity, decreased with quartiles of DDS. OR of having abdominal adiposity became weaker after adjusting for BMI, but still remained significant.
Table 3 Multivariate-adjusted OR and 95 % CI for having abdominal adiposity, overweight and obesity across quartile categories of DDS
DDS, dietary diversity score.
*Quartile cut-points of DDS are as follows: first, <3; second, 3–<5·5; third, 5·5–<8·5; fourth, ≥ 8·5.
†Adjusted for age and physical activity.
‡Adjusted for age, physical activity and total energy intake.
§Adjusted for BMI.
OR for having obesity and abdominal adiposity across quartiles of vegetable diversity score is shown in Fig. 1. Risk of obesity and abdominal adiposity was significantly lower among those in the highest quartile of the vegetable diversity score (P < 0·04 and P < 0·03, respectively). The result was the same in the case of the diversity score of fruit and obesity (P < 0·04), as well as abdominal adiposity (P < 0·04). There was no significant association between the bread-grain group and the prevalence of obesity and abdominal adiposity. This was the case for the diversity score of both the meat group and the dairy group.
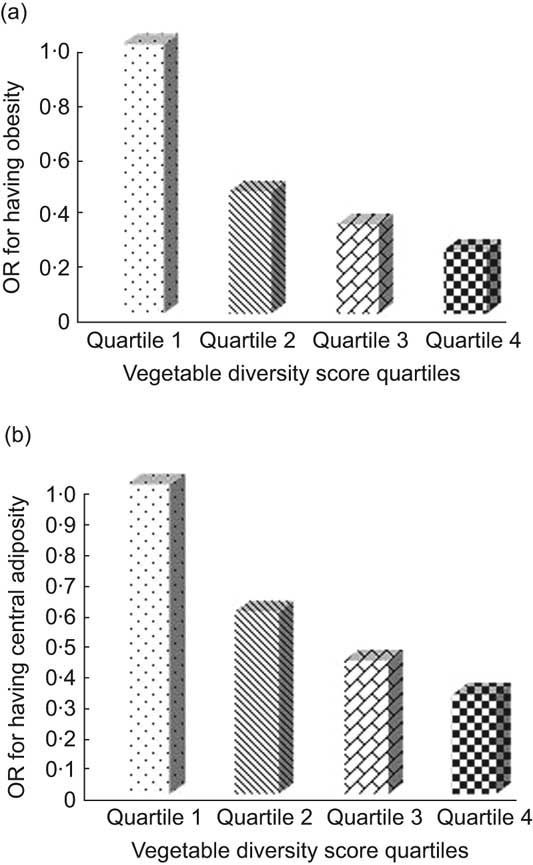
Fig. 1 (a) OR for having obesity (P for trend = 0·04) and (b) abdominal adiposity (P for trend = 0·03) across quartiles of vegetable diversity score
There was a significant and positive correlation between DDS and total energy intake in the present study (R 2 = 0·40; P < 0·05).
Discussion
The present study, conducted for a representative sample of Iranian female university students, showed an inverse association of DDS with obesity and abdominal adiposity. We used this population because there is little nutritional information specific for this group in Iran. Furthermore, data on dietary characteristics and abdominal adiposity are rare. Moreover, we are not aware of any nutritional study on female students of Isfahan University of Iran. As DDS reflects a holistic view of the diet, it is a useful indicator for assessing the correlations between diet and diseases.
The results of the present study showed a direct association between energy intake and DDS. Some earlier studies indicated a direct association between DDS and energy intake(Reference Raynor and Epstein28, Reference Raynor, Jeffery and Tate30). They reported that by increasing DDS, energy intake was also increased. Torheim et al.(Reference Torheim, Ouattara and Diarra41) indicated a positive correlation between energy intake and DDS, as well as variety of different food groups in Mali. The results for Tehranian men were the same(Reference Azadbakht, Mirmiran and Azizi19). Indeed, among Tehranian men energy intake explained 48 % of the variance in the mean probability of nutrient adequacy in the regression model(Reference Azadbakht, Mirmiran and Azizi19). Foot et al.(Reference Foote, Murphy and Wilkens42) also revealed the role of energy in the association between variety and the mean probability of adequacy in a linear regression model. According to their results, energy was an important component of the regression model. This might prove to be a limitation for a variety of indices in health promotion programmes. The new recommendations advocate consumption of a varied diet while staying within energy needs(Reference Esmaillzadeh and Azadbakht43).
In the present study, increase in energy intake was related to increasing energy intakes of fruit, vegetable and whole grains. Therefore, the increasing energy intake, following the increase in DDS, was due to increasing consumption of healthy food groups. Increasing DDS is not always associated with increasing weight, because this index can be increased by consuming more different types of healthy and low-energy-dense food groups such as vegetables, whole grain and fruit. In fact, there is a large variety of vegetables and fruits available in Iran, but refined grain products and meat- or fat-containing commercial products are limited. Therefore, increasing DDS in the Iranian population is mainly achieved by increasing the vegetable or fruit diversity score. In the present study, women who had higher DDS consumed more fruits, vegetables, dairy and grain, which might be correlated with lower incidence of obesity and abdominal adiposity.
Although DDS was correlated with energy intake, after adjusting the total energy intake it was negatively correlated with overweight, obesity and abdominal adiposity. Therefore, another factor such as energy density might play a role in this regard. In fact, by increasing DDS, vegetable, fruit and whole grain intake was also increased. All these groups had low energy density. Therefore, it is suggested that future studies report the correlation between DDS and energy density.
Although DDS was designed according to the food guide pyramid and this pyramid does not control energy intake, those in the top quartile of DDS had lower risk for obesity and overweight, which might be related to their specific choices for increasing the diversity score of their diet. Therefore, they increased their dietary diversity score with low-energy-dense items.
In the present study, diversity scores of vegetable and fruit groups were separately correlated with obesity and abdominal adiposity. None of the earlier studies focused on the diversity score of each food group. This might be considered as a separate analysis that cleared the more specific association between the diversity of food groups and obesity.
Earlier studies indicated that dairy consumption(Reference Azadbakht, Mirmiran and Esmaillzadeh32), hydrogenated vegetable oil(Reference Esmaillzadeh and Azadbakht43), fruit and vegetable intake(Reference Esmaillzadeh, Kimiagar and Mehrabi44) and whole grain ingestion(Reference Esmaillzadeh, Mirmiran and Azizi45) are associated with metabolic syndrome, one of the important features of which is abdominal adiposity.
Those in the top quartile of DDS had the lowest level of fast food intake. Fast foods are one of the major sources of trans fat intake, which is mainly correlated with abdominal adiposity(Reference Dorfman, Laurent and Gounarides46). Fast food consumption might also be correlated with general obesity, abdominal adiposity and other chronic diseases, mainly because of high content of energy and trans fat(Reference Azadbakht and Esmaillzadeh9). An analysis of Iranian fast foods and commercial oils also indicated a high amount of trans fats in these kinds of products(Reference Asgary, Nazari and Sarrafzadegan47, Reference Asgary, Nazari and Sarrafzadegan48). Among the university student population, those who followed a healthier diet had a higher DDS, which was in contrast to the findings of some other studies(Reference Raynor and Epstein28, Reference Raynor, Jeffery and Tate30). However, in line with the results of the present study, Kant et al.(Reference Kant and Graubard49) indicated that DDS was a negative predictor of BMI. In their study, DDS was also an important index for predicting disease.
The results of the present study are not surprising because earlier studies in Iranian populations also indicated an inverse association between this index and metabolic syndrome(Reference Azadbakht, Mirmiran and Azizi23), as well as cardiovascular risk factors(Reference Azadbakht, Mirmiran and Esmaillzadeh25, Reference Wahlqvist, Lo and Myers26). It seems that DDS among the Iranian population is a good indicator for health, and increasing DDS is favourably associated with metabolic abnormalities. Other studies in other populations also indicated that diverse diet could protect against cancer(Reference Fernandez, Negri and La Vecchia50); hypertension(Reference Miller, Crabtree and Evans27) and macrovascular diseases among diabetic patients(Reference Wahlqvist, Lo and Myers26). Earlier studies mostly focused on the relationship between cancer and DDS(Reference McCollough, Feskanich and Stampfer24, Reference Fernandez, Negri and La Vecchia50, Reference La Vecchia, Munoz and Braga51), whereas the present study provided a possibility to see the relationship between DDS and obesity. Compared to earlier studies on the association between DDS and obesity, the age group and characteristics of the population of the present study (female, university students) was different from other populations(Reference Raynor and Epstein28, Reference Raynor, Jeffery and Tate30).
DDS is an index for assessing dietary pattern. Even dietary interventions in a population can affect this score(Reference Sarrafzadegan, Azadbakht and Mohammadifard52). Different dietary patterns might be associated with obesity and abdominal adiposity among different populations(Reference Esmaillzadeh and Azadbakht53). Therefore, focusing on DDS and excluding other aspects of dietary patterns in relation to obesity is questionable.
In the present study, even after adjusting for BMI, DDS was inversely correlated with abdominal adiposity. Although BMI and WC have a high colinearity, this model remained significant even after adjustment.
One of the important strengths of the present study was its consideration of the potential confounders that were adjusted in the reported models of the logistic regression. Potential effects of age, total energy intake and physical activity were adjusted in our analysis.
There are several limitations to the study. The data we used were cross-sectional, and hence a prospective association remains to be identified. Misclassification of the study participants, due to the use of an FFQ, was a concern in our study. Although we tried to control for known confounders, residual confounding cannot be excluded in our findings. The small sample size of the present study was another limitation. However, despite the small sample size, there are few studies in this regard, especially from Middle Eastern countries. Therefore, conducting this research even in a small sample may evoke new ideas in the field of DDS and chronic diseases. The prevalence of obesity was low among the female students. Therefore, it was more effective to analyse the overweight and obese participants together in one model and not in separate models. However, in the present study using tertiles of DDS instead of quartiles was not a useful method to increase cell numbers. It is suggested that future studies should mostly focus on the more prevalent obese groups to determine the association between DDS and obesity. We used a multi-stage randomised sampling method to choose the sample size of the current study. Hence, in this way we tried to have a representative sample of female students in our study. As some of the students were living in the school dormitory, we cannot extrapolate the results of the present study to all the female students in the same age group, and the results are limited to female university students. Furthermore, as the population of the present study was female university students in medical sciences and their level knowledge was higher than others in the same age group, we cannot generalise these results to all the women in this age group. Therefore, there are some concerns regarding the external validity of the current study. The classification of subgroups was based on the USDA Food Guide Pyramid. There is no emphasis on the whole grain intake in this pyramid. Automatically, the bread-grain subgroup classification did not consider the weight of refined and whole grains in its classification. The bread-grain group was heavily weighted for refined grains if a participant ate at least half a serving of refined items in biscuits, cornflakes, macaroni and rice per day. However, the whole grain biscuits and macaroni and whole flour and whole grain cornflakes will be calculated in the mentioned subgroups as well. This means that not only whole grain bread consumption, but also whole grain biscuits, cornflakes or macaroni can increase the diversity score of the bread-grain group. In this way, we cannot say that only whole grain bread among the whole grain items has a role in increasing DDS.
In addition to conducting epidemiological studies, specifically clinical trials, longitudinal trials(Reference Azadbakht, Atabak and Esmaillzadeh54) might determine the effect of consuming more varied diet on weight change. However, increasing the variety score of fruit, vegetable and whole grains could be further emphasised. It is suggested that future studies clarify the association between this score and some possible mediators in the association between DDS and obesity, such as inflammatory factors. However, earlier studies showed some association between food consumption and inflammation(Reference Azadbakht and Esmaillzadeh55, Reference Esmaillzadeh and Azadbakht56). In addition to considering the association between food and inflammatory markers, paying attention to the dietary pattern and some scores related to dietary variety and inflammation might be useful in describing the association between diet and obesity or abdominal adiposity.
In conclusion, the present study suggests that dietary diversity score is associated with lower risk of obesity and abdominal adiposity. Further prospective investigations should be carried out to confirm this finding.
Acknowledgements
This study was supported by a grant from the School of Health, Isfahan University of Medical Sciences. The authors have no conflict of interest. The authors are grateful the participants of the study for their enthusiastic cooperation, and they express their gratitude to the research council of the School of Health, Isfahan University of Medical Sciences for financial support. L.A. and A.E. designed the study, collected and analysed the data, and wrote the manuscript.
Appendix
The mean and sd of the diversity score within food groups among female students of the university