Sodium, mostly in the form of sodium chloride or salt, is used to enhance flavour, preserve and improve processing in a wide range of foods. However, dietary salt consumption in many countries, including New Zealand, significantly exceeds the WHO recommended maximum intake of 5 g/d for adults(1). Current estimates suggest that the mean salt intake for New Zealanders is about 9 g/d (CD Thomson and AJ Colls, unpublished results), considerably more than the recommended upper limit for New Zealand adults of 6 g/d (or 2300 mg Na/d)(2). The adverse health effects of excessive dietary sodium have been well documented. Observational and intervention studies have shown a consistent causal association between high sodium intake and elevated blood pressure(Reference Stamler, Rose and Stamler3, Reference Vollmer, Sacks and Ard4), with consequent increased risk of CHD and stroke(Reference He and MacGregor5). A high salt intake is also associated with an increased risk of kidney disease, gastric cancer and osteoporosis(Reference He and MacGregor6). US estimates suggest moderating Americans’ sodium intake by as little as 1200 mg/d could reduce annual deaths by 44 000 and save between $US 10 billion and $US 24 billion in annual health-care costs(Reference Bibbins-Domingo, Chertow and Coxson7).
Processed foods account for about three-quarters of sodium intake in Western diets, with a further 10–15 % added in cooking and at the table(Reference Mattes and Donnelly8–10). Changing food composition, and thus consumers’ food supply, would offer the greatest opportunity to reduce population sodium intake(Reference He and MacGregor6, Reference Mattes and Donnelly8). Reducing the amount of sodium in processed food has formed the cornerstone of salt reduction campaigns, and many food manufacturers have committed to sodium reduction programmes to this end(Reference Wyness, Butriss and Stanner11). However effective nutrition labelling has also been shown to be a cost-effective intervention to improve population nutrition(Reference Campos, Doxey and Hammond12). Labelling also enables consumers to have greater control over their nutrition in an environment that promotes unhealthy food choices.
The UK Food Standards Authority's salt reduction campaign launched in 2003 included the publication of sodium targets for a wide range of foods, and has resulted in a 10 % reduction in population mean salt intake from 9·5 g/d in 2000/01 to 8·6 g/d in 2008. The campaign also included a public awareness campaign focusing on educating consumers about the adverse health effects of a high salt intake, supported by education about how to interpret food labels, enabling consumers to identify low-salt options(Reference Wyness, Butriss and Stanner11). Successful interventions in Finland have also attempted to shape demand by making it easier for consumers to differentiate between products with high and low sodium concentrations(Reference Pietinen, Valsta and Hirvonen13).
Regulators in many countries have used nutrition labels to provide information that could assist consumers to make healthier food choices. Recent attempts have sought to mandate labels that enhance consumer understanding and research has focused on identifying which label formats communicate information most effectively(Reference Malam, Clegg and Kirwan14). The Food and Drug Administration and the Institute of Medicine in the USA have recently called for further research to identify the best way to communicate nutritional information to consumers through food labelling(15). The European Union recently decided to mandate nutrition labelling of pre-packed foods, but decided against requiring a Traffic Light (TL) label in favour of a Percentage Daily Intake (PDI) model after intense lobbying by the food industry(16).
There is ongoing debate about whether to use the term ‘sodium’ or ‘salt’ on food labels. The USA and Canada widely use the term ‘sodium’ in a public health context; however public health campaigners in the UK and Australia have generally chosen to use ‘salt’ as a term that people are likely to be more familiar with and this is reflected in the use of ‘salt’ in nutrition claims. The European Union has also recently decided to use the word ‘salt’ in preference to ‘sodium’ in front-of-pack labels. In New Zealand and Australia there is some confusion among consumers about the relationship between sodium and salt in food labels(Reference Gilbey and Fifield17, Reference Grimes, Riddell and Nowson18). Although the sodium and salt are not the same (1 g sodium = ∼2·5 g salt) we have used the terms interchangeably in the present paper as about 90 % of sodium intake is from salt, and this approach reflects how the terms appear in existing label and claim formats.
We tested three labelling formats, illustrated in Fig. 1. The Nutrition Information Panel (NIP) has been mandatory in New Zealand since 2002, and is highly numeric. Several food manufacturers have voluntarily introduced front-of-pack PDI labels in New Zealand that they believe complement the mandatory NIP(19) while the TL label was developed in 2007 by the Food Standards Agency in the UK to communicate fat, saturated fat, salt and sugar levels of food and is not currently in use in New Zealand. The TL label has no numeric information, but instead has low, medium and high nutrient categories, using the traffic light to convey the appropriate category grading in a highly visual way. Both front-of-pack labels (PDI and TL) have greater visual impact than the NIP, which is usually small and situated on the back or side of a food packet.
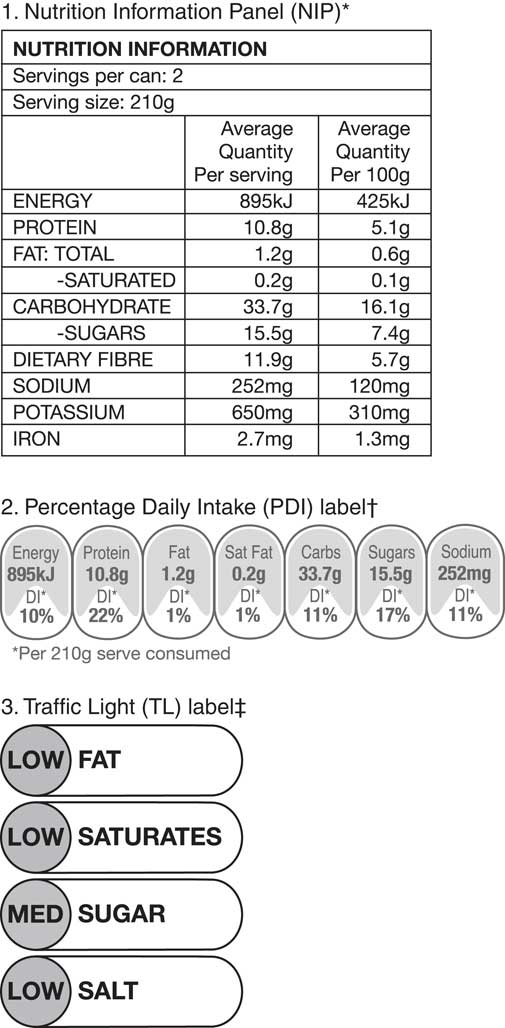
Fig. 1 Examples of the three labelling formats used. *The NIP is highly numeric, situated on back or side of the pack, and has been mandatory in New Zealand since 2002. †The PDI label was introduced voluntarily by several food manufacturers; it is a front-of-pack label with greater visual impact, although still highly numeric. ‡The TL label contains no numeric information; it is a front-of-pack label and has the highest visual impact, with green, amber and red colours representing low, medium and high levels, respectively. The TL label was developed by the UK Food Standards Agency in 2007 and is not currently in use in New Zealand
To explore alternative methods of communicating information about sodium content to consumers, we used a choice modelling study to compare how three different nutrition label formats and two nutrition claims influenced consumers’ choice behaviour. Stated choice experiments simulate actual behaviour and enable the importance of attributes to be estimated rather than assumed. Given that consumers often overestimate their use of nutritional information(Reference Tanner and Carlson20, Reference Ni Mhurchu and Gorton21), this methodology is particularly appropriate for estimating behaviours such as food purchasing, where self-reported behaviour may be affected by social desirability bias. We tested three key hypotheses:
1. Consumers’ ability to discriminate between high- and low-sodium foods would increase as nutrition labels become less numeric and more visual.
2. Consumers with hypertension would have a greater awareness of the importance of sodium reduction for blood pressure control and so would demonstrate stronger discrimination between high- and low-sodium foods when these featured nutrition labels that were less numeric and more visual.
3. The persuasive effect of product nutrition claims would diminish as nutrition labels become less numeric and more visual.
Experimental methods
A random sample of participants was recruited from New Zealand's largest pre-existing national online research panel, which comprises over 125 000 New Zealanders. The sample had been pre-screened to include individuals who reported that a doctor had diagnosed them with hypertension. The sample was randomly selected from the online panel and recruitment closed once the required sample (600 people with hypertension and 300 people without hypertension) had been achieved. Respondents were asked to identify whether they were ‘mainly responsible’, ‘partly responsible’ or ‘not at all responsible’ for their household grocery shopping. Only those who indicated that they were mainly or partly responsible were able to continue with the remainder of the survey. Participants viewed choice sets containing three fictitious baked bean brands that differed in their sodium content, nutrition label format and nutrition claim (‘low salt’ or ‘reduced salt’). Levels of other nutrients did not differ between the high- and low-sodium products. The three label formats (illustrated in Fig. 1) included (i) an NIP situated on the back of the can, (ii) an NIP on the back and a PDI label on the front, and (iii) an NIP on the back and a TL label on the front.
Although each screen showed front-of-can images, participants could view the NIP by hovering their mouse over each image; this revealed a back-of-can image and simulated in-store behaviour, where consumers must make a conscious decision to view a product's NIP. The ‘low salt’ claim was not used on the cans with the high-sodium nutrition profile, as this would have been illogical and contrary to current New Zealand regulations. These state that a product can be labelled ‘low salt’ if it contains less than 120 mg Na/100 g, and labelled ‘reduced salt’ if the food has at least 25 % less sodium than the comparative reference food(22). Respondents viewed ten showcards, each featuring three images that varied according to the brand, nutrition profile, nutrition label and nutrition claim (see Table 1). They reviewed the images as though they were in a supermarket considering buying baked beans, then selected the brand they would buy if they had only the options shown available to them. The presentation order was randomized and balanced using a Latin square design(Reference Macfie and Bratchell23). Finally, participants answered questions relating to their use of food labels and provided basic demographic and health information, including whether they had ever been told they had high blood pressure.
Table 1 Experimental design
PDI, Percentage Daily Intake; TL, Traffic Light.
†The ‘low salt’ claim was not used with the high-sodium product since this would have created a logically inconsistent option, and would not be consistent with current New Zealand labelling regulations.
Statistical methods
Descriptive analyses and linear regression testing of associations between education and self-reported use of nutrition labels were performed using the STATA statistical software package version 11·1 (StataCorp LP, College Station, TX, USA). To examine the effects of different labelling formats including addition of a PDI or TL label and the presence or absence of a nutrition claim, we fitted a multinomial logit regression model that enabled the attributes’ main and interaction effects to be estimated, following the method of Chen and Kuo(Reference Chen and Kuo24), using the software GenStat version 13 (2010; VSN International Ltd, Hemel Hempstead, UK).
Results
Nine hundred and seventy-four people responded to the survey; of these, 678 had been pre-screened as having reported a history of diagnosed hypertension and 296 were from the general sample. In order to ensure real differences between groups, we excluded those in the pre-screened people with hypertension who answered ‘no’ to the question ‘Have you ever been told you have high blood pressure?’, leaving 500 in the group of people with hypertension. We excluded those in the general population sample who answered ‘yes’ to the question ‘Have you or someone you live with ever been told you have high blood pressure?’, leaving 191 participants in the group without hypertension.
People with hypertension were significantly older than those without, but there was no significant difference between the two groups with respect to education (Table 2). People with hypertension were significantly more likely than people without hypertension to report being on a special diet (61 % v. 41 %, respectively) and were more likely to have been advised to reduce the salt in their diet (58 % v. 20 %, respectively). People with hypertension were significantly more likely to report reading nutrition panels and were more likely to report reading the NIP on a new brand of food. However, there was no significant difference between the groups with respect to self-reported confidence in using the NIP to evaluate foods (Table 3).
Table 2 Demographic information of participants by hypertensive status: New Zealanders aged 18–79 years participating in an online nationwide research panel

†Participants were able to identify with more than one ethnic group, so adds to >100 %.
‡Using the t test for difference between means.
§Using the χ 2 test for difference in proportions.
Table 3 Self-reported label use of participants by hypertensive status: New Zealanders aged 18–79 years participating in an online nationwide research panel

†Using the t test for difference between means.
Linear regression analysis showed a statistically significant relationship between level of education and participants’ self-reported reading of NIP. As participants’ education level increased, they were more likely to report reading the NIP (β = 0·26, 95 % CI 0·14, 0·38, P < 0·001) but were less likely to report feeling confident about using the NIP (β = −0·16, 95 % CI −0·28, −0·04, P = 0·009).
To test the first and second hypotheses, we examined whether the different label formats affected respondents’ ability to differentiate between products with varying sodium content by hypertensive status. The multinomial logit model indicated that all three factors (label format, sodium level and nutrition claim) significantly affected choice, and there were significant interactions between these factors. However, most of these effects were the same for people with hypertension and those without hypertension. The only significant interaction between the groups and the factors was for the sodium level; while both groups favoured low-salt options, the preference was stronger in the group of people with hypertension (Wald statistic = 7·6, 1 df, P = 0·006).
Figure 2 shows the results of the multinomial logit model results for differences in label format, sodium level and hypertensive status. The corresponding numerical values are shown in Table 4. Consumers generally preferred the low-sodium product, and this effect was significantly stronger for people with hypertension than those without hypertension across all three label formats.
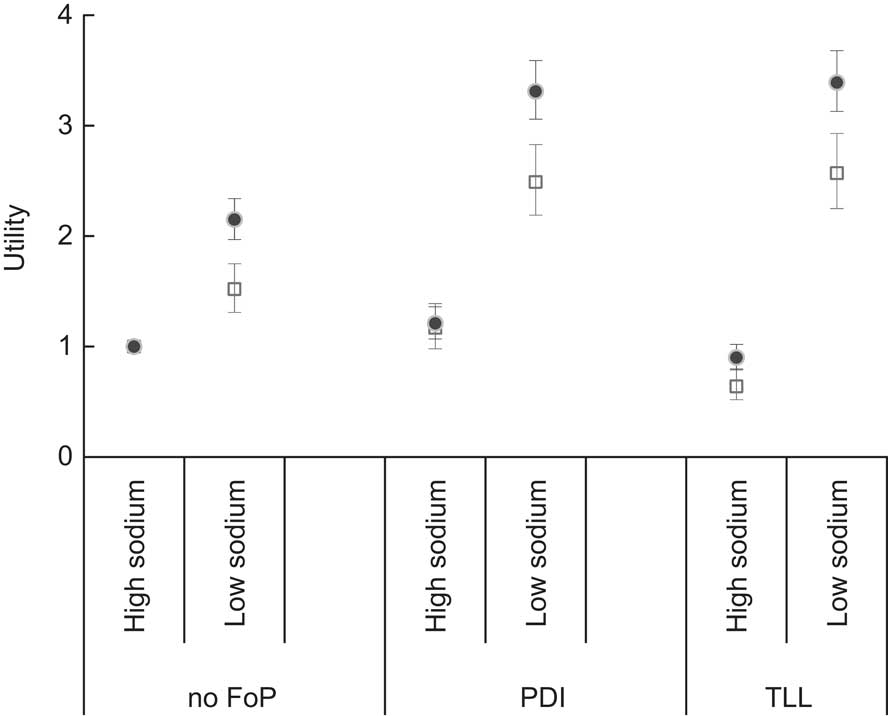
Fig. 2 Utility of different label formats (FoP, front-of-pack; PDI, Percentage Daily Intake; TL, Traffic Light) on choice behaviour for high- and low-sodium products, analysed by hypertensive status (□, not hypertensive, n 191; ●, hypertensive, n 500), among New Zealanders aged 18–79 years participating in an online nationwide research panel. Values are means, with 95 % confidence intervals represented by vertical bars
Table 4 Multinomial logit regression results for utility based on different label formats by hypertensive status: New Zealanders aged 18–79 years participating in an online nationwide research panel

FoP, front-of-pack; PDI, Percentage Daily Intake; TL, Traffic Light.
Results are presented with two statistical significance levels: P = 0·05 by convention and P = 0·01 to account for multiple comparisons.
Significantly different from 1·00 at *P = 0·05, **P = 0·01.
When no front-of-pack label was present, participants’ ability to discriminate between the profiles was relatively weak, especially for the people without diagnosed hypertension. The introduction of a PDI label significantly increased the utility of the low-sodium product for both groups: from 2·15 (95 % CI 1·97, 2·34) to 3·31 (95 % CI 3·06, 3·59) for the people with hypertension and from 1·52 (95 % CI 1·31, 1·75) to 2·49 (95 % CI 2·19, 2·83) for people without hypertension. However, the addition of the PDI label also increased the utility of the high-sodium product from 1·00 (reference category) for both groups to 1·21 (95 % CI 1·07, 1·36) for people with hypertension and 1·17 (95 % CI 0·98, 1·39) for those without hypertension, although this was significant only for the group with hypertension. The TL label also sharply increased the utility of the low-sodium product compared with the NIP only control to 3·39 (95 % CI 3·13, 3·68) for people with hypertension and 2·57 (95 % CI 2·25, 2·93) for those without diagnosed hypertension. However, the TL label reduced the utility of the high-sodium product to 0·90 (95 % CI 0·79, 1·02) for people with hypertension and 0·64 (95 % CI 0·52, 0·80) for people without diagnosed hypertension. Overall, the TL label resulted in the greatest discrimination between the profiles tested.
Figure 3 shows the results relating to our third hypothesis that ‘reduced salt’ or ‘low salt’ nutrition claims would interact with front-of-pack labels and reduce the influence these had on respondents’ choice behaviour. We tested whether there was an interaction between hypertensive status and nutrition claim effect using the test of fixed effects. This showed that there was no significant interaction between hypertensive status and claim effect (Wald statistic = 0·54, P = 0·765) or any of the interactions involving claim (Wald statistic = 0·01 to 0·67, P = 0·972 to 0·510). As there was no significant difference between the two groups, we examined the effect of adding a nutrition claim on the combined (people with and without diagnosed hypertension) sample for simplicity, and to reduce multiple comparisons. The results are shown in Table 5.
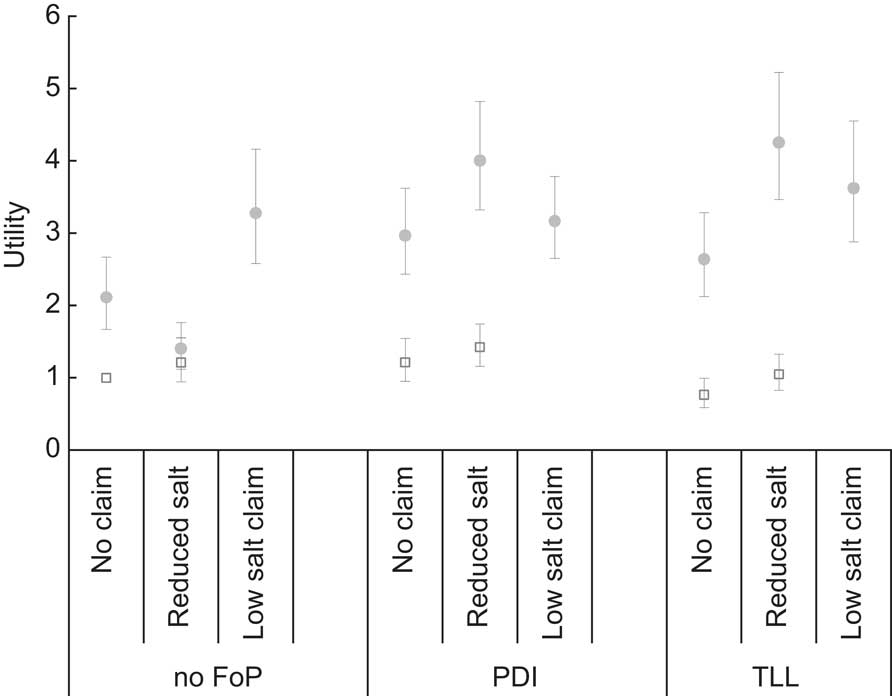
Fig. 3 Utility of different label formats (FoP, front-of-pack; PDI, Percentage Daily Intake; TL, Traffic Light) and nutrition claims (‘reduced salt’ and ‘low salt’) on choice behaviour for high-sodium (□) and low-sodium (●) products among New Zealanders aged 18–79 years (n 691) participating in an online nationwide research panel. Values are means, with 95 % confidence intervals represented by vertical bars
Table 5 Multinomial logit regression results for utility based on different label formats and presence of a nutrition claim for combined sample: New Zealanders aged 18–79 years participating in an online nationwide research panel
FoP, front-of-pack; PDI, Percentage Daily Intake; TL, Traffic Light.
Results are presented with two statistical significance levels: P = 0·05 by convention and P = 0·01 to account for multiple comparisons.
Significantly different from 1·00 at *P = 0·05, **P = 0·01.
In general, the addition of a nutrition claim was associated with an increased utility, especially in the presence of a front-of-pack label. For the low-sodium product, compared with the control no front-of-pack label, no claim product (utility = 2·11, 95 % CI 1·67, 2·67), significantly higher utilities were seen in the PDI label ‘reduced salt’ claim (utility = 4·00, 95 % CI 3·32, 4·82), the TL label ‘reduced salt’ claim (utility = 4·25, 95 % CI 3·47, 5·22) and the TL label ‘low salt’ claim (utility = 3·62, 95 % CI 2·88, 4·55) products. The exception to this general pattern was the no front-of-pack label ‘reduced salt’ claim product, which was not significantly different from the control no front-of-pack label, no claim product (utility = 1·40, 95 % CI 1·12, 1·76).
For the high-sodium product (which was ineligible for the ‘low salt’ claim), the combination of a ‘reduced salt’ claim and a PDI label on the front of the pack was associated with a significantly increased utility of 1·42 (95 % CI 1·16, 1·74) compared with the control reference category of no front-of-pack label, no claim product (utility = 1·00), whereas the TL label ‘reduced salt’ claim product was not significantly different (utility = 1·05, 95 % CI 0·83, 1·33). For the high-sodium product the TL label was slightly (but significantly P = 0·005) less attractive than the PDI label.
Discussion
To our knowledge, the present research is first published that tests how alternative sodium nutrition label formats and nutrition claims influence consumers’ choice behaviour. The results support the first hypothesis that consumers’ ability to discriminate between foods with high and low sodium content increased as front-of-pack labels became less numeric and more visual. In this experiment the TL images facilitated healthier choices more effectively than either the PDI plus NIP or NIP alone formats. While both front-of-pack labels significantly increased consumers’ ability to differentiate between high- and low-sodium products compared with the NIP alone, the TL label promoted greater discrimination and, in particular, enabled better identification of the high-sodium product.
The results also supported our second hypothesis; that consumers with hypertension would demonstrate stronger discrimination between high- and low-sodium foods when these featured nutrition labels that were less numeric and more visual. Figure 2 shows that those with hypertension were significantly more likely to choose low-sodium products than those without hypertension, and this effect was significantly higher with the addition of a front-of-pack label. There was also a greater difference between the utilities for high- and low-sodium products for people with hypertension and those without hypertension when a front-of-pack label was present. Interestingly, the PDI label increased the attractiveness (utility) of the high-sodium product for people with hypertension, whereas the TL label did not. The TL label significantly reduced the utility of the high-sodium product for people without hypertension. This result shows that the TL label more effectively enabled those with hypertension to avoid high-sodium processed foods. Although it is useful for consumers to easily recognize low-sodium products, calls for them to reduce sodium intake means they must be able to identify high-sodium products. It is particularly important that food labels designed to inform consumers about potentially harmful nutrients such as sodium do not in fact increase the attractiveness of products high in those nutrients, as the PDI label did in the present study.
Increasingly, researchers have concluded that simple visual labels such as the TL stimulate the greatest discrimination between products with differing nutrition profiles(Reference Cowburn and Stockley25, Reference Grunert and Wills26). Many people find nutritional information labels too time-consuming to read(Reference Signal, Lanumata and Robinson27) and may lack both the mathematical ability to understand the information and the nutritional knowledge to interpret the information provided(Reference Ni Mhurchu and Gorton21, Reference Rothman, Housam and Weiss28). The rapid decision making that typically occurs in supermarkets may also preclude review of more detailed label formats(Reference Hutchinson and Alba29), with one observational study in the UK showing consumers spent an average of 29 s per product bought and 31·8 % of consumers were noted not to have looked at the product in detail(Reference Grunert, Wills and Fernandez-Celemín30). This implies that many consumers find the time required to use nutrition information exceeds the time they have available to evaluate and compare food products(Reference Grunert and Wills26, Reference Signal, Lanumata and Robinson27). The rapidity of consumers’ decision making suggests they rely on habitual behaviours and heuristics, both of which simplify their choices, and raises the possibility that even knowledgeable consumers may not use nutrition labels if they feel under time pressure. Therefore simple labels that place fewer demands on consumers’ numeracy and background knowledge such as the TL are more likely to promote healthful food choices. Our findings support this conclusion. In fact, in practice these differences may be greater in a supermarket setting, as although New Zealand consumers are familiar with the NIP and PDI, the TL is not currently in use. Once familiar with the TL format, New Zealand consumers may use it to even greater effect.
Nutrition claims
New Zealand allows nutrition claims such as ‘reduced salt’ and ‘low salt’, which consumers may use to identify lower-sodium products. However, nutrition claims may generate positivity bias, where consumers assume products featuring a nutrition claim are more healthful than is the case(Reference Roe, Levy and Derby31). In the present experiment, both the PDI and TL labels enabled better identification of the low-sodium product in the presence of a ‘reduced salt’ claim. For the high-sodium product only the TL label was able to counteract the potentially misleading effect of the ‘reduced salt’ claim.
Experience in Finland suggests that nutrition claims have the potential to reduce population salt intake(Reference Pietinen, Valsta and Hirvonen13). However, from a public health perspective these claims are only useful if they are consistent with a product's nutrition profile. In this context current regulations permit a ‘reduced salt’ claim to be applied to a high-salt product if the food has at least 25 % less sodium than a comparative reference food. This may be misleading if consumers believe that ‘reduced salt claim’ implies low sodium content. Our findings relating to nutrient content claims have particular salience since these claims may exert a stronger influence on consumers than the NIP, even when the claims made are inconsistent with the NIP. Food labelling regulations regarding sodium content need to ensure that foods are carefully screened before nutrition claims are permitted, as even in the presence of a PDI label a nutrition claim may actually enhance consumers’ perceptions of a high-sodium product.
Limitations
There are several potential limitations to the present study. While the sample was not selected as nationally representative, the demographic profiles of participants broadly reflect the New Zealand population when compared with data from the most recent New Zealand Population Census of 2006 with respect to ethnicity and education(32). This leads us to believe that the results will be generalizable in the New Zealand context. The results are consistent with other international research(Reference Campos, Doxey and Hammond12, Reference Cowburn and Stockley25), and so are likely to have more general application. The online survey simulates behaviour in a supermarket, which is difficult to observe directly, and, while still removed from actual behaviour, it is closer to this than surveys eliciting self-reported estimates of behaviour. However, the results may have been affected by social desirability bias and so may not fully reflect actual purchasing behaviour, although the anonymity afforded by the online mode is likely to have reduced this potential error. In the experiment, only sodium content was varied; however, factors such as other nutrients or price may have a more powerful influence on actual purchasing behaviour and should be tested in future studies(Reference Andreyeva, Long and Brownell33). The role of more detailed label review at home in ongoing purchasing decisions should also be examined in future research.
Conclusions
Dietary sodium reduction is an important and cost-effective public health strategy(Reference Bibbins-Domingo, Chertow and Coxson7). With 75 to 80 % of dietary sodium intake coming from sodium contained in processed foods, reformulation is an important population wide strategy for dietary salt reduction. However, effective food labelling has the potential to enable consumers to moderate their own salt intake. The present results support the widespread use of front-of-pack labelling of sodium content and suggest a TL label, rather than a PDI label, would assist all consumers to discriminate between high- and low-sodium products more effectively. The TL label was particularly effective in enabling consumers to identify the high-sodium product, even in the presence of a nutrition claim. To avoid consumer deception, policy makers must ensure that nutrition claims are accurate, do not create misleading impressions about products’ nutrition profiles, and are used together with an easily understood front-of-pack label such as a TL.
Acknowledgements
This study was funded by the Health Research Council of New Zealand through the University of Otago. There are no known conflicts of interests relating to this work. R.M. led the writing and contributed to the statistical analysis and design of the study. J.H. designed and supervised the study and contributed to the writing. D.H. led the statistical analysis and contributed to the writing. The authors are grateful to the Health Research Council of New Zealand for funding this study, and to Professor Jim Mann who provided helpful comments throughout.










