Childhood obesity is a significant public health problem(Reference Ebbeling, Pawlak and Ludwig1). Overweight and obese children are at increased risk of experiencing co-morbidities, such as CVD, type II diabetes and hypertension(Reference Rocchini2–Reference Biddle, Gorely and Stensel4). Being overweight or obese in childhood consistently increases the risk of being overweight or obese in adolescence and adulthood(Reference Fuentes, Notkola and Shemeikka5–Reference Singh, Mulder and Twisk7), thereby leading to further co-morbidities(Reference Whitaker, Wright and Pepe8). A recent US study also suggested that, given the marked increase in the proportion of obese people, obesity has become an equal, if not greater, contributor to the burden of disease than smoking(Reference Jia and Lubetkin9).
Poor nutritional habits and physical inactivity are two health behaviours that are believed to be linked with increasing rates of overweight and obesity in children, but these two behaviours are themselves manifestations of changing social and economic conditions(Reference Yach, Stuckler and Brownell10). Environmental factors that contribute to obesity include communities designed to encourage driving rather than walking or cycling, unequal access to recreation facilities and green spaces, sedentary technologies that occupy our leisure time and ‘fast food’ restaurants that provide energy-dense, nutrient-poor food that is highly accessible, inexpensive and available in increasing portions(Reference Giskes, Kamphuis and van Lenthe11–Reference Taveras, Berkey and Rifas-Shiman15). Together, these factors have created an ‘obesogenic environment’, described as ‘the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations’(Reference Swinburn, Egger and Raza16). As physical inactivity and poor nutrition are both determinants of obesity, health promotion initiatives aimed at modifying either or both of these health behaviours are increasingly being implemented, particularly those aimed at childhood obesity prevention(Reference Story, Nanney and Schwartz17). Further, evidence is accumulating for the importance of providing supportive environments for where children live, learn and play(Reference Story, Nanney and Schwartz17, Reference Chang, Gertel-Rosenberg and Drayton18). However, often such interventions are poorly implemented and evaluated(Reference Swinburn and de Silva-Sanigorski19) and lack an understanding of the health impact and costs associated with obesity prevention strategies.
While previous research has now clearly established that obese children have higher health-care costs than normal-weight children(Reference Trasande and Chatterjee20, Reference Kuhle, Kirk and Ohinmaa21), limited data are available on how mediating health behaviours like improved nutrition and physical activity may influence health-care costs and utilization and whether investments in health promotion strategies that address them are likely to be cost-effective(Reference John, Wenig and Wolfenstetter22). Data are also limited on the utility of measures of these exposures in assessing health-care costs. The objective of the present study was therefore to explore the use of two measures of diet quality, as well as measures of physical activity and screen time, in assessing health-care costs and to determine whether children who reported healthier behaviours, as determined by these measures, also had lower health-care utilization.
Methods
Study design
The study design is a population-based cross-sectional study, linking data from the 2003 Children's Lifestyle and School Performance Study (CLASS)(Reference Veugelers and Fitzgerald23) with Nova Scotia administrative health data. CLASS comprised a population-based survey of grade 5 students and their parents, conducted in the Canadian province of Nova Scotia in 2003(Reference Veugelers and Fitzgerald23). The study consisted of a questionnaire that was completed at home by the parents; a Canadian version of the Harvard Youth/Adolescent Food Frequency Questionnaire (YAQ)(Reference Rockett, Wolf and Colditz24), administered to the students in the schools by study assistants; and a measurement of the students’ height and weight. The YAQ is a self-administered tool designed for children and adolescents aged 9–18 years which gathers information on both dietary intake and habits pertaining to mealtime behaviours, and has been shown to be a valid measure of nutritional intake among this age group(Reference Rockett, Wolf and Colditz24). The survey also included validated questions on the frequency of physical activities and the number of hours of sedentary activities (watching television, working on a computer, playing video games) taken from the National Longitudinal Survey of Children and Youth (NLSCY)(25). The home questionnaire collected information on sociodemographic factors, the child's place of birth and residency, as well as household income level, parental educational attainment, breast-feeding practices, self-rated parental physical activity and diet quality. In addition to the above information, participating parents were asked to provide the Nova Scotia health insurance number for their child, along with informed consent to allow future linkage with administrative health databases. Of the 291 public schools in Nova Scotia (>97 % of students in Nova Scotia attend public schools) with grade 5 classes, 282 (96·9 %) participated in the study. The average rate of return of questionnaires and consent forms was 51·1 % per school.
In Canada, a publicly funded health-care system is in place(26). This provides Canadians with universal access to all medically necessary hospital and physician services. Canada's universal single-provider health-care system therefore poses no financial barriers to seeking health services and tracks use and costs of hospital and physician services in each province. The Medical Services Insurance database was the administrative health database used for the present analysis. This contains individual patient-level information including patient demography (age, gender, location, etc.), attending physicians, diagnoses and procedures performed, service transfers while in hospital, specialty services received (e.g. physiotherapy, occupational therapy) and case complexity (e.g. resource intensity weight). The health system of Nova Scotia is predominantly fee-for-service, which means that physicians bill the province for each patient visit. If an alternative payment plan is in effect, physicians engage in ‘shadow-billing’, where they provide a code for the patient visit as if they were to be reimbursed. We used data from this physician billing data set in the current analysis. Given the structure of the data set and the availability of diagnostic codes, we are able to rule out visits for wellness and/or immunizations. Aggregate costs of health-care episodes for physician visits were obtained from the Ontario Case Costing Initiative(27). Costs were adjusted to 2006 Canadian dollars using the Canadian Consumer Price Index(28). The administrative health data sets were linked with the CLASS data through the health card numbers provided by the students’ parents. Where no direct match was found, the birth date and civic address were used to establish a probable match. Of the 5200 students who participated in CLASS by completing the surveys, 4380 (84·2 %) could be linked with information in the administrative data sets. In the remaining children, parents had provided an invalid or no health insurance number. When comparing the original CLASS sample with the linked sample, there were no statistically significant differences in sociodemographic factors or weight status between the two groups. More detailed information on CLASS, the administrative data sets and the data linkage can be found elsewhere(Reference Kuhle, Kirk and Ohinmaa21).
Outcomes
The primary outcome was health-care utilization, defined as both (i) the total physician costs (in Canadian dollars) and (ii) the number of physician visits, from 2001 to 2006. The 2001–2006 time frame was chosen to reflect health-care utilization patterns around the CLASS data collection period.
Exposures
The main exposures were: (i) the Diet Quality Index (DQI; continuous, on a scale from 0 to 1, with 1 indicating highest diet quality)(Reference Kim, Haines and Siega-Riz29); (ii) the Healthy Eating Index (HEI; continuous, on a scale from 0 to 1, with 1 indicating highest diet quality)(Reference Kennedy, Ohls and Carlson30); (iii) physical activity (parental report; four levels: ≤2 × /week, >2 to 4 × /week, >4 to 7 × /week, >7 × /week); and (iv) screen time (time spent watching television or playing computer/video games as per parental report; three levels: ≤2 h/d, >2 to 4 h/d, >4 h/d). DQI values encompass dietary variety (i.e. overall variety and variety within protein sources, to assess whether intake comes from diverse sources both across and within food groups), adequacy (i.e. the intake of dietary elements that must be supplied sufficiently to guarantee a healthy diet), moderation (i.e. intake of food and nutrients that are related to chronic diseases and that may need restriction) and balance (i.e. the overall balance of the diet in terms of proportionality in energy sources and fatty acid composition). The HEI is based on a ten-component system of five food groups, four nutrients and a measure of variety in food intake(Reference Kennedy, Ohls and Carlson30). Both the DQI and HEI were calculated on the basis of students’ responses to the YAQ and Canadian Food Tables. Although these indices were correlated (Pearson's r = 0·87), we included both measures because they are commonly used within the nutrition field. The polychoric correlation coefficient for the measures of physical activity and screen time was 0·32, i.e. unrelated, therefore both measures were included. Other covariates considered in the regression models were: (i) gender; (ii) household income (four levels: $CAN 0 to 20 000, $CAN 20 001 to 40 000, $CAN 40 001 to 60 000, >$CAN 60 000; 23 % missing values); (iii) parental education attainment (three levels: secondary school or lower, college, university; 7 % missing values); and (iv) geographic region (urban, rural; based on the second character of the forward Sortation Area in the postal code; rural post codes contain a 0 as the second character)(31).
Statistical analysis
Mean physician costs and number of physician visits were calculated by health behaviours (diet quality and physical activity) and sociodemographic factors. The association between health behaviours and health-care utilization was investigated using a series of multivariable regression models. Regression models were adjusted for gender, household income, parental education and geographic region (urban v. rural). Missing values for income (23 %) and education (7 %) were considered as separate covariate categories in the regression models but results are not presented. The health-care cost data were skewed to the right and therefore were log-transformed to yield a normal distribution; for students with $CAN 0 physician costs (n 51), cost values were replaced with half of the observed minimum non-zero health care costs (0·5 × $CAN 27) before log transformation. Linear regression was used to examine associations between lifestyle factors and log-transformed costs. After ascertaining homoscedascity, regression coefficients and their confidence intervals were back-transformed by taking the anti-log. The exponentiated coefficients represent cost ratios relative to the reference group. The distribution of the number of physician visits showed overdispersion, therefore these outcomes were modelled using negative binomial regression. As participation rates for CLASS in residential areas with lower estimates of household income were slightly lower than the average, response weights were calculated to overcome potential non-response bias(Reference Veugelers and Fitzgerald23) and to yield provincial population estimates for children born in 1992 in Nova Scotia. The Stata/SE statistical software package version 11 (Stata Corp, College Station, TX, USA) was used to perform the statistical analyses.
The study, including data collection, parental informed consent forms and data linkage, was approved by the Health Sciences Human Research Ethics Board of Dalhousie University, the IWK Health Centre Research Ethics Board, the Reproductive Care Program Joint Data Access Committee and the Dalhousie University Population Health Research Unit Data Access Committee.
Results
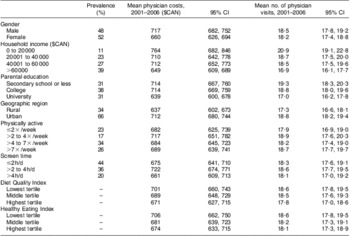
Table 1 shows the health-care utilization in the sample by sociodemographic factors and health behaviours. Students in households with a higher socio-economic status (i.e. higher household income and parental education) or higher diet quality had lower total physician costs and fewer physician visits during the study period. However, no such trends were observed for physical activity or screen time. Students residing in urban areas also had higher health-care costs and more physician visits.
Table 1 Health-care utilization in grade 5 students from the Canadian province of Nova Scotia by sociodemographic and lifestyle factors
Multivariable regression analysis showed a trend towards fewer physician visits and lower physician costs in children with healthier diets, as defined by the DQI and HEI (Table 2). However, only one result was statistically significant, with children in the highest tertile of diet quality having fewer physician visits in the unadjusted model only. There was no statistically significant relationship for physical activity and screen time measures, although there was a non-significant trend towards increasing health-care costs associated with increasing physical activity and decreasing screen time. Odds ratios displayed little variation between univariate and fully adjusted models.
Table 2 Exponentiated linear regression coefficients (physician cost) and incidence rate ratios (number of physician visits) for the association of health behaviours with health-care utilization in grade 5 students from the Canadian province of Nova Scotia
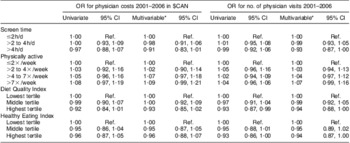
Exponentiated coefficients of the natural logarithm of physician costs represent the relative cost v. the reference group (Ref.).
*Adjusted for gender, household income, parental education and geographic region.
Discussion
Our findings have revealed a trend towards lower health-care utilization associated with the highest tertile of diet quality in this population sample of children; however, this was not statistically significant. The ranges of costs associated with diet and physical activity measures were also narrow, making it difficult to show an association with the measures of diet and physical activity used. This likely reflects the lower exposure of children in this age group to the health-care system. It is also possible that the 6-year time frame for assessing health-care utilization was not sufficient time for the full health consequences of physical inactivity or healthy eating to become fully apparent in the children. The lack of statistical association should therefore be interpreted with these limitations in mind, while also considering the population health implications, given the trend towards lower health-care utilization, at least for diet quality. Such a trend may therefore be of public health (clinical) significance, even while failing to reach statistical significance.
The present analysis used two measures of diet quality, the DQI and the HEI, with both showing a similar pattern; this is an important finding, given the interest in the use of composite measures of diet for assessing health outcomes(Reference Kant32). Diet quality has been shown in previous research to be associated with improved health outcomes in adults, although the measures used to define diet quality were not comparable to those in the current study(Reference Kant32). However, there is a paucity of data on diet quality and health in children(Reference Smithers, Golley and Brazionis33), making the present paper one of the first to our knowledge that has explored this link in school-aged children. Although nutritional intake was based on self-reported food frequency, the Harvard YAQ measures habitual food intake and has been validated in this population. Further, the use of a composite measure of diet quality, along with the HEI, makes this a more reliable measure of dietary patterns over time. FFQ data were chosen for the present study to reduce participant burden, given that CLASS was a population-based survey that was administered to more than half of all grade 5 children in the province of Nova Scotia in 2003 (n 5200).
The relationship between physical activity, sedentary behaviours and health-care utilization suggests higher health-care utilization with higher reported physical activity or lower reported screen time. One possible explanation for this is that children with higher levels of physical activity may be more likely to become injured. Spinks et al. quantified the likelihood of injury occurring during physical activity in Australian children aged 4 to 12 years by measuring exposure to activity and injury occurrence over 12 months(Reference Spinks, McClure and Bain34). They found that a high number of injuries sustained by the cohort (88 %) were directly related to physical activity. It was not possible to tell if the children from our study experienced injuries associated with physical activity as such data were not collected, but nor could this be excluded as a reason for the increased health-care costs associated with physical activity.
A significant strength of our study is the availability of individual-level health-care costs, applied to a population-based study. The use of population-based data provides a more complete and less biased picture of health behaviours associated with health-care use, as Canada's publicly funded health-care system reduces financial barriers to seeking health services. Limitations include the relatively short duration for assessing health-care utilization (6 years), the fact that physician data are collected for billing purposes only and may not have been recorded accurately(Reference Peabody, Luck and Jain35), and the use of self-reported measures of physical activity, screen time and dietary behaviours, measured at one period of time (2003). However, for the dietary measures at least, the assessment tools measure habitual intake, thereby providing a more valid measure of nutritional intake. Given that this is a large, population-based sample, we are confident that the use of FFQ data is justified in the study. Further research using more robust measures of dietary exposure would help explain these findings and allow specific components of the diet to be explored in relation to health-care utilization. The measures of physical activity and screen time used in the survey were not captured in such depth, only assessing frequency of activity, not intensity. Therefore, better measures in future studies would improve the accuracy of the analysis for these behaviours.
Despite these limitations, considered in the context of the existing evidence base, our findings are of importance to public health, particularly given the trend towards lower health-care costs for children with the healthiest diets. Future research should therefore extend the time frame for measuring health-care utilization to take account of the likelihood that the main associated diseases may not yet have emerged in this sample of children. Our previous analysis on health-care costs in the same sample of children found that obese children used health care more often and incurred higher health-care costs than normal-weight children(Reference Kuhle, Kirk and Ohinmaa21). Since physical inactivity and poor diets are believed to be linked with the temporal increase in overweight prevalence among children(Reference Willms, Tremblay and Katzmarzyk36–Reference Tremblay and Willms38), strategies that facilitate healthy eating and active living behaviours should remain a critical focus of population health and health promotion. Veugelers and Fitzgerald have previously reported that students attending schools with a comprehensive school health promotion approach were more physically active, had better diets and were less likely to be overweight and obese(Reference Veugelers and Fitzgerald39). Further, the impact of healthy eating behaviours has been linked to specific educational outcomes; for example, a recent publication has demonstrated an independent association between overall diet quality and academic performance(Reference Florence, Asbridge and Veugelers40). Evidence is also emerging that multifaceted school-based interventions targeting nutrition and physical activity behaviours may be cost-effective(Reference Carter, Moodie and Markwick41). Diet and physical activity should therefore remain important targets for health promotion efforts to reduce health-care costs in the future.
Conclusions
Our findings suggest that healthy eating habits established in childhood may be associated with lower health-care utilization, as defined by total physician visits and physician costs, in this population-based sample of children. However, this trend was not statistically significant and requires further research over a longer time period. Both measures of diet quality – the DQI and the HEI – produced similar results, suggesting that composite measures of diet quality may have utility for analyses of this type.
Acknowledgements
Support for administrative data linkage was provided by a Canada Foundation for Innovation Leaders Opportunity Fund award to S.F.L.K. The CLASS project was funded through a Canadian Population Health Initiative operating grant. S.F.L.K. was supported through a Canadian Institutes of Health Research (CIHR) Canada Research Chair in Health Services Research. P.J.V. was supported through a Canada Research Chair in Population Health and an Alberta Innovates Health Solutions Health Scholarship. The interpretations and options expressed in this manuscript are those of the authors. The authors declare that there is no conflict of interest. Data analysis was conducted by S.K. All authors contributed to the drafting of the manuscript. The authors would like to thank all grade 5 students, their parents, schools, school boards and the Department of Education for contributing to this research. They also thank Charmaine Cooke and Yan Wang from the Population Health Research Unit, Dalhousie University, for their assistance with data provision and access.




