Reducing the number of people who suffer from hunger by 2015 was one of the UN Millennium Development Goals published in 2000( 1 ). Despite many global efforts to reduce the number of food-insecure households, the rise in food prices following the latest global economic crisis (2008–09) has prompted increased concern about this problem in different nations( Reference Pérez-Escamilla 2 ). The alarming estimates published by a variety of institutions in recent years seem to justify this concern. According to the FAO, although the prevalence of estimated household food insecurity (HFI) may have decreased by 17 % between 1990–92 and 2011–13, the state of affairs is still unacceptable because there are still approximately 842 million individuals living with food insecurity( 3 ).
In different parts of the world, several programmes have been devised to reduce the number of food-insecure and hungry people. Although these proposals have yielded some positive results, creating interventions based solely on the supply of financial resources to a vulnerable population group does not seem to have the power to completely eliminate the problem( Reference Melchior, Caspi and Howard 4 ). This has led some researchers to begin investigating whether other determinants beyond income could be involved that could therefore be the target of measures to tackle food insecurity( Reference Melchior, Caspi and Howard 4 – Reference Tarasuk, Mitchell and McLaren 7 ).
Some authors suggest that psychosocial factors and aspects of a couple’s relationship could influence HFI( Reference Melchior, Caspi and Howard 4 , Reference Hernandez, Marshall and Mineo 5 , Reference Chilton and Booth 8 – Reference Chilton, Rabinowich and Woolf 10 ), but the number of studies investigating these factors is still limited. Only five studies have examined the impact of intimate partner violence (IPV) on HFI. Two used primarily qualitative methods( Reference Chilton and Booth 8 , Reference Chilton, Rabinowich and Woolf 10 ), whereas the other three were population-based epidemiological studies( Reference Melchior, Caspi and Howard 4 , Reference Hernandez, Marshall and Mineo 5 , Reference Ribeiro-Silva, Fiaccone and Barreto 11 ).
One finding emerging from the qualitative studies concerns women’s perceptions that the control exerted by their partners on the financial resources needed to buy food could be used as a form of coercion( Reference Chilton and Booth 8 ). The other qualitative study showed that the stress caused by IPV contributed to a decrease in food intake, not only in the woman herself but in other family members as well. Many women have also stated that exposure to violence affects their mental health to the extent that they have given up their studies and jobs, putting a strain on the household budget and therefore the possibility of having a varied and sufficient diet( Reference Chilton, Rabinowich and Woolf 10 ). These effects of IPV on women’s mental health have been repeatedly highlighted by several authors( Reference Trevillion, Oram and Feder 12 – Reference Reichenheim, Moraes and Lopes 14 ) and by the WHO in its recent publication on the health effects of IPV( 15 ).
The three quantitative studies have suggested that under some circumstances, IPV could contribute to HFI( Reference Melchior, Caspi and Howard 4 , Reference Hernandez, Marshall and Mineo 5 , Reference Ribeiro-Silva, Fiaccone and Barreto 11 ). One was a population-based epidemiological study conducted in the UK between 1999 and 2006( Reference Melchior, Caspi and Howard 4 ). That follow-up study involving 1116 families showed that domestic violence remained a risk factor for HFI after controlling for several confounders. A study conducted by Hernandez et al.( Reference Hernandez, Marshall and Mineo 5 ) on a sample of 1690 socially disadvantaged mothers of young children in twenty US cities reached the same conclusions. The authors also raised the possibility that the relationship between IPV and HFI could be mediated by maternal depression, which is consistent with what is proposed by the WHO( 15 ). However, the interpretation of their findings is somewhat limited because there was no analytical approach suitable to analyse the role of mediating variables. A more recent study conducted in Brazil also suggested an association between physical IPV and HFI( Reference Ribeiro-Silva, Fiaccone and Barreto 11 ). In that study, couples reporting minor and severe physical IPV were more likely to experience HFI compared with those not reporting these types of IPV. Moreover, although touching on novel issues, none of the quantitative studies yielded new findings regarding the importance of the independent and separate roles of psychological and physical IPV in HFI.
The high prevalence of domestic violence worldwide and the severity of its impact on women’s mental health( Reference Trevillion, Oram and Feder 12 – Reference Reichenheim, Moraes and Lopes 14 ) justifies testing whether these two phenomena jointly contribute to the explanatory models of HFI. The relevance of HFI per se, combined with the apparent inability of theoretical models confined to addressing socio-economic issues to fully consider the complexities involved, indicate that more studies are needed. Investigating to what extent and means different forms of IPV are related to the occurrence of HFI could facilitate the development of new proposals to prevent or mitigate this problem. The present study thus investigated how psychological and physical IPV, mental disorders and HFI are interrelated in the light of common antecedents and potential confounders.
Methods
Study design and participants
The current population-based cross-sectional study was conducted in Duque de Caxias, a municipality in Greater Rio de Janeiro, Brazil. Data collection occurred from April to December 2010. Participants were selected by multiple-stage cluster sampling (census blocks, permanent private households and individuals) using inverse sampling as the field strategy( Reference Haldane 16 , Reference Hirai and Anjos 17 ). The study population comprised 849 female adolescents and adult women involved in an intimate relationship within the 12 months prior to the interview. Due to missing data, the number of individuals effectively participating in the analysis before imputation varied from 793 to 849 depending on the variable (see below). Information was obtained through face-to-face interviews with the female person in charge of buying and preparing meals. All interviews were held in a designated area without the presence of the partner. The participants were assured of their full anonymity and confidentiality. The study was approved by the Federal University of Rio de Janeiro research ethics committee (protocol number 73/2009) in accordance with the principles set forth in the Declaration of Helsinki.
Theoretical model, variables and questionnaires
Figure 1 presents the directed acyclic graph of the ‘propositional’ model initially tested. Given the limited number of studies focusing specifically on the relationship between IPV and HFI, this model was developed based on knowledge about the impact of IPV on the mental health of women and the macro-structural factors related both to domestic violence and HFI. The model encompassed seven domains: socio-economic status, demographic characteristics and social support of the women, alcohol misuse by the partner, psychological and physical IPV, common mental disorders (CMD) in women and HFI. The path diagram moves from the left to the right, respecting the postulated hierarchical sequence of events. The related variables are described below, including definitions and the respective instruments used when applicable.

Fig. 1 Propositional model: directed acyclic graph of the relationships between intimate partner violence, common mental disorders and food insecurity (‘Hh food insecurity’, household food insecurity; ‘Common mental disorders’, common mental disorders in the woman; ‘Psychological IPV’, psychological intimate partner violence; ‘Physical IPV’, physical intimate partner violence; ‘Alcohol misuse (partner)’, alcohol misuse by the partner; ‘Social support (women)’, woman’s social support; ‘C & A under 18’, presence of children and adolescents under 18 years old in the household; ‘Race/ethnicity (women)’, woman’s self-reported skin colour; ‘Economic classification’, Brazilian Economic Classification Criterion; ‘Age (women)’, woman’s age)
Women’s socio-economic status was represented by two variables: an economic classification variable measured by the Brazilian Economic Classification Criterion and self-reported race/ethnicity. The Brazilian Economic Classification Criterion is a composite index consisting of several household assets, information on whether there is a domestic employee at home and the educational status of the main income earner( 18 ). As recommended, the index was categorized into five strata, ranging from the richest (A; high income) to the most disadvantaged group (E; very low income). Women’s self-reported race/ethnicity was analysed as a dichotomized variable: white v. non-white. This categorization aimed to represent the sociodemographic and cultural differences present in Brazilian society. Many studies have shown that compared with whites (mostly Caucasians from European background), non-whites (African descendants, Mestizos, Asians and South American native populations) have lower incomes, live in households with poorer sanitation and have a lower level of schooling( 19 ).
The demographic variables comprised women’s age, marital status and whether there were any children or adolescents under the age of 18 years old in the household. Age was analysed as a continuous variable and marital status as a binary variable (either married/cohabiting or single/divorced/widowed). The presence of children and adolescents under 18 years old was also dichotomized (yes or no).
Social support perceived by the women was assessed through the Portuguese version of the material support subscale developed for the Medical Outcomes Study( Reference Chor, Griep and Lopes 20 , Reference Sherbourne and Stewart 21 ). This subscale covers the respondents’ perceptions of four types of third-party help received in daily activities and in case of illness. The score ranges from 4 to 20 and is calculated as the sum of the responses to each of the component items (1=never, 2=rarely, 3=sometimes, 4=almost always, 5=always).
Alcohol misuse by the woman’s partner was measured through the Portuguese version of the CAGE questionnaire (Cut-down; Annoyed; Guilty; Eye-opener)( Reference Masur and Monteiro 22 , Reference Mayfield, McLeod and Hall 23 ) administered to the women by proxy. The CAGE consists of four yes/no questions covering the social repercussions of alcohol misuse. In line with the literature, positive answers to two or more items indicated potential alcohol misuse in the descriptive analysis; whereas the raw score (0–3) was employed in the path analyses.
The Portuguese version of the Revised Conflict Tactics Scale (CTS2)( Reference Moraes and Reichenheim 24 – Reference Reichenheim, Klein and Moraes 27 ) was used to assess IPV. Only two of the five available subscales were of interest in the present study: psychological and physical violence. The subscale on psychological IPV comprises eight dichotomous items (whether the event has ever happened or not) relating to women as perpetrators and/or victims. Raw scores thus range from 0 to 16. Likewise, the physical IPV subscale consists of twelve items, with a respective score varying from 0 to 24. For analysis purposes, the few individuals with scores of 10 or above were grouped into a single category. IPV was dichotomized for descriptive purposes; a positive response to at least one of the items in the respective subscale defined a positive case. Raw scores per subscale were used in the main path analyses. The recall period covered the 12 months prior to the interview.
The evaluation of CMD used the Portuguese version of the twelve-item General Health Questionnaire (GHQ-12)( Reference Mari and Williams 28 ). The items on this questionnaire measure how often symptoms occurred in the preceding two weeks. As the items contain four response options, the total score varies from 12 to 48. Women scoring 3 or above were defined as possible cases of CMD for descriptive purposes( Reference Goldberg and Williams 29 ).
HFI was measured using the Brazilian Food Insecurity Scale( Reference Segall-Corrêa, Escamilla and Sampaio 30 ). This version has been cross-culturally adapted from the US Household Food Security Survey Module (HFSSM)( Reference Bickel, Nord and Price 31 ), which is regarded as the best epidemiological instrument currently available( Reference Marques, Reichenheim and de Moraes 32 ). This version of the Brazilian scale encompassed fifteen dichotomous items on food insecurity experienced in the previous 3 months, upon which households were classified into four groups: food and nutritionally secure (adult-only and child and adolescent (C&A) scales, score=0), mildly food insecure (adult-only scale, score=1–5; C&A scale, score=1–3), moderately food insecure (adult-only scale, score=6–10, C&A scale, score=4–6) and severely food insecure (adult-only scale, score=11–15, C&A scale, score=7–8)( Reference Segall-Corrêa, Escamilla and Sampaio 30 , Reference Facchini, Nunes and Motta 33 ). In the present study the latter two categories were grouped together. The main outcome was thus modelled as a three-level variable.
Statistical analysis
As conveyed before, a multiple imputation procedure was first employed to address the missing data. Assuming a MAR (missing at random) pattern, twenty imputed databases were generated using Mplus 7.13( Reference Muthén and Muthén 34 ). These databases were subsequently exported to the statistical software package Stata 13 (‘mi passive’ command) for data managing and processing.
The modelling process used path analyses. As the distributions of the outcome variables differed according to the equations in the system, so too did the respective models. Returning to the variables in Fig. 1, the following models were used: ‘Hh food insecurity’, ordinal logit model; ‘Common mental disorders’, linear model; ‘Psychological IPV’, ordinal logit model; ‘Physical IPV’, ordinal logit model; ‘Social support (women)’, linear model; ‘Alcohol misuse (partner)’, ordinal logit model; ‘C & A under 18’ and ‘Marital status’, logit model. Regarding the ordinal logit models, proportional odds assumptions were tested ahead of the main modelling process using the ‘omodel’ Stata command. Three variables from the directed acyclic graph were completely exogenous (‘Race/ethnicity (women)’, ‘Age (women)’ and ‘Economic classification’) and therefore did not require a distributional specification.
The analyses employed the Mplus robust maximum likelihood estimator( Reference Muthén and Muthén 34 ). The fit of the model was evaluated using the Bayesian information criterion (BIC). The model with the lowest BIC value was considered the best fitting model( Reference Schwarz 35 ).
The modelling process consisted of two steps. Starting with the ‘propositional’ model presented in Fig. 1, misspecifications that suggested paths to add or remove were assessed in the first stage. Modification indices provided by Mplus were scrutinized to this end. Re-specification occurred if the BIC value dropped after freely estimating the model with the suggested new path or with a removal. The decision to explore and retain/remove a path was also based on theoretical plausibility( Reference Brown 36 ).
The second stage involved systematically trimming non-significant paths, i.e. those involving coefficients with an estimated P value of >0·05. However, paths with P values between 0·05 and <0·1 were preserved when they led to a significant reduction in the BIC value. This process respected the specific hierarchy of the initial ‘propositional’ model. The trimming process started on the left and moved to the right: (i) starting with all of the paths originating from the more distal variables (‘Race/ethnicity (women)’, ‘Age (women)’ and ‘Economic classification’); (ii) moving to the first-level intermediate variables (‘Marital status’, ‘C & A under 18’, ‘Social support (women)’ and ‘Alcohol misuse (partner)’); (iii) progressing to the second-level intermediate variables (‘Psychological IPV’ and ‘Physical IPV’); (iv) and finally from the most proximal variable (‘Common mental disorders’). The overall process was stopped when no additional path was suggested, all remaining paths were statistically significant and the fit of the model was acceptable. This stage of the analysis was also conducted using Mplus version 7.13( Reference Muthén and Muthén 34 ).
Results
Profile of the participants in the study
As shown in Table 1, 39·4 % of the families were food insecure at the time of the interview and of those, over a quarter were classified as having moderate or severe food insecurity. Nearly three-quarters of the women reported having been involved in at least one episode of psychological violence and approximately a quarter reported at least one episode of intimate partner physical aggression in the 12 months prior to the interview. Of those reporting psychological violence, 41·1 % also stated experiencing physical violence in their relationships, 93·9 % who alleged physical violence said that they had also suffered psychological violence. Approximately 80 % of the women reported three or more symptoms of mental distress, 71·1 % belonged to the lower middle-income class (class C), just over a third of the women described themselves as white, and nine out of ten said they were in a stable relationship at the time of the interview. Most women were of childbearing age. Approximately two-thirds of the households had at least one child or adolescent, and 10·3 % of the partners were identified as potential misusers of alcohol.
Table 1 Profile of the study population: women (n 849) who had been in a relationship in the 12 months preceding the interview, Campos Elíseos, Duque de Caxias, Rio de Janeiro State, Brazil, 2010

* Brazilian Economic Classification Criterion( 18 ).
Main findings
The ‘propositional’ model was first analysed with the covariance between the distal variables specified (‘Race/ethnicity (women)’, ‘Age (women)’ and ‘Economic classification’) and without the path from ‘Psychological IPV’ to ‘Physical IPV’. As all three covariances were largely non-significant at the conventional level (P<0·05), the model was tested without the covariances involving exogenous variables. This reduced the BIC value by 32·2 % (from 28 370·241 to 19 244·720). Based on the indications from the modification indices, a path between the two types of violence was introduced, which again improved the fit of the model (BIC=19 035·174). In the second stage of the modelling process, several of the paths originally proposed were deleted because they proved statistically non-significant at the specified levels or failed to reduce the BIC value. According to the scheme described in the Methods section, the analysis took nine sequential steps to reach a simplified ‘final’ model.
Figure 2 shows the directed acyclic graph of this ‘final’ model. The estimates of each path are shown in Table 2. Interestingly, HFI was associated with both psychological and physical violence. There was a direct path between psychological violence and HFI, indicating that part of this relationship may be mediated by factors not included in the model. In addition to this direct link, mediation through physical violence and CMD was also apparent. The association between physical violence and HFI seemed to occur exclusively through CMD. Notably, this relationship had to be smaller than the overall psychological IPV because the latter contained additional positive paths to the outcome. All estimates were adjusted for the other variables in the system and potential confounders in the process.
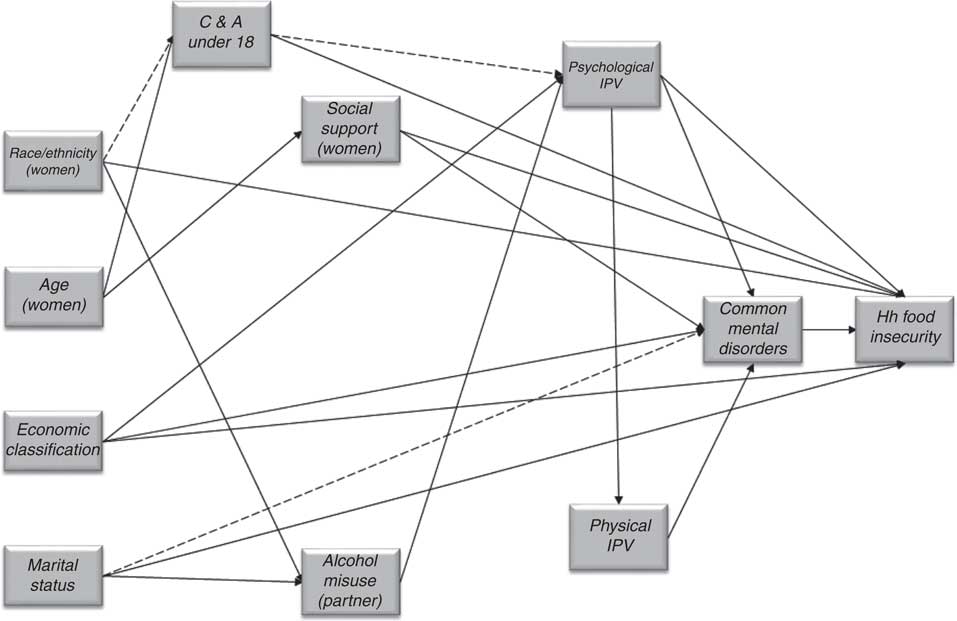
Fig. 2 ‘Final’ model: directed acyclic graph of the relationships between intimate partner violence, common mental disorders and food insecurity (‘Hh food insecurity’, household food insecurity; ‘Common mental disorders’, common mental disorders in the woman; ‘Psychological IPV’, psychological intimate partner violence; ‘Physical IPV’, physical intimate partner violence; ‘Alcohol misuse (partner)’, alcohol misuse by the partner; ‘Social support (women)’, woman’s social support; ‘C & A under 18’, presence of children and adolescents under 18 years old in the household; ‘Race/ethnicity (women)’, woman’s self-reported skin colour; ‘Economic classification’, Brazilian Economic Classification Criterion; ‘Age (women)’, woman’s age)
Table 2 ‘Final model’: point estimates, 95 % CI, statistical significance levels and fit indexFootnote *

‘Common mental disorders’, common mental disorders in the woman; ‘Psychological IPV’, psychological intimate partner violence; ‘Social support (women)’, woman’s social support; ‘C & A under 18’, presence of children and adolescents under 18 years old in the household; ‘Economic classification’, Brazilian Economic Classification Criterion; ‘Physical IPV’, physical intimate partner violence; ‘Alcohol misuse (partner)’, alcohol misuse by the partner; ‘Race/ethnicity (women)’, woman’s self-reported skin colour; ‘Age (women)’, woman’s age; ‘Hh food insecurity’, household food insecurity; BIC, Bayesian information criterion.
* Interpretations of paths’ estimates according to outcome (incoming arrow): proportional odds ratio → ‘Hh food insecurity’, ‘Psychological IPV’, ‘Physical IPV’ and ‘Alcohol misuse (partner)’; odds ratio → ‘C & A under 18’; linear regression coefficient → ‘Common mental disorders’ and ‘Social support (women)’.
As conveyed in Fig. 2 and Table 2, in addition to the two types of violence and CMD, there were also direct or indirect connections between the other antecedents and HFI. Considering only the direct path, food insecurity was approximately 6·6 times more likely to take place in families in the lowest socio-economic groups (classes D and E according to the economic classification) than in middle-income families (class B). Race/ethnicity also showed a strong association with HFI. Again, considering only the direct path, women who self-identified as non-whites were about twice as likely to be food insecure than those characterizing themselves as white.
Demographic variables were also important risk factors for HFI. Having a child or adolescent in the household and not being married or cohabiting at the time of the interview increased the chance of HFI threefold and twofold, respectively. Conversely, the lower the level of social support, the higher was the HFI. It should be noted that these estimates refer only to the direct links between these variables and the outcome. It follows that the total relationship must be far greater, as the result of adding all of the mediated paths.
Two variables that showed rather different behaviour were women’s age and alcohol misuse by the partner. The ‘final’ model suggested that the effects of both variables were completely mediated by other variables in the system and did not have a direct association by themselves. As maternal age increased, the degree of social support also rose, whereas the likelihood of having children or adolescents in the household diminished, thus reducing the likelihood of CMD and HFI by extension. Alcohol misuse by a partner seemed to be related only to psychological violence, which, as already mentioned, was connected to HFI through several pathways.
Discussion
Both psychological and physical violence were identified as significant risk factors of HFI. The prominence of psychological violence in the process was noticeable. Its connection to HFI seemed to occur through at least three different pathways. One went through physical violence and CMD, another was exclusively through CMD, and the third path linked psychological violence directly to HFI. This direct route suggests that there are other variables mediating this relationship beyond mental disorders and physical violence. A hypothesis could be that in relationships in which psychological violence is the norm, the partner tends to exert control over the family’s budget as a means of establishing power and control over the woman, thus decreasing the priority of buying foodstuffs. This conjecture requires more in-depth discussion and research.
The notion that CMD precedes HFI also requires further research. Although backed by influential work in the scientific literature( 15 , Reference García-Moreno and Riecher-Rossler 37 ), this directionality requires further insight because it is not universally held. Some authors postulate that HFI is actually a risk factor for affective disorders, rather than the opposite( Reference Hadley and Patil 38 , Reference Vozoris and Tarasuk 39 ). Clearly, both directions are acceptable and further analyses examining non-recursive and/or time-related longitudinal transition models could shed further light on the matter( Reference Sorsdahl, Slopen and Siefert 40 , Reference Gundersen and Ziliak 41 ).
However, in keeping with the original hypothesis suggested in the ‘propositional’ model, CMD seemed to function as a mediator between both types of violence and HFI. Again, this is consistent with the specific literature on the repercussions of IPV, of which mental disorders among women are considered one of the most important( 15 , Reference Devries, Mak and Bacchus 42 – Reference Reichenheim, Moraes and Lopes 44 ). It is quite conceivable that the presence of these disorders affects women’s motivations to buy and cook food. This demotivation could be related to the loss of appetite and apathy that is commonly expressed in CMD and/or to the physical and psychological exhaustion often felt by people experiencing domestic violence( Reference Marazziti, Consoli and Picchetti 45 , 46 ). Another possibility is isolation. Women experiencing mental distress are less capable of seeking out help and support from government institutions designed to reduce HFI. In addition, there is the utilitarian hypothesis alluded to in the introduction according to which women exposed to violence and mental distress have more trouble getting and sustaining jobs or finishing school. Opportunities and adequate income thus progressively decrease, with insufficient diet ensuing as a long-term end result( Reference Chilton, Rabinowich and Woolf 10 , Reference Chilton, Knowles and Rabinowich 47 ). From this perspective, the finding that CMD is a significant factor in the process between both types of violence and HFI suggests that HFI is not just a result of short financial means to buy food. Dysfunctional relationships in a family, with or without other psychosocial risk factors such as alcohol abuse or drug use, seem to play a relevant role too.
The effective link between psychological and physical IPV is also related to previous studies and theories. The first investigations in the USA by Straus and Gelles( Reference Straus, Gelles and Steinmetz 48 , Reference Straus and Gelles 49 ) indicated that in most homes where there is physical violence, there is also a backdrop of psychological violence. Over the years, this finding has repeatedly recurred in the literature, continually underscoring the concomitance of different forms of violence in conflictive relationships within couples( Reference Krug, Dahlberg and Mercy 50 ) and the fact that psychological violence almost always precedes physical abuse( Reference Gellert 51 ).
Another noteworthy finding was that a low economic status was partially associated with HFI over psychological violence and increased mental disorders. This again indicates that in addition to the direct impact of low income on the means to buy food, part of the relationship could also be due to the greater vulnerability of these families to psychosocial stressors such as IPV and mental disorders. These findings reinforce the importance of considering more complex models that include different aspects of individuals’ lives to better understand the situations leading to HFI. Following corroboration, it would be helpful for interventions designed to reduce HFI to not be restricted to macro-structural measures such as cash transfers to boost family budgets but to consider other approaches to address IPV and the resulting emotional vulnerability of those involved.
Interestingly, alcohol misuse by the partner was related to HFI only through psychological violence and its consequences. Based on this premise, it may well be that when food insecurity occurs in families in which the partner abuses alcohol there is also rampant psychological aggression, which, if not tackled, may spiral into physical violence, mental distress and ultimately more insecurity. The current results also support evidence from previous research reporting that non-white women rearing children or adolescents as single mothers are considerably more prone to food insecurity( 52 – 55 ). These findings reinforce the proposition that different manifestations of violence among those most vulnerable play a fundamental role in food insecurity, illustrating the need to address HFI through multi-tiered interventions implemented by different professionals and sectors( 52 – 55 ).
The results of the current study should be considered in the light of its strengths and weaknesses. Jointly studying psychological and physical IPV in a single model is a positive aspect of the study. Another strength may be the novelty of investigating the associations between these two forms of IPV and HFI mediated by maternal mental health. Use of causal graphs was a strength in this regard because it allowed for the estimation of indirect relationships in addition to direct associations. Path analysis was additionally relevant to show the associations with other economic, demographic and lifestyle-related antecedents. Another favourable methodological decision was the population-based sampling strategy employed that enabled representative prevalence estimates of the events of interest. The use of different validated epidemiological instruments to measure more complex constructs deserves mentioning, as this helped reduce the underestimation of events and misclassification bias to some extent( Reference Moraes and Reichenheim 24 , Reference Straus, Hamby and Boney-McCoy 25 , Reference Reichenheim, Klein and Moraes 27 ). Still, future studies should contemplate more complex structural equation models to better address measurement errors.
Using a cross-sectional approach could be considered a potential weakness. According to Gundersen and Ziliak( Reference Gundersen and Ziliak 41 ), a causal relationship between food insecurity and other health outcomes in cross-sectional studies is not as clear. In principle, this data collection strategy cannot ensure that IPV precedes HFI. However, the 12-month time frame used to record violence should be extensive enough to represent events suffered over a long period of time, thereby covering habitual and persistent experiences of violent behaviour or victimization. The perspective that intimate violence is often a ‘chronic’ experience is grounded in the findings of several studies that reported that the time normally elapsing before a woman will end a violent relationship exceeds 10 years. Moreover, women who have suffered violence once tend to experience the same patterns of violence in subsequent relationships( Reference Krug, Dahlberg and Mercy 50 ). This tends to reinforce the hypothesis that the associations identified in the present study occur in mostly one direction, i.e. from left to right as conveyed in Fig. 2. However, some studies have noted that experiencing food insufficiency during childhood and adolescence could be a potential risk factor for depression and other mental health problems years later. To determine the directionality of this relationship would require a longitudinal study, which should be encouraged( Reference Alaimo, Olson and Frongillo 56 , Reference McIntyre, Williams and Lavorato 57 ).
As noted in the introduction, epidemiological studies on this subject are still rare. The current research programme is still in its infancy and, as such, the ‘final’ model should be viewed only as a start. Although it is a refined version of the cruder ‘propositional’ model, it still requires improvements and many issues to be addressed. Further corroboration studies are needed. The associations proposed and identified in the present study not only need to be replicated but should be studied through increasingly comprehensive models as previously stated. Unobserved characteristics related to both HFI and IPV may be likely and would need to be controlled for. Moreover, adding other factors that are not yet explored could lead to improved explanations. How the types of violence studied here are related to sexual violence, community violence and illicit drug consumption are still issues needing answers.
A relevant question concerns whether the study findings would hold true in different population domains and contexts. Despite recent progress in increasing the true income of the poorest in Brazil, the present results seem to suggest that HFI is still a major public health problem. Its frequency in the population studied (approx. 40 %) is higher than the national estimate (30·2 %) and the average identified in the State of Rio de Janeiro (28·3 %). The figures are more akin to those quoted for the north and north-east of the country (40·3 % and 46·1 %, respectively), which are known as the poorest regions of Brazil( 52 ). IPV, a reality in many homes, is also an issue worth addressing. As mentioned earlier, approximately two-thirds of the women interviewed reported having been involved in at least one act of psychological violence in the 12 months prior to the interview and a quarter of the women had experienced physical violence in the same period. It is quite likely that the magnitude of these two phenomena originates from the poor socio-economic conditions typical of the areas to which the study population belong. Future studies should evaluate the reproducibility of the main findings presented here in areas characterized by a higher income and level of education.
Despite the limitations and gaps mentioned above, the results of the present study indicate – and reinforce, if considered in light of the related literature( Reference Melchior, Caspi and Howard 4 , Reference Hernandez, Marshall and Mineo 5 , Reference Chilton and Booth 8 , Reference Chilton, Rabinowich and Woolf 10 ) – the importance of IPV and CMD in models designed to understand the processes leading to HFI. Recognizing these factors in families at risk may provide professionals involved in direct assistance more latitude in potential interventions. The findings are of equal importance to managers and professionals responsible for public health policies, as the results may offer key elements that can support recent and innovative approaches to eliminating this serious public health problem, which have been strongly called for by agencies involved in comprehensive intersectorial efforts( 58 , 59 ).
Acknowledgements
Financial support: E.S.M. was partially supported by the Brazilian National Research Council (CNPq). C.L.M. was partially supported by the CNPq (grant number 302430/2011-3) and the Rio de Janeiro Research Foundation (FAPERJ) (grant number E 26/110·756/2010). M.E.R. was partially supported by the CNPq (grant number 301221/2009-0). The institutions contributed to the study design, conduct of the study, analysis of data, interpretation of findings and the preparation of the manuscript. Conflict of interest: None. Authorship: C.L.M. designed the study, supervised the data collection process, undertook the analysis and collaborated in writing the manuscript. E.S.M. collaborated in analysing the data and writing the final version of the manuscript. M.E.R. designed the study, supervised the data collection process, undertook the analysis and collaborated in writing the manuscript. M.F.F. collaborated in undertaking the literature review and in the data analysis. R.S.C. collaborated in designing the study, in supervising the data collection process and in writing the final version of the manuscript. All authors have read and approved the final manuscript. Ethics of human subject participation: The research was approved by the Ethics Committee of the Federal University of Rio de Janeiro (protocol number 73/2009).