More than 89 % of the African population was at risk of insufficient iodine intake before the wide-scale implementation of population-oriented iodine supplementation through food fortification around 1995(Reference Kavishe1,Reference Joy, Ander and Young2) . Iodine deficiency to a large extent was a result of low iodine content in soil and groundwater, and a diet rich in goitrogens(Reference Taga, Oumbe and Johns3–Reference Farebrother, Zimmermann and Abdallah5). As from 1995, nationwide universal salt iodisation became the main approach of population-based iodine fortification in most African countries(Reference De Benoist, McLean and Andersson6). Other vehicles of iodine fortification in some African countries include bouillon cubes, canned foodstuffs and other processed foods which are not necessarily regularly consumed(Reference Abu, Oldewage-Theron and Aryeetey7,Reference Spohrer, Knowles and Jallier8) .
Iodine nutritional status in countries in Africa and elsewhere around the world has been monitored using school-age children (SAC) median urinary iodine concentration (mUIC)(9). However, SAC mUIC does not correctly predict iodine nutritional status in pregnancy(Reference Gowachirapant, Winichagoon and Wyss10,Reference Wong, Sullivan and Perrine11) . This can be attributed to the pregnancy-induced physiological changes that predispose pregnant women to iodine deficiency through increased thyroid hormone production, increased renal perfusion, increased iodine filtration and urinary iodine excretion in addition to increased transfer of iodine to the fetus(Reference Zantour, Alaya, Marmouch and Potluková12). In the general population, a mUIC of 100–199 μg/l is considered sufficient nutrition, while a pregnancy median UIC (pMUIC) below 150 μg/l indicates insufficient iodine intake(Reference Zantour, Alaya, Marmouch and Potluková12).The prevalence of insufficient iodine intake in pregnancy is likely to be high in African countries where a significant proportion of the population has mUIC below 150 μg/l. In such countries, large proportions of women of childbearing age could therefore be at risk of iodine deficiency in pregnancy and associated adverse outcomes such as miscarriage, fetal and childhood growth restriction, still-birth, postpartum thyroiditis, subclinical and overt hypothyroidism, dyslipidaemia, neuro-cognitive and psychomotor deficits(Reference Zimmerman and Boelaert13–Reference Lee, Shin and Song15). There is a paucity of data on iodine nutrition status in pregnancy in Africa. Hence, this study was carried out to assess the prevalence of iodine deficiency in pregnancy in Africa using the estimated pMUIC.
Methods
We estimated iodine nutrition in pregnancy using the most recent SAC mUIC from the Iodine Global Network (IGN) 2019 score card(16). The IGN publishes and updates the national iodine nutrition status for most countries every 2 years. In the IGN 2017 score card(17), sixty-five countries, including eleven in Africa, had data showing both SAC mUIC and pMUIC. We plotted the SAC mUIC against the pMUIC of these sixty-five countries to depict the linear relationship between the SAC mUIC and the pMUIC (Fig. 1) defined by the following regression equation:
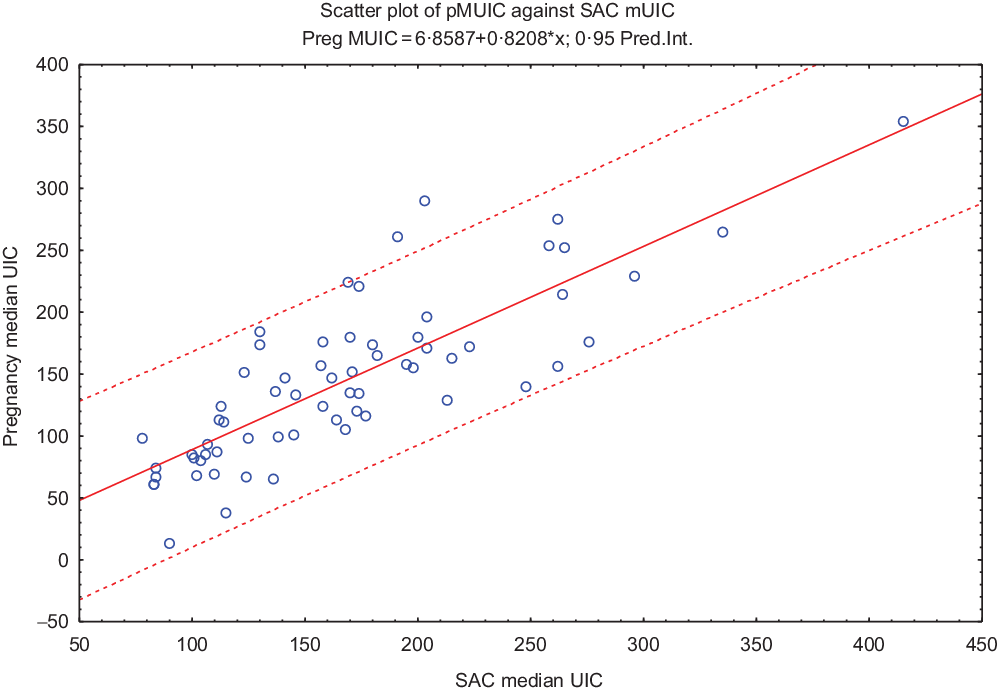
Fig. 1 Scatter plot, line of best fit and regression equation of pregnancy median urinary iodine concentration (UIC) against school-age children (SAC) median UIC
pMUIC = 6·8587 + 0·8208 × SAC mUIC (r = 0·8164, P < 0·001; r 2 = 0·6665)
Using this regression equation and the most recent SAC mUIC of African countries obtained from the IGN 2019 score card(16), the pMUIC was estimated for all the African countries with recent iodine nutrition survey data.
Results
Fifty of the fifty-five countries in Africa had data on iodine nutrition status in the general population, estimated mainly through SAC UIC surveys (44/50) carried out between 2002 and 2018, exception for Botswana, Central African Republic, Rwanda and Swaziland where the most recent SAC UIC surveys were conducted between 1993 and 1999. Eleven of these fifty countries also had pMUIC survey data(16,17) . Four countries had the iodine nutrition status estimated through surveys involving samples of women of reproductive age (Algeria, Gambia, Madagascar and Sierra Leone), one from a sample of adults (Mauritius) and another from a sample with broad age (Central African Republic). Five countries (Congo, the Comoros, Libya, Sao Tome and Principe, and Seychelles) had no data on iodine nutrition.
Of the fifty countries with UIC survey data available, three had insufficient iodine intake with moderate deficiency (20–49 µg/l); seven had insufficient iodine intake with mild deficiency (50–99 µg/l); eighteen had adequate iodine intake (100–199 µg/l); seventeen had more than adequate iodine intake (200–299 µg/l) exposing susceptible population groups to iodine-induced hyperthyroidism, while five had excessive iodine intake (≥300 µg/l) which increases the risk of autoimmune thyroid disease in addition to iodine induced hyperthyroidism(Reference Andersson, Karumbunathan and Zimmermann18) (Table 1).
Table 1 School-age children (SAC) median urinary iodine concentration (mUIC), measured and estimated pregnancy mUIC (pMUIC) (μg/l) for African countries
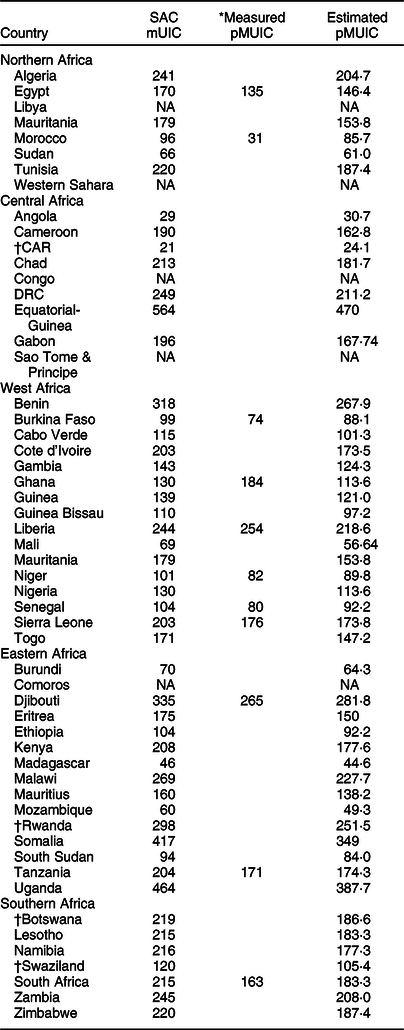
NA: data not available.
* Measured pregnancy median UIC (IGN 2017).
† Data collected before 2002.
The African countries with the lowest iodine intake in the general population (moderate iodine deficiency status) were Angola, Central African Republic and Madagascar. Most countries with mild iodine deficiency were from Eastern and Western Africa, while countries with optimal iodine nutrition in the general population were evenly distributed across the northern, eastern and western regions of Africa. All Southern Africa countries apart from Swaziland had more than adequate iodine intake in the general population (SAC mUIC 200–299 µg/l). Benin, Djibouti, Equatorial-Guinea, Somalia and Uganda had excessive iodine intake (SAC mUIC > 300 µg/l), likely attributable to enthusiastic implementation of iodine fortification programmes without regular evaluation(Reference Andersson, Karumbunathan and Zimmermann18); and in the case of Somalia and Djibouti, the use of ground water that has high iodine concentration(Reference Farebrother, Zimmermann and Abdallah5).
Of the eleven African countries with pMUIC survey data, Burkina Faso, Egypt, Morocco, Niger and Senegal had inadequate iodine intake during pregnancy. Ghana, Sierra Leone, South Africa and Tanzania had adequate intake, while Djibouti and Liberia had more than enough iodine intake in pregnancy(17).
The pMUIC values calculated in the current study are comparable to findings from population-based surveys from nine countries. The exceptions include Ghana (with sufficient intake) found to have insufficient iodine intake in pregnancy in the current study and Liberia (more than adequate intake) classified as having adequate iodine intake in pregnancy (Fig. 2).
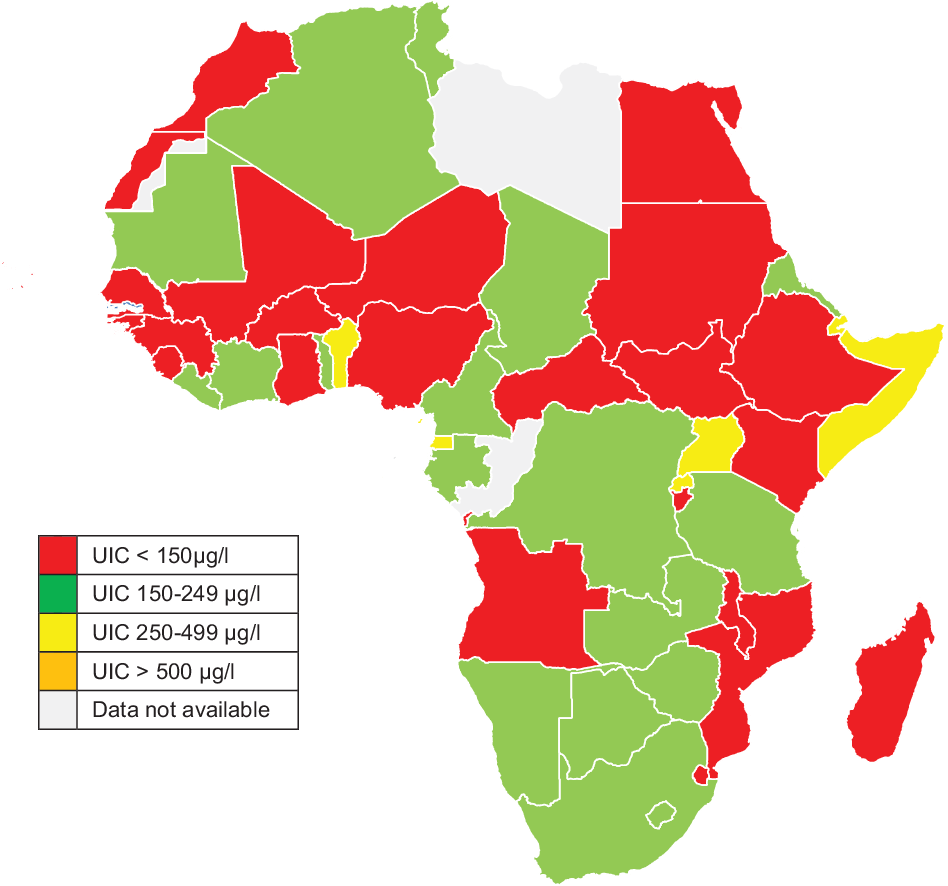
Fig. 2 Map of Africa showing country-specific iodine nutrition status during pregnancy (pregnancy median urinary iodine concentration (UIC)) as estimated from school-age children (SAC) median UIC
After applying the WHO criteria for monitoring progress towards sustainable IDD elimination where pMUIC < 150 μg/l indicates insufficient iodine intake during pregnancy(Reference De Benoist, Andersson and Egli19), twenty-two of the forty-four countries with median SAC data available had insufficient iodine nutrition during pregnancy (Fig. 2). Sixteen had adequate and five had more than adequate iodine intake in pregnancy. None of the African countries with available data had pMUIC in the range of excessive iodine intake (pMUIC > 500 μg/l). The current study also found that a cut-off school age mUIC of ≤175 µg/l correlated with insufficient iodine intake in pregnancy (pMUIC ≤ 150 μg/l) (Fig. 1).
Egypt, Gambia, Ghana, Guinea, Guinea-Bissau, Niger, Nigeria, Senegal and Togo are African countries classified as having sufficient iodine intake in the general population (IGN 2019) that in the current study have been found to have insufficient iodine intake in pregnancy (estimated pMUIC < 150 μg/l).
Discussion
Despite more than 25 years of iodine fortification in Africa, the prevalence of iodine deficiency in pregnancy in Africa appears to have remained high. This high prevalence seems to be masked by the reliance on SAC mUIC for the monitoring of the iodine nutrition status of populations. Although forty out of fifty African countries are currently classified as having adequate or more than adequate iodine intake based on SAC mUIC (IGN 2017 and IGN 2019), the current study estimated that pregnant women in more than half of the forty countries may be prone to insufficient iodine intake. This finding correlates with results from other studies that have shown SAC mUIC to inaccurately reflect the state of iodine nutrition of pregnant women within the same study settings(Reference Gowachirapant, Winichagoon and Wyss10,Reference Wong, Sullivan and Perrine11,Reference Lazarus20) . The observed discrepancy between the SAC mUIC and pMUIC can be attributed to variations in access to iodine-fortified foodstuffs, differences in food choices between school-age children and pregnant women, and the high depletion of iodine stores in pregnancy secondary to increased thyroid hormone production, elevated renal filtration and urinary iodine excretion, and trans-placental transfer of iodine to the fetus(Reference Gowachirapant, Winichagoon and Wyss10–Reference Zantour, Alaya, Marmouch and Potluková12).
If the results of the current study are confirmed by future studies, there will be a need to revisit ongoing iodine fortification strategies, especially in endemic areas for iodine deficiency. While universal salt iodisation is a popular and inexpensive approach suggested by the WHO and ICCIDD, African countries with pMUIC < 150 µg/l could require iodine supplementation during pregnancy, especially those countries with SAC mUIC below 175 µg/l. Oral iodised oil has previously been shown to improve and maintain the level of iodine nutrition within normal limits among adults and children in areas with endemic iodine deficiency, without causing neonatal or maternal hypothyroidism, hyperthyroidism or auto-immune thyroiditis(Reference Benmiloud, Chaouki and Gutekunst21–Reference Delange23). This may help mitigate the morbidity that may accrue from widespread insufficient iodine nutrition in pregnancy in Africa.
Since iodine deficiency tends to induce the most adverse effects during pregnancy, infancy and lactation, an appropriate assessment of iodine nutrition would benefit from a direct estimation of the pMUIC as one of the baseline metrics. This can be complemented by assessing the iodine nutrition status of infants, although this may be quite challenging. This could however be achieved through the use of the dry blood spot thyroglobulin test(Reference Stinca, Andersson and Weibel24) if this becomes readily available for public health use in iodine deficient endemic areas and populations.
Although the current study found that five African countries are likely to have more than adequate iodine intake in pregnancy, the thyroid dysfunction associated with high iodine intake tends to be transient and mild, especially if the increase in iodine intake in formerly iodine-deficient countries was gradual(Reference Andersson, Karumbunathan and Zimmermann18). Populations in countries with endemically higher water iodine content such as Djibouti and Somalia tend to be tolerant to high daily iodine intake(Reference Farebrother, Zimmermann and Abdallah5). However, it is recommended that excessive iodine intake should be prevented, especially in countries formerly with chronic iodine deficiency(Reference Laurberg, Cerqueira and Ovesen25).
Strength and limitations
This study has provided an estimate of the level of iodine nutrition state in pregnancy for most countries in Africa and the minimum SAC mIUC that can be used to predict adequate iodine nutrition status among pregnant women in these settings. The current study design precluded a reliable estimation of the true magnitude of iodine deficiency in pregnancy. However, the data from the current study form a basis for further research to ascertain the true iodine nutrition status among pregnant women in various countries in Africa. While deriving the regression equation for estimating the pMIUC, we assumed that SAC mUIC would correlate with pMIUC. However, this may not always be the case given the different vehicles of iodine fortification around the world and the diverse nutritional practices during pregnancy.
Conclusion
Insufficient iodine nutrition in pregnancy seems to be prevalent in several African countries, even in countries thought to have sufficient iodine intake in the general population on the basis of SAC mUIC surveys. The SAC mUIC, the current recommended method by WHO to assess iodine nutrition status, seems to conceal insufficient iodine nutrition in pregnancy. Optimum assessment of iodine nutrition status in pregnant women may not be achieved without direct estimation of the pMUIC. Oral iodised oil supplementation could be a possible remedy for insufficient iodine nutrition in pregnancy in countries with a high proportion of the population still prone to moderate-to-severe iodine deficiency despite universal salt iodisation.
Acknowledgements
Acknowledgements: Iodine Global Network for the primary data (IGN 2017 and 2019 score cards). Financial Support: The authors received no funding for this work. Conflict of interest: The authors have no competing interests. Authorship: C.B.B. conceived and designed the study, analysed and interpreted the data, and wrote the first manuscript. A.P.K. and L.M.B. critically reviewed the first manuscript. All the authors reviewed and approved the final manuscript. Ethics of human subject participation: This is not applicable as the study did not involve individual human participants.






