The older population is one of the fastest growing segments of the US population. The population aged 65 years and over increased 34 % from 37·8 million in 2007 to 50·9 million in 2017 and is projected to reach 94·7 million in 2060(1). Moreover, the average life expectancy of persons who have reached age 65 was 19·5 years(1). With the increased life expectancy, older adults face elevated risk of developing age-related chronic diseases. According to the Centers for Disease Control and Prevention(2,3) , 28·1 % of adults aged 65 years and older had heart disease, 26·8 % had diabetes and 19·3 % had cancer.
Fruits and vegetables are important components of a healthy diet, which promote healthy ageing. Fruits and vegetables contain a variety of vitamins and minerals, and dietary fibres that help maintain body function and health(Reference Slavin and Lloyd4). Fruits and vegetables also supply numerous phytochemicals which lower oxidative stress and inflammation and protect against age-related diseases(Reference Slavin and Lloyd4–Reference Song, Derito and Liu7). Previous studies have reported that higher fruit and vegetable consumption is associated with a lower risk of CVD(Reference Aune, Giovannucci and Boffetta8–Reference Dauchet, Amouyel and Hercberg10), type 2 diabetes(Reference Cooper, Sharp and Lentjes11,Reference Wang, Fang and Gao12) , and cancer(Reference Aune, Giovannucci and Boffetta8,Reference Jansen, Bueno-de-Mesquita and Feskens13) , as well as overall mortality(Reference Aune, Giovannucci and Boffetta8,Reference Bazzano, He and Ogden9,Reference Genkinger, Platz and Hoffman14,Reference Wang, Ouyang and Liu15) . Several studies also found that older adults with a higher intake of vegetables showed less or slower cognitive decline(Reference Kang, Ascherio and Grodstein16,Reference Morris, Evans and Tangney17) .
Despite the numerous health benefits, both fruit and vegetable consumption for most older adults is below daily recommendations. The US Department of Health and Human Services and the US Department of Agriculture(18) recommend eating 2–2½ cup equivalents of fruits and 2½–3½ cup equivalents of vegetables for males aged 51 years and older, and 1½–2 cup equivalents of fruits and 2–3 cup equivalents of vegetables for females aged 51 years and older. However, the average intake of fruits and vegetables was below these levels: 1·2 cup equivalents of fruits and 1·9 cup equivalents of vegetables for males aged 51–70 years, 1·4 cup equivalents of fruits and 1·7 cup equivalents of vegetables for males aged 71 years and older, 1·2 cup equivalents of fruits and 1·8 cup equivalents of vegetables for females aged 51–70 years and 1·3 cup equivalents of fruits and 1·5 cup equivalents of vegetables for females aged 71 years and older(18). In 2015, only 12·4 % of older adults met federal fruit intake recommendations and only 10·9 % met federal vegetable intake recommendations(Reference Lee-Kwan, Moore and Blanck19).
Appropriate fruit and vegetable consumption could potentially be more difficult for older adults living alone. Poor nutritional intake among older adults living alone, including lower frequency(Reference Tani, Kondo and Takagi20–Reference Murphy, Rose and Davis23) and lower diversity of food intake(Reference Conklin, Forouhi and Surtees24,Reference Conklin, Forouhi and Surtees25) , has been reported in previous studies. Lower consumption of fruits and vegetables among older adults living alone has also been observed(Reference Tani, Kondo and Takagi20,Reference Davis, Murphy and Neuhaus21,Reference Murphy, Rose and Davis23,Reference Hunter, McNaughton and Crawford26–Reference Sharkey, Johnson and Dean28) , suggesting living alone is a risk factor for poor nutrition and chronic diseases that are associated with fruit and vegetable consumption. This trend may occur because living alone in older age poses extra constraints that are associated with store accessibility, grocery shopping, meal preparation and eating appropriately, including poor health and physical limitations, financial difficulties and social isolation.
Social networks have been identified as a protective factor reducing poor nutrition and low fruit and vegetable consumption, since these networks can be a source of instrumental support, including help with grocery shopping and cooking(Reference Tani, Kondo and Takagi20,Reference Conklin, Forouhi and Surtees24,Reference Bloom, Edwards and Jameson29–Reference Salehi, Eftekhar and Mohammad32) . Also, social engagements provided by social networks motivate older adults to cook and eat healthy, while loneliness and eating alone were associated with undesirable dietary patterns, including meal skipping, low intake of core foods (e.g. fruits, vegetables and fish) and low nutrient intake or malnutrition(Reference Tani, Kondo and Takagi20,Reference Davis, Murphy and Neuhaus21,Reference Conklin, Forouhi and Surtees24,Reference Sharkey, Johnson and Dean28,Reference Boulos, Salameh and Barberger-Gateau33,Reference Hanna and Collins34) . In this sense, children and friends living nearby could be a potential source of social and emotional support, encouraging a healthy diet, including fruit and vegetable consumption, especially for older adults living alone.
However, our understanding of the role of social networks in the relationship between living alone and fruit and vegetable consumption is limited. Therefore, the current study aims to use the 2013 Health Care and Nutrition Survey (HCNS) of the Health and Retirement Study (HRS) to investigate whether living arrangements and having children and friends nearby are associated with daily fruit and vegetable consumption among older adults. Based on previous findings, we hypothesise that older adults who live alone will have lower fruit and vegetable consumption than those who are living with someone, and older adults who have children and/or friends nearby will have higher fruit and vegetable consumption than those who do not have children or friends nearby. The findings of the current study may contribute to our understanding of older adults’ fruit and vegetable consumption, help to identify older adults who are at the greatest risk of poor nutrition and promote healthy eating, which will eventually help maintain or even improve their health.
Methods
Data and sample
The HRS has engaged in biennial surveys of approximately 20 000 people from a nationally representative sample of older Americans (over age 50) since 1992. The HRS has been widely used in previous studies that explored issues related to older adults living alone(Reference Henning-Smith, Shippee and Capistrant35–Reference Waite and Hugfies39).
For the current study, we used the 2013 HCNS, an off-year supplement of the HRS. For the HCNS, the survey questionnaires on healthcare access, food purchases, food consumption and nutrition were mailed to a subsample of the HRS respondents and their spouses/partners (n 12 418), and 65 % (n 8073) completed the survey(40). Respondents who provided answers to <3 % of the food consumption questions (n 37) and respondents who were using a feeding tube (n 1) were removed from the data set by the HRS team(40). The HRS replenished the sample in 2010 with a younger cohort, so in 2013 the sample was aged 53 years and older. Since the 2013 HCNS includes a subsample of the HRS respondents and their spouse/partner regardless of their age, we excluded those who were below age 53 when interviewed (n 535) to only include age-eligible respondents. Several HRS data files with sociodemographic, social network and neighbourhood environment information, collected in 2012, were then merged with the HCNS, and respondents who were not included in other HRS data products (i.e. HRS, RAND HRS and HRS Contextual Data Resources) (n 245) and those with missing values on key variables and covariates (n 390) were excluded from the sample. The independent variable and four control variables, poverty/food insecurity, self-perceived health, difficulties and help with meal preparation, and following a special diet, contained missing values. Respondents who were excluded from the analytic sample are more likely to be non-Hispanic Blacks, Hispanics, and had higher educational attainments, greater daily energy intakes and more healthy food outlets. No significant differences in age, sex and difficulties and help with grocery shopping are observed. We conducted Little’s test of missing completely at random and confirmed that the missing data in the five variables were missing at random.
After excluding respondents with missing data, the analytic sample included 6865 respondents, 91·5 % of the age-eligible sample (see Fig. 1). When data have missing values >10 %, the results obtained from the data may be biased(Reference Bennett41). Since the data missing constituted about 8·5 % of the age-eligible sample, omitting these respondents should not bias the results.
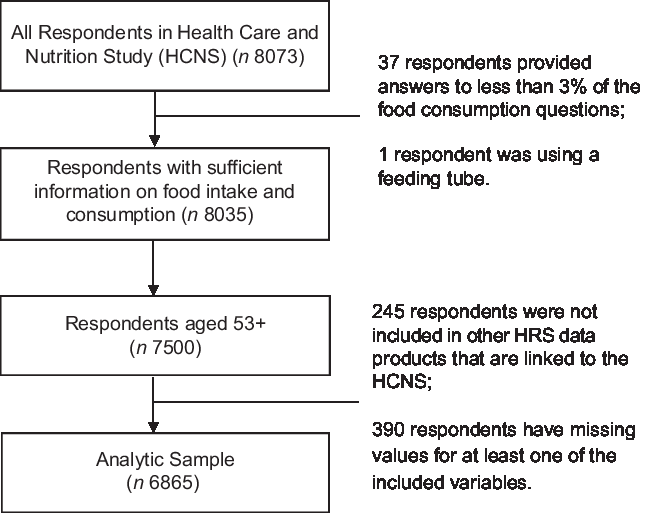
Fig. 1 Sample inclusion criteria
Measures
Daily fruit and vegetable consumption
Respondents were asked about their average intake of nineteen fruits and twenty-eight vegetables over the past 12 months, including related food products (e.g. juice and sauce). For each item, a different unit and response option were provided. For example, the unit for melon (e.g. cantaloupe, honeydew and watermelon) was a 1/4 melon, and the response options for the average intake include ‘never,’ ‘less than once per month,’ ‘1–3 times per month,’ ‘once per week,’ ‘2–4 times/week,’ ‘5–6 times per week,’ ‘once per day,’ ‘2–3 times per day’ and ‘4 or more servings per day.’ Based on participants’ responses, the University of Michigan calculated a daily serving portion for each item, using Harvard University’s food serving conversion guides (https://regepi.bwh.harvard.edu/health/nutrition.html). ‘For example, 1 serving per week is equivalent to 0·14 servings per day (1/7), and 5–6 servings per week is equivalent to 0·8 servings per day (5·5/7)’(40). For the analysis, we summed daily serving portions of twelve fruits and twenty-one vegetables to create measures for overall fruit and vegetable consumption (summed number of servings per day). To reflect the intake of fresh fruit and vegetables, items such as juices and sauces were excluded. Daily fruit and vegetable consumption ranged from 0 to 24 and 0 to 26 servings, respectively. Due to skewness of the distribution, we top-coded both fruit and vegetable consumption at the 99th percentile, with the final category indicating six or more servings for fruits and nine or more servings for vegetables.
Living arrangements and social networks in neighbourhoods
The HRS includes information on respondents’ living arrangements and on their social networks in their neighbourhoods.
In the HRS, living arrangements had six categories: (0) married or partnered, living with partner; (1) married or partnered, not living with spouse/partner; (2) not married or partnered, living with other unrelated adult; (3) not married or partnered, living with relative (including minor children) or unrelated minor child; (4) not married or partnered, living alone; and (5) living arrangements unknown. Regarding their social networks, participants were asked if they had children within ten miles ((0) no; (1) yes) and good friends in their neighbourhood ((0) no; (1) yes). Using these questions, we created a new variable with four categories: (0) living with someone (i.e. spouse/partner, children, relative or other unrelated adults) and having children and/or friends nearby; (1) living with someone and having no children or friends nearby; (2) living alone and having children and/or friends nearby and (3) living alone and having no children or friends nearby. Having children with whom the respondent had no contact as no.
The control variables included age, gender ((0) male; (1) female), race/ethnicity ((0) White/other, non-Hispanic; (1) Black, non-Hispanic; (2) Hispanic), years of education, poverty/food insecurity ((0) household income above poverty threshold and enough money to buy food; (1) household income below poverty threshold and/or not enough money to buy food), self-perceived health ((0) poor–(4) excellent), difficulties and help with grocery shopping and meal preparation due to health or memory problems ((0) no difficulty; (1) difficulty, receiving help; (2) difficulty, not receiving help), following a special diet (e.g. weight reduction/low energies, low cholesterol, low Na, diabetic, low fat, low TAG, ulcer and high potassium), daily energy intake (divided by 1000 and then logged) and number of healthy food outlets (i.e. grocery stores and farmers’ markets) in respondents’ county of residence.
Statistical analysis
We first presented descriptive information on the analytic sample. T tests and χ 2 tests were conducted to compare gender differences. Bivariate analyses were then conducted to ascertain differences in daily fruit and vegetable consumption (i.e. number of servings per day, whether daily recommendations were met) according to living arrangements (i.e. living with someone v. living alone) and social networks in the neighbourhood (e.g. having no children or friends nearby v. having children or friends nearby). Finally, a series of multivariate analyses examining the relationship of living alone and having children or friends nearby with fruit and vegetable consumption were conducted using Stata 15. Based on previous findings on gender differences in food intake and eating behaviour(Reference Tani, Kondo and Takagi20,Reference Davis, Randall and Forthofer22,Reference Bennett41) , we stratified the models by gender. Daily serving portions of fruits and vegetables are count variables; therefore, Poisson regression models were used in these estimations. For these analyses, we applied sample weights provided by the HRS to account for differential selection probabilities due to the complex survey design.
Results
Participant characteristics
Table 1 presents descriptive information on the analytic sample. The average fruit and vegetable consumption was 0·95 (sd 1·18) and 2·18 (sd 1·90) servings, respectively, which is significantly lower than the daily recommendations of 2–3 servings of fruits and 4–6 servings of vegetables(18) (P < 0·001, except for vegetable consumption among females which was not statistically different from the daily recommendation). Most of the sample respondents were living with someone and had children or friends nearby (64·0 %) and were female (55·0 %), non-Hispanic White/other (84·1 %), not in poverty and food secure (84·0 %), have no difficulty with grocery shopping (94·5 %) and meal preparation (84·5 %), and not following a special diet (84·5 %). The average age was 66·07 (sd 9·72), the average years of education was 13·33 (sd 2·83), the average self-perceived health was 2·32 (sd 1·05), which is between good and very good, the average daily energy consumption, which was divided by 1000, was 1·84 (sd 1·00), and the average number of healthy food outlets in respondents counties (471 counties) was 221·52 (sd 423·52).
Table 1 Descriptive information on the analytic sample (n 6865)*
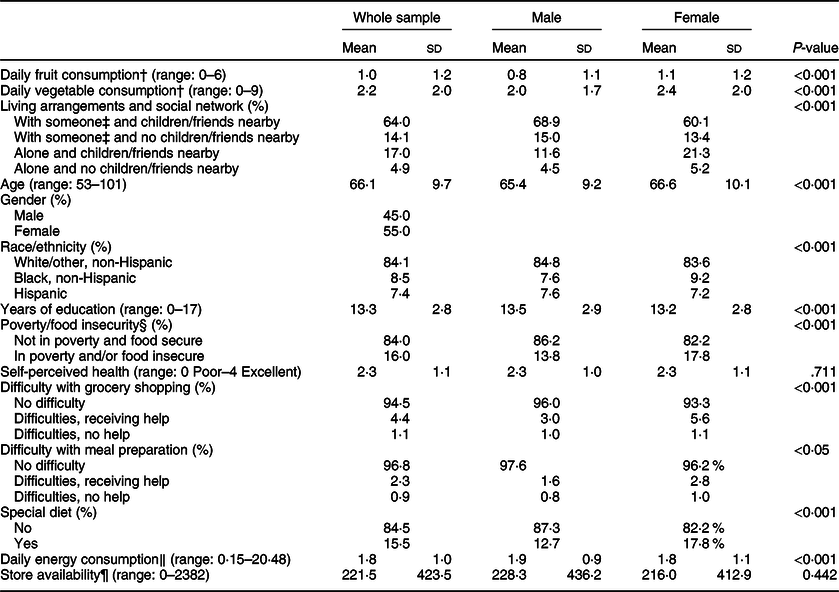
* T tests and χ 2 tests were conducted to compare gender differences.
† Daily fruit and vegetable consumption is summed by number of servings per day.
‡ Living with spouse/partner, children and/or others.
§ Household income below poverty threshold and/or not enough money to buy food.
‖ Daily energy intake was divided by 1000.
¶ Number of healthy food outlets (i.e. grocery stores and farmers’ markets) (county-level).
Older females consumed a slightly greater number of fruits and vegetables compared with older males.
Bivariate analysis
We performed bivariate analyses to ascertain differences in daily fruit and vegetable consumption according to living arrangements and social networks (Table 2). While other groups consumed a similar amount of fruits and vegetables (0·87–1 serving of fruits and 2·12–2·25 servings of vegetables), older adults who lived alone with no children or friends nearby consumed the lowest amount of fruits and vegetables. The average servings of fruits and vegetables for them were 0·69 and 1·67, respectively, which were approximately 70 and 74 % of the number of servings consumed by older adults who lived with someone and had children or friends nearby.
Table 2 Pairwise differences in fruit and vegetable consumption (n 6865)†
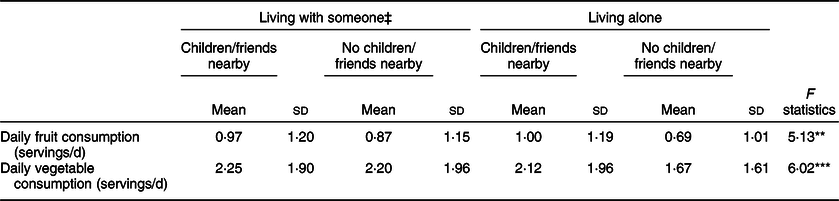
† The model F-statistic was obtained by a series of simple (bivariate) regression models.
‡ Living with spouse/partner, children and/or others.
**P < 0·01, ***P < 0·001.
Living alone, having children and friends nearby, and daily fruit and vegetable consumption
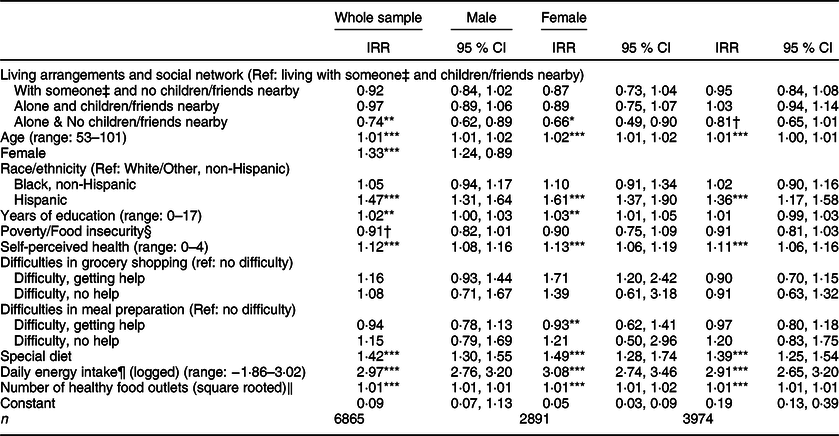
Tables 3 presents the results of the Poisson regression models for the association of living arrangements and social networks in the neighbourhood with daily fruit consumption (servings/d). Compared with older adults who lived with someone and had children or friends nearby, daily servings of fruit consumption were lower by 8 % for those who lived with someone and had no children and friends nearby (incidence rate ratio (IRR) = 0·92; 95 % CI 0·84, 1·02, P > 0·10) and by 3 % for those who lived alone and had children or friends nearby (IRR = 0·97; 95 % CI 0·89, 1·06, P > 0·10) although statistically insignificant. Living alone without children and friends nearby was statistically associated with a 26 % decrease in daily fruit consumption, or about 1/3 of a serving (IRR = 0·74; 95 % CI 0·62, 0·89, P < 0·01).
Table 3 Poisson regression explaining daily fruit consumption (servings/d)

IRR, incidence rate ratio.
† P < 0·10, *P < 0·05, **P < 0·01, ***P < 0·001.
‡ Living with spouse/partner, children and/or others.
§ Household income below poverty threshold and/or not enough money to buy food.
¶ Daily energy intake was divided by 1000.
‖ Grocery stores and farmers’ markets in respondents’ county of residence.
Table 4 presents the results of the Poisson regression models explaining vegetable consumption (servings/d). Compared with older adults who lived with someone and had children or friends nearby, daily servings of vegetable consumption decreased by 3 % for those who lived with someone and had no children and friends nearby (IRR = 0·97; 95 % CI 0·91, 1·04, P > 0·10) and by 5 % for those who lived alone and had children or friends nearby (IRR = 0·95; 95 % CI 0·90, 1·02, P > 0·10). The number of servings of vegetables consumed by respondents who lived alone without children and friends nearby decreased by 25 % compared with those who lived with someone and had children or friends nearby (IRR = 0·75; 95 % CI 0·67, 0·85, P < 0·001).
Table 4 Poisson regression explaining daily vegetable consumption (servings/d)
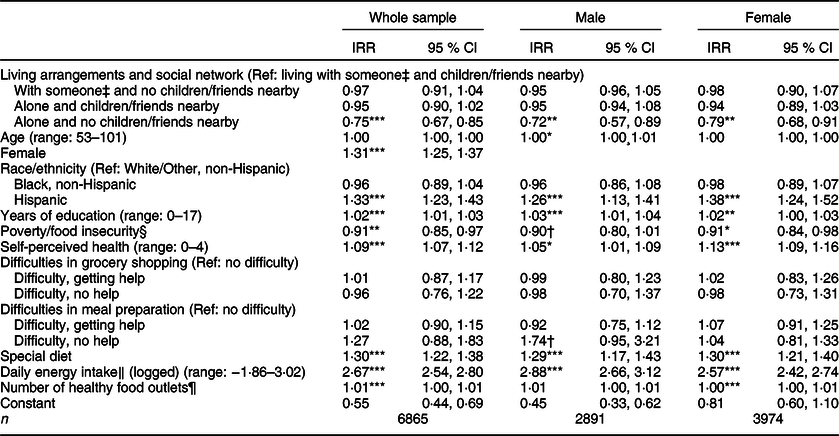
IRR, incidence rate ratio.
† P < 0·10, *P < 0·05, **P < 0·01, ***P < 0·001.
‡ Living with spouse/partner, children, and/or others.
§ Household income below poverty threshold and/or not enough money to buy food.
‖ Daily energy intake was divided by 1000.
¶ Grocery stores and farmers’ markets in respondents’ county of residence.
Older age (significant only for fruits), being female, being Hispanic, higher education, better health status, following a special diet, greater daily energy intake and greater availability of healthy food outlets were associated with higher fruit and vegetable consumption, while poverty and/or food insecurity were associated with lower fruit and vegetable consumption.
Gender differences
Overall, the results of stratified models showed similar patterns, although a greater decrease in the daily fruit and vegetable consumption was observed among men when they lived alone with no children or friends nearby. Compared with those who lived with someone and had children or friends nearby, daily fruit consumption decreased by 34 % or about 1/2 serving for older men (IRR = 0·66; 95 % CI 0·49, 0·90, P < 0·05) and 19 % for older women (IRR = 0·81, 95 % CI 0·65, 1·01, P < 0·10) who lived alone without children or friends nearby. Living alone without children or friends nearby was also associated with a decrease in daily vegetable consumption of 28 %, or about 1/3 serving among older men (IRR = 0·72, 95 % CI 0·57, 0·89, P < 0·01) and a 21 % decrease among older women (IRR = 0·79, 95 % CI 0·68, 0·91, P < 0·01). However, an interaction term to test the gender difference was not statistically significant.
Secondary analysis
We conducted additional analyses to see if living alone and having social networks in neighbourhoods are associated with meeting daily recommendation for fruits and vegetables rather than the numbers of servings (see Supplementary Material Tables S1 and S2). Similar patterns were shown for meeting the daily recommendations for fruits and vegetables. For example, compared with older adults who lived with someone and had children or friends nearby, the likelihood of meeting daily recommendations for fruits and vegetables was 39 % (OR = 0·62, 95 % CI 0·34, 1·14, P > 0·10) and 55 % (OR = 0·45, 95 % CI 0·27, 0·76, P < 0·01) lower for those who lived alone without children or friends nearby.
We also explored whether there was any difference between having children and having friends nearby and found that having friends nearby was consistently associated with greater daily fruit and vegetable consumption as well as an increased likelihood of meeting daily recommendations for fruits and vegetables among older females. However, having children nearby was not significantly associated with fruit and vegetable consumption. The effect of social networks (having children or friends nearby) on fruit and vegetable consumption was greater for older adults who were living alone. The results are shown in the online Supplementary Material (Tables S3 and S4).
Discussion
This is the first study, to our knowledge, that uses a nationally representative sample of older Americans to examine whether social networks in homes and neighbourhoods are associated with daily fruit and vegetable consumption. The results suggest that living alone is associated with lower fruit and vegetable consumption, which is consistent with the existing literature(Reference Tani, Kondo and Takagi20,Reference Davis, Randall and Forthofer22,Reference Murphy, Rose and Davis23,Reference Hunter, McNaughton and Crawford26–Reference Sharkey, Johnson and Dean28) . Previous studies have identified poor physical health and financial constraints, which are prevalent among older adults living alone(Reference Kharicha, Iliffe and Harari27,Reference Stepler43) , as barriers to healthy eating which affect access to food, cooking and meal preparation(Reference Sharkey, Johnson and Dean28,Reference Salehi, Eftekhar and Mohammad32,Reference Lyon and Colquhoun44–Reference Sidenvall, Nydahl and Fjellström48) . Lack of motivation for cooking and eating due to social isolation, loneliness and depression may be another reason for lower fruit and vegetable consumption among older adults living alone(Reference Conklin, Forouhi and Surtees24,Reference Sidenvall, Nydahl and Fjellström48,Reference Locher, Robinson and Roth49) . Previous studies have reported that older adults living alone are also more likely to be socially isolated and to suffer from loneliness and depression(Reference Kharicha, Iliffe and Harari27,Reference Dean, Kolody and Wood50–Reference Stahl, Beach and Musa52) .
The results of the current study also revealed that social networks in neighbourhoods may attenuate the negative associations between living alone and daily fruit and vegetable consumption. The daily fruit and vegetable consumption of respondents who lived alone with children or friends nearby was not statistically different from those who lived with someone and had children or friends nearby, while those who lived alone without children or friends nearby had significantly lower fruit and vegetable consumption. This may be because social interaction and support from children and friends help with acquiring and preparing fruits and vegetables and encourage healthy eating(Reference Salehi, Eftekhar and Mohammad32,Reference Nicklett and Kadell42,Reference Seguin, Connor and Nelson47) . In a study by Huang et al.(Reference Huang, Rosenberg and Simonovich53), rides from friends were the second most frequently used transportation mode to access food-related destinations. Coveney and O’Dwyer(Reference Coveney and O’Dwyer54) also found that help from family and friends increases people’s access to food. Having children and friends may also increase the number of social gatherings and prevent people from eating alone, which motivates cooking and eating(Reference Nicklett and Kadell42,Reference Locher, Robinson and Roth49) . However, having children or friends nearby did not make a significant difference in fruit and vegetable consumption among cohabiting respondents. Our findings suggest that having a social network either at home or in the neighbourhood complements the absence of one or the other.
Previous studies have reported that men are more affected by living arrangements and social networks in terms of eating behaviours, including food and nutrient consumption(Reference Tani, Kondo and Takagi20,Reference Davis, Randall and Forthofer22) because men tend to be less concerned about health and nutrition and have limited cooking skills(Reference Tani, Kondo and Takagi20,Reference Budesa, Egnor and Howell55,Reference Hartmann, Dohle and Siegrist56) . In our study, the decrease in the number of servings of fruits and vegetable was greater among men when they lived alone with no children or friends nearby. However, the difference was not statistically significant. This may be because fruit and vegetable consumption does not require complex cooking skills.
In the secondary analyses, having friends nearby was consistently associated with higher daily fruit and vegetable consumption for older women. The social and emotional support that friends provide may be an explanation for this finding. The findings of Rugel and Carpiano(Reference Rugel and Carpiano57) indicate the importance of emotional and informational support in promoting older women’s fruit and vegetable consumption, and greater emotional and psychological benefits from friends over family members, including children, have been reported in the previous studies(Reference Larson, Mannell and Zuzanek58–Reference Huxhold, Miche and Schüz61). However, having children nearby was not significantly associated with fruit and vegetable consumption for both men and women. This may be because relying on children violates the norms associated with older adults’ parent role(Reference Silverstein, Chen and Heller62,Reference Thomas63) and prevents older adults from asking their children for help.
Limitations
The current study has several limitations. First, we used a measure of social networks that may not completely reflect social relationships or interactions. For example, having children nearby was measured by using the question ‘Do you have children living within ten miles?’ This question does not provide any further information about their relationship. In addition, while numerous studies highlighted social gatherings or the presence of people during mealtimes as motivators for cooking and eating(Reference Jansen, Bueno-de-Mesquita and Feskens13), we are unsure as to whether cohabitation or having social networks in the neighbourhood increased opportunities for social gatherings or in-person interactions. Therefore, further research should be conducted for a more comprehensive understanding of older adults’ fruit and vegetable consumption. Last, sociodemographic, social network and neighbourhood data were derived from multiple HRS products that were collected in 2012. Although this information often does not change greatly within a short period of time, there is a potential discrepancy in social networks and food environments due to the 1 year difference.
Conclusions
Existing literature emphasised the role of family and friends in promoting a healthy diet(Reference Murphy, Rose and Davis23,Reference Park, Smith and Dunkle38) . Our results confirm that living alone while having no children and friends nearby is associated with lower fruit and vegetable consumption, which highlights the importance of social networks at home and in the neighbourhood. Based on the findings, older adults who are living alone with a limited social network in the community may be at the greatest risk of poor nutrition due to low levels of social support and motivation to cook and eat. Provision of help with grocery shopping (e.g. transportation, Supplemental Nutrition Assistance Program) and meal preparation (e.g. home-delivered meals) as well as social support networks and more opportunities that can improve social engagement appear to be necessary in order to encourage a healthy dietary intake.
Acknowledgements
Acknowledgements: Not applicable. Financial support: This work was supported by the National Institute on Aging (T32-AG000037). Conflict of interest: None. Authorship: Y.J.C. formulated the research questions, designed the overall study, completed the analyses and wrote the original draft. J.A.A. and E.M.C. supervised the study and reviewed drafts of the article. Ethics of human subject participation: Not applicable. This study was conducted using a publically available data, which includes adults over age 50.
Supplementary material
For supplementary material accompanying this please visit https://doi.org/10.1017/S1368980020002475