Cash transfers (CT) are becoming a popular intervention of choice by agencies and non-governmental organisations as a complementary or alternative approach to food-based assistance, as part of an emergency response. There is strong evidence that CT programmes lead to an increase in household income and protect household assets from being sold, resulting in an increase in food quantity and improved dietary diversity which in turn are thought to protect children from malnutrition( 1 ). However, the evidence for an impact of CT on undernutrition is mixed and inconclusive( Reference Manley, Gitter and Slavchevska 2 – Reference Bailey and Hedlund 7 ). Despite this, CT are increasingly being used in emergency responses with an objective of preventing acute malnutrition.
The mainstay of interventions to treat and prevent moderate acute malnutrition among children aged 6 months to 5 years have been targeted supplementary feeding programmes and blanket supplementary feeding programmes, respectively. The effectiveness of targeted supplementary feeding programmes in some contexts has been called into question( Reference Navarro-Colorado, Mason and Shoham 8 ), while the cost-effectiveness of blanket supplementary feeding programmes has also been challenged. As a result the use of unconditional CT is becoming more common, whereby cash is given to poor parents (usually the mother), who have children at risk of becoming undernourished, during periods of food insecurity or during emergencies.
The present study took place in Aguié district in Maradi region in southern Niger, where poverty and food insecurity have been identified as major factors contributing to undernutrition in children( 9 ). Over the past decade the prevalence of acute malnutrition in Maradi region has mostly remained above 15 %, the threshold applied by the WHO to classify the situation as critical, and is the highest within Niger. In November 2011 the Government of Niger declared a nutrition emergency.
If emergency CT programmes are to prevent malnutrition it is important to understand not only whether the cash is effective in safeguarding households’ assets, but also how cash is used and whether this has an indirect effect on children’s nutritional status. Due to the ethical difficulties of undertaking a randomised controlled study, the study described here was a prospective observational study. This pre–post intervention study involved the same cohort of households with a non-acutely malnourished child at baseline, to assess (i) changes in mediating factors within the causal pathway between unconditional CT and child nutritional status and (ii) risk factors for acute malnutrition post-intervention.
Methods
Study area
The study was conducted in the twenty-one villages participating in the Save the Children CT programme in Aguié department, located 80 km to the east of the regional capital, Maradi. The department has an estimated population of 386197 inhabitants whose livelihoods are based on agriculture and rearing livestock. The local agriculture is rain fed – between June and September millet, sorghum and legumes are cultivated, while livestock holdings are small. The period from April/May to September is the most difficult for households because it corresponds to both the lean and rainy seasons, when food availability is poor and field work is intense. During this time, the poorest households borrow grain or money to buy food, which peaks in price on the market due to insufficient supply( 10 ). Households are categorised into wealth groups according to local definitions of wealth and assets using a Household Economy Approach( 10 , 11 ). The Household Economy Approach defines a wealth group as a group of households sharing a similar capacity to exploit the different food and income options within a particular livelihood zone( 12 ), so the divisions depend on how the community views its own society. In this specific context the ‘poorest’ households were estimated to comprise 42 % of the community and typically had seven members, owned 0·8 ha of land, and had no cattle, two goats and four hens, while the ‘poor’ households comprised 28 % of the community and had eight household members, owned 1·5 ha of land, and had no cattle, three goats and eight hens( 10 ).
Save the Children UK has implemented CT programmes in Maradi and neighbouring Zinder nearly every lean season since 2008, except 2010, with the objective of protecting people’s livelihoods and preventing undernutrition. In 2012, the CT programme was part of a comprehensive, multi-sector emergency response strategy including health, nutrition, food security and livelihoods; water, sanitation, hygiene (WASH); and child protection. However, only the nutrition and CT components were funded and implemented at scale; other sectors were severely underfunded. The CT amounts were set by Save the Children as part of its CT programme and were estimated to meet 80 % of the energy requirements for an average-sized household. The CT was initially equivalent to about GBP32 per household per month, rising to about GBP43 in June when food prices increased.
Save the Children’s eligibility criteria for the CT programme depended on two factors: (i) households identified as ‘poor’ or ‘very poor’; and (ii) households with a child less than 5 years old. Some households were also included if considered vulnerable, for example female- or child-headed households.
Procedures and participants
The CT programme took place over six consecutive months. Enrolment and baseline data collection for the study started two weeks prior to the first cash distribution, in April 2012. The last data, a repeat of the baseline data, were collected a week before the final cash distribution in September 2012; thus the data cover five months of CT distributions. The Save the Children CT programme list for Aguié was used as the sampling frame to randomly select eligible households for the study (n 642); those with a child aged 6–36 months without obvious chronic or physical illness affecting anthropometric measurement and not classified as acutely malnourished (defined as weight-for-height Z-score (WHZ) ≥−2 compared with the WHO growth reference, or mid-upper arm circumference (MUAC) above 125 mm, and free of bilateral oedema). In the small number of cases where there were two or more children aged 6–36 months in the household, one child was randomly selected by the enumerators on the day of enrolment.
The Niger Ministry of Health granted approval for the study. Study participants gave written informed consent with the option to opt out at any time. Each mother was given an identification card with a photograph of the enrolled child for identification purposes in follow-up procedures. To allow collection of data on practices performed at home, as well as ensuring attrition remained low, all data collection was carried out at the homes of enrolled households.
The sample size for the current analysis includes 412 children from households with no missing data. A post hoc power estimation, based on the change in mean WHZ and taking into consideration correlation from repeated measures, was >90 %.
Any child who was identified as acutely malnourished (WHZ <−2 and/or MUAC <125 mm or with oedema) at baseline (n 184, 28·7 %) was not included in the study but referred to the nearest supplementary feeding centre.
All quantitative data were collected using a questionnaire which was administered to the mothers of enrolled children during both surveys. The guiding framework (Fig. 1) for our study was adapted from a model developed by Gaarder et al. ( Reference Gaarder, Glassman and Todd 5 ), which postulates that CT are mediated through twenty-six underlying community-, household- and individual-level variables which affect a number of necessary health behaviours, so influencing nutritional outcomes. The questionnaire was designed to capture each of these elements. Qualitative data, using a set of open questions mainly to provide information on programme delivery and uptake, were collected through taped key informant interviews with CT beneficiaries (seventeen mothers with an acutely malnourished child were matched geographically and by age and sex of the child to those with a non-acutely malnourished child) and focus group discussions with the three Save the Children programme field staff and the ten study team leaders.
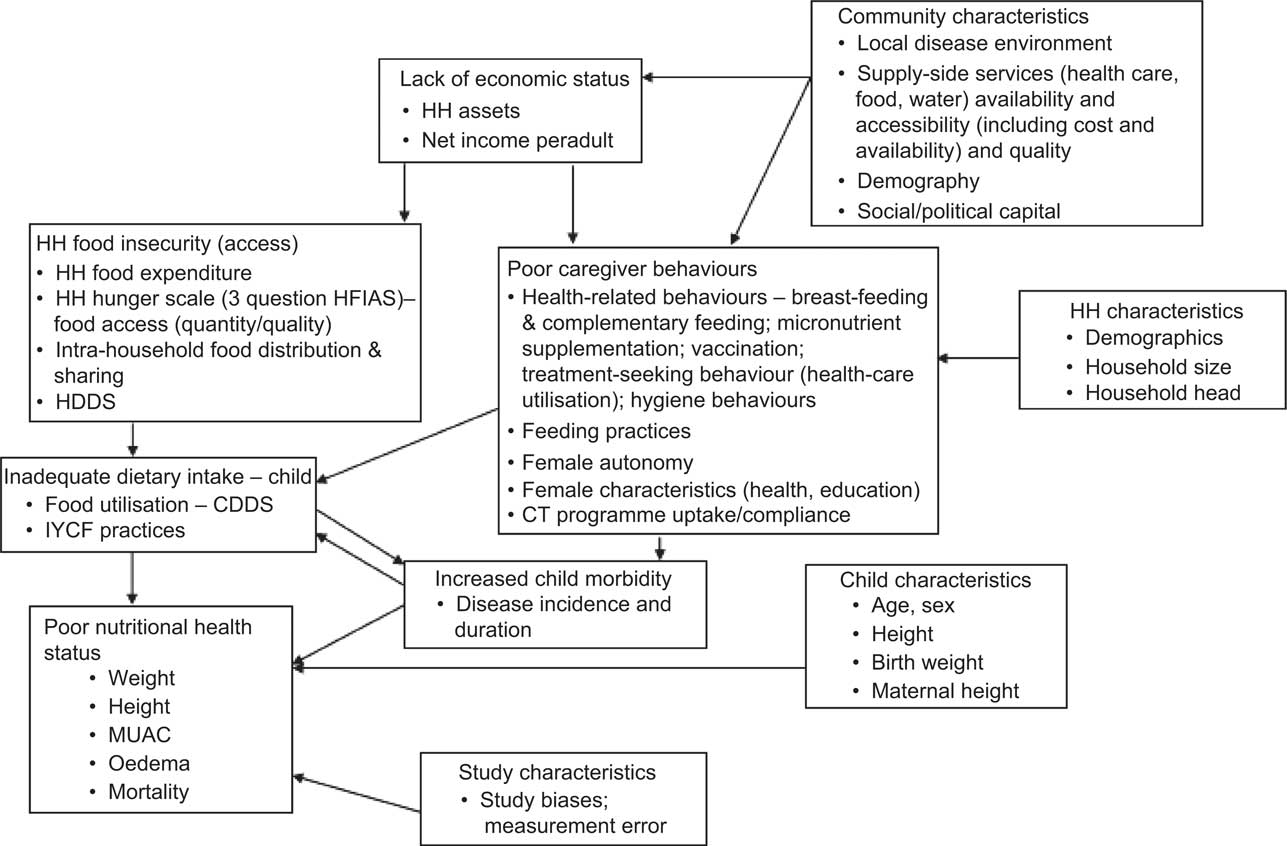
Fig. 1 Conceptual framework for understanding causal pathways for cash transfers (HH, household; HFIAS, Household Food Insecurity Access Scale; HDDS, household dietary diversity score; CDDS, child dietary diversity score; IYCF, infant and young child feeding; MUAC, mid-upper arm circumference; CT, cash transfer)
Composite variables were constructed by either summing or scoring data collected. A measure of food security was based on the shortened validated version of the Household Food Insecurity Access Scale (HFIAS)( Reference Coates, Swindale and Bilinsky 13 ). A household dietary diversity score was created by summing the number of food groups consumed in the past 24 h. A child dietary diversity score was adapted from Ruel and Menon( Reference Ruel and Menon 14 ) based on breast-feeding, meal frequency and number of food groups consumed each day, appropriate for each age group. A hygiene score was created by combining observations regarding cleanliness of the house, presence or not of animal faeces near the front of the house, presence or not of a hand-washing device in the house or compound, the type of vessel water was stored in (narrow necked, covered or not), and a score for access to safe water from a protected water source that took less than 30 min to collect. A depression score was calculated from the Self-Reporting Questionnaire (SRQ-19) to assess mental health symptom change( Reference Harding, Arango and Baltazar 15 , Reference Beusenberg and Orley 16 ).
Women’s autonomy was assessed through validated questions aimed at capturing whether or not she had sole, or joint (with husband), control to make decisions on five important issues: women’s own health, large and daily household purchases, family visits and daily meals. Social networking was assessed through membership to available groups within the community.
Enumerators were trained to make anthropometric measurements using standard techniques( Reference Habicht 17 ), applying SMART (Standardised Monitoring & Assessment of Relief & Transitions) guidelines( 18 ) and standardisation tests during training and refresher training, using the Emergency Nutrition Assessment (ENA) software( 19 ). Weight was recorded to a precision of 0·1 kg using an electronic baby/toddler scale (Tanita BD-590, USA); the length of children <87 cm was measured to a precision of 1mm using a baby mat (SECA S210, UK); and the height of children ≥87 cm was measured using a plastic stadiometer (Leicester, Child Growth Foundation, UK). A tape was used to measure MUAC on the left arm to a precision of 1mm. The presence of bilateral pitting oedema was recorded. Moyo weight-for-height charts( Reference Sikorski, Kerac and Fikremariam 20 ) were used to assess and interpret a child’s weight-for-height (according to WHO growth standards for girls and boys) in the home. Age was determined by asking to see a birth certificate or by asking the mother/carer directly; or, if not known, it was estimated using a local event calendar.
Child morbidity (diarrhoea (three watery stools per day), fever, cough or difficulty breathing, malaria) was assessed from mother’s knowledge of the child’s symptoms during the previous two weeks and verified if the child had been taken for treatment. Co-morbidity was defined as the presence of two or more of these symptoms/diseases.
Statistical analysis
Data were double entered into EpiInfo version 7( Reference Dean, Arner and Sunki 21 ) by two data-entry clerks on the day after data collection. Data were imported, merged and analysed in the STATA statistical software package version 12. Anthropometric indicators of the attained growth standards were calculated using the WHO macro for STATA( 22 ).
Baseline variables for household, mother and child were expressed either as medians (with interquartile range) for continuous variables or percentages for categorical variables. Two-sample Wilcoxon rank-sum (Mann–Whitney U) tests (medians) and z tests (categorical variables) were carried out to compare variables between survey rounds. To assess risk factors for acute malnutrition, a GEE (generalized estimating equations) approach( Reference Diggle, Liang and Zeger 23 ) was used to construct a multivariable logistic regression model, with a logit link and binomial distribution, to account for possible within-child correlation between repeated measures and adjusting for potential confounders. More detailed analyses of risk factors using data collected monthly will be reported elsewhere.
Results
Baseline characteristics for households, mothers and children are shown in Table 1. The sample of households was largely of Hausa ethnicity. The median household size was 7·0 with a median of 5·0 household members less than 18 years of age. Half the sample reported having access to safe water. The median reported time to walk to a health facility was 30 min (interquartile range: 10–60 min); 119 (28 %) households had to walk for an hour or longer. The median age of mothers was 30 years; two children had no mother so a primary carer was identified. Nearly 94 % of mothers in the study had no formal education.
Table 1 Household, mother and child characteristics at baseline (n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency among households with a non-acutely malnourished child aged 6–36 months, Aguié district, Maradi region, Niger, April–September 2012
IQR, interquartile range; WHZ, weight-for-height Z-score; HAZ, HAZ, height-for-age Z-score.
* Percentage yes with card or with mother’s knowledge.
† Over past 6 months.
‡ BCG (Bacillus Calmette–Guérin) vaccination against tuberculosis.
§ Two measurements were flagged (outside biological range of ±6) and so excluded from analysis.
¶ Stunting defined as HAZ <−2.
Girls and boys were equally represented in the sample with a combined median age of 22·2 months. Coverage of children immunised against tuberculosis (BCG vaccine), receiving vitamin A supplementation and vaccinated against measles met district targets (>80 %)( 24 ). The percentage of children who were stunted was very high (67·8 %).
Data on changes in reported expenditures (from recall) and income are shown in Table 2. Expenditures on food and non-food items and medical costs for adults between the baseline and final surveys, with recall periods of 3 months, a month and a week were all significantly higher (P<0·001). This increase was lower, but still significant, for medical expenditure on children during the previous week (P=0·001) and during the previous month (P=0·01). Medical expenditures on children are difficult to assess because the government provides free services for children under 5 years of age, although some families took their child to non-government health service providers, including drug peddlers, for treatment where costs were incurred. Reported incomes, recalled from the past month, were significantly higher (P=0·003); as was the number of people in waged employment (P<0·001; data not shown).
Table 2 Comparison of median (and interquartile range) expenditures and incomes between rounds (exclusive of those households without expenditures and incomes; n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency among households with a non-acutely malnourished child aged 6–36 months, Aguié district, Maradi region, Niger, April–September 2012
IQR, interquartile range.
* P value for two-sample Wilcoxon rank-sum (Mann–Whitney U) test.
† West African franc.
Baseline and final survey comparisons for household and child variables are shown in Table 3. According to the same Household Economy Approach classification at baseline, the number of households classified as ‘very poor’ decreased significantly over time (P=0·04); 7 % of households were identified as being in the top two wealth groups, compared with 1 % at baseline. There were significant differences (P<0·001) between survey rounds in the number of assets bought (higher) and sold (lower), especially among ‘very poor’ households. The percentage of households in financial debt (self-reported) was significantly lower in the final survey (P=0·01) as was the percentage of households with men migrating for work (P<0·001), reflecting increased incomes and employment with more men returning to the community.
Table 3 Comparison of baseline and final survey household and child variables (n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency among households with a non-acutely malnourished child aged 6–36 months, Aguié district, Maradi region, Niger, April–September 2012
HEA, Household Economy Approach; WHZ, weight-for-height Z-score; MUAC, mid-upper arm circumference.
* P value for paired z test for categorical variables.
† P value for two-sample Wilcoxon rank-sum (Mann–Whitney U) test for continuous variables.
‡ One of diarrhoea, malaria, respiratory infection or measles.
§ With two or more diseases occurring together.
|| Became acutely malnourished (WHZ <−2).
Social networking improved significantly over time: twice as many households reported joining a community group (P = 0·02) compared with baseline, although the percentage of households belonging to any group was still small (8·7 %). Women’s decision making declined significantly with an increasing number of men making decisions alone, especially on spending money on large household purchases (P<0·001), small daily household items (P=0·01) and on what was eaten each day (P=0·01).
While there was a significant improvement in mother’s self-reported mental health, women perceived that their physical health declined. Child morbidity reported during the previous two weeks, especially malaria incidence, was also significantly higher than at baseline, coinciding with the usual malaria transmission during the rainy season which started in July( 25 ).
There was an improvement in food security indicated by a significant average increase in dietary diversity for both households and children (P<0·001). The proportion of children who developed acute malnutrition post-intervention was 4·1 % (n 17); 1 % (n 4) were severely acutely malnourished (WHZ <−3). Ten children (2·4 %) had MUAC <12·5 cm; all of these children also had WHZ <−2. Anthropometric measurements (WHZ and MUAC) showed significant improvements (P<0·001) from baseline. Children who were acutely malnourished post-intervention showed a significant decline in both WHZ and MUAC (P<0·001) from baseline, as would be expected. Risk factors associated with acute malnutrition adjusted for age and sex (Table 4) were belonging to a very poor household at baseline (P=0·015), starting the lean season with WHZ <−1 but ≥−2 (P=0·015) and the presence of co-morbidity (P=0·021). The percentage of children with WHZ <−1 to ≥−2 was significantly lower in the final survey (30·0 % v. 45·8 % at baseline; P<0·001) with a higher percentage of children with WHZ>−1 (Fig. 2).
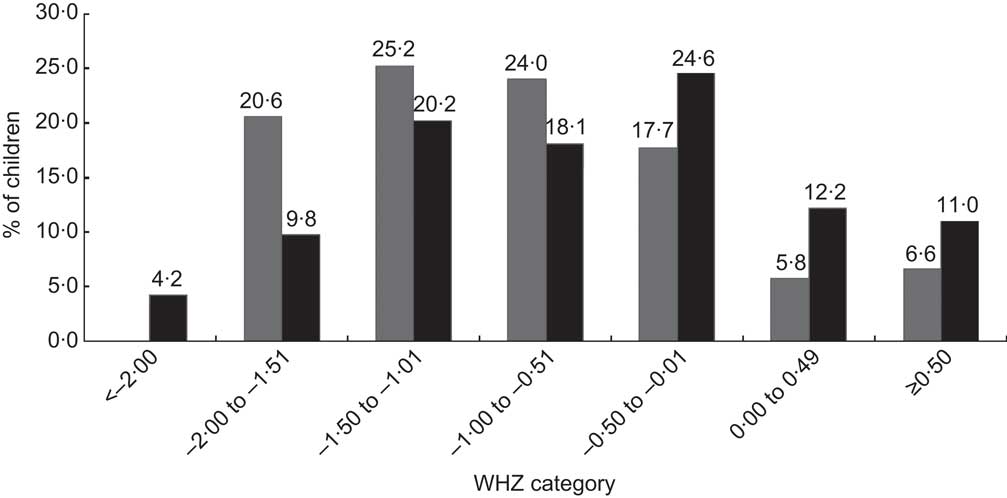
Fig. 2 Distribution of weight-for-height Z-score (WHZ) category over time (![]() , April 2012;
, April 2012; ![]() , September 2012) among non-acutely malnourished children aged 6–36 months (n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency in Aguié district, Maradi region, Niger
, September 2012) among non-acutely malnourished children aged 6–36 months (n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency in Aguié district, Maradi region, Niger
Table 4 Multivariable analysis of risk factors associated with acute malnutrition using generalised estimating equations (n 412) in a pre–post intervention observational study on the role of unconditional cash transfers during a nutritional emergency among households with a non-acutely malnourished child aged 6–36 months, Aguié district, Maradi region, Niger, April–September 2012
WHZ, weight-for-height Z-score; Ref., referent category.
* Log odds.
† z Statistic.
‡ Corresponding P value.
Qualitative data indicated that programme delivery was very good, with timely monthly payments made to every enrolled household as planned. Uptake of the programme was 100 % and satisfaction high. One of the most commonly stated reasons for this was that men were less likely to migrate for work and those who did, returned earlier than usual.
Discussion
The present study captured many of the moderating factors within the causal framework for undernutrition and the results are consistent with the direction of many of the pathways. The study shows that over five months of cash distribution, indicators of the living standards of ‘poor’ and ‘very poor’ households were raised; indicated by a reduction in indicators of poverty (improvement in household expenditures, incomes, employment, asset protection, wealth rank, access to social networks) and an improvement in indicators of household food security (household food security score, household and child dietary diversity). Furthermore, anthropometric measurements for children aged 6–36 months improved significantly, despite an increase in the incidence of child disease and decline in women’s well-being and autonomy. Children were more likely to be acutely malnourished if they started the lean season in a household classified as ‘very poor’, with low WHZ at baseline and/or experienced co-morbidity. The important findings from the study are consistent with the available evidence on the general impact of CT( Reference Manley, Gitter and Slavchevska 2 , Reference Leroy, Ruel and Verhofstadt 3 , Reference Gaarder, Glassman and Todd 5 , Reference Bailey and Hedlund 7 ) and as such suggest plausible improvements due to the CT.
There are a number of study limitations. Without a control group it is not possible to attribute the changes seen in the participants to the cash alone. Secular trends and seasonality may also explain some of the differences seen in the study findings. For example, the reduction in number of households reporting male members migrating for work may have been a result of normal seasonal changes( 26 ) or increased household income from the CT. Qualitative interviews with key informants and Save the Children field staff indicated that men had come back to the community earlier than expected because they heard about the CT programme. That there were more men within the community during the final survey may help explain why women’s autonomy declined significantly. It is common practice in this area for men to buy the staple foods from the markets and so, even though women were the targeted beneficiaries of the CT programme, the cash would be handed over to their husbands, who would then give a small amount back to the women to buy other mainly non-food items. This was consistent with information from qualitative interviews.
Improved access to food through increased incomes could help explain some of the improvements in food security and dietary diversity for both households and children. The main grain harvest usually starts in October( 25 ); thus improved access to food through increased availability would not be expected until the harvest, which was not covered by the present study.
The decline in perceived health status of women and increase in child morbidity are related to the rainy season, which coincides with the annual malaria epidemic( 9 , Reference Ehrhardt, Burchard and Mantel 27 ). It is difficult to say here by how much child anthropometric status would have improved had the incidence of disease also declined, but the strong association between nutritional status and disease indicates that reducing morbidity could have added benefits to child anthropometric status.
Finally, potential sources of bias, especially regarding collection of expenditure data, need consideration. Important here are both recall and social desirability bias in which respondents tend to give answers that will be viewed favourably by others( Reference Paulhus 28 ). Recall of expenditures on food, non-food and medicines may be different. For example, it is difficult to separate out expenditure on a child’s food if that food is part of the household food as opposed to expenditure on non-food items and medicines specifically for the child.
Conclusions
The results from the present study are consistent with the available evidence from impact evaluations of CT programmes and plausibly show that giving cash during an emergency can help safeguard living standards of the very poor and poor in this population.
The results also show that the nutritional status of children aged 6–36 months who remained non-acutely malnourished improved, although without a control group it is difficult to say with certainty whether this was due to the CT programme and/or seasonal or secular trends. Interestingly, those children who fared worse were already worse off at baseline and this information provides important evidence as to the potential barriers to preventing acute malnutrition. To make a probability statement would require formal testing using controlled experimental or quasi-experimental methods, with a focus on areas that did not improve during the study and that are often associated with child nutrition status, such as child health; as well as investigating the effect of earlier transfers of cash to prevent low WHZ and to increase resilience of households prior to the lean season.
Acknowledgements
Acknowledgements: The authors acknowledge the CT study field staff and Save the Children staff in the Tessaoua and Niamey offices for their support in the implementation of the CT study, especially Cyrille Niameogo (Country Director, Save the Children Niger), Nadine Thea Beurey (Head of Operations, Save the Children Niger), Akebou Sawadogo (Tessaoua Area Manager, Save the Children Niger), Ibrahima Issa (Maradi FSL Coordinator, Save the Children Niger), Abdou Malam Dodo (FSL Coordinator, Save the Children Niger), Ashley Hughes (M&E Adviser, Save the Children Niger) and Jessica Saulle (Humanitarian FSL Adviser, Save the Children UK), among many others. They also thank the Ministry of Health in Niger, in particular Doctor Maimouna Guero for her support. Additional thanks go to Assaye Tolla for cleaning the data, Sarah Styles for contributing to the training of enumerators and data-entry staff, and Jessica Bliss for transcribing duties. The contributions of many other individuals who supported the implementation and evaluation of the CT study are also gratefully acknowledged, especially the participating members of the CT communities. Their patience and cooperation is so gratefully appreciated. Finally, the authors acknowledge Dr Andrew Hall from Save the Children UK for his useful comments on an earlier draft of this manuscript; and would also like to thank the reviewers for their helpful comments. Financial support: The CT study was implemented through the Emergency Nutrition Network and funded by the Office of US Foreign Disaster Assistance (OFDA). OFDA had no role in the design, analysis or writing of this article. The CT programme was a Save the Children programme in Maradi region, Niger, with funding from the Ministry of Foreign Affairs (Norway); the Department for International Development (DFID) UK; and Save the Children Australia, Norway, UK and Italy. Conflict of interest: None. Authorship: B.F. was principal investigator for the study and designed the final protocol, supervised the research facilitator, analysed the data, and drafted and finalised the manuscript. G.N. was the study research facilitator, trained and supervised enumerators and survey staff, was responsible for data collection and data entry, and edited the manuscript. V.S. contributed to study design, facilitated study implementation and contributed to the data interpretation, as well as providing comments on all drafts of the manuscript. C.D. and J.S. proposed the idea for the study, contributed to study design, facilitated study implementation and contributed to the data interpretation, as well as providing comments on all drafts of the manuscript. Ethics of human subject participation: The Niger Ministry of Health granted approval for this study. Study participants gave written informed consent with the option to opt out at any time.








