Food insecurity refers to the lack of constant access to sufficient, safe and nutritious food for an active and healthy life(1). This definition is based upon four fundamental preconditions of food security: (1) availability of sufficient amount of nutritionally adequate food, (2) physical and financial access to sufficient amount of nutritionally adequate food, (3) resources and capacity for appropriate utilisation of food and (4) stability of all of the above over time(2). A deficit in any single or a combination of these preconditions can result in food insecurity.
The negative consequences of food insecurity are well established and highlight the importance of this issue from a public health point of view. In high-income countries, food insecurity is linked to a number of adverse nutrition and health outcomes, including low consumption of fruit and vegetables, increased consumption of inexpensive energy-dense, nutrient-poor foods, a cyclic compromise of food quantity when access to food is hindered, and overcompensatory eating patterns when access is restored(Reference Laraia3). In such countries, food insecurity among adults is consistently associated with health conditions such as overweight/obesity(Reference Pan, Sherry and Njai4), particularly among women(Reference Townsend, Peerson and Love5–Reference Moradi, Mirzababaei and Dadfarma7); chronic disease, particularly type 2 diabetes and CVD(Reference Seligman, Bindman and Vittinghoff8,Reference Redmond, Dong and Goetz9) ; poor management of diabetes(Reference Seligman, Davis and Schillinger10); poor self-reported general health(Reference Stuff, Casey and Szeto11,Reference Gundersen and Ziliak12) ; and higher levels of stress and poorer mental health outcomes(Reference Leung, Epel and Willett13,Reference Martin, Maddocks and Chen14) . Some of these consequences arise independently of poverty(Reference Burns15), a known contributor to poor health outcomes; so a study on food insecurity can contribute new information to our understanding of the social determinants of health.
Food insecurity can be measured at the individual, household or population levels and at different levels of severity(Reference Barrett16). In the USA, an eighteen-item questionnaire (US Household Food Security Scale) classifies respondents/households into food-secure, marginally food-secure (or food-insecure with low severity of food insecurity), food-insecure (without hunger) and severely food-insecure (with hunger)(Reference Lee, Gundersen and Cook17). This is the most widely used tool and the gold standard for measuring food insecurity across high-income countries. In Australia, food insecurity is measured using a single question that asks if in the last 12 months any member of the household had run out of food and could not afford to buy more(18). This question assesses one aspect of food insecurity – that of financial access to food – and does not account for the quality of foods consumed or the severity of food insecurity.
Food insecurity is a growing concern in many high-income countries(Reference Coleman-Jensen, Rabbitt and Gregory19–Reference Loopstra, Reeves and Stuckler21). In the USA, food insecurity has been rising continuously since 2001, reaching a high of 14·9 % in 2011 and declining only slightly thereafter(Reference Coleman-Jensen, Rabbitt and Gregory19). In Canada, the rates of insecurity increased from 11·3 % in 2007–2008 to 12·4 % in 2011–2012 and remained at the same levels until 2014(Reference Tarasuk, Mitchell and Dachner20). In Europe, a trend of rising household food insecurity has been observed since 2010 with a rise from 8·7 % in 2009 to 10·9 % in 2012 and elevated rates thereafter(Reference Loopstra, Reeves and Stuckler21).
In Australia, estimates of food insecurity range from 2 % in older Australians to up to 76 % in at-risk groups(Reference McKay, Haines and Dunn22) such as refugees (71 %)(Reference Gallegos, Ellies and Wright23) or remote Aboriginal communities (76 %)(Reference Ferguson, Brown and Georga24). Estimates from representative national samples, such as the National Nutrition Survey in 1995/1996, show prevalence rates of 5·2 % in adults aged ≥19 years and up to 10 % in younger people aged 16–24(25). The most recent national estimates from the 2011/2012 Australian Health Survey indicate that 3·5 % of adults aged ≥19 years and 5·9 % of those aged 2–18 experience food insecurity(26).
The New South Wales (NSW) Population Health Survey (PHS) collects food insecurity data using the single-question indicator. In NSW, data on food insecurity were being collected routinely from 2002 to 2014 (except 2011 and 2013). However, the food insecurity question was removed from the survey after 2014. As a result, there are no food insecurity state data from 2015 onwards. At a national level, food insecurity was last measured in the 2011/2012 National Health Survey, while the latest National Health Survey in 2015/2016 did not assess food insecurity. The above indicates a current gap in the monitoring of this important issue.
Few studies in Australia have assessed food insecurity, and most have used the single-item question(Reference McKay, Haines and Dunn22), which means that data on food insecurity, in particular population data, are likely to underestimate the true magnitude of the problem. More in-depth studies using more sensitive, multidimensional measurement tools report higher food insecurity rates compared to those reported by national and state population surveys(Reference Nolan, Williams and Rikard-Bell27–Reference Butcher, O’Sullivan and Ryan30). In addition, recent reports from FoodBank Australia, a charity providing emergency food relief, raise further concern about the size and potential consequences of the problem(31).
Assessing food insecurity at a population level and understanding its association with different sociodemographic factors is an important step in appraising the magnitude of the problem and designing appropriate responses, both in terms of surveillance and intervention. This study aims to present a summary of existing data from 2002 to 2014 in order to evaluate the prevalence and sociodemographic factors associated with food insecurity in NSW. The study will explore the relationship of food insecurity with key sociodemographic variables over a 12-year period using a series of large population samples in order to provide an overview of the issue and a baseline for future studies.
Methods
New South Wales Population Health Survey
The NSW PHS collects self-reported data through computer-assisted telephone interviewing. Participants are selected from the general population using random digit dialling. Included in the sample are people with a landline, or landline and mobile number (since 2010), or mobile only (since 2012). Interviews are conducted between February and December each year. The survey sample is weighted to adjust for differences in the probability of selection among household members. Post-stratification weights are used to reduce the effect of differing non-response rates among males and females and different age groups on the survey estimates. These weights are adjusted for differences between the age and sex structure of the survey sample and the NSW population(32).
Food insecurity/outcome
The question used to measure food insecurity was: ‘In the last 12 months, were there any times you ran out of food and could not afford to buy more?’ This was coded as a dichotomous variable (no/yes) classifying respondents as food-secure or food-insecure.
Sociodemographic covariates
Age, sex, marital status, country of birth, education, employment status, household income, smoking status, alcohol intake, self-rated health, household size, socioeconomic disadvantage and remoteness were the sociodemographic covariates examined. Two different age variables were used: (1) age <20 years, (2) age ≥20 years. The association of both these variables with food insecurity was analysed. Marital status was defined as a categorical variable with five levels: married (this refers to registered marriages); divorced; never married; separated but not divorced; widowed. Country of birth was defined as a dichotomous variable with two levels: born in Australia/not born in Australia. Education was defined as a categorical variable with five levels: less than high school; high school; TAFE certificate or diploma; tertiary or higher; other. Employment status was defined as a categorical variable with two levels: a salary- or wage-earner or conducting a business; and unpaid work or did not have a job. Household income per year was defined as a categorical variable with six levels: <$20 000; $20 000–$40 000; $40 000–$60 000; $60 000–$80 000; >$80 000; don’t know. Smoking status was defined as a categorical variable with five levels: I smoke daily; I smoke occasionally; I don’t smoke now, but I used to; I’ve tried a few times but never smoked regularly; I’ve never smoked. Alcohol intake was defined as a categorical variable with three levels: I don’t drink; I drink less than once per week; I drink weekly or more. Household size was expressed as number of people in the household and was defined as six discrete categories for households with 1–6 people, and a seventh category for households with ≥7 people. Socioeconomic disadvantage was described based on the Index of Relative Socio-Economic Disadvantage (IRSD)(33). Participants were grouped into five quintiles of socioeconomic disadvantage, from least (first quintile) to most disadvantaged (fifth quintile), based on the IRSD score of their area of residence. Remoteness was based on the Accessibility/Remoteness Index of Australia Plus (ARIA plus), which classifies areas into major cities; inner regional; outer regional; remote; very remote(34). In this analysis, regional and remote categories were amalgamated into one category so that remoteness was coded as a dichotomous variable with two levels: major cities v. remote/regional.
Analysis
Data from 2003 to 2014 were aggregated forming a sample of 212 608 respondents. Survey year 2002 was excluded due to missing country-of-birth data on that year. After excluding observations with age <16 years and survey years 2011 and 2013 where food insecurity data were not collected, the sample dropped to 150 767 observations. Observations with missing values for any covariate or the food insecurity question were also excluded resulting in an active sample of 80 433 observations for analyses. Univariate and multivariate logistic regression analyses were undertaken to test the association between food insecurity and a range of sociodemographic covariates. Multivariate logistic regression models were used to investigate the effect of time on the association between food insecurity and the sociodemographic covariates; interactions between each covariate and time period were tested. Time was defined as a categorical variable with three levels, 2003–2005, 2006–2009 and 2010–2014, noting that data for the years 2011 and 2013 were not available. A sensitivity analysis comparing univariate models with complete observations (n 80 433) against models using all observations, including those with missing data (n 150 767), was conducted to assess the risk of bias. Data were analysed using the R statistical software package (version 3.5.1) in RStudio (version 1.1.463)(Reference Bates, Chambers and Dalgaard35).
Results
Between 2003 and 2014, on average 6 % (95 % CI 5·8, 6·3) of adults aged ≥16 years experienced food insecurity in NSW at least once over a recall period of 12 months (Fig. 1). The prevalence of food insecurity ranged from 5·1 % in 2007 to 7·2 % in 2012. Univariate regression analysis showed evidence of an association between food insecurity and survey year (OR 1·02, P = 0·013). After adjustment, the multivariate analysis showed that for one unit increase in survey year (i.e. from survey year 2003 to 2004), the odds of experiencing food insecurity were increased by a factor of 1·05.
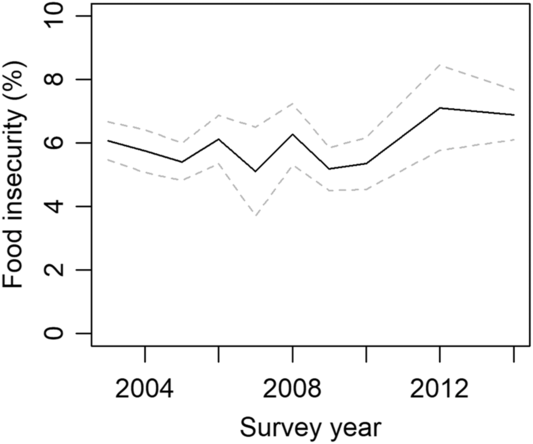
Fig. 1 Prevalence of food insecurity (%) by survey year, 2003–2014. The dotted line above and below shows the 95 % confidence limits for food insecurity prevalence estimates
The prevalence of food insecurity was higher among those who did not attend high school (7·4 %), did not have a job (8 %), were most disadvantaged (8·4 %), earned <$20 000 per year (12·5 %), were separated but not divorced (14·1 %), lived in households of ≥7 people (13·5 %), smoked daily (15·4 %) and rated their health as very poor (18 %). Also, more women experienced food insecurity compared with men (6·6 v. 5·4 %), more people living in remote areas compared with major city dwellers (6·7 v. 5·8 %) and more Australian v. overseas-born people (6·3 v. 5·4 %) (Table 1).
Table 1 Sociodemographic characteristics of survey sample* 2003–2014 by percentage of food insecurity
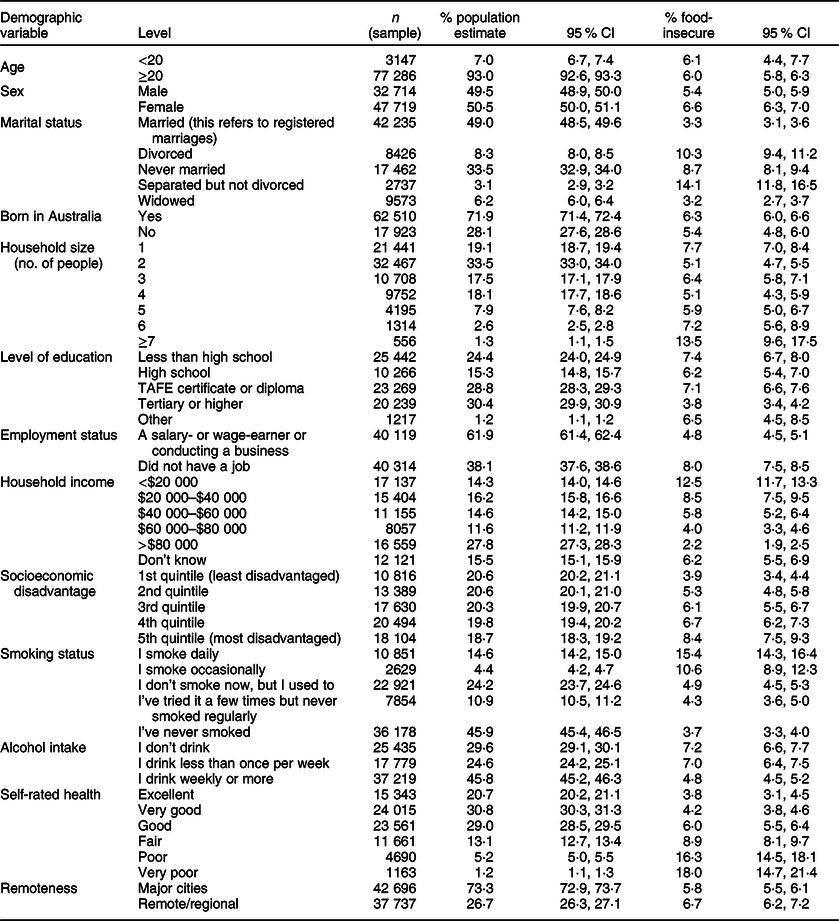
* Missing values (%): food insecurity (8·8), socioeconomic disadvantage (0·2), born in Australia (8·5), level of education (18·0), employment status (17·2), income (7·9), self-rated health (5·5), sex (<0·1), smoking status (21·8), people in household (1·2), marital status (0·4), locality (0·2), alcohol use (22·1).
In the univariate models, a significant association was observed between food insecurity and all sociodemographic variables included in the analysis (Table 2). In the multivariate model, no significant association was found with country of birth (P = 0·3), socioeconomic disadvantage (most disadvantaged compared with least disadvantaged; P = 0·6) or remoteness (P = 0·9). The associations with age, sex, marital status, household size, education, employment status, household income, smoking status, alcohol intake and self-rated health remained significant in the multivariate model (Table 2).
Table 2 Univariate and multivariate logistic regression analyses of food insecurity by sociodemographic variables
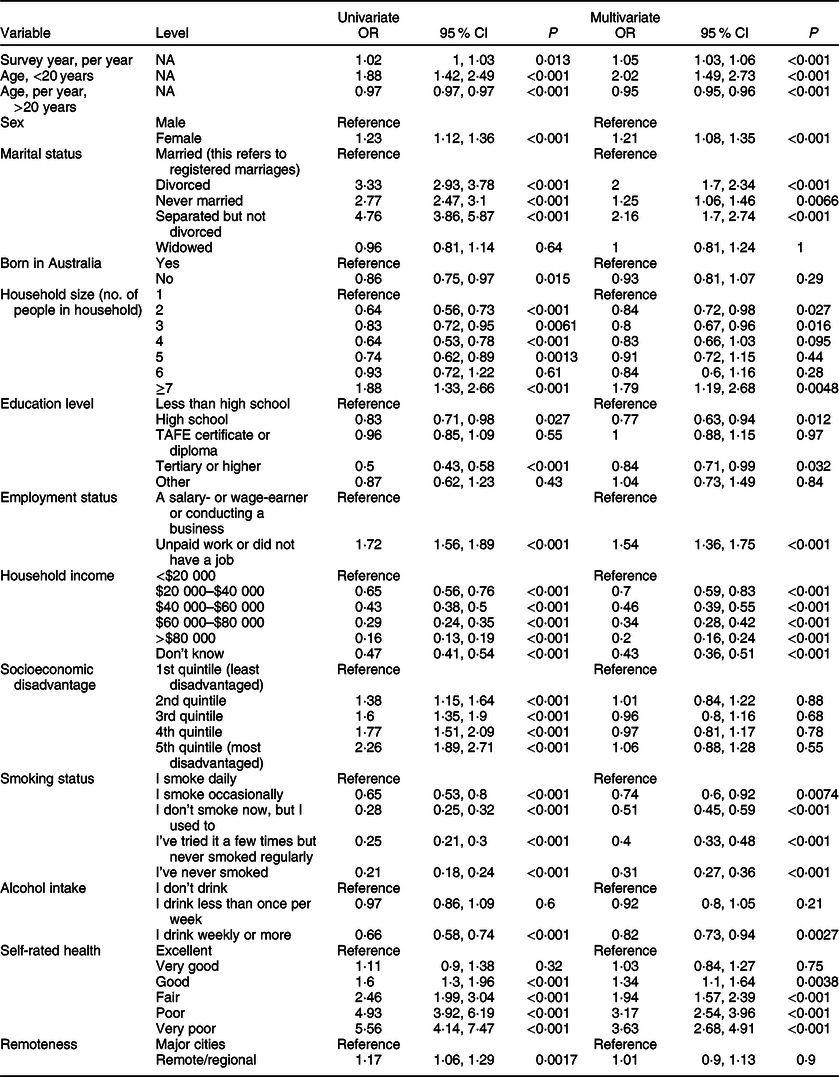
After adjusting for all other variables in the model, those who attended high school had 0·77 times the odds of experiencing food insecurity (P = 0·01) compared with those who did not attend high school, and those who did not have a job, had 1·54 times the odds of being food-insecure compared with those on a salary (P < 0·001). The association between food insecurity and income was highly significant (P < 0·001) across all income levels compared with the reference group of those earning <$20 000 per year. This association followed a gradient, with the odds of food insecurity increasing as income decreased. Those in the highest income group (>$80 000) had one-fifth the odds of food insecurity (OR 0·2) compared with those in the lowest income group, and these odds increased in a stepwise fashion as income decreased from highest to lowest. The association with smoking and self-rated health also showed a gradient. As smoking increased from ‘never smoked’ to ‘smoking daily’ and as self-rated health changed from ‘excellent’ to ‘very poor’, so did the odds of food insecurity. Those with a very poor self-rated health had almost four times the odds of food insecurity compared with those who rated their health as excellent (OR 3·63), and those who smoked daily had more than three times the odds of food insecurity compared with those who had never smoked (OR 3·23). Drinking weekly or more was associated with lower risk of food insecurity compared with not drinking (OR 0·82). The association of food insecurity with number of people in the household went in two directions: compared with single-member households, those in households of two or three members had lower odds of food insecurity (OR 0·84 and 0·8, respectively), whereas those in households of ≥7 members had much higher odds of food insecurity (OR 1·79). Marital status remained significantly associated with food insecurity in the multivariate model: people who were divorced or separated had about twice the odds of food insecurity (OR 2 and 2·16, respectively) compared with married people. People who never married were at an increased risk of food insecurity compared with married people (OR 1·25), but less so compared with people who were divorced or separated. Women were also at an increased risk of food insecurity compared with men (OR 1·24).
Plotted against age, food insecurity appeared to increase from the age of 16 up to 19 years and then to decrease from the age of 20 onwards (Fig. 2). In the multivariate model, two different age variables were included: age <20 and age ≥20 years. Both appeared significantly associated with food insecurity. For every year increase in age from the age of 16–19, the odds of food insecurity increased by a factor of 2·02 (P < 0·001), whereas for every year increase after the age of 19, the odds of food insecurity decreased by a factor of 0·95 (P < 0·001).
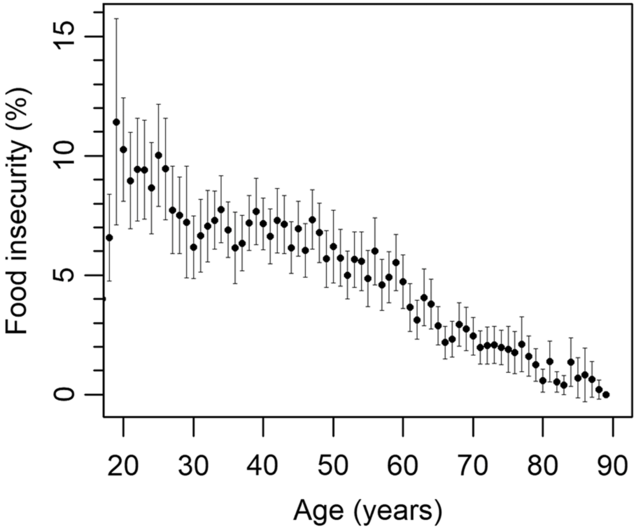
Fig. 2 Food insecurity by age in years with 95 % CI
Multivariate analyses of the associations over time found no significant interaction between the covariates and time period except in the case of remoteness, household income and self-rated health as shown in Fig. 3(a–c). There was strong evidence that the effect of income (P < 0·001) was modified by time (Fig. 3(a)). The odds of food insecurity decreased as income increased, and this association was consistent across the three time periods; however, the gradient in the association was attenuated in recent years whereby the difference in the odds of food insecurity between those who earned <$20 000 per year and those who earned $20 000–40 000 was no longer evident. There was some evidence that the effect of self-rated health was also modified by time, although statistical significance was borderline (P = 0·05) (Fig. 3(b)). While there was a clear ‘dose–response’ relationship with the odds of food insecurity increasing as self-rated health deteriorated in early years, in later years the odds of food insecurity in those with good and excellent health appeared to be similar. However, the elevated odds of food insecurity of those with very poor self-rated health relative to those with excellent health remained similar to previous years. There was strong evidence that the effect of remoteness (P = 0·003) varied by time period (Fig. 3(c)), after adjusting for other covariates. While the odds of food insecurity in remote/regional areas were lower compared with major cities in 2006–2009, this association was reversed in 2010–2014 whereby those who lived in remote/regional areas were more at risk of food insecurity compared with those living in major cities. The interaction of all other covariates with time was non-significant after adjustment.
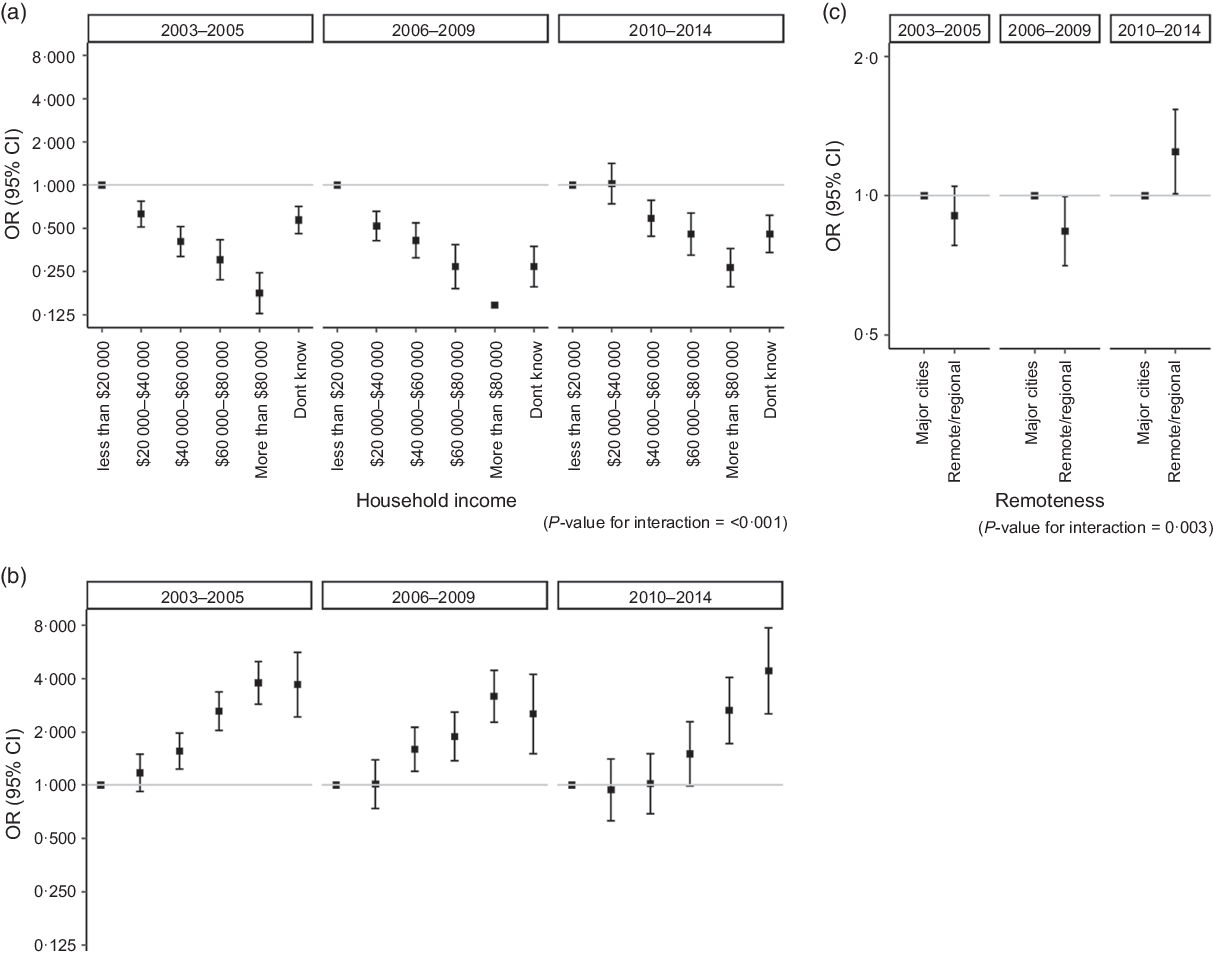
Fig. 3 Association of food insecurity with (a) household income, (b) self-rated health and (c) remoteness, stratified by time period
Discussion
This analysis of NSW PHS is the first to show prevalence rates of food insecurity over 12 years and how they are associated with sociodemographic factors. The average prevalence of food insecurity between 2003 and 2014 was 6 % and increased by 41 % between 2009 and 2012, but overall rates fluctuated (Fig. 1). A slight upwards trend was observed showing that the odds of food insecurity increased by a factor of 1·05 from one survey year to the next (P < 0·001). Food insecurity prevalence was higher at younger ages, with young adults aged 16–19 years being particularly at risk. In addition, food insecurity was independently associated with sex, marital status, household size, education, employment status, household income, smoking status, alcohol intake and self-rated health, with most of these associations appearing to be highly significant (P < 0·001).
Increased food insecurity among young adults has been demonstrated in other Australian studies(Reference Howse, Hankey and Allman-Farinelli36), some of which have focused on particular at-risk groups such as university students(Reference Hughes, Serebryanikova and Donaldson37) and youth accessing homelessness support services(Reference Crawford, Yamazaki and Franke38). Nutritional vulnerability in young adulthood, a period characterised by transition, has been linked to a range of factors including lack of time, facilities, knowledge and motivation to plan, shop, prepare and cook healthy food(Reference Munt, Partridge and Allman-Farinelli39).
The association with income was the strongest among all covariates: households with an income <$20 000 per year had five times the odds of food insecurity compared with those with an income >$80 000 per year. This association followed a gradient with decreasing odds of food insecurity as income increased along the income scale. This gradient was retained in the multivariate model with only minor reductions in the adjusted OR, thus confirming existing evidence on the role of income as a major predictor of food insecurity(Reference Furness, Simon and Wold40–Reference Stuff, Horton and Bogle42). This suggests that the use of a tool to measure financial access to food is imperative.
Our results also support previous evidence on the role of smoking as an independent risk factor for food insecurity(Reference Cutler-Triggs, Fryer and Miyoshi43). There was strong evidence of an association between smoking status and food insecurity in the univariate model. Daily smokers had almost five times the odds of food insecurity compared with those who never smoked (OR 0·21, 95 % CI 0·18, 0·24, P < 0·001). After adjusting for all other factors, daily smokers appeared to have 3·2 times the odds of food insecurity compared with people who never smoked. A graded decrease in the odds of food insecurity was noted as smoking levels decreased. The presence of a dose–response relationship points to a potential direction of effect going from smoking to food insecurity; however, it is not possible to draw reliable conclusions in the absence of longitudinal data. Other studies have found that the association between smoking and food insecurity is potentially bidirectional, with smoking leading to food insecurity on one hand, but food distress also leading to smoking on the other hand(Reference Kim, Flentje and Tsoh44,Reference Hosler and Michaels45) .
Possible mechanisms of the effect of smoking on food security status have been suggested previously(Reference Cutler-Triggs, Fryer and Miyoshi43). One such mechanism is the economic burden of smoking, which is much greater for low-income households. In these households, the cost of cigarettes can represent a significant proportion of their disposable income and can negatively influence spending on healthy food(Reference Cutler-Triggs, Fryer and Miyoshi43). It is likely that the cost of cigarettes imposes financial restrictions on people’s ability to purchase food, but more in-depth data would be needed to verify this hypothesis. Another possible explanation is based on behavioural differences in terms of dietary habits and attitudes towards healthy eating between smokers and non-smokers(Reference Cutler-Triggs, Fryer and Miyoshi43). Given that our study solely assesses financial access to food and does not account for the quality of foods consumed or specific dietary patterns associated with food insecurity, it is not possible to ascertain if the association between smoking and food insecurity is due to such behavioural factors.
The association of alcohol intake with food insecurity went the opposite direction compared with that of smoking. Those who drank weekly appeared to be at a lower risk of food insecurity relative to those who did not drink. This is consistent with the literature which suggests that alcohol use alone is associated with higher socioeconomic status, whereas risky alcohol consumption is linked to lower socioeconomic status(Reference Huckle, You and Casswell46,Reference Bonevski, Regan and Paul47) . It is likely that in our data set, drinking weekly or more was correlated with higher income, explaining the reduced odds of food insecurity in this group. Given the absence of data on excessive alcohol consumption, it was not possible to assess the relationship of risky alcohol use with food insecurity.
Food insecurity was strongly associated with very poor self-rated health (OR 3·63, P < 0·001). The relationship between self-rated health and food insecurity is complex and potentially bidirectional(Reference Temple48). Food insecurity is a contributor to poor health outcomes such as obesity and chronic disease, but according to studies on cancer and HIV-affected populations, disease may also contribute to higher rates of food insecurity, only partially explained by other sociodemographic correlates(Reference Gany, Lee and Ramirez49,Reference Anema, Weiser and Fernandes50) . Given the cross-sectional nature of our study, it was not possible to ascertain the direction of effect in this association.
Women were at more risk of food insecurity compared with men (OR 1·24). This is consistent with previous studies in Canada, USA and New Zealand(Reference Tarasuk51–Reference Carter, Lanumata and Kruse53). Several explanations have been given for this difference. One explanation is based on the different gender roles, with women being more often charged with the responsibility of feeding the family(Reference Martin and Lippert54). According to a previous study, women are more likely to sacrifice their food to feed other members of the family and, therefore, more likely to report food insecurity(Reference McIntyre, Glanville and Raine55). They are also more likely to be sole parents, and sole parenthood has been shown to be associated with food insecurity(Reference Nord, Andrews and Carlson52,Reference Carter, Lanumata and Kruse53) .
In the adjusted model, there was no evidence of an association between food insecurity and country of birth, remoteness (i.e. regional/remote areas v. major cities) or socioeconomic disadvantage. This is inconsistent with previous population surveys in NSW and South Australia that found an association with remoteness and socioeconomic disadvantage(Reference Foley, Ward and Carter56,Reference Innes-Hughes57) . It is possible that in our study, disadvantage is mainly driven by household income and educational level, both of which were significant in the multivariate model. Given that our study examines food insecurity over 12 years, there is less risk of random sampling bias in our study compared with studies using data from 2 or 3 years.
The associations between our covariates and food insecurity appeared to be fairly consistent over the study period. Time did not have a significant effect on these associations except a minor effect on income and self-rated health, where the gradient in the association with food insecurity was less evident in some years. The most important interaction with time was in the case of remoteness where the odds of food insecurity changed from being lower in remote areas compared with major cities in the first time period, to being slightly higher over the following years.
A strength of this study is the use of large population samples and multiple measurement points over a long period of time. However, there are some limitations. The data are cross-sectional, which precludes inferences about the direction of effect and causality between the sociodemographic variables and food insecurity. For some of the covariates in our models, there was missing data, which impacted the sample size for analyses, potentially affecting our estimates. However, we conducted a sensitivity analysis comparing univariate models with complete observations (n 80 433) against models using all observations, including those with missing data (n 150 767), to assess the risk of bias (online Supplementary Table 1). This showed only very small differences in the OR. Where larger differences were observed (change in OR >10 %), this did not appear to change the overall results in terms of which variables were found to be associated with food insecurity or the presence of a gradient effect. It should also be noted that given all variables from the univariate analysis were included in the multivariate model, potential bias from missing data in the univariate model would have limited impact on the results. From 2002 to 2012, NSW PHS had response rates ranging from 59·4 to 68·8 %, defined as the number of completed interviews over the sum of completed interviews, partial interviews and refusals(Reference Barr58). Although high rates of non-response could be a source of bias, the sample was weighted to adjust for differences in the probabilities of selection among respondents, and post-stratified to the Australian Bureau of Statistics’ latest mid-year population estimates to reduce the effect of differing non-response rates by gender and age group on the survey estimates(Reference Barr58).
The biggest limitation of this study is the use of a single-item measurement tool that likely underestimates the prevalence of food insecurity(Reference McKechnie, Turrell and Giskes29). The gold standard for measuring food insecurity across high-income countries is the US Department of Agriculture Food Security Survey Module (USDA-FSSM), an eighteen-item tool that could reliably assess food insecurity(Reference Coleman-Jensen, Rabbitt and Gregory19,Reference Marques, Reichenheim and de Moraes59) . Different studies have compared USDA-FSSM against the single-item tool used in Australian surveys and have found significant differences in the estimates of food insecurity. In a survey of 2334 Australian participants using the short form of the multi-item US Household Food Security Survey Module (HFSSM), Butcher et al.(Reference Butcher, O’Sullivan and Ryan30) found that 36 % of the study population experienced some form of food insecurity, and the prevalence of ‘low’ and ‘very low’ food security was 20 and 16 %, respectively. These estimates are significantly higher than national Australian estimates of 4–6 %. Another study comparing the single-item tool to a sixteen-item food security scale found that the single-item tool underestimated food insecurity by 6 %(Reference Nolan, Williams and Rikard-Bell27).
The limitations in our measurement tool did not affect the observed trend, that is, increase or decrease in the prevalence of food insecurity over time. Any measurement error in the prevalence of food insecurity would be consistent across the study period. Rates of food insecurity prevalence appeared to fluctuate over the study period, and findings showed a minimal consistent increase between 2003 and 2014. It was not likely that national or regional economic conditions had a bearing on the results. Overall, the Australian annual GDP growth has ranged between 1 and 4 % since 2000(60). This is in line with similar developed nations. As the NSW economy is service- and knowledge-focused, there has not been substantial changes to the social or economic policies since 2000, and overall government spending did not change over this time period(60). Furthermore, the NSW economy experienced almost two decades of uninterrupted economic growth despite the global financial crisis(60). This suggests that the observed rates of food insecurity could potentially increase substantially under weaker economic conditions.
Food insecurity is a growing public health concern in many developed countries and Australia. Understanding its impact on different sociodemographic groups is important to design appropriate interventions. The findings of the present study provide support for interventions targeting high-risk groups such as low-income, young and unemployed people. Income remains the strongest predictor of food insecurity among all sociodemographic covariates; however, the prevalence of food insecurity within low-income groups varies, suggesting that factors other than income also play a role(Reference Burns15). An American study has found that financial and food management skills – for example, ability to make a budget – reduced the likelihood of food insecurity, and this association persisted in a subgroup analysis of households with very low incomes(Reference Gundersen and Garasky61). Interventions targeting low-income groups should include income supplementation policies and changes to the Australian welfare system(Reference McKay and Lindberg62), but they should also address the additional barriers that prevent certain low-income groups from being more food-secure.
It is important to note that data on food security are no longer being collected in NSW PHS. The lack of food insecurity data post-2011 nationally and post-2014 in NSW precludes an accurate appraisal of the magnitude and current impact of food insecurity. Further, the single-item tool used in national population surveys and NSW PHS does not account for important aspects of food insecurity, such as the nutritious value of foods consumed, the frequency and severity of food insecurity. Abbreviated versions of more sensitive tools capturing multiple dimensions of food insecurity could be considered to maintain the advantages of large-scale population studies in terms of generalisability while improving the internal validity of these studies.
Given that the prevalence of food insecurity seems to be rising over time and taking into account the negative health consequences of food insecurity, we strongly recommend that the rates of food insecurity continue to be monitored in NSW and nationally using valid comprehensive tools.
Acknowledgements
Acknowledgements: The authors would like to acknowledge the NSW Ministry of Health for access to data. Financial support: NSW Ministry of Health (access to data). Conflict of interest: None. Authorship: S.M. and B.D. designed the research project; B.D. and L.S. performed statistical analyses; P.D. wrote the primary draft of the article with feedback and modifications from all; P.D. has the primary responsibility for the final content. All authors have read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and in accordance with the Australian National Health and Medical Research Council National Statement on Ethical Conduct in Human Research 2007. This is a secondary analysis of de-identified survey data.
Supplementary material
For supplementary material accompanying this article visit https://doi.org/10.1017/S1368980019005159







