CVD affects 3·5 million (17 %) Australians( 1 ) and is a leading cause of death (34 % of all deaths in 2008)( 2 ). The major risk factors contributing to the burden of CVD in Australia include high blood pressure (42 %), high cholesterol (35 %), physical inactivity (24 %)( Reference Begg, Vos and Barker 3 ) and overweight and obesity (21·3 %)( 1 ). It is estimated that 90 % of Australians have at least one modifiable risk factor for CVD( 4 ). This demonstrates the need for effective models of preventive health care that target elevated blood pressure, high cholesterol and weight to reduce CVD risk( Reference Galani and Schneider 5 ).
Growing evidence supports effective CVD risk reduction from dietary patterns that include plant sterols( Reference Mensink, de Jong and Lutjohann 6 ), long-chain n-3 fatty acids( Reference Harris, Kris-Etherton and Harris 7 ), fruits and vegetables( Reference Dauchet, Amouyel and Hercberg 8 ), nuts( Reference Kris-Etherton, Hu and Ros 9 ) and unsaturated oils( Reference Mozaffarian, Appel and Van Horn 10 , Reference Moore 11 ). A previous 6-week clinical-based intervention, conducted in sixty-five hypercholesterolaemic patients, showed that a structured lipid-lowering dietary pattern that utilised the synergistic effect of cardioprotective foods had significant positive health outcomes( Reference Cleanthous, Noakes and Brinkworth 12 ). When compared with participants who received either (i) qualitative lifestyle advice alone or (ii) qualitative lifestyle advice together with 20 mg simvastatin/d, the intervention group exhibited significantly reduced LDL-cholesterol (LDL-C) by 15 % and reduced weight and waist circumference( Reference Cleanthous, Noakes and Brinkworth 12 ). However, prior interventions have predominantly relied upon intensive face-to-face counselling, which is limited by financial cost, resource availability and reach.
General practitioners offer an alternative delivery approach, as they are well placed to initiate successful preventive interventions( Reference Tham and Young 13 , Reference Britt, Miller and Charles 14 ) with 88 % of the population visiting a general practitioner at least once per annum( Reference Knox, Harrison and Britt 15 ). Yet general practitioners face barriers in delivering primary prevention strategies due to the complexity of patient counselling in lifestyle behaviour modifications( Reference Silwer, Wahlstrom and Lundborg 16 ), time constraints( Reference Silwer, Wahlstrom and Lundborg 16 – Reference Aoun, Donovan and Johnson 18 ) and inadequate training in applying behavioural-change and weight-loss counselling( Reference Lawlor, Keen and Neal 17 , Reference Aoun, Donovan and Johnson 18 ). Therefore approaches to support general practitioners overcome these obstacles and assist in referral pathways to implement effective CVD risk reduction for their patients are needed.
Another body of research suggests that lifestyle behavioural coaching delivered by allied health professionals via the telephone has the potential to complement and enhance general practitioners’ management of patients at risk of CVD. In a systematic review of studies that predominantly used telephone coaching as the principal method of delivering behavioural change interventions, the majority (twenty of twenty-six studies) achieved significant behavioural improvements in diet (83 %), physical activity (69 %) or both (75 %)( Reference Eakin, Lawler and Vandelanotte 19 ). Three further telephone-based coaching studies conducted within workplaces and community medical centres showed significant reductions in objectively measured weight( Reference Damschroder, Lutes and Goodrich 20 – Reference Vanwormer, Boucher and Pronk 22 ) and improvements in self-reported dietary patterns and physical activity( Reference Eakin, Reeves and Lawler 23 ). In one study where patients were recruited from general practices, significant dietary changes including increased self-reported consumption of vegetables were achieved over 12 months with telephone counselling support( Reference Eakin, Reeves and Lawler 23 ). Despite these positive effects, to date most telephone coaching studies have limited their evaluations to self-reported behaviour changes of diet and/or physical activity as opposed to objective markers of CVD risk factors( Reference Eakin, Lawler and Vandelanotte 19 ). Additionally, most studies have recruited overweight and obese people directly from the community, as opposed to otherwise healthy patients from general practice who have been identified by their general practitioner as being at future risk of CVD( Reference Damschroder, Lutes and Goodrich 20 , Reference Van Wier, Ariens and Dekkers 21 , Reference Sherwood, Jeffery and Welsh 24 ). Currently, there is a lack of a strong evidence base on the effectiveness of telephone-based coaching on CVD risk factor reduction and weight management in the primary care setting( Reference Hardcastle, Taylor and Bailey 25 ). Therefore the purpose of the current pilot study was to evaluate a primary prevention care model using telephone support delivered through an existing health call centre to general practitioner-referred patients at risk of developing CVD, using objective measures of CVD risk reduction and weight loss.
Experimental methods
The present pilot study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human patients were approved by the CSIRO Food and Nutritional Sciences Human Research Ethics Committee. Written informed consent was obtained from general practices and all patients prior to study commencement. The trial was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12610000341022).
General practice and participant recruitment
Two general practices in South Australia were recruited: Hills Medical Service at Aldgate (Aldgate) and Golden Grove Health Centre at Wynn Vale (Golden Grove). Electronic medical records were initially searched via key terms (age 30–56 years; BMI ≥ 26·0 and ≤40·0 kg/m2; waist circumference >102 cm for men, >88 cm for women) to match participants to the study inclusion criteria. General practitioners (five at Aldgate and ten at Golden Grove) reviewed the final patient lists to remove participants who could not perform physical activity without pain, had insulin-dependent type 2 diabetes or cancer, were on medication that may have been adversely affected by the intervention (e.g. warfarin), and/or were pregnant or breast-feeding. Eligible participants were then sent a letter from the general practice inviting them to participate in the study. Each participating general practice received a $AUD 1500 payment to reimburse general practitioners’ and staff's time and administrative costs.
A total of 237 participants (n 73 Aldgate; n 164 Golden Grove) were invited to participate in the study. Of those, fifty-six participants returned consent forms in reply-paid envelopes to the research office indicating they wished to be contacted. Five participants did not meet the inclusion criteria and two participants declined to participate. A total of forty-nine participants were enrolled into the study which was conducted between August and November 2010. Thirty participants were female and the age range of the sample was 35–56 years (mean 48·0 (sd 5·88) years), with mean BMI of 33·13 (sd 5·39) kg/m2.
Design
Eligible participants took part in a 12-week randomised parallel study in which they were electronically block randomised, stratified by general practice, to either the treatment group (who received a comprehensive lifestyle intervention programme (CLIP), n 26) or the control group (who received usual care from the general practitioner (‘usual GP care’), n 23; see Fig. 1). At baseline (Week 0) and at the end of the intervention (Week 12), participants attended their usual general practice for measurements of fasting plasma lipids, blood pressure, weight, height and waist circumference by the practice nurse. Participants also completed questionnaires assessing physical activity( Reference Craig, Marshall and Sjostrom 26 ) and motivation and self-efficacy( Reference Levesque, Williams and Elliot 27 ). Following baseline assessments, participants were provided with a copy of their clinical results and a package of study intervention materials, which contained either the CLIP or the control information. The nurse and the participant were blind to the treatment condition with CLIP and control packages identical in size and appearance, identified only by an ID number and a treatment code, which were recorded by the practice nurse.
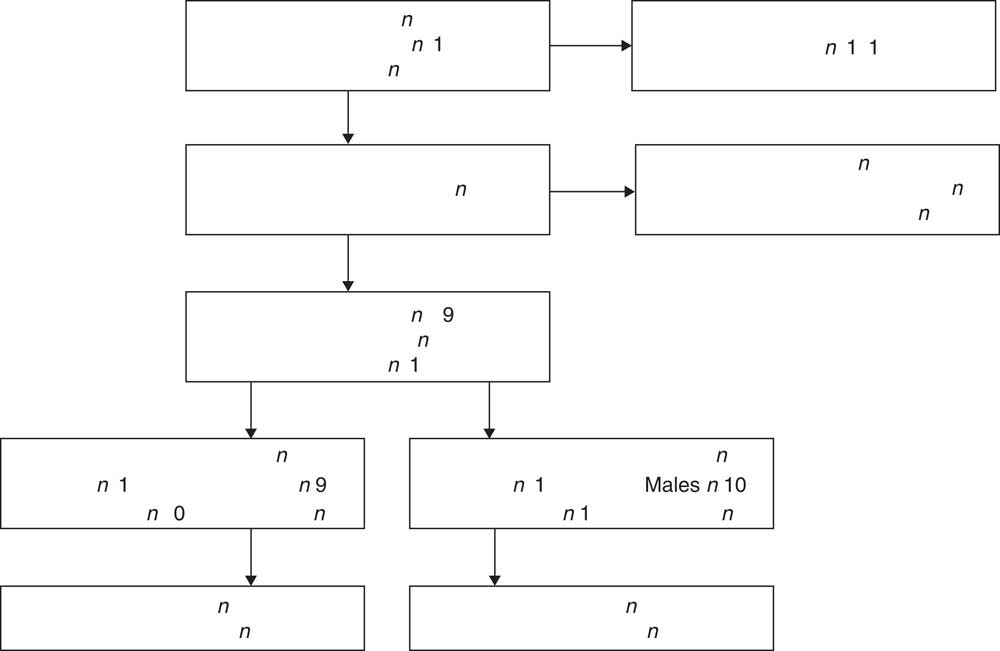
Fig. 1 Flow diagram for the study recruitment process and participant flow across treatment conditions and general practice (CLIP, telephone-supported comprehensive lifestyle intervention programme; usual GP care, usual care from the general practitioner)
Interventions
Treatment (CLIP) group
At baseline the CLIP group received the CLIP handbook, containing a summary dietary guide, sample menu plans and recipes based on the clinical cardiovascular dietary intervention( Reference Cleanthous, Noakes and Brinkworth 12 ). The programme was kilojoule (kJ) controlled, low in saturated fat (<8 % total energy) and sodium, contained 2 g of plant sterols, was high in n-3 fatty acids from fish and enriched foods (>500 mg/d), was high in soluble fibre and included cardioprotective foods such as whole grains, nuts, fruit and vegetables. At the commencement of Week 4, intervention participants received a full copy of the CSIRO Healthy Heart Programme( Reference Noakes and Clifton 28 ) commercial book publication. This coincided with the introduction of the CLIP aerobic exercise component, which consisted of brisk walking for 30–60 min for 3–5 d/week, depending on fitness level. At Week 6, a muscle-strengthening programme was initiated, comprising of two sets of eight to ten repetitions of whole-body exercises on two non-consecutive days of the week. Participants were encouraged to keep a daily exercise diary to monitor their exercise compliance. Throughout the 12-week intervention, participants also continued with their usual GP care.
One week into the intervention, participants were prompted to contact the Heart Foundation Health Information Service (HIS) to initiate telephone coaching sessions. The HIS is accessible to the whole community and provides information on heart health to people currently living with CVD, those with CVD risk factors and those wishing to develop healthier lifestyles. Staff at the HIS included one dietitian and five qualified health professionals trained in motivational interviewing and heart health. Prior to study commencement, HIS staff received training on the fundamental aspects of the CLIP by a Heart Foundation dietitian in collaboration with research staff. Participants received a total of seven calls from the same staff member – these comprised an introductory call to explain the programme, followed by one call every two weeks for twelve weeks. In the introductory call, coaches discussed the normal ranges expected for the baseline measurements taken, outlined the key features of the CLIP diet, and encouraged participants to set a programme goal that they could achieve before the next call. Participants were instructed to record and report their weight and waist circumference every fortnight. The following six calls focused on supporting the participant with goal progress, checking that key foods were being accurately consumed, solving any problem with dietary issues that had arisen in the previous two weeks and supporting the participant with exercise compliance. The introductory telephone call averaged 37 (sd 7) min and the following six calls averaged 20 (sd 11) min in duration. Participants received an average of 6·5 calls.
Control (usual GP care) group
The control group received usual GP care and general printed lifestyle materials, which provided them with a guide to healthy lifestyle choices. The written materials were produced from current Australian Government health initiatives and are readily available to the general public. They included: (i) The Australian Guide to Healthy Eating( 29 ), a guide to help people make healthy and varied food choices; (ii) the Go for 2 Fruit and 5 Vegetables booklet( 30 ), which discusses the importance of fruit and vegetable consumption and illustrates how to include more in the diet; and (iii) the Measure Up booklet( 31 ), which encourages the measurement of waistline so as to be aware that larger waistlines increase the risk of developing chronic diseases such as CVD.
Outcome measures
A CardioChek PA® Analyser (Polymer Technology Systems, Inc., Indianapolis, IN, USA) was used to measure LDL-C and total cholesterol using a fresh capillary whole blood sample. Results obtained with a CardioChek PA Analyser are clinically interchangeable with those obtained by sending samples to a laboratory( 32 ). Seated blood pressure was measured for three consecutive readings with an OMRON® Intelli sense (Digital Model No. HEM-907; Omron Healthcare, Inc., Lake Forest, IL, USA) and averaged. Participants wore light clothing and were weighed without shoes using electronic digital scales (TANITA® BF-681; Tanita Corporation of America, Inc., Arlington Heights, IL, USA). Waist circumference was measured at the top of the iliac crest with a plastic measuring tape and taken at minimal respiration for three consecutive readings, which were averaged. Height was measured, without shoes, using a stadiometer (SECA®, Hamburg, Germany). Physical activity was assessed using the International Physical Activity Questionnaire (IPAQ), which is a measure of self-reported physical activity in the preceding 7 d( 33 , Reference Craig, Marshall and Sjostrom 34 ).
Motivation was assessed using the Treatment Self-Regulation Questionnaire (TSRQ)( Reference Levesque, Williams and Elliot 27 ) and is a measure of two types of motivation: autonomous and controlled( Reference Williams, Grow and Freedman 35 ). Autonomous motivation is the motivation to change behaviours because the person perceives that it is his/her choice to do so( Reference Williams, Grow and Freedman 35 – Reference Ryan, Patrick and Deci 37 ). Controlled motivation is where a person adopts or changes behaviour because he/she feels guilt or pressure to do so( Reference Williams, Grow and Freedman 35 – Reference Ryan, Patrick and Deci 37 ). Participants answered twelve questions on a scale of 1–7, with the scores for each subscale (autonomous motivation; controlled motivation) averaged separately. Health self-efficacy was measured using a single question (‘I am confident that I can manage to stick to a healthy diet’) with a scale ranging from 1 to 7, where 7 = ‘very confident’.
Statistical analysis
Statistical analyses were performed with the statistical software package SPSS PASW Statistics 18. Prior to analysis, data were checked for normality. Due to a positive skew in the physical activity data, a log transformation was performed before conducting the analysis. Reliability analyses were also conducted on the baseline scores of the TSRQ (total α = 0·87: autonomous α = 0·88, controlled α = 0·91) to check for internal consistency. One-way ANOVA was used to determine any baseline between-group differences. A series of mixed models using unstructured covariance matrices was conducted to assess the effect of treatment on outcome variables with BMI and gender as covariates, allowing for analysis of all available data. When a main effect was observed, post hoc analyses were performed using Bonferroni correction. Correlation analyses were used to determine baseline predictors of outcome measures. Data are presented as estimated means (EM) with their standard errors, unless otherwise stated, with the probability value set at P < 0·05.
Results
Participants
Of the forty-nine participants who entered the study at baseline, five withdrew before the completion of the intervention at Week 12 (CLIP n 3, control n 2; Fig. 1). Twelve participants were recruited from the Aldgate general practice (CLIP n 6, control n 6), with thirty-seven participants from the general practice at Golden Grove (CLIP n 20, control n 17). One participant from the control group was excluded because they had an extreme LDL-C reading that was greater than 3 sd above the group mean. Data from forty-eight participants were used for analysis of the physiological measurements. Of the participants, eleven (CLIP n 3 v. control n 8, P = 0·41) were taking blood pressure medication, with 15 % of the participants hypertensive, and five (CLIP n 2, control n 3) were taking lipid-lowering medication, with 58 % of participants classified as having dyslipidaemia. There was no change in lipid or blood pressure medication after 12 weeks for either group.
Lipids, blood pressure, weight and waist circumference
There was a significant time-by-treatment interaction effect for LDL-C (F(1,42) = 11·33, P = 0·002) and total cholesterol (F(1,41) = 8·36, P = 0·006). Post hoc analyses revealed that CLIP participants demonstrated significantly greater reductions in LDL-C and total cholesterol at Week 12 when compared with controls (Table 1). There was also a significant main effect for treatment on LDL-C (F(1,43) = 15·50, P = 0·001) and total cholesterol (F(1,44) = 8·18, P = 0·006), but this was modified by the interaction over time.
Table 1 Results for LDL-C, total cholesterol, SBP, DBP, weight, waist circumference and TSRQ autonomous motivation, at Week 0 and Week 12, for CLIP and control groups
EM, estimated mean; LDL-C, LDL-cholesterol; SBP, systolic blood pressure; DBP, diastolic blood pressure; TSRQ, Treatment Self-Regulation Questionnaire; CLIP, telephone-supported comprehensive lifestyle intervention programme; control, usual care from the general practitioner (usual GP care).
Significant time-by-treatment interaction: *P < 0·05, **P < 0·01.
Significant post hoc between-group difference: †P < 0·05, ††P < 0·01.
There was no significant effect of treatment on systolic (F(1,45) = 0·28, P = 0·60) or diastolic blood pressure (F(1,43) = 0·52, P = 0·47), with levels remaining stable across the intervention in both groups (Table 1).
At Week 12, CLIP participants weighed less compared with controls, but this difference did not reach statistical significance (F(1,42) = 3·63, P = 0·063; Table 1). Similarly, there was no significant effect of treatment for waist circumference (F(1,43) = 0·32, P = 0·577).
In CLIP, there was a significant positive correlation between weight loss and the reduction in LDL-C (r = 0·560, n 26, P = 0·003) and total cholesterol (r = 0·526, n 26, P = 0·006).
Physical activity
Thirty-eight participants (CLIP n 20, control n 18) were included in the IPAQ analyses. Six participants in each group did not complete and/or return the IPAQ at baseline, and two further participants (CLIP n 1, control n 1) were excluded according to the IPAQ guidelines (Rule 7·2) for reporting excessive minutes of activity( Reference Ainsworth, Haskell and Leon 38 ). At baseline, physical activity levels were similar between both groups (P = 0·27) and remained relatively constant in both groups throughout the intervention (F(1,36) = 1·07, P = 0·31 for time-by-treatment effect).
Psychological measures
A total of thirty-eight participants (CLIP n 20, control n 18) completed the TSRQ and the health self-efficacy question at baseline and Week 12, and were included in the analyses. There were no significant differences between the groups on any of the baseline measures. There was no effect for the controlled motivation subscale of the TSRQ, but a significant time-by-treatment interaction effect occurred for the autonomous subscale (F(1,36) = 6·88, P = 0·013). Post hoc analyses revealed that the CLIP participants reported greater autonomous motivation at Week 12 compared with controls (Table 1).
Weight loss was moderately correlated with changes in health self-efficacy for both CLIP (r = −0·68, n 20, P = 0·001) and control groups (r = −0·55, n 18, P = 0·019), with no significant difference between the two correlations (z = −0·59, P = 0·28) and no interaction effect.
Discussion
The current pilot study showed that applying a novel approach to a primary care prevention model for CVD effectively reduced blood lipids and CVD risk in general practitioner-referred patients who were at future risk of developing CVD. By using telephone coaching support delivered through an existing health call centre, participants in the CLIP group achieved reductions of 16·8 % in LDL-C and 10·4 % in total cholesterol. This was significantly greater than in the control group, and is quantitatively similar to the LDL-C reduction achieved with the CLIP delivered in a clinical setting( Reference Cleanthous, Noakes and Brinkworth 12 ). Importantly, in line with recommendations that a reduction in LDL-C of approximately 10 % is clinically significant for reducing CHD disease risk( Reference Bresson, Flynn and Heinonen 39 , Reference LaRosa 40 ), these results have pertinent clinical relevance.
While many studies with a clinical focus have reported reductions in LDL-C and total cholesterol of similar magnitude( Reference Ebrahim, Taylor and Ward 41 ), community interventions appear to report reductions much lower than in the current investigation( Reference Sherwood, Jeffery and Pronk 42 ). In one community study conducted in Pennsylvania, USA, participants (n 150) in the treatment group received high-fibre foods once weekly, plus weekly telephone calls( Reference Kris-Etherton, Taylor and Smiciklas-Wright 43 ). Over 7 weeks, this approach successfully reduced participants’ LDL-C by 7·1 % and total cholesterol by 5·6 %, which was significantly different compared with the usual care group. In the current study, the CLIP achieved a reduction in LDL-C, total cholesterol and weight (albeit not significant) with seven coaching telephone calls over 12 weeks. With the exception of one study( Reference Byrne, Cooper and Fairburn 44 ), previous investigations have achieved similar improvements in health but have implemented programmes outside the general practice setting with greater contact intensity and frequency of contact( Reference Damschroder, Lutes and Goodrich 20 – Reference Hardcastle, Taylor and Bailey 25 ).
Despite not reaching statistical significance, there was a trend for an effect of treatment on weight loss, with results comparable to previous research( Reference Eakin, Lawler and Vandelanotte 19 – Reference Van Wier, Ariens and Dekkers 21 , Reference Eakin, Reeves and Lawler 23 , Reference Sherwood, Jeffery and Welsh 24 , Reference Sherwood, Jeffery and Pronk 42 ). Participants in the CLIP group achieved a mean weight loss of 3·6 kg over the course of the intervention. In line with our results, a 12-week study in American veterans (n 14) recruited from a Veteran Affairs Medical Center showed a mean weight loss of 3 kg( Reference Damschroder, Lutes and Goodrich 20 ) with support from twelve telephone calls, while a 16-week study in primary care patients (n 146) achieved a mean 2 kg weight loss with the use of a clinician-delivered intervention( Reference Wilson, Johnson and Jones 45 ). Despite the provision of standard government information, participants in the control group for our study achieved a lower mean weight loss of 1 kg than the intervention group of 3 kg. This is consistent with a WHO review of the effectiveness of interventions in primary health care, which found that printed health education materials alone are generally not effective in changing behaviour( Reference Anderson, Parker and Steyn 46 ). Importantly, however, there was a significant association between the reduction in LDL-C and total cholesterol and weight loss. This demonstrates that CLIP played an important role in weight management, which can be attributed, at least in part, to the marked reductions in lipid and total cholesterol levels, and thus overall reduction in CVD risk.
The CLIP was effective in enhancing self-motivation to adopt a healthy lifestyle. This is in line with an evaluation of the TSRQ, which found that autonomous motivation was positively associated with healthier lifestyle choices such as higher levels of fruit and vegetable consumption and increased levels of physical activity( Reference Levesque, Williams and Elliot 27 ). While the use of motivation measures in telephone interventions is scarce, a 16-week Internet programme with a focus on weight loss reported significant increases in autonomous motivation for participants who achieved a 5 % weight loss( Reference Webber, Tate and Ward 47 ). There was no correlation in the present study between autonomous motivation and weight loss, but autonomous motivation was a significant predictor of LDL-C reduction for participants in CLIP. It is possible that the combination of CLIP with telephone coaching engaged participants more in cholesterol change behaviours rather than weight loss, increasing their motivation to make personal lifestyle choices to reduce their CVD risk.
For both CLIP and the control group, changes in self-efficacy were associated with weight loss, suggesting that confidence in adhering to a healthy diet improves with weight loss. However, the difference between the two correlations was not significant. Previous studies have reported that self-efficacy influences weight loss through the mediating effects of behaviours such as goal setting, planning and the monitoring of behaviours( Reference Linde, Rothman and Baldwin 48 , Reference Bas and Donmez 49 ). Future interventions should assess other factors that may contribute to health self-efficacy, such as participants’ satisfaction and perception of weight in relation to weight-loss goals( Reference Byrne, Cooper and Fairburn 44 ).
CLIP participants did not appear to increase physical activity levels relative to controls. A comprehensive systematic review reported that of four studies evaluating the effect of telephone-supported interventions on dietary intake and physical activity, two reported significant positive outcomes for diet and exercise( Reference Vale, Jelinek and Best 50 , Reference Emmons, McBride and Puleo 51 ) while one found a trending improvement across both behaviour domains( Reference Hellerstedt and Jeffery 52 ) but not to a significant level( Reference Eakin, Lawler and Vandelanotte 19 ). Akin to the current investigation, the fourth study( Reference Kris-Etherton, Taylor and Smiciklas-Wright 43 ) reported significant changes for diet only with no changes in physical activity. Unlike previous studies that recruited motivated participants with a recent diagnosis( Reference Vale, Jelinek and Best 50 , Reference Emmons, McBride and Puleo 51 ), the current study and the aforementioned investigation recruited otherwise healthy adults who were at risk of CVD. It may be that engagement in the programmes across all four studies was affected by the immediacy of need for behaviour change. Importantly, however, CLIP and the latter study( Reference Kris-Etherton, Taylor and Smiciklas-Wright 43 ) incorporated physical activity within a total lifestyle change programme that was supported by a professionally tailored and personable telephone service, rather than a monitoring telephone call every 4–6 weeks( Reference Vale, Jelinek and Best 50 , Reference Emmons, McBride and Puleo 51 ). It is therefore possible that using a holistic approach to behaviour change may not allow the participant opportunity to concentrate their motivations on a specific behaviour change (i.e. diet or physical activity), but rather supports their overall efforts towards better health.
Strengths and limitations
A key strength of the study and the primary prevention care model developed includes the referral of participants by their general practitioners and the use of an existing call centre infrastructure. Furthermore, the collection of objective outcome measures within the community/telephone setting was an innovative approach and enabled a greater understanding of the clinical impact of CLIP on CVD risk reduction. This enabled general practitioners to deliver their usual care without having to deliver the complexity of a lifestyle intervention and ongoing support. This facilitates the potential translation of these research findings into a general practice care model subject to long-term cost-effectiveness analysis. A limitation of the study is the lack of power to detect differences in physical activity, waist circumference and blood pressure, as well as the short duration of treatment (3 months). However, these data provide the requisite information necessary to derive appropriate sample size calculations for these parameters to inform future studies. The present study did not assess changes in dietary intake and quality, although lipid and weight changes corroborate reductions in saturated fat intake and energy balance. The generalisability of findings across socio-economic groups cannot be assumed as there was little socio-economic variability in the communities from which the participants were drawn( 53 ).
Conclusions
In general practitioner-referred participants, the CLIP supported by telephone coaching through the Heart Foundation call centre was effective in providing a significant reduction in LDL-C and a trend towards a modest weight reduction without face-to-face contact. The telephone coaching sessions were well accepted and able to be tailored to the participants’ needs. Further research is warranted to determine the long-term cost-effectiveness of this approach.
Implications for practice
CVD is one of the leading preventable diseases in Australia( 1 ), with most risk factors modifiable by lifestyle and dietary choices( 4 ). General practitioners are a respected source of information( Reference Tham and Young 13 , Reference Britt, Miller and Charles 14 , Reference Aoun, Donovan and Johnson 18 ), and a general practitioner diagnosis can be a significant predictor of behaviour change( Reference Singh, Somers and Clark 54 ). However, many general practitioners are constrained by time, finances and resources to successfully implement preventive strategies. Telephone coaching on the CLIP can reduce LDL-C and is able to complement general practitioner care by providing ongoing support to patients to reduce cardiovascular risk.
Acknowledgements
Sources of funding: The present study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Conflicts of interest: The authors have no conflict of interests. Authors’ contribution: K.L.S. was responsible for analysis and preparation of the manuscript. B.W. was responsible for study development and assistance with manuscript write up. K.B. was responsible for the study coordination and assistance with additional analysis. N.S., G.B., P.M. and M.N. were responsible for overall study design and supervision of the project. Acknowledgements: The authors gratefully acknowledge Lisa Clements for collecting the objective measures; Jackie Rakowski and the team at the Heart Foundation Health Information Service for conducting the telephone coaching sessions; Lindy Lawson for nursing expertise; and Julia Weaver and Pennie Taylor for coordinating the data sources.




