Obesity and type 2 diabetes are increasing among children due in part to poor diet habitsReference Fagot-Campagna, Pettitt, Engelgau, Burrows, Geiss and Valdez1–Reference Pinhas-Hamiel and Zeitler3. Many dietary behaviours are learned within a family context. Parents influence children’s dietary behaviours through control of access to foods, meal structure, family rules regarding food intake, modelling, children’s perception of adult dietary behaviours, use of bribes and threats, and sharing of health knowledgeReference Feunekes, De Graaf, Meyboom and Van Staveren4–Reference Francis and Birch10. There is still much that is not understood about the complex interaction between parents and children around food, especially with regard to teenagers and pre-teensReference Baranowski, Hearn and Gochman11.
To control their disease, most adults with diabetes need to change their dietary behaviours. Such changes may challenge habitual family interactions around food. Yet adult-focused diabetes interventions and counselling often provide little or no guidance on how to make personal dietary changes while also providing food to children in the household. When adults are motivated to make changes for themselves, there may be an opportunity to help parents extend those dietary changes to their children. But first those working with parents must better understand the interactions between adults and children during adults’ transitions to healthier dietary habits.
Since previous work has not described this phenomenon, we chose a qualitative methodology to explore the parent–child dynamics and practical issues arising in this context. Our study examines families in which one inner-city African American or Latino adult caregiver with diabetes had completed a diabetes self-management intervention promoting healthy dietary behaviours and was actively attempting to make dietary changes. We explored how these adults approached providing food for their children and how their children reacted to household dietary changes.
Methods
We followed community-based participatory research principles that emphasise community involvement throughout the research processReference Schulz, Parker, Israel, Becker, Maciak and Hollis12. We conducted qualitative, semi-structured parallel interviews of adults with diabetes who had completed one year of a community-based intervention and a child in their home.
The REACH intervention
Racial and Ethnic Approaches to Community Health (REACH) Detroit Partnership, funded by the Centers for Disease Control and Prevention, is community-based intervention in inner-city Detroit aimed at improving self-management and outcomes among African American and Latino adults with type 2 diabetes. The intervention involved one year of activities, including 11 weekly two-hour self-management training sessions and regular meetings with a ‘family health advocate’, a trained lay person acting as a case manager and lifestyle coach. Intervention messages focused on diabetes self-management, healthy diet and exercise; none included information on children. REACH participants showed a statistically and clinically significant decrease in average blood glucose (glycosolated haemoglobin: −0.8%) vs. a comparison group that showed no change, and reported significant dietary improvementsReference Feathers, Kieffer, Palmisano, Anderson, Sinco and Janz13, 14.
Sampling
To gather information-rich cases, we used purposeful sampling based on the age and sex of the child and the race/ethnicity of the familyReference Patton15–Reference Sandelowski17. We purposefully sampled children aged 10–17 years from REACH families with a goal of recruiting at least two children (one male and one female) of each race in each age range (10–11, 12–13, 14–15, 16–17 years). We recruited families in waves to fulfil our sampling framework until all eligible families were contacted.
Inclusion criteria for children were their age (between 10 and 17 years) and living with a REACH participant for at least one year, while exclusion criteria included a diagnosis of diabetes. Adult inclusion criteria were completion of one year of REACH activities (including at least two REACH classes) and having an eligible child. Adults and children were required to speak either English or Spanish. We enrolled more 12–13-year-olds than initially planned as we found in early interviews that they expressed themselves more clearly than the younger children but were more dependent on their parents than the older children.
Data collection interviews
We conducted audio-taped, semi-structured, face-to-face interviews with children for 50–75 min in the child’s preferred language (English or Spanish) without the adult present. Relevant domains included messages received from parents and others regarding eating, descriptions of family meals, current eating behaviours and dietary changes, and changes in family diet behaviours since the adult was diagnosed with diabetes and since completing the REACH programme (see examples in Table 1).
Table 1 Sample of questions from the semistructured interview guides
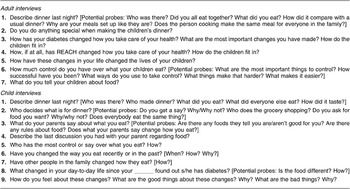
Adult interviews lasted 30–90 min. Relevant domains included perceptions of the child’s diet; descriptions of family meals; changes in the household diet since the adult developed diabetes and since the adult started the REACH programme; how these changes affected the children; parent’s perceived influence on children’s eating habits; messages to children about diet, and facilitators and barriers to child diet change (see Table 1). The principal investigator (H.H.L.) conducted all English-language interviews. Trained, Masters-level, native Spanish-speaking interviewers conducted Spanish-language interviews, with the principal investigator present to add questions as she saw necessary. The study was approved by the Institutional Review Board of the University of Michigan School of Medicine.
Analysis
Interviews were audio-taped, transcribed and verified. Data were analysed and collected concurrently so insights from completed interviews could inform ongoing data collection and analysis. We analysed the interviews thematically, assisted by QSR NVivo. Our overall approach followed the ‘Editing Analysis Style’, which contains both deductive and inductive elementsReference Crabtree and Miller18. Deductive codes were derived from analysis frameworks based on social cognitive theory and literature review. Inductive codes were derived from the interviews to create new categories and refine framework categories.
Following this approach, two investigators independently coded transcripts and used an iterative process to compare results until agreement was reached. Other research team members read selected transcripts to compare their code interpretations with the two primary coders. After the coding scheme was developed, the principal investigator coded all transcripts; a second researcher coded a subset to verify code reliability. All Spanish transcripts were independently coded in Spanish by a trained native Mexican-Spanish speaker and the principal investigator. Coded transcripts allowed cross-case comparison and analysis of patterns and themes. We increased the credibility of this analysis through rigorous and systematic data collection and analysis, the use of multiple readers and coders, and by documenting the reasons for analytic decisionsReference Mason19. All authors were involved in refining the thematic analysis and at least two team members compared the final analysis with the original transcripts.
Results
Sample description
The final sample included 29 interviews from 15 families (14 adult–child pairs and one child only) (see Table 2). Although baseline data indicated that 50 of 180 families had children between 10 and 17 years old, only 30 families were eligible: 10 did not meet participation criteria, nine had no eligible children and one relocated. Of 30 eligible families approached for enrolment, 15 accepted, 10 declined and five could not be contacted. Fourteen of 15 adult participants were women. There were 10 parents and five grandparents. All grandparents except one were the child’s primary caregiver. The other grandparent shared parenting responsibility with the child’s mother but was primarily in charge of meal preparation. We use the term ‘parent’ to denote parent or grandparent. There were eight male and seven female children ranging from 10 to 17 years of age; seven of the 15 children were in the 12–13-year-old range and two were in the 16–17-year-old group (see Table 2). Eligible non-participants were more likely to be African American (53% vs. 33%), have taken fewer REACH classes (mean: 5.7 vs. 7.7) and have shown a smaller increase in fruit and vegetable consumption after the intervention. After repeated failed attempts to complete the corresponding adult interview, the single child interview was included because it added to the breadth of child perspectives on change.
Table 2 Characteristics of families interviewed
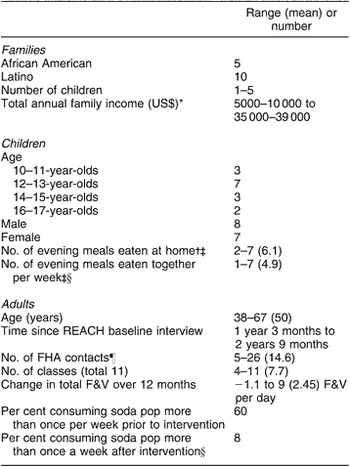
REACH – Racial and Ethnic Approaches to Community Health; FHA – family health advocate; F&V – fruits and vegetables.
*Out of 12 responses.
†Out of 14 responses.
‡Child report.
§Out of 13 responses.
¶FHA contacts include in-person meeting and phone calls with documented in-depth interaction or documented length over 10 min.
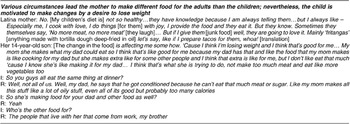
The final sample included 14 motivated adults who all expressed the desire to include their children in the healthy dietary changes they were making or had made. A few adults described ambivalence about the extent of the changes they desired in their children’s diets. (The results section uses the following convention: a few = two or three; some = four to six; half = seven; a majority = eight or nine; many = 10 to 12; almost all = 13 or 14). A majority of parents tried to decrease children’s intake of candy and soda and a majority stated that they were motivated by concern about their children developing diabetes or about their child’s weight (either that they were already overweight or might become overweight). One Latina mother said: ‘She wants to eat all the time. And I tell her that’s not right… Because she’s going to get fat and then she’ll get diabetes afterwards.’
Five of the 15 children described themselves in the survey portion as overweight, and two additional children described themselves as the right weight but were trying to lose weight. (One of these two children in the interview described herself repeatedly as ‘a little fat’ and ‘kind of fat’ and the other said he was ‘fat’ but had lost some weight and was now ‘big boned’ and still needed to lose more weight; both had self-reported body mass index (BMI) greater than the 95th percentile.) All of these seven children appeared overweight to the interviewer (H.H.L.). No survey response was available for two children described by the interviewer (H.H.L.) as ‘skinny/appropriate’ and ‘skinny’ (this child’s BMI was in the 15th percentile).
A majority of children acknowledged that their parents’ dietary changes were probably also good for them, and none described the changes as unhealthy or bad for them. Although a few children accepted the changes, many children were ambivalent and a majority of children resisted changing their diets. One child airily expressed a theme common among resistant children: ‘You [parent] change your diet. You’re a diabetic.’ Ten of the 15 children reported obtaining junk food outside the home (store, school) ranging from one large bag of candy a month to chips and soda every day.
Family patterns of dietary change
As adults tried to change their own dietary patterns, family meals became both a main venue where parents sought to influence children’s diets and a battleground for conflict about those changes. Four different family patterns emerged from the interviews. Patterns were characterised by whether or not parents routinely provided alternative foods to their children and whether or not children resisted dietary changes.
• Same food: children are expected to eat the same food as the adult with diabetes and alternatives are not offered.
• Different food: if children do not want to eat the new healthier food, they are prepared alternatives or allowed to make food for themselves.
• No resistance: child and adult describe the child as going along with changes with minimal or no resistance.
• Resistance: child, adult or both describe the child as resisting changes (i.e. refusing to eat desirable food, bringing restricted food into home).
These patterns are useful analytic categories. While no one family exactly fits into one pattern at all times, each family was categorised based on their general attitude and approach towards dietary change and the children’s overall response. A few families described shifting from one pattern to another over time, especially as children accepted some dietary changes.
All families varied in the extent of dietary changes made. Some changed many parts of their diet simultaneously while others focused on changing certain habits incrementally, such as decreasing soda consumption.
Family Pattern 1: Same food/no or little resistance
In Pattern 1 families (five families; see Table 3), one meal is made for everyone and the children are generally expected to eat the same food as the adult with diabetes. While in the home, children went along with most of the dietary changes.
Table 3 Same food/no or little resistance
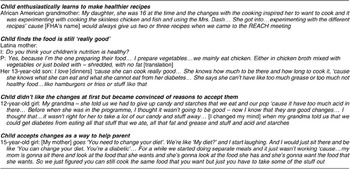
Children in these families did not resist changes but varied in how fully they accepted them. One child (a sibling not interviewed) was described by her parent to have actively promoted dietary changes by learning and cooking new recipes. Two children expressed contentment because the food still tasted good. Two described resisting the changes initially but eventually accepting them (one as a way to help her parent). Another child went along with the changes since he ate what he wanted outside the house. Despite accepting changes at home, three of these five children said they still ate fast food, chips and soda elsewhere once to three times a week. Pattern 1 included one child who described him/herself as overweight, two African American families and three grandparents.
Family Pattern 2: Same food/resistance
In Pattern 2 families (three families; see Table 4), one meal is made for everyone and children are generally expected to eat the same food as the adult with diabetes but there is ongoing conflict over food. Forms of resistance included refusing certain foods, complaining, bringing home restricted foods, and sneaking other food from the kitchen. In this group and in Pattern 3 families, many children disliked the taste of ‘healthy’ food and were reluctant to give up foods such as chips, soda, candy and pizza. One parent described how her children accepted some changes over time, such as consuming less soft drinks or drinking lower-fat milk, but her daughter claimed that she had not changed. In another family, the child said she was getting used to some vegetables but still refused eat other new foods. Pattern 2 included two children described as overweight, two African American families and one grandparent.
Table 4 Same food/resistance
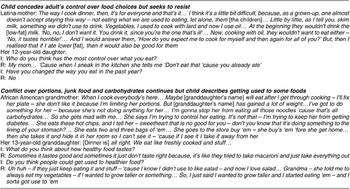
Family Pattern 3: Different food/resistance
In Pattern 3 families (six families; see Table 5), children resist dietary changes and parents allow the children alternatives to new food choices. When they do not like the food prepared for the adult, either children make food for themselves or some parents make children a separate or altered meal. In some families the adult with diabetes would eat a ‘healthy’ frozen dinner or salad while the family ate a dinner that they preferred. Whether prepared by themselves or a parent, children often chose less healthy alternatives (e.g. hotdogs, sugary cereal, ice cream and frozen meat lasagne) but occasionally ate fruit and healthier cereals.
Table 5 Different foods/resistance

Two families in this group expected children to decrease soda or sugar consumption. Some described gradual small changes in the children’s diets as children accepted new foods.
Two parents indicated ambivalence towards how much change their children should be expected to make but overall believed in making changes. Ambivalent about her children eating foods low in salt and fat, a third parent decreased them in her own but not her children’s diet. However, she was attempting to switch the family to diet soda and sugar substitutes.
Three families described a child trying to motivate his/her parents to make dietary changes while resisting changes for him/herself. In two of these families, resistance from the spouse added to the need for separate meals. In contrast, another family in the same meal/no resistance group was trying to include a resistant father. However, if the father ate separately then the children ate healthier food with their mother. Finally, three different meal/resistance parents described struggling with health issues and fatigue which sometimes led them to allow children to make their own meals. In Pattern 3, three of the six children described themselves as overweight, one family was African American and one adult was a grandparent.
Family Pattern 4: Different food/no resistance
In Pattern 4 families (one family; see Table 6), the child does not resist changes but the parent is still providing different food for the children. In the only interviewed family of this type, the Latina mother made special food for herself and the father but different or modified food for everyone else. Interestingly, although the mother continued to make him separate food, the overweight child interviewed wanted to change his diet to lose weight. He described eating his parent’s meals because they were healthier and had fewer calories.
Table 6 Different foods/no resistance
Discussion
When adults with diabetes are motivated to make dietary changes for themselves, there may also be an opportunity to improve the diets of their children. In our study, adults found various ways to make personal dietary changes while providing food for their family, ranging from expecting everyone to eat the same thing to preparing separate meals. Many children resisted dietary changes but some did acquiesce. Children who went along with changes reported resisting initially then adjusting (one changed to help her parent); not resisting because the food still tasted good; or not resisting because they obtained the food they wanted elsewhere. The intersection of adults’ meal strategies (expecting the children to make the same dietary changes as the adult with diabetes vs. offering separate meal options) and children’s reaction to the changes (resistance or acceptance) can be used to categorise families into patterns. These patterns highlight the tension between an adult who must make dietary changes to control his/her diabetes and a child who is accustomed to certain foods and not necessarily motivated to make changes and also suggest hypotheses for future research.
We found no prior published studies of how dietary changes in chronically ill adults affect their children. However, data on families with middle-school children suggests that about a third allow teenagers to make themselves dinner and to eat dinner separate from the familyReference Boutelle, Lytle, Murray, Birnbaum and Story20, Reference Boutelle, Birnbaum, Lytle, Murray and Story21. Thus, while other families may also allow teenagers to avoid food they dislike, this strategy may become more pronounced in the setting of adult’s dietary changes. Furthermore, our study found that the younger children and sometimes the spouse also ate something different from the parent with diabetes.
Patterns seen in our study may in part reflect the cultural/racial differences in parenting style noted in other studies. Four of five African American families were among the two same food patterns and in contrast six of the 10 Latino families were in the two different food patterns. One study suggested that Latino families practised more permissive parentingReference Cullen, Baranowski, Owens, de Moor, Rittenberry and Olvera22 and anotherReference Kaiser, Melgar-Quiñonez, Lamp, Johns and Harwood23 suggested that less acculturated Latina mothers were more likely to offer alternatives when a child refuses to eat. Although this was consistent with many of our Latino families, some chose a less permissive style towards diet. In addition these patterns reflect more than just feeding style, as parents’ initial plans are often modified by children’s reactions and other social circumstances. For example, one African American mother planned to feed everyone the same way but it became too difficult because of children’s resistance, her hectic work schedule and other relatives sharing her home.
How the child’s weight affected family patterns deserves further study. Although each pattern included both children who perceived themselves as overweight and normal weight, the same food/no resistance pattern included five children only one of whom was considered overweight. A reviewReference Faith, Scanlon, Birch, Francis and Sherry24 suggests that heavier children experience more maternal restriction and parental discouragement of eating. One could hypothesise this might increase conflict and resistance to change. On the other hand, these differences could reflect different family dynamics which also contributed to the children’s weight. In general, the factors influencing parents’ choice of different strategies (such as health status, response of spouse and children’s reactions) warrant additional study.
Beyond describing family behaviour, this study has implications for future intervention design and evaluation. A better understanding of the significant variation in family responses to adult dietary change is crucial to designing effective dietary interventions. Motivated parents who adopted each of these strategies promoted some positive dietary change among their children, such as decreasing soda availability in the household. Interventions may enhance this positive change through tailored guidance and support. We hypothesise that for certain families it may make more sense to encourage parents to first make the needed changes for themselves and then gradually include children or give them healthier alternatives. Despite the availability to children of less healthy alternative food, families in both of the different food patterns described small changes in the children’s diets over time. Parents focused on specific changes, such as limiting soda pop and cooking everyone’s food with less fat. In addition some also encouraged their children to try the new food. While a potential downside to this approach is the increased burden on the meal preparer, one mother reduced this burden by using the same base items, such as meat, and changing only a portion of the meal for her children.
Other families (e.g. same food/resistance pattern) may require further study as to whether they inadvertently encourage excessive rigidity around food choices. Studies in younger children suggest that this could increase consumption in unrestricted settingsReference Birch, Fisher and Davison25 and decrease ability to self-regulate caloric intakeReference Francis and Birch10, Reference Johnson and Birch26. Furthermore, overly ‘controlling’ parenting has been associated with unhealthy eating among young Latina girlsReference Arredondo, Elder, Ayala, Campbell, Baquero and Duerksen27. A couple of families described children hiding food and sneaking food from the kitchen. It is important to determine the prevalence, frequency and amount of such secretive behaviour among children in these families, whether it improves over time, and how to help parents adjust their strategies both to reduce this behaviour as well as the overall conflict around food. Perhaps strategies adopted from family-based child obesity treatment programmes could help instruct parents in adult lifestyle programmes in the delicate balance between too much restriction and necessary changes to help children eat healthilyReference Edwards, Nicholls, Croker, Van, Viner and Wardle28, Reference Kitzmann and Beech29.
This study also suggests that some families may benefit from learning to prepare appetising healthy meals and from encouragement to keep offering new foods. Consistent with other literature, taste affected children’s reactions to dietary changesReference Story, Neumark-Sztainer and French7. Resisting children complained about the taste of new foods and accepting children emphasised that the food still tasted good. Some children described adapting to and even liking new foods over time. This suggests that some combination of factors such as lack of unhealthy alternatives, availability of healthy foods and parental encouragement over time could lead some children to accept new healthy foods. This is consistent with studiesReference Birch30, Reference Birch, Fisher and Gaull31 showing that young children must try some foods five to 10 times before they will accept it, and older children may need even more exposureReference Skinner, Carruth, Wendy and Ziegler32.
Limitations
Several limitations should be considered when interpreting these results. First, although we believe we reached informational redundancy on this topic, it would have been ideal to interview several more families for confirmation. Unfortunately, we exhausted the pool of eligible families. Second, the descriptions of family diet behaviours are self-reported and subject to social desirability bias. Some children seemed reluctant to criticise their parents’ food choices. On the other hand, many parents candidly described the conflicts about food and their mealtime strategies. Obtaining views from an adult and a child in the same family strengthens the validity of our findings. Third, our typology is primarily based on dietary behaviour where both parent and child are present in the home. It may be less applicable to families who rarely interact around food. Fourth, our findings are based on a small group of African American and Latino families living in inner-city neighbourhoods having a member with type 2 diabetes and thus are most applicable to groups with similar characteristics. In addition, though our sample spanned the spectrum of ages 10–17 years, we had difficulty recruiting the 16–17-year-old group so the breadth of possible responses from this group may not be as well represented. On the other hand, our over-sampling of 12–13-year-olds provided greater breadth and understanding of this group and thus our findings may be particularly applicable to this group. Finally, BMI data were not available on some children. However, children’s reports of either being overweight or trying to lose weight were consistent with the interviewer’s assessments and available BMIs, and perception of being overweight may influence behaviour more than actual weight.
Conclusion
When adults with children attempt dietary changes, family eating patterns may also change. The resulting family patterns highlight the tension between an adult desiring to make dietary changes and children who are not necessarily motivated to make similar changes. Our initial exploration provides a framework from which to hypothesise how these patterns might ultimately influence dietary behaviour in families and implications for designing interventions. Understanding the variation among family responses could help adult-focused interventions and providers tailor their guidance to parents and assist parents in including their children in their dietary change.
Acknowledgements
Sources of funding: This research was support by the Robert Wood Johnson Clinical Scholars Program and by the National Institute of Child Health and Human Development (T32 HD007534 to H.H.L.). M.H. is a VA HSR&D Career Development awardee. REACH Detroit Partnership is funded by the Centers for Disease Control and Prevention (US0/CCU417409). The authors acknowledge the generous support of the REACH Detroit Partnership Steering Committee and staff, CHASS, and the University of Michigan School of Social Work. REACH Detroit is affiliated with the Detroit-Community Academic Urban Research Center. This material is the result of work supported with resources and the use of facilities at the Iowa Veterans Affairs Medical Center. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of interest declaration:The authors have no conflicts of interest to declare.
Authorship responsibilities: H.H.L., J.F., G.P. and M.H. all contributed to the research conceptualisation and design. H.H.L., J.F., M.M.D. and M.H. contributed to the analysis through development of the coding scheme and thematic interpretation of the data. H.H.L. drafted the initial manuscript and all authors critically reviewed, edited and added to the manuscript content. G.P. also assisted in research implementation. In addition, H.H.L. led the research project, conducted interviews and coded interviews.
Acknowledgements: The authors also thank Michael Anderson, family health advocates supervisor, REACH Detroit Partnership, for his help with designing and coordinating recruitment plans; Nancy Shore and Lorena deAnda for their coding of interviews; the REACH family health advocates for their input on recruitment, interview guides and community characteristics; Joel Howell MD for his guidance and manuscript editing; and Keva Anderson and Theresita Lezuch for their help with cultural interpretation.








