There is an ongoing discussion as to the question of which childhood growth references to use for which population. The WHO child growth standard (0–5 years) was designed as a universal norm, because WHO concluded that growth of affluent children between birth and 5 years of age was found to be quite similar on all continents. Despite it being implemented in over 125 countries, including a complementary reference for 5–19-year-olds(
Reference de Onis, Martinez-Costa and Nunez
1
), the universal application of both the standard and the reference for assessing growth of children has been questioned repeatedly, especially its use in Asian populations(
Reference Wang, Moreno and Caballero
2
–
Reference de Wilde, Dekker and Middelkoop
6
).
In this issue of Public Health Nutrition, Sandjaja et al. contribute to the discussion with their South-East Asian Nutrition Surveys (SEANUTS) study of weight and BMI in children from four South-East Asian countries (Malaysia, Thailand, Indonesia and Vietnam). They derived population-specific weight-for-age and BMI-for-age reference values from their pooled data from these four countries. They recommend using these reference values in clinical practice as well as for research and public health applications, as an additional tool to the WHO reference values, and instead of country-specific values(
Reference Sandjaja, Poh and Rojroongwasinkul
7
).
As swapping references may have a profound impact on the detection of children at risk, such a recommendation needs thorough investigation and discussion. Sandjaja et al.’s article is an illustration of the difficult questions we are confronted with in the area of something seemingly as simple as optimal height and weight of children. For several reasons these questions are difficult. First, growth is influenced by genetic, epigenetic, lifestyle and environmental factors, and we do not exactly know the impact of each type of factor on a global scale nor in specific populations. Second, regarding weight and BMI as estimators of fat mass, we know that these quantities do not differentiate between fat and lean body mass. In addition, secular changes in height may represent a third difficulty. However, a disturbing influence of height on BMI reference values is likely limited. Therefore, we do not deal with this subject here.
First, we discuss the problem of using weight or BMI as an estimator of fat mass. It is currently well known that the body composition of Asian people differs from Caucasians. For any given BMI (or weight), Asian populations generally have a larger fat mass together with a smaller muscle mass than Caucasian populations(
Reference Deurenberg, Deurenberg-Yap and Guricci
8
). This is found in all age groups and even at birth; a well-known example is the so-called ‘thin-fat’ Indian baby with low birth weight and high fat mass(
Reference Yajnik, Fall and Coyaji
9
–
Reference Stanfield, Wells and Fewtrell
11
). In Sri Lankan children, even in those considered thin, the fat mass was much higher than in Caucasian children(
Reference Wickramasinghe
12
).
These studies stress the problem of using a single measure of body size (weight or BMI), not differentiating between fat and lean body mass(
Reference Wells
13
). This is especially true when universally applicable growth standards such as those of WHO are used. In several cases, country-specific or national BMI-for-age references were shown to be superior in detecting an excess of body fat compared with universal references and may therefore be more appropriate for use in clinical practice(
Reference Wells
13
,
Reference Reilly, Kelly and Wilson
14
).
We now use our own studies on growth of South Asian children in the Hague, the Netherlands, as an example of the problems one encounters because of the complexity of the factors influencing growth. In our ‘1976 study’ of South Asian children living in the Netherlands, we developed reference values based on data from South Asian children born in 1974–1976, living in affluent circumstances but before the obesity epidemic started. We found a left shift in the ethnic-specific BMI reference, compared with the WHO reference. As a result, many children with underweight according to the WHO reference actually had a normal weight when based on ethnic-specific norms. And at the other end of the BMI spectrum, many children now had overweight, although they had a normal weight according to the universal standard. So, on the one hand, parents might have been wrongly informed to stimulate their child to eat more; and, on the other, parents might have been wrongly reassured that their child had a normal weight. Some years after developing these South Asian-specific reference values, we studied growth in South Asian children 0–19 years of age. In that cross-sectional study, performed in 2007–2010, children with a high BMI were over-represented in 5–19-year-olds, compared with the distribution of the South Asian-specific reference from the ‘1976 study’ and even compared with the WHO reference. Apparently, these results reflected the effects of the obesity epidemic. So, if we would have used a reference based on more recently acquired data, we would have underestimated overweight and obesity prevalence figures in this group(
Reference de Wilde, Dekker and Middelkoop
6
). Actually, our estimation would have been even worse than an estimation based on the universal standard. So, a first conclusion from our studies would be that the requirement of restriction to children growing up in affluence falls short: in addition, the data should have also been gathered in a non-obesogenic environment. A second conclusion, important for many countries, is that national growth references may not be representative of growth in some ethnic minority groups.
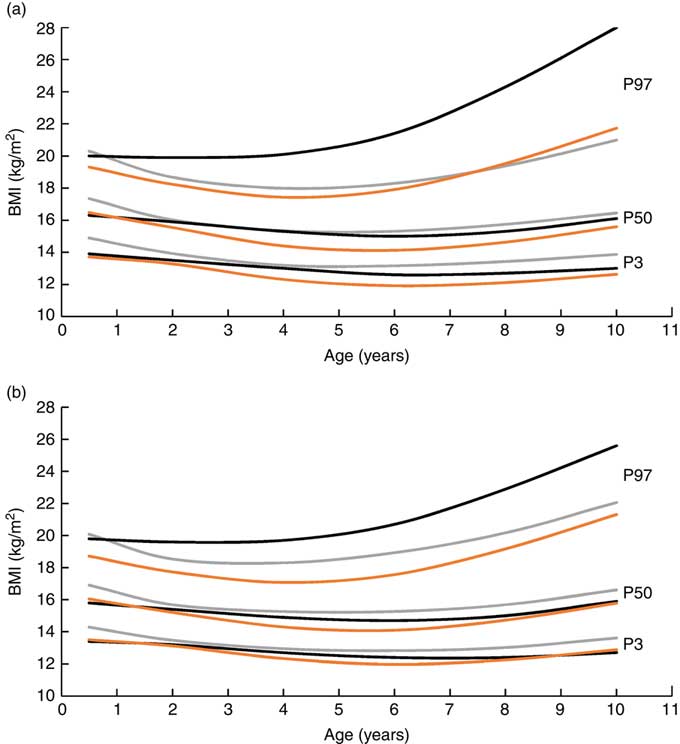
With these results in mind, next we comment on the findings and recommendations of the SEANUTS study. We plotted data from WHO, SEANUTS and our ‘1976 study’ on one graph (Fig. 1). The median BMI values of the pooled SEANUTS data were generally found to be lower than of the WHO reference. Similarly, the 3rd percentile of most sex/age groups was lower. These results suggest the well-known left shift of the BMI distribution in Asian populations, that we also found in South Asian children in the Netherlands(
Reference de Wilde, Dekker and Middelkoop
6
). However, according to the SEANUTS data, from the age of 2 years the 97th percentile was higher, and even much higher at the age of 10 years, compared with the WHO reference. Therefore, the use of a BMI-for-age reference derived from the pooled SEANUTS data would result in a lower overweight and obesity prevalence compared with figures based on the WHO reference. This is an unexpected outcome, as, considering their thin-fat body composition, we would have expected the prevalence based on WHO cut-offs to be lower than that based on ethnic-specific BMI criteria. The considerably higher 97th percentile likely indicates the effects of the obesity epidemic while the lower percentiles are less affected, which is what we also concluded for South Asian children in the Netherlands(
Reference de Wilde, Dekker and Middelkoop
6
). Therefore, the SEANUTS population does not seem to represent a true (normative) reference population, which traditionally is an affluent population unaffected by the obesity epidemic. The recommendation of Sandjaja et al. to use their BMI-for-age reference would therefore potentially have unwanted effects: while the criteria for thinness would be more appropriate, the criteria for overweight and obesity would likely lead to an underestimation of adiposity.
Another intriguing aspect of the SEANUTS study is the relatively large effect of exclusion of Malaysia respectively Indonesia. This raises the question whether the obesity epidemic might have especially affected the children in Malaysia. At the same time, one may wonder if enough children measured in Indonesia met the WHO requirement of affluence, considering the large proportion of children with low educated mothers in Indonesia compared with Malaysia.
The question remains what reference should be used in these countries. Applying references derived from the pooled data of the SEANUTS study would result in a lower overweight and obesity prevalence than applying standards derived from the WHO reference. However, even the WHO reference very likely leads to an underestimation of these prevalence figures, which is confirmed by the high fat mass percentages presented in Table 6 of the SEANUTS study, not only for the group >95th percentile, but also for the group between the 5th and 95th percentile. So, replacing the WHO reference by the proposed SEANUTS reference seems not to be a good idea.
On the one hand, the findings of the SEANUTS study underline the importance of the requirement of affluence when developing reference values. But at the same time, they demonstrate the relevance of the criterion of a non-obesogenic environment. In fact, the study underlines the present problems of deriving normative weight-for-age and BMI-for-age references from measurements of contemporary children.
In conclusion, the SEANUTS study supports the need of considering ethnic-specific growth standards as it shows high body fat percentages already in the normal BMI range, according to the WHO reference. However, it also illustrates the difficulties in assessing ethnic-specific references in populations that either do not yet fulfil the requirement of affluence or, on the contrary, have already been affected by the obesity epidemic.



There is an ongoing discussion as to the question of which childhood growth references to use for which population. The WHO child growth standard (0–5 years) was designed as a universal norm, because WHO concluded that growth of affluent children between birth and 5 years of age was found to be quite similar on all continents. Despite it being implemented in over 125 countries, including a complementary reference for 5–19-year-olds( Reference de Onis, Martinez-Costa and Nunez 1 ), the universal application of both the standard and the reference for assessing growth of children has been questioned repeatedly, especially its use in Asian populations( Reference Wang, Moreno and Caballero 2 – Reference de Wilde, Dekker and Middelkoop 6 ).
In this issue of Public Health Nutrition, Sandjaja et al. contribute to the discussion with their South-East Asian Nutrition Surveys (SEANUTS) study of weight and BMI in children from four South-East Asian countries (Malaysia, Thailand, Indonesia and Vietnam). They derived population-specific weight-for-age and BMI-for-age reference values from their pooled data from these four countries. They recommend using these reference values in clinical practice as well as for research and public health applications, as an additional tool to the WHO reference values, and instead of country-specific values( Reference Sandjaja, Poh and Rojroongwasinkul 7 ).
As swapping references may have a profound impact on the detection of children at risk, such a recommendation needs thorough investigation and discussion. Sandjaja et al.’s article is an illustration of the difficult questions we are confronted with in the area of something seemingly as simple as optimal height and weight of children. For several reasons these questions are difficult. First, growth is influenced by genetic, epigenetic, lifestyle and environmental factors, and we do not exactly know the impact of each type of factor on a global scale nor in specific populations. Second, regarding weight and BMI as estimators of fat mass, we know that these quantities do not differentiate between fat and lean body mass. In addition, secular changes in height may represent a third difficulty. However, a disturbing influence of height on BMI reference values is likely limited. Therefore, we do not deal with this subject here.
First, we discuss the problem of using weight or BMI as an estimator of fat mass. It is currently well known that the body composition of Asian people differs from Caucasians. For any given BMI (or weight), Asian populations generally have a larger fat mass together with a smaller muscle mass than Caucasian populations( Reference Deurenberg, Deurenberg-Yap and Guricci 8 ). This is found in all age groups and even at birth; a well-known example is the so-called ‘thin-fat’ Indian baby with low birth weight and high fat mass( Reference Yajnik, Fall and Coyaji 9 – Reference Stanfield, Wells and Fewtrell 11 ). In Sri Lankan children, even in those considered thin, the fat mass was much higher than in Caucasian children( Reference Wickramasinghe 12 ).
These studies stress the problem of using a single measure of body size (weight or BMI), not differentiating between fat and lean body mass( Reference Wells 13 ). This is especially true when universally applicable growth standards such as those of WHO are used. In several cases, country-specific or national BMI-for-age references were shown to be superior in detecting an excess of body fat compared with universal references and may therefore be more appropriate for use in clinical practice( Reference Wells 13 , Reference Reilly, Kelly and Wilson 14 ).
We now use our own studies on growth of South Asian children in the Hague, the Netherlands, as an example of the problems one encounters because of the complexity of the factors influencing growth. In our ‘1976 study’ of South Asian children living in the Netherlands, we developed reference values based on data from South Asian children born in 1974–1976, living in affluent circumstances but before the obesity epidemic started. We found a left shift in the ethnic-specific BMI reference, compared with the WHO reference. As a result, many children with underweight according to the WHO reference actually had a normal weight when based on ethnic-specific norms. And at the other end of the BMI spectrum, many children now had overweight, although they had a normal weight according to the universal standard. So, on the one hand, parents might have been wrongly informed to stimulate their child to eat more; and, on the other, parents might have been wrongly reassured that their child had a normal weight. Some years after developing these South Asian-specific reference values, we studied growth in South Asian children 0–19 years of age. In that cross-sectional study, performed in 2007–2010, children with a high BMI were over-represented in 5–19-year-olds, compared with the distribution of the South Asian-specific reference from the ‘1976 study’ and even compared with the WHO reference. Apparently, these results reflected the effects of the obesity epidemic. So, if we would have used a reference based on more recently acquired data, we would have underestimated overweight and obesity prevalence figures in this group( Reference de Wilde, Dekker and Middelkoop 6 ). Actually, our estimation would have been even worse than an estimation based on the universal standard. So, a first conclusion from our studies would be that the requirement of restriction to children growing up in affluence falls short: in addition, the data should have also been gathered in a non-obesogenic environment. A second conclusion, important for many countries, is that national growth references may not be representative of growth in some ethnic minority groups.
With these results in mind, next we comment on the findings and recommendations of the SEANUTS study. We plotted data from WHO, SEANUTS and our ‘1976 study’ on one graph (Fig. 1). The median BMI values of the pooled SEANUTS data were generally found to be lower than of the WHO reference. Similarly, the 3rd percentile of most sex/age groups was lower. These results suggest the well-known left shift of the BMI distribution in Asian populations, that we also found in South Asian children in the Netherlands( Reference de Wilde, Dekker and Middelkoop 6 ). However, according to the SEANUTS data, from the age of 2 years the 97th percentile was higher, and even much higher at the age of 10 years, compared with the WHO reference. Therefore, the use of a BMI-for-age reference derived from the pooled SEANUTS data would result in a lower overweight and obesity prevalence compared with figures based on the WHO reference. This is an unexpected outcome, as, considering their thin-fat body composition, we would have expected the prevalence based on WHO cut-offs to be lower than that based on ethnic-specific BMI criteria. The considerably higher 97th percentile likely indicates the effects of the obesity epidemic while the lower percentiles are less affected, which is what we also concluded for South Asian children in the Netherlands( Reference de Wilde, Dekker and Middelkoop 6 ). Therefore, the SEANUTS population does not seem to represent a true (normative) reference population, which traditionally is an affluent population unaffected by the obesity epidemic. The recommendation of Sandjaja et al. to use their BMI-for-age reference would therefore potentially have unwanted effects: while the criteria for thinness would be more appropriate, the criteria for overweight and obesity would likely lead to an underestimation of adiposity.
Fig. 1 BMI-for-age percentiles for boys (a) and girls (b), according to WHO( Reference de Onis, Martinez-Costa and Nunez 1 ) ( ), SEANUTS(
Reference Sandjaja, Poh and Rojroongwasinkul
7
) (
), SEANUTS(
Reference Sandjaja, Poh and Rojroongwasinkul
7
) ( ) and the ‘1976 study’(
Reference de Wilde, Dekker and Middelkoop
6
) (
) and the ‘1976 study’(
Reference de Wilde, Dekker and Middelkoop
6
) ( ). SEANUTS, South-East Asian Nutrition Surveys; P3, 3rd percentile; P50, median; P97, 97th percentile
). SEANUTS, South-East Asian Nutrition Surveys; P3, 3rd percentile; P50, median; P97, 97th percentile
Another intriguing aspect of the SEANUTS study is the relatively large effect of exclusion of Malaysia respectively Indonesia. This raises the question whether the obesity epidemic might have especially affected the children in Malaysia. At the same time, one may wonder if enough children measured in Indonesia met the WHO requirement of affluence, considering the large proportion of children with low educated mothers in Indonesia compared with Malaysia.
The question remains what reference should be used in these countries. Applying references derived from the pooled data of the SEANUTS study would result in a lower overweight and obesity prevalence than applying standards derived from the WHO reference. However, even the WHO reference very likely leads to an underestimation of these prevalence figures, which is confirmed by the high fat mass percentages presented in Table 6 of the SEANUTS study, not only for the group >95th percentile, but also for the group between the 5th and 95th percentile. So, replacing the WHO reference by the proposed SEANUTS reference seems not to be a good idea.
On the one hand, the findings of the SEANUTS study underline the importance of the requirement of affluence when developing reference values. But at the same time, they demonstrate the relevance of the criterion of a non-obesogenic environment. In fact, the study underlines the present problems of deriving normative weight-for-age and BMI-for-age references from measurements of contemporary children.
In conclusion, the SEANUTS study supports the need of considering ethnic-specific growth standards as it shows high body fat percentages already in the normal BMI range, according to the WHO reference. However, it also illustrates the difficulties in assessing ethnic-specific references in populations that either do not yet fulfil the requirement of affluence or, on the contrary, have already been affected by the obesity epidemic.
Acknowledgments
Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: B.J.C.M. wrote the first draft of the commentary. J.A.d.W. commented on and added to the draft and produced the figure. Ethics of human subject participation: Not applicable.