Adversity experienced early in childhood can create deep psychological and neurobiological vulnerabilities. Reference Teicher and Samson1 In this regard, institutional care settings pose rather particular risks and have distinctive effects on development. Reference Kumsta, Kreppner, Kennedy, Knights, Rutter and Sonuga-Barke2 In such settings there may be limited personalised care, restricting the chance for children to develop close, stable and loving relationships with individual carers. Reference Rutter3 There may also be a lack of linguistic and intellectual stimulation. Reference Castle, Groothues, Bredenkamp, Beckett, O'Connor and Rutter4 In more extreme cases, nutrition and hygiene are compromised. Reference Rutter3 The effects of these institutional exposures can be seen in subsequent elevated rates of neurodevelopmental disorders and mental health problems – with more severe institutional deprivation associated with worse outcomes persisting into adulthood. Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 Some of the difficulties observed in individuals who have been previously institutionalised represent deprivation-related variants of more general, common childhood problems, such as attention-deficit hyperactivity disorder (ADHD), Reference Kennedy, Kreppner, Knights, Kumsta, Maughan and Golm6 autism spectrum disorder (ASD) Reference Kumsta, Kreppner, Rutter, Beckett, Castle and Stevens7 and behavioural and emotional problems. Reference Sonuga-Barke, Schlotz and Kreppner8 In contrast, disinhibited social engagement (DSE, as defined in DSM-5 9 ) is a diagnosis restricted to individuals who have experienced institutional deprivation or other forms of gross early social neglect. It presents as an inappropriate over-familiarity with, and lack of wariness of, strangers, and a failure to observe appropriate physical and verbal boundaries during social interaction. For example, it can involve an inappropriate seeking out of physical proximity and/or asking overly intrusive and overly familiar questions. Reference Zeanah and Gleason10,Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11 Within the social ecology of poor-quality care in institutions, DSE behaviours may be adaptive – they may fulfil a need for social intimacy and increase access to care from staff. Reference Minnis, Fleming and Cooper12 However, post-institutionally they represent a potential source of vulnerability and impairment. Reference Zeanah and Gleason13 Individuals with DSE may be perceived by peers as tiresome and/or hostile, and the indiscriminate nature of their social behaviours may undermine friendship development. Reference Lyons-Ruth, Bureau, Riley and Atlas-Corbett14 Their overly trusting nature may increase risk of exploitation within dysfunctional relationships. Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11
DSE is considered a condition of early childhood and although recent evidence suggests that DSE can persist into later childhood and adolescence, Reference Humphreys, Nelson, Fox and Zeanah15–Reference Kreppner, Kumsta, Rutter, Beckett, Castle and Stevens18 little is known about its long-term persistence into adulthood. Reference Rutter, Sonuga-Barke, Beckett, Castle, Kreppner and Kumsta19 To address this point, we have recently reported childhood-to-adult developmental trajectories for DSE behaviours in the English and Romanian Adoptees (ERA) study cohort Reference Rutter and Sonuga-Barke20 of individuals who experienced extreme early deprivation in the institutions of the latter years of the Ceauşescu regime, before adoption into UK families. Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 Perhaps against expectation, DSE behaviours showed strong persistence into adulthood alongside more expected persistence of ASD and inattention/overactivity (representing a subset of symptoms of ADHD) symptoms – 35% of young adult adoptees who experienced deprivation for longer than the first 6 months of life displayed evidence of DSE behaviours compared with 6% in a comparison group of UK adoptees. In the current paper, we extend this initial analysis of the persistence of DSE behaviours. Our aim is to address the following questions. What are the characteristic features of the young adult DSE presentation in individuals who have experienced early deprivation? Can DSE behaviours still be directly observed? To what extent are affected adults aware of their own DSE behaviours? Do DSE behaviours overlap with continuing neurodevelopmental disorders? Does young adult DSE have an impact on social functioning, mental health, service use and quality of life (QoL)? Given prior findings we predicted that DSE behaviours would persist into adulthood but be less observable than at younger ages and affected individuals would show some awareness of their own tendency towards DSE. We also predicted that DSE behaviours would be associated with impaired social functioning and reduced QoL.
We were also interested in exploring the relationship between DSE behaviours and parent–child relationships – especially their link with attachment security in adulthood. This is of interest because the DSE pattern was initially conceptualised in terms of attachment. However, against this view, DSE has since been shown to persist even after the formation of secure attachment relationships. Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11 Our own earlier data suggest that the core of the DSE pattern is linked to unmodulated and indiscriminate social behaviours with relative strangers rather than a lack of selectivity of attachment behaviours with regard to carers. At age 6, for instance, there was only a weak negative association between DSE and attachment security; 53% of those displaying DSE were coded as secure compared with 79% of those without the DSE pattern. Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11 As a result of this Rutter et al Reference Rutter, Kreppner and Sonuga-Barke21 concluded that the DSE pattern should not be conceptualised as an attachment disorder – a view consistent with the work of Zeanah and colleagues, Reference Zeanah and Gleason10 and the eventual designation of DSE as a separate disorder in DSM-5. 9
Method
Participants
In total, 165 Romanian (91 females) and 52 UK adoptees (18 females – no deprivation history) and their adoptive families entered the study in the mid-1990s. In the UK group, data were available for 47 (90%) and 39 (75%) individuals in adolescence and in young adulthood respectively. In the Romanian group these figures were 148 (90%) and 107 (65%) individuals respectively. The average age at young adult assessment was 23.2 (UK) and 23.6 years (Romanian). A comparison of age 15 characteristics of those that dropped out in young adulthood and those that remained in the study provided no evidence of selective attrition. The proportion of UK and Romanian individuals was similar at the two ages and there was no difference between those remaining in the study at the young adult follow-up and those dropping out in terms of gender of child, age, IQ or the proportion with deprivation-related problems at age 15 years (data available from authors on request). A total of 18.4% of the retained sample met the criteria for DSE whereas 21.6% of those who dropped out did. This difference was non-significant (P = 0.648).
Measures
DSE
The assessment of DSE behaviours was based on interviewers' ratings of parents' answers based on three codes used at previous assessment waves. Reference Kumsta, Kreppner, Rutter, Beckett, Castle and Stevens7,Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11,Reference Kreppner, Kumsta, Rutter, Beckett, Castle and Stevens18 These were: (a) too friendly with strangers or too eager to approach strangers; (b) makes very personal comments or asked intrusive questions of others they have just met; and (c) unaware of social boundaries, or the closeness of interaction with unfamiliar people. Two additional questions were included in the young adult assessment: (d) excessive self-disclosure and (e) not stranger-aware. A rating between 0 and 2 was made – with 0 representing ‘no evidence of disinhibition’ and 2 ‘definite evidence of disinhibition’. Interrater agreement in adulthood was high, with a mean intraclass correlation of 0.91 (range 0.81–0.97). Interviewers masked to prior DSE status also directly observed the adoptees' behaviour during their assessment visit for evidence of the following: (a) social disinhibition, (b) inappropriate physical contact, (c) inappropriate/intrusive comments, (d) violation of physical social boundaries and (e) violation of verbal social boundaries. Ratings were made using the same coding scheme as for the parent-based ratings.
Self-awareness of their DSE behaviours by young adults was assessed using specific DSE items from the Social Emotional Functioning Interview. Reference Rutter, LeCouteur, Lord, Macdonald, Rios, Folstein, Schopler and Mesibov22 These items were: general social disinhibition with others; a lack of the concept of friendship; an inability to differentiate between friends and non-friends; a lack of awareness of any problems with peers/others; and a lack of the concept of loneliness. Items were rated on a three-point scale (0–2) with the higher rating reflecting definite difficulty. Difficulties were deemed present when any item was positively endorsed at the level of 1 or 2 (i.e. some or definite). Given the non-specific nature of social difficulties, this scale had reasonable internal consistency (α = 0.58). This scale also had high interrater reliability between two raters on a randomly selected 20% subsample, with an average kappa of 0.890 (range 0.71–1). Further information on individual items used available on request from the authors.
Co-occurring young adult developmental and mental health problems
ADHD, conduct and mood problems. ADHD (18 items), generalised anxiety (13 items), major depression (15 items) and conduct disorder (14 items) symptoms were assessed using the Conners Behaviour Rating Scales (CBRS) using standardised T-scores. Reference Conners, Pitkanen and Rzepa23 ADHD assessment was based on parent report whereas the other outcomes were based on self-report, in line with established guidelines. 24 Callous–unemotional traits were measured using the parent report Inventory of Callous-Unemotional traits (ICU), Reference Essau, Sasagawa and Frick25 which measures the affective personality features of psychopathy. It contains 24 items assessed on a 0- to 3-point rating scale with higher scores reflecting increased levels of callous-unemotional traits. The ICU had good internal consistency (α = 0.90).
ASD. The Social Communication Questionnaire (SCQ) Reference Rutter, Bailey and Lord26 is a parent-completed and clinically validated 35-item screen for ASD symptoms that maps onto DSM diagnostic criteria. To ensure its developmental appropriateness in young adulthood our analysis was based on a 15-item version with five items from each scale (social reciprocal interaction; communication and repetitive and stereotyped behaviours). Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 Items were rated as either 0 for ‘No’ or 1 for ‘Yes’. This revised 15-item scale demonstrated high reliability (α = 0.88).
IQ. A shortened version of the Wechsler Abbreviated Scale of Intelligence (WASI, two-subscale (vocabulary and block design) version) Reference Wechsler27 was administered in early adulthood.
Clinical service use
Information about lifetime history of clinical service use was gathered from parents and young people during interviews at ages 6, 11 and 15 years and during the young adult follow-up.
Young adult-parent attachment security
Young adults' attachment was measured using the Parental Attachment Questionnaire (PAQ) Reference Kenny28 and the Inventory of Parent and Peer Attachment (IPPA) Reference Armsden and Greenberg29 – validated in this age group. Reference Kenny and Sirin30 PAQ has three subscales: affective quality (27 items), facilitation of independence (14 items) and support (13 items), with items rated on a scale of 1 to 5. In the present sample, scale reliability was high for each subscale (α = 0.96, 0.90 and 0.85 respectively). IPPA is a 25-item measure of mother–and father–child attachment. Items are rated on a scale of 1 to 5, with higher scores indicating greater attachment security. Both mother and father attachment subscales showed high scale reliability in this sample (α = 0.97 and 0.96 respectively).
QoL
Participants self-rated QoL using the five-item Satisfaction with Life Scale Reference Diener, Emmons, Larsen and Griffin31 (1, strongly disagree to 5, strongly agree). They reported whether they (a) see their current life as ideal; (b) are satisfied with life; (c) would live life again in the same way; (d) find life excellent and; (d) think they have secured the important things in life. This scale had high internal consistency (α = 0.90).
Functioning within different social domains
Social functioning was assessed with the work, romantic relationships, friendships, non-specific social contacts and coping subscales of the Revised Adult Personality Functioning Assessment (RAPFA), Reference Hill, Pilkonis, Morse, Feske, Reynolds and Hope32 each on a scale of 1–9 – where a score of 3 or more represents the presence of dysfunction. Reference Mackie, Hill, Kondryn and McNally33 Interrater reliability was high, with intraclass correlations ranging from 0.78 to 0.96, based on a randomly selected 20% of the whole sample. Participants were grouped as 0 for ‘no significant dysfunction’ or 1 for ‘evidence of significant dysfunction’.
Education and employment status
Key indicators of young adult functioning were derived from young adult and parent reports. These were (a) currently being unemployed and (b) having lower educational achievement (i.e. GCSEs or less). These were coded in a binary form (0, does not apply; 1, applies).
Adoptive family demographics
Adoptive family socioeconomic status (SES) was based on data on parents' occupation at the age 15 follow-up. Reference Rutter and Sonuga-Barke20 Families were divided into high and low SES groups based on the Registrar General's classification. Reference General34 Manual and unskilled occupations were classified as low SES and skilled, managerial/technical and professional occupations as high SES. Parental marital status was derived from parental reports made at young adult follow-up to create a binary code (marriage intact, 1; original adoptive parents divorced, separated or widowed, 0).
Statistical analysis
First, we used correlational analysis to examine the structure of parent-rated young adult DSE. Second, we used χ2 and Fisher's exact tests to examine the relationship between deprivation and DSE. As in previous papers we divided the Romanian adoptees into two groups – those who had experienced less than 6 months of deprivation (Rom < 6 group) and those who experienced between 6 and 43 months deprivation (Rom > 6 group). This was based on evidence for a step increase in risk between 6 and 12 months of deprivation exposure and the finding of equally low risk of problems in the UK and the Rom < 6 groups. Reference Kreppner, Rutter, Beckett, Castle, Colvert and Groothues35 These groups were compared in terms of the proportion of individuals with a score of 1 (probable DSE) for each of the five parent-rated items. Third, we estimated the proportion of individuals meeting criteria for DSE based on interviewer coding of parent interviews using thresholds equivalent to those used in previous studies. Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11 More specifically, DSE was deemed present if an individual had two or more positive endorsements (a score of either 1 or 2) from the five items. These proportions were then compared across the three groups. Fourth, we split the Rom > 6 group into those with and without DSE (DSE+ v. DSE−) and then validated this DSE categorisation against (a) interviewer observations and (b) self-ratings. For these measures, separate binary outcomes were created so that those with no self-reported or observed disinhibition could be compared with those with at least one positive item. Fifth, we examined patterns of continuity between adolescence and young adulthood using McNemar's statistical test, which compared the proportion of individuals meeting threshold at our two time points. Sixth, using the same group comparison we examined patterns of co-occurring neurodevelopmental, mental health problems and clinical service use as well as QoL, functioning within different social domains, employment and educational status. Seventh, where the above analysis revealed significant differences between DSE+ and DSE− groups we ran a series of multiple logistic regression analyses with other deprivation-specific problems (ADHD, ASD), callous–unemotional traits and IQ entered as covariates to assess the extent to which poor outcomes were specific to DSE.
Results
The five parent-reported adult DSE items were significantly inter-correlated (Spearman's rs = 0.39 to 0.83) creating a single scale with high internal consistency (α = 0.82). Figure 1 presents the proportion of positive DSE-item endorsements for young adults within the UK, Rom < 6 and Rom > 6 groups. Adult DSE behaviours were strongly related to levels of prior deprivation. There were equally low rates in the UK and Rom < 6 groups (χ2(1) = 0.07, P = 0.79), but they were significantly greater in the Rom > 6 group compared with the Rom < 6 group (χ2(1) = 11.8, P = 0.001). Individuals in the Rom > 6 group were seven and six times more likely to meet our thresholds than those in either the UK (χ2(1) = 11.8, P = 0.001) or the Rom < 6 group respectively (χ2(1) = 12.1, P = 0.001). Furthermore, there was significant persistence of DSE behaviours, with 64% of those in the Rom > 6 group meeting criteria for DSE at 15 also meeting criteria in young adulthood (McNemar, P = 0.79).
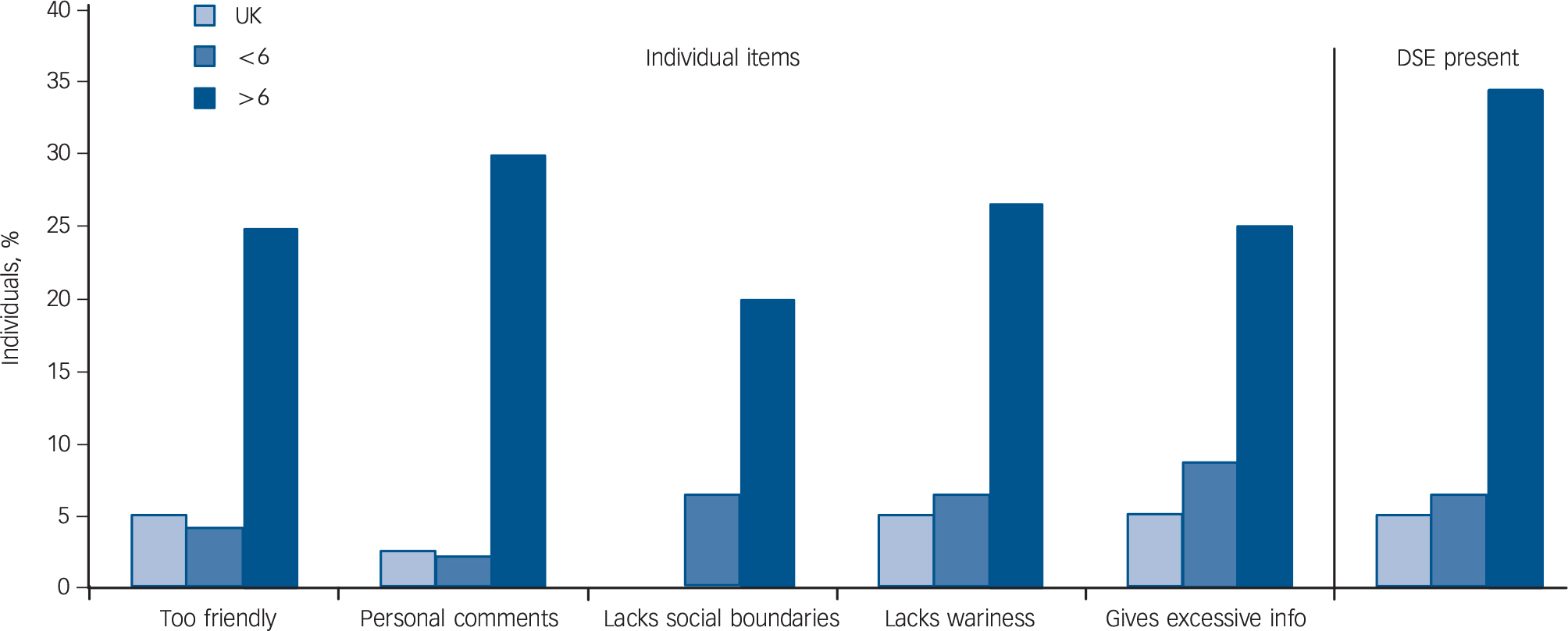
Fig. 1 The proportion of individuals in each group scoring positively for each disinhibited social engagement (DSE) trait (on left) and the proportion of individuals who met criteria for the presence of DSE overall as coded by the interviewer based on parental descriptions (on right).
UK, UK adoptees; < 6, Romanian adoptees with less than 6 month of deprivation; > 6, Romanian adoptees with more than 6 month of deprivation.
Given the similarity in terms of low parent-derived DSE levels in the UK and Rom < 6 groups we then tested whether these groups differed in terms of self-rated and observed DSE behaviours: there were no significant differences (P = 0.054 and P = 0.34 respectively). The UK and Rom < 6 groups were therefore combined for subsequent analyses into a low deprivation group (LoDep group). This group was then compared with the Rom > 6 group divided into DSE+ v. DSE− groups. Figure 2 compares these three groups in terms of observed and self-rated DSE behaviours. The Rom > 6 group DSE+ had significantly higher levels of any self-rated (46.7% v. 4.9%; Fisher's Exact, P < 0.001) and observed DSE (41.2% v. 1.2%, Fisher's Exact, P < 0.001).
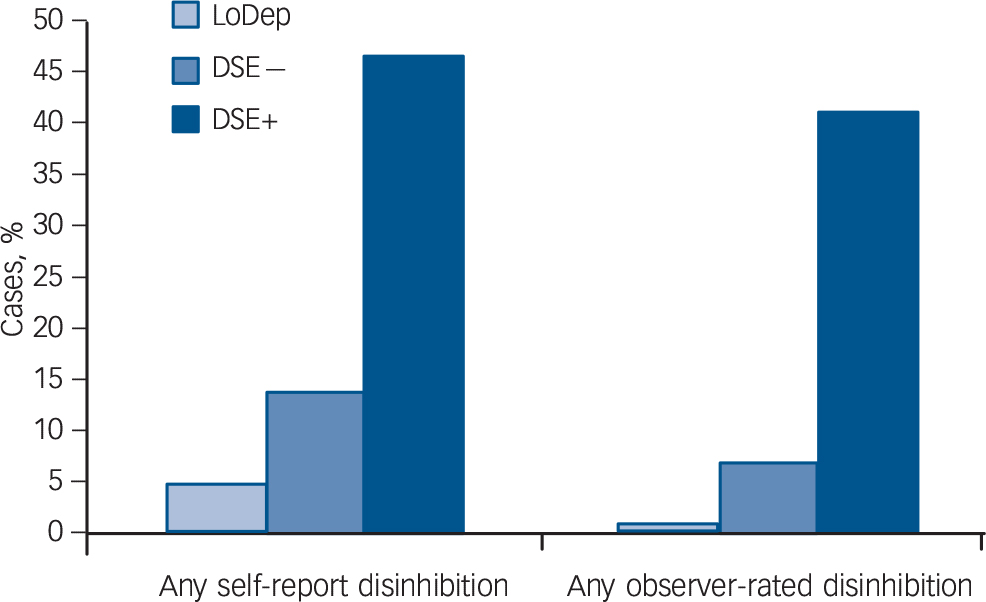
Fig. 2 The proportion of individuals with and without disinhibited social engagement (DSE) who met criteria for self-reported and observed social disinhibtion.
LoDep, combined UK adoptees with Romanian adoptees with less than 6 months of deprivation. DSE−, Romanian adoptees with more than 6 months of deprivation not meeting DSE criteria; DSE+, Romanian adoptees with more than 6 months of deprivation meeting DSE criteria
Table 1 presents group differences in family demographics and levels of young adult co-occurring neurodevelopmental problems, mental health symptoms, clinical service use, educational attainment, employment status, functioning within different social domains and QoL. There was no difference between the DSE− and DSE+ groups in terms of gender, SES or the intactness of the adoptive family. Levels of ASD and ADHD symptoms and callous-unemotional traits and clinical service use were significantly greater in the Rom > 6 DSE+ group than either the LoDep or the Rom > 6 DSE− group. The same pattern was seen for clinical service use, lower educational attainment and unemployment. DSE+ and DSE− did not differ in terms of anxiety, depression or IQ. The groups did not differ in terms of QoL or RAPFA measures of functioning within any social domains.
Table 1 Demographic characteristics and clinical outcomes

| Rom > 6 group | Group contrasts | |||||
|---|---|---|---|---|---|---|
| LoDep (n = 92) | DSE− (n = 51) | DSE+ (n = 21) | LoDep v. DSE− | LoDep v. DSE+ | DSE− v. DSE+ | |
| Female, n (%) | 43 (46.7) | 24 (47.1) | 15 (71.4) | χ2 (1) = 0.00 P = 0.971 |
χ2 (1) = 4.17 P = 0.041 |
χ2 (1) = 3.56 P = 0.059 |
| Low socioeconomic status, a n (%) | 11 (12.2) | 5 (10.4) | 4 (21.1) | χ2 (1) = 0.10 P = 0.752 |
χ2 (1) = 1.03 P = 0.310 |
χ2 (1) = 1.32 P = 0.250 |
| Intact families, n (%) | 71 (78.0) | 30 (75.0) | 13 (61.9) | χ2 (1) = 0.14 P = 0.705 |
χ2 (1) = 2.36 P = 0.124 |
χ2 (1) = 1.14 P = 0.287 |
| Neurodevelopmental problems, mean (s.d.) | ||||||
| ADHD symptoms b | 50.47 (10.57) | 56.24 (14.39) | 73.55 (12.18) |
t(57.96) = −2.24 P = 0.029 |
t(102) = −8.67 P = 0.001 |
t(58) = −4.68 P = 0.021 |
| ASD symptoms c | 0.93 (2.12) | 1.73 (2.76) | 3.98 (3.36) |
t(120) = −1.77 P = 0.79 |
t(22.77) = −3.87 P = <0.001 |
t(57) = −2.74 P = 0.008 |
| IQ | 102.68 (16.10) | 96.36 (11.03) | 91.00 (14.21) |
t(95.72) = 2.43 P = 0.79 |
t(90) = 2.62 P = 0.017 |
t(49) = 1.45 P = 0.153 |
| Callous-unemotional traits d | 19.59 (10.43) | 21.41 (11.99) | 32.84 (13.22) |
t(118) = −0.85 P = 0.79 |
t(100) = −4.83 P <0.001 |
t(56) = −3.33 P = 0.002 |
| Mental health in early adulthood, mean (s.d.) | ||||||
| Depression b | 54.29 (13.96) | 58.22 (12.03) | 63.31 (18.22) |
t(106) = −1.44 P = 0.152 |
t(19.10) = −1.86 P = 0.078 |
t(21.03) = −1.02 P = 0.318 |
| Anxiety b | 54.15 (13.63) | 58.50 (11.44) | 62.69 (16.67) |
t(107) = −1.55 P = 0.102 |
t(87) = −2.18 P = 0.032 |
t(21.53) = −0.92 P = 0.371 |
| Conduct disorder b | 46.38 (10.78) | 47.25 (9.33) | 53.31 (16.54) |
t(106) = −0.42 P = 0.679 |
t(17.93) = −1.60 P = 0.126 |
t(19.38) = −1.37 P = 0.186 |
| Clinical service use, young adulthood: n (%) |
15 (16.7) | 12 (30.8) | 13 (68.4) | χ2 (1) = 3.27 P = 0.071 |
χ2 (1) = 22.01 P <0.011 |
χ2 (1) = 7.39 P = 0.007 |
| Young adult functioning, quality of life: e mean (s.d.) |
16.92 (5.38) | 16.47 (6.21) | 16.87 (3.96) |
t(102) = −0.37 P = 0.710 |
t(85) = 0.03 P = 0.973 |
t(40.52) = −0.27 P = 0.792 |
| RAPFA – social domain dysfunction, n (%) | ||||||
| Work | 23 (28.4) | 24 (55.8) | 11 (68.8) | χ2 (1) = 8.97 P = 0.003 |
χ2 (1) = 9.56 P = 0.002 |
χ2 (1) = 0.81 P = 0.369 |
| Romantic relationships | 37 (46.3) | 27 (64.3) | 12 (80.0) | χ2 (1) = 3.59 P = 0.058 |
χ2 (1) = 5.76 P = 0.116 |
χ2 (1) = 1.26 P = 0.261 |
| Friendships | 20 (24.7) | 24 (55.8) | 10 (62.5) | χ2 (1) = 11.89 P = 0.001 |
χ2 (1) = 8.94 P = 0.003 |
χ2 (1) = 0.21 P = 0.644 |
| Non-specific social contacts | 11 (13.6) | 10 (23.3) | 7 (43.8) | χ2 (1) = 1.87 P = 0.172 |
χ2 (1) = 8.05 P = 0.005 |
χ2 (1) = 2.39 P = 0.122 |
| Coping | 18 (23.1) | 17 (40.5) | 8 (53.3) | χ2 (1) = 4.00 P = 0.045 |
χ2 (1) = 5.72 P = 0.017 |
χ2 (1) = 0.74 P = 0.389 |
| Unemployed | 11 (12.0) | 12 (23.5) | 14 (66.7) | χ2 (1) = 2.26 P = 0.071 |
χ2 (1) = 29.70 P <0.001 |
χ2 (1) = 12.00 P = 0.001 |
| Low education (GCSE or less) | 24 (26.4) | 15 (29.4) | 14 (66.7) | χ2 (1) = 0.15 P = 0.700 |
χ2 (1) = 12.36 P <0.001 |
χ2 (1) = 8.58 P = 0.003 |
| Attachment security, mean (s.d.) | ||||||
| IPPA mother | 98.26 (19.06) | 95.98 (27.29) | 93.11 (23.48) |
t(43.36) = 0.43 P = 0.672 |
t(83) = 0.91 P = 0.366 |
t(45) = 0.35 P = 0.727 |
| IPPA father | 96.71 (20.32) | 99.96 (21.79) | 94.62 (18.36) |
t(96) = −0.72 P = 0.473 |
t(77) = 0.33 P = 0.741 |
t(41) = 0.75 P = 0.457 |
| PAQ affective quality | 108.38 (19.72) | 103.85 (26.67) | 101.15 (26.72) |
t(50.89) = 0.88 P = 0.382 |
t(84) = 1.21 P = 0.230 |
t(47) = 0.33 P = 0.746 |
| PAQ facilitators of independence | 51.52 (11.08) | 51.84 (14.19) | 48.22 (12.53) |
t(96) = −0.13 P = 0.899 |
t(84) = 1.03 P = 0.308 |
t(47) = 0.85 P = 0.398 |
| PAQ source of support | 45.32 (9.49) | 44.07 (11.31) | 43.67 (9.51) |
t(103) = 0.59 P = 0.557 |
t(84) = 0.61 P = 0.543 |
t(47) = 0.12 P = 0.904 |
LoDep, combined UK adoptees with Romanian adoptees with less than 6 months of deprivation. DSE−, Romanian adoptees with > 6 months of deprivation individuals not meeting DSE criteria; DSE+, Romanian adoptees with more than 6 months of deprivation meeting DSE criteria; ADHD, attention-deficit hyperactivity disorder; ASD, autism spectrum disorder; RAPFA, Revised Adult Personality Functioning Assessment; IPPA, Inventory of Parent and Peer Attachment; PAQ, Parental Attachment Questionnaire.
a. Based on family occupational status at age 15.
b. Self-rated Conners Behaviour Rating Scales T-score.
c. Parent-rated Social Communication Questionnaire.
d. Parent-rated.
e. Self-rated Satisfaction with Life Scale score.
Note: n's may not sum due to missing data. where degrees of freedom have decimal places, corrected values have been used to account for unequal variances.
Multiple logistic regression analyses, with service use, educational attainment and unemployment as dependent variables showed that associations of DSE with service use (Exp(B) = 1.52, P = 0.64), low educational attainment (Exp(B) = 2.55, P = 0.31) or unemployment (Exp(B) = 1.03, P = 0.97) all dropped to non-significant levels when ASD and ADHD symptoms, callous-unemotional traits and IQ were added as predictors alongside DSE. Interestingly, the effects relating to service use were driven by the specific association with co-occurring ADHD symptoms (Exp(B) = 1.14, P = 0.011). For employment, IQ drove the association (Exp(B) = 0.91, P = 0.019). ADHD symptoms and IQ accounted jointly for educational performance; (ADHD: Exp(B) = 1.10, P = 0.035; IQ: Exp(B) = 0.92, P = 0.044). Finally, DSE was not related to adult attachment security, whether measured via the IPPA or the PAQ (Ps > 0.05; see Table 1).
Discussion
Main findings
The term DSE has been used to describe an inappropriate, overfamiliar and socially intrusive pattern of behaviour displayed by children who have experienced early social adversity – especially neglect. Reference Kay, Green and Sharma36 Past research has shown DSE to be at the core of a pattern of deprivation-specific problems observed in children and adolescents who have experienced institutional deprivation including those in the ERA study. Reference Kumsta, Kreppner, Rutter, Beckett, Castle and Stevens7 In such individuals we recently reported the persistence of DSE behaviours into adulthood alongside ADHD and ASD symptoms. Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 Here we present the first detailed characterisation of deprivation-related DSE behaviours in adulthood. There were a number of findings of note.
First, each of the five parent-reported young adult DSE descriptions were similarly elevated in individuals who experienced more than 6 months of deprivation – including the new items ‘lack of stranger wariness’ and ‘excessive self-disclosure’ – items that extend the DSE construct in potentially important ways. In particular, an overtrusting nature and willingness to divulge private and confidential information could increase the risk of abuse and exploitation.
Second, high DSE status, established by pooling across interviewer-codings of parent-derived information, was corroborated by investigator-based observations and self-ratings by the young adults themselves. This provided external validation of the young adult DSE construct. This is important because it is possible that parental descriptions could be conditioned by the child's history of DSE behaviours rather than reflecting the current situation. The fact that specific DSE behaviours could be observed during a short interview session is quite striking given the expectation for social conformity in such situations. Noteworthy here is that none of the interviewers of young adults had visited participants in the past phases of the project. The evidence that individuals with DSE had insight into their own gregarious nature and open social interpersonal style is also potentially important – because self-knowledge can represent a necessary, although not sufficient, condition for the development of coping and defensive strategies that can reduce social risks.
Third, DSE behaviours still strongly overlapped with the two other core deprivation-specific problems features (ASD and ADHD symptoms), providing further evidence for the idea of a loosely configured deprivation syndrome as previously proposed by Rutter et al Reference Rutter, Sonuga-Barke, Beckett, Castle, Kreppner and Kumsta19 The fourth element of the original deprivation-specific problems cluster, cognitive impairment, was more weakly related to DSE than in the previous follow-up assessments – largely because in general individuals in the Rom > 6 group displayed cognitive recovery by young adulthood with IQs in the normal range even for the most deprived. Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 We also provide the first evidence that adult DSE behaviours overlap to a degree with callous-unemotional traits. Callous–unemotional traits were examined in the sample for the first time at the adolescent follow-up. We have recently reported that callous–unemotional traits are also linked to ADHD in young adults who were exposed to early deprivation. Reference Kennedy, Kreppner, Knights, Kumsta, Maughan and Golm6 These data together raise the possibility that callous–unemotional traits might be a core feature of a deprivation syndrome alongside ADHD, ASD and DSE – at least in adulthood.
Fourth, and perhaps most strikingly, adult DSE behaviours appeared to be largely clinically benign. They were unrelated to both the development of anxiety and depression, despite the increase in these aspects of mental health problems observed between adolescence and early adulthood more generally Reference Sonuga-Barke, Kennedy, Kreppner, Knights, Kumsta and Maughan5 and appeared not to have a significant impact on either functioning within different social domains or QoL – at least as perceived by the young adults themselves. Where there were effects (on educational and employment status) it appeared that these were due to co-occurring neurodevelopmental problems (particularly ADHD symptoms and low IQ), rather than to DSE itself. This lack of an association with impairment casts doubt on whether, at least in adulthood, DSE on its own should be considered a disorder as characterised in the DSM-5 revisions. It is even possible that certain features of disinhibited social behaviours may be beneficial in certain settings and occupations. Indeed, in discussion with the young adults with DSE it became clear that some of them had found a successful niche in jobs in for instance sales that exploited their ‘natural’ openness and friendliness. Despite these specific examples, there was no suggestion in our current analysis that DSE had an overall positively protective quality in the face of co-occurring problems. There is one important caveat to the conclusion that DSE is benign – in our previous work, we have proposed that it is in combination with other deprivation-specific problems, especially ASD, that DSE becomes especially impairing. This question will be explored in future papers.
Finally, DSE was unrelated to both young adults' own and their adoptive parents' perceptions of attachment security. This is significant because initially DSE was cast clinically as an attachment disorder with its origins in the absence of appropriate attachment figures in institutions leading to later disrupted attachment behaviours. Reference Lyons-Ruth37 However, our data in the past suggested that the association between attachment security/insecurity and the DSE pattern was not so clear-cut. Reference Kreppner, Kumsta, Rutter, Beckett, Castle and Stevens18,Reference Rutter, Kreppner and Sonuga-Barke21,Reference Kreppner, Rutter, Marvin, O'Connor and Sonuga-Barke38 Specifically, over time, it became apparent that individuals with DSE were often also securely attached – although a somewhat lower proportion of children with DSE, compared with those without DSE, were rated as secure. Reference Rutter, Colvert, Kreppner, Beckett, Castle and Groothues11 To date, it is unclear whether persistence in DSE into young adulthood would have a negative impact on parent-child attachment relationships. Our data suggest that there were no differences between those with DSE and those without it in the way the young adults, or their parents, perceived their attachment relationship.
Strengths and limitations
This paper is the first to present a systematic characterisation of DSE behaviours in adulthood. It has a number of strengths including its prospective longitudinal nature, natural experimental adoption design and the stratification of deprivation-related risk (by duration) to increase statistical power. However, there are also a number of limitations that need to be considered when interpreting the findings. First, DSE was assessed by a limited number of items at each age. However, these appeared to be psychometrically robust and to capture important deprivation-related features that were validated by direct observation and self-reports. Second, attrition at the young adult assessment was higher than the very low rates seen at previous ERA follow-up assessments. This, although not surprising given the age range of the young adults, limited the statistical power of the analysis especially in the comparison of DSE+ and DSE− groups. However, attrition appeared to be non-selective in nature. Third, we had limited information on pre-institutional risks such as maternal smoking or stress exposures during pregnancy and these could have been elevated in the current sample. However, it seems unlikely that Rom > 6 children would have been exposed to sufficiently greater risk prenatally than their Rom < 6 group counterparts, in part at least because the timing of adoption was largely determined by the fall of the Ceauşescu regime. Fourth, because duration and timing of deprivation overlapped, we were unable to address the key issue of sensitive developmental windows in any detail.
In summary, DSE behaviours continue to be core to the deprivation-related pattern in young adulthood in the ERA study – it is strongly related to the duration of deprivation and other deprivation-specific patterns such as ADHD and ASD. However, unlike these other patterns, DSE in and of itself appears to be relatively benign – apparently not, in and of itself, affecting QoL, functioning within different social domains, or educational and employment status.
Funding
This work was funded by a project grant from the UK Economic Social Research Council ().
Acknowledgements
We would like to express our sincere gratitude to all the families and young people who have participated in this study over the many years it has been running. Without them this work would not be possible. We are also grateful for the comments of Dr Graeme Fairchild during initial planning meetings. Thanks go to all the previous researchers on the project especially Dr Celia Beckett, Jenny Castle, Dr Suzanne Stevens, Dr Emma Colvert, Christine Groothues and Amanda Hawkins who were involved in the collection of data during the mid-adolescent phase of the project. We thank our advisory board for all their useful suggestions especially Professor Megan Gunnar, Professor Trevor Robbins and Dr John Simmonds.






eLetters
No eLetters have been published for this article.