Long duration of untreated psychosis (DUP) confers a poor prognosis in schizophrenia (Reference Crow, Macmillan and JohnsonCrow et al, 1986; Reference Johnstone, Macmillan and FrithJohnstone et al, 1990; Reference Loebel, Lieberman and AlvirLoebel et al, 1992; Reference Jablensky, Sartorius and ErnbergJablensky et al, 1992). These effects appear to persist for years after first onset (Reference WyattWyatt, 1991; Reference Scully, Coakley and KinsellaScully et al, 1997). Reducing delays in initial detection and treatment might improve long-term outcome (Reference Birchwood, Todd and JacksonBirchwood et al, 1998; Reference McGlashan and JohannessenMcGlashan & Johannessen, 1996). However, what delays presentation is poorly understood. We aimed, first, to identify the illness-related factors which delay treatment. This might clarify the feasibility of, and suggest strategies for, early intervention. We hypothesised that particular symptoms (like poor insight) and aspects of social function (like preserved living skills) prolong DUP. Second, we aimed to investigate the link between DUP and the outcome of treatment, both to exclude confounding variables and to estimate the likely gains from early intervention. Our hypothesis was that long DUP leads to poor treatment response, even after accounting for the severity of the symptoms at admission.
METHOD
Sample
Patients were recruited from consecutive day- and in-patient admissions for first episodes of psychosis over a 26-month period, as part of a randomised, controlled psychological treatment study (the Study of Cognitive Reality Alignment Therapy in Early Schizophrenia - SOCRATES). They were aged 16-64 and admitted from three geographically defined catchment areas (Manchester, Liverpool, North Nottinghamshire) with a combined population of 2 260 000. Communities in these areas ranged from deprived urban populations to prosperous or rural ones. Investigators contacted all in- and day-patient units weekly to find suitable admissions.
Eligible patients met criteria for DSM-IV (American Psychiatric Association, 1994) schizophreniform disorder, schizophrenia, schizoaffective disorder, delusional disorder and psychosis not otherwise specified. Patients were excluded if substance misuse was judged to be the major cause of the psychosis. Patients were randomised to one of three treatment conditions on top of routine care: cognitive—behavioural therapy (CBT), supportive counselling and no extra treatment.
Baseline assessments
Three clinicians, one at each centre (R.J.D., C.J.H., S.A.), interviewed and assessed patients within 14 working days of admission. Consensus decisions about DSM-IV diagnoses were made with a central supervisor (S.W.L.). Assessments were made as follows.
Duration of untreated psychosis
We measured DUP from the first onset of delusions and hallucinations. This is measured reliably compared to alternatives such as the time from the onset of deterioration in social function (Reference Larsen, Johannessen and OpjordsmoenLarsen et al, 1998). DUP was estimated after combining different sources of information using an algorithm. In every case, there was a face-to-face semi-structured patient interview, supplemented by review of case notes, referral letters and questioning of staff. If relatives were available, they were also interviewed. Interrater reliability was assessed from audiotaped interviews with 11 patients: intraclass correlation was 0.86.
The Positive and Negative Syndrome Scale for schizophrenia
This is a well-validated scale for the assessment of psychotic and allied symptoms (PANSS) (Reference Kay, Fishbein and OpierKay et al, 1987). The raters were trained using interviews with patients, face-to-face and on video. Intraclass correlations for the positive, negative and general sub-scale scores were 0.93, 0.76 and 0.77, respectively, and for total score was 0.73.
The Social Functioning Scale
This is a widely used, self-completed measure with established reliability and validity (SFS) (Reference Birchwood, Smith and CochraneBirchwood et al, 1990). Sub-scales give continuously distributed scores for (a) social withdrawal, (b) relationships, (c) social and recreational activities, (d) performance and competence in activities of daily living, and (e) occupational function.
Follow-up assessments
Subjects were re-interviewed with the PANSS 6-12 weeks after baseline interview. Follow-up was completed in 87%. Patients treated with CBT or counselling had therapy for 5 weeks, and then booster sessions over another 7.
Analysis
Using SPSS 6.1 for Windows, we examined associations between DUP and demographic, symptomatic and social functioning variables at baseline using correlation measures. After initial data analysis, DUP was normalised by taking the logarithm to base 10 (log10DUP) to allow the use of parametric statistics (i.e. Pearson's r, t-tests), and these results are presented.
Our first hypothesis was that concern about symptoms or social dysfunction, either by patients or their social network, would lead to presentation and hence shorten DUP. We could not measure concern directly so we nominated variables a priori that would be particularly closely related to concern and hence most strongly associated with DUP. We proposed that patients with poor insight would be unconcerned and those who were socially avoidant would also present later, so these items from the PANSS would correlate with long DUP.
We also proposed that patients whose daily living skills were deteriorating would concern others more, whereas those who were poorly socially integrated would cause less concern. We derived an index of social integration from the social withdrawal and relationships sub-scales of the SFS ((a) and (b) above), and an index of coping skills from the SFS daily living competence and performance sub-scales ((d) above). Therefore, we predicted that poor integration and better coping would be associated with longer DUP.
Finally, we predicted that all other PANSS items and demographic factors would not be directly related to DUP, after the specified key variables had been taken into account.
We performed a general factorial analysis of variance (ANOVA) with log10DUP as the dependent variable (this let us include categorical confounders like ethnicity more easily than a multiple regression). First, independent variables were transformed, if necessary, to be suitable for the ANOVA. Heavily skewed or bimodal PANSS items were reduced to binary variables. Age at onset and years of full-time education were normalised by taking the reciprocal of the original values. Substance use was reduced to a binary variable: either daily use of illicit drugs (or alcohol dependence), or not.
The key variables were added as independent covariates. These were the insight variable (from PANSS item G12); social avoidance (PANSS item G16), the social integration index and the coping index (derived from the SFS). Last, confounding demographic and symptom variables were added as cofactors (ethnicity, gender, substance misuse, binary PANSS items) or covariates (age at onset and years of education, and all the other PANSS items). We predicted that the key variables would correlate significantly with log10DUP, but not the other symptom or demographic variables. We also repeated the ANOVA with DUP as the dependent variable, to compare the fit of the model.
To test the second hypothesis, about recovery after treatment, we first correlated log10DUP with change in PANSS total score over the follow-up period. Then we used baseline variables (including log10DUP and determinants of log10DUP) to predict change in PANSS as the dependent variable in an ANOVA, as for the analysis of determinants of DUP. This would reveal whether log10DUP still had a significant association with the outcome of initial treatment after correcting for confounders. We included the treatment group in the SOCRATES trial as an independent variable.
RESULTS
Sample characteristics
From 281 eligible first admissions, 248 consented to serial assessments after 32 (11%) refused and 6 (2%) were unable to consent within the recruitment period. Patients were assessed within a median period of 6 days after admission. Demographic details are summarised in Table 1. Overall, cannabis was the most widely used illicit drug (77% of all illicit drug users and 78% of daily users). A further 22 (9% of the sample) used alcohol daily.
Table 1 Demographic and diagnostic characteristics of the sample
| Variable | n | (%) |
|---|---|---|
| Gender | ||
| Male | 173 | (70%) |
| Female | 75 | (30%) |
| Age at admission, years: median (range) | 27.4 | (16-64) |
| Full-time education, years: median (range) | 11 | (7-21) |
| DSM-IV diagnosis | ||
| Schizophreniform disorder | 97 | (39%) |
| Schizophrenia | 86 | (35%) |
| Schizoaffective disorder | 33 | (13%) |
| Delusional disorder | 22 | (9%) |
| Psychosis NOS | 10 | (4%) |
| Ethnicity (self-ascribed) | ||
| White | 215 | (87%) |
| African—Caribbean | 19 | (8%) |
| South Asian | 4 | (2%) |
| Other | 10 | (4%) |
| Illicit drug use in 12 months before assessment | ||
| None | 97 | (39%) |
| Occasional | 30 | (12%) |
| Weekly | 17 | (7%) |
| Daily | 23 | (9%) |
| Unknown | 81 | (33%) |
Duration of untreated psychosis
This ranged from 4 to 624 weeks. The median was 12 weeks, and mean 38 weeks. Sixteen patients had untreated psychoses for between 2 and 12 years. However, transformation of the DUP by taking the logarithm to base 10 showed that these extreme scores were part of the resulting distribution, rather than being outliers. Mean of log10 DUP was 1.172, corresponding to a DUP of 14.9 weeks.
Correlates of DUP at admission
Log10DUP was not significantly associated with gender or age at onset of psychosis, nor was there a significant overall effect of ethnicity (one-way ANOVA). Illicit drug users did not have a log10DUP significantly different from non-users. For users, median DUP was 10 weeks, range 4-624; for non-users median was 14 weeks, range 4-600. There was no trend for increasing frequency of substance misuse to relate to shorter DUP.
At baseline, log10DUP correlated positively with the PANSS total score (r=0.13, P=0.04): the longer the DUP the more severe the symptoms at admission. Pearson correlations with the positive symptom and general psychopathology sub-scale scores were 0.14 (P=0.03) and 0.15 (P=0.02), respectively, but with the negative sub-scale r was 0.05 (P=0.49).
Although DUP did not correlate significantly with SFS total score (for log10DUP r=0.04, NS), this masked correlations with component sub-scales in opposite directions. DUP correlated negatively with the social integration index (r=-0.14, P=0.05), and positively with the coping index (r=0.16, P=0.03); thus, long DUP was predicted by worse social integration on the one hand, but by better coping with daily activities on the other.
ANOVA with baseline symptoms, social function indexes and demographics as independent variables predicted 18% of the variance in log10DUP. Poor insight, poor integration and avolition predicted longer DUP. Shorter DUP was predicted by poor coping and the presence of pre-occupation or hostility. Table 2 shows the correlation between these independent variables and DUP corrected for confounders (using β values for each covariate in the ANOVA, and point biserial correlation for binary variables). ANOVA with untransformed DUP as the dependent variable had much inferior fit and explanatory power.
Table 2 Correlation of baseline variables with duration of untreated psychosis
| Variable | Correlation | P |
|---|---|---|
| PANSS lack of insight | 0.351 | <0.001 |
| SFS integration | -0.231 | 0.004 |
| SFS coping | 0.171 | 0.04 |
| PANSS poor volition | 0.191 | 0.02 |
| PANSS preoccupation | -0.181 | 0.02 |
| PANSS hostility | -0.152 | 0.03 |
Comparison of day patients and in-patients
As a first admission study our criteria excluded out-patients and those not referred to specialist services, a potential source of bias. Because we did not have data on these other groups we compared the 36 day patients to the 212 in-patients as an indication of any effect of treatment setting. There was no significant difference in log10DUP, social factors, PANSS total or subtotals, or PANSS absolute or percentage change. Day patients were significantly more likely to use illicit drugs daily, and to have schizoaffective disorder or delusional disorder (χ2). Adding setting as a variable did not affect the result of the analysis of variance.
Does DUP predict symptoms after 3 months?
Overall, 215 (87%) of patients were re-assessed prospectively with the PANSS at 6-12 weeks. Mean baseline PANSS scores at baseline and follow-up were 88.7 (s.d.=16.8) and 64.5 (s.d.=18.7). PANSS score decreased by a mean of 23.9 points (s.d.=19.3), or 40% (s.d.=31.3), by 6-12 weeks.
Longer DUP clearly predicted less improvement in PANSS during treatment. Log10DUP correlated 0.32 (Pearson's r, P<0.0005) with PANSS score at re-interview and, after allowing for baseline PANSS, the partial correlation for log10DUP and PANSS at re-interview was 0.28 (P<0.0005). The partial correlation between log10DUP and change in PANSS, controlling for PANSS at baseline, was 0.29 (P<0.0005).
To examine DUP as a predictor of response to treatment we used the change in PANSS score between baseline and re-interview as the dependent variable in another ANOVA. Change in PANSS was calculated as a percentage of baseline score. Log10DUP, age, education, gender, ethnic group, daily drug use and treatment group within the SOCRATES trial (counselling, CBT or no psychotherapy) were entered as independent variables. The four primary variables from the previous analysis — insight, social avoidance, social integration and coping — were also entered. Finally, the strongest predictors of log10DUP (see Table 2) were included as independent variables.
This model explained 13% of the variance in change in PANSS. Log10DUP remained a predictor of change (β=0.17, P=0.041), with longer DUP again predicting less improvement. Better social integration predicted more improvement in PANSS score (i.e. greater decrease over treatment: β=-0.18, P=0.046). Surprisingly, better coping predicted less improvement (β=+0.30, P=0.001). Insight, the strongest predictor of long DUP, was not significantly associated with change in PANSS (β=0.04, P=0.64). Male gender predicted less improvement (point biserial correlation 0.14, P=0.055). Other demographic variables were not strongly associated with PANSS change (all P>0.30); nor was treatment condition (P=0.52). We repeated the ANOVA, substituting DUP for log10DUP as an independent variable, but again its explanatory power and fit were poorer (DUP β =0.09, P=0.40).
We used the model with log10DUP to estimate the size of the effect of DUP on treatment outcome (see Table 3 and Fig. 1). We used the gradient of log10DUP against PANSS change, mean values of log10DUP and PANSS change, and the proportion of variance explained by the model to calculate the percentage change in PANSS score predicted by a given DUP (Reference AltmanAltman, 1991).
Table 3 Predicted impact of duration of untreated psychosis on the amount of improvement in Positive and Negative Syndrome Scale (PANSS) score after 12 weeks of treatment
| DUP1 | Mean improvement in PANSS score2 | 95% CI3 |
|---|---|---|
| 1 month | -44% | -50 to ‒39 |
| 6 months | -38% | -41 to ‒34 |
| 1 year | -35% | -40 to ‒30 |
| 6 years | -29% | -40 to ‒18 |
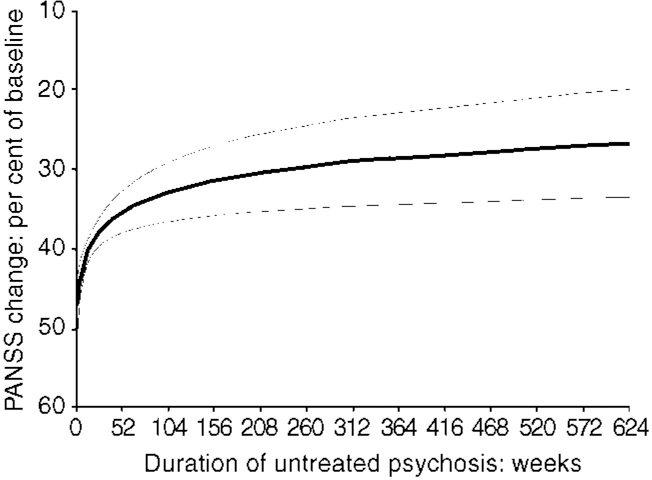
Fig. 1 Predicted change in Positive and Negative Syndrome Scale (PANSS) against duration of untreated psychosis (with 95% Cls).
DISCUSSION
Duration of untreated psychosis emerged as the single strongest predictor of symptom severity after 6-12 weeks of treatment in this sample, the association remaining strong even controlling for severity of symptoms at baseline. This replicates previous findings in a large, prospectively assessed, first-admission sample. We modelled the determinants of DUP: poor insight, avolition and poor social integration were linked to long DUP, whereas hostility and poor coping led to a short DUP. However, these variables did not fully account for the link between long DUP and response to treatment. This suggests that the link is not explained by a subtype of illness that causes both a long DUP and a poor outcome, as proposed by Crow et al (Reference Crow, Macmillan and Johnson1986).
Limitations and methodology
This was a first-admission rather than first-contact sample, which may be a source of bias. Although day patients were not significantly different from in-patients on most variables, differences between out-patient or primary-care contacts and our sample may be greater. None the less, the administrative incidence for schizophrenia-related disorders in this study (0.67 per 10 000 per year) compares to the 0.8 per 10 000 per year reported by Der et al (Reference Der, Gupta and Murray1990) and suggests most first episodes were included. Importantly, we did not collect data concerning pathways to care or responsiveness of services, which might well affect DUP. Service factors examined elsewhere include poor recognition of psychosis and undertreatment after recognition (Reference Johnstone, Crow and JohnsonJohnstone et al, 1986; Reference Larsen, Johannessen and OpjordsmoenLarsen et al, 1998). Clear evidence of the contribution of these effects relative to illness-related factors is lacking.
Critically for the analysis of determinants of DUP, we have no information actually gathered during the period of untreated psychosis, so we rely on baseline measures to estimate these variables retrospectively. Nor could we measure ‘concern’ directly, so we depended on indirect measures like insight and coping. Although we expect that these distortions generally predispose to type 2 error, it may be that retrospective bias affects some variables more than others.
Previous studies have been limited by relatively small or uncharacteristic samples; unstandardised assessments made some time after first treatment; and a lack of longitudinal, prospective follow-up. Many have excluded patients with significant drug use or dependence. These limits reduced the degree to which their findings generalised to clinical practice, and potentially introduced bias. In our sample, the effect of illicit drug use on DUP and change in symptoms was small. However, the change in symptoms over 3 months is more of an estimate of speed of recovery than long-term outcome, which we did not assess.
DUP and its determinants
We found the median DUP to be 12 weeks (mean 38 weeks), which is shorter than in some other studies. Definitions of DUP based on duration of delusions and hallucinations, as here, give shorter DUPs than definitions which depend on the duration of other, less clear-cut symptoms (Reference Häfner, Maurer and LöfflerHäfner et al, 1993). In similar samples, MacMillan et al (Reference Macmillan, Crow and Johnson1986) found delay from onset of positive symptoms to admission had a median of 18 weeks, and Ring et al (Reference Ring, Tantam and Montague1991) 9 weeks.
Overall social function was not significantly associated with DUP, but different aspects of social function had different effects, which suggests that treating social dysfunction in schizophrenia as a simple global deficit is untenable in studies such as this. The prediction that social avoidance would independently delay patients from acting on their own concerns, or under pressure from others, was not borne out. Although hostility, avolition and preoccupation were not predicted to be determinants of DUP before the analysis, it is easy to see that they do not necessarily invalidate the basic hypothesis that concern and acting on concern determine the timing of presentation.
It is possible to argue that poor insight and avolition could as well be consequences of long DUP as causes of it. However, the direction of causation is clear with other variables: poor coping with the activities of daily living must lead to early presentation, rather than long DUP improving coping skills. Therefore, the simplest way to explain the overall pattern of findings is that concern causes presentation; at present there is no evidence to the contrary. This is consistent with sociological models for the determinants of presentation for many other illnesses, based on concern by the patient or significant others (Reference MechanicMechanic, 1978).
DUP and recovery
DUP predicted less recovery after 3 months of treatment even after covarying for the determinants of DUP and the severity of symptoms at baseline. Although these variables do not fully mediate the relationship between continuing, untreated symptoms and poor recovery, the psychological or biological processes that might are unclear.
If delaying treatment has an effect on recovery, how large might it be? Modelling of the effect of DUP on change in PANSS scores over the treatment period allowed us to estimate this (see Fig. 1). It appears that the gains in treatment effect resulting from earlier detection will be much greater in the early stages of illness (Table 3): reducing DUP from 6 months to 1 month produces gains in outcome similar to reducing it from 6 years to 1 year. This emphasises the importance of ensuring an efficient community recognition and referral system, with prompt delivery of effective treatments, particularly for patients with recent onset of psychotic symptoms.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Longer duration of untreated psychosis (DUP) predicts worse symptoms at admission; and, even accounting for this and for demographic factors, it predicts poorer response after treatment.
-
▪ Early intervention services should concentrate on shortening the shortest DUPs, since the effect of DUP on recovery is greatest in the early stages of illness.
-
▪ DUP is partly determined by concern about the illness by sufferers or people in their social networks. This concern is influenced by the poor insight and social deficits of the sufferers.
LIMITATIONS
-
▪ Factors determining DUP were estimated retrospectively using measures taken after admission, and ‘concern’ was not measured directly.
-
▪ Change in symptoms over the first 3 months of treatment for the first episode of psychosis is more a measure of speed of recovery than of final outcome.
-
▪ Only patients admitted to day units or in-patient units were included, so undetected cases and patients treated in primary care or as out-patients were excluded.
ACKNOWLEDGEMENTS
We gratefully acknowledge the help of Professor Graham Dunn in the analysis and presentation of this work, and the rest of the SOCRATES team.







eLetters
No eLetters have been published for this article.