Psychological stress occurring during either childhood or adulthood has been related to psychosis. Reference Van Winkel, Stefanis and Myin-Germeys1 Childhood adversity as a form of psychological stress has been shown to be a risk factor for the development of psychotic symptoms in clinical samples Reference Bendall, Jackson, Hulbert and McGorry2,Reference Bebbington, Bhugra, Brugha, Singleton, Farrell and Jenkins3 and psychotic-like experiences in individuals from the general population. Reference Kelleher, Harley, Lynch, Arseneault, Fitzpatrick and Cannon4,Reference Spauwen, Krabbendam, Lieb, Wittchen and van Os5 Despite this established relationship, it is necessary to consider the type and severity of any environmental exposure, together with a specific individual genetic background of risk, in order to understand the development of psychosis in adulthood. The term childhood adversity usually refers to a wide range of severe adverse experiences occurring early in life (before 16 years of age) and includes sexual, physical and emotional abuse and neglect. In this regard, several lines of research have suggested a strong relationship between childhood abuse and positive psychotic symptoms. Reference Janssen, Krabbendam, Bak, Hanssen, Vollebergh and de Graaf6 However, less attention has been paid to the effect of neglect, and studies examining the impact of both types of childhood adversity are still relatively scarce. Genetic factors are also likely to be involved in the individual variation in response to stress. Genes involved in regulating the adaptive behavioural response to stress represent plausible candidates to explore putative gene–environment interaction effects in the association between childhood adversity and psychotic symptoms. In this context, the BDNF-Val66Met polymorphism has been related not only to psychosis but has also been shown to moderate the impact of childhood adversity on the later expression of affective symptoms. Reference Chen, Jing, Bath, Ieraci, Khan and Siao7,Reference Aguilera, Arias, Wichers, Barrantes-Vidal, Moya and Villa8 Brain-derived neurotrophic factor (BDNF) is a neurotrophin that promotes the growth and differentiation of developing neurons in central and peripheral nervous systems. Reference Buckley, Mahadik, Pillai and Terry9 It has been shown that early stress can influence BDNF expression and produce long-lasting effects on neurotrophic processes, thereby having an impact on neuronal maturation and plasticity in later life. Reference Van Winkel, Stefanis and Myin-Germeys1 However, studies of the relationship between the functional BDNF-Val66Met polymorphism and schizophrenia have produced mixed results, Reference Buckley, Mahadik, Pillai and Terry9 which may be because of the underlying gene–environment interaction. Reference van Os, Sham, Murray, Jones, Susser, van Os and Cannon10 One recent study found that Met carriers (negatively affecting intracellular processing and secretion of the mature protein) report more paranoid feelings in the presence of social stress than do Val/Val carriers. Reference Simons, Wichers, Derom, Thiery, Myin-Germeys and Krabbendam11 Thus, it is plausible that the BDNF-Val66Met polymorphism might play a moderating role in the association between childhood adversity and psychosis. The present study aimed to explore whether childhood adversity (childhood abuse and childhood neglect) have a differential impact on the presence of psychotic-like experiences. Furthermore, a possible moderating effect of the BDNF-Val66Met polymorphism on the relationship between childhood adversity and psychotic-like experiences was also investigated.
Method
Sample
The sample consisted of 533 individuals who were recruited from the campus of the Jaume I University in Castelló (Spain), as well as from university offices and community technical schools in the metropolitan area of Barcelona (Spain). All the participants were adults (mean age 22.9 years, s.d. = 5.4) and 45.4% were males. At the time of the assessment 77% of the participants were students. Exclusion criteria were the presence of any major medical illness affecting brain function, neurological conditions and a history of head injury. All participants were of Spanish (White) ancestry, thereby reducing the possibility of confounding genetic differences by population stratification. Reference Freedman, Reich, Penney, McDonald, Mignault and Patterson12 Ethical approval was obtained from local research ethics committees. All participants provided written informed consent before inclusion in the study.
Measures
The Community Assessment of Psychic Experiences (CAPE) Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis and Stefanis13 was used to assess positive and negative psychotic-like experiences in the sample. This validated self-report questionnaire measures the lifetime prevalence of psychotic-like experiences on a frequency scale ranging from ‘never’ to ‘nearly always’. Examples of the items assessing the positive and negative dimension are, respectively, ‘do you ever feel as if things in magazines or TV were written especially for you?’ and ‘do you ever feel that you experience few or no emotions at important events?’. The CAPE provides a total score per dimension by adding up the scores on the frequency items.
Childhood adversity was assessed by the shortened version of the Childhood Trauma Questionnaire (CTQ). Reference Bernstein14 This questionnaire consists of 28 items measuring five types of childhood trauma: emotional abuse, physical abuse, sexual abuse, emotional neglect and physical neglect. Childhood adversity was grouped into two main types: childhood abuse (including emotional, physical and sexual abuse) and childhood neglect events (including emotional and physical neglect). This was done in order to explore the putative specificity of the impact of these two types of childhood adversity. Childhood abuse and childhood neglect were calculated by summing the items included for each type of childhood adversity. Example items of childhood abuse and childhood neglect are, respectively, ‘people in my family hit me so hard that it left me with bruises or marks’ and ‘my parents were too drunk or high to take care of the family’. The score for each item ranges from 1 to 5 (‘never true’ to ‘very often true’), depending on the extent to which individuals agree with the statement. Reliability and validity of the CTQ have both been demonstrated. Reference Bernstein, Stein, Newcomb, Walker, Pogge and Ahluvalia15
Because schizotypal personality, cannabis use and anxiety levels have all been related to both childhood adversity and psychotic-like experiences, and given the relationship between them, Reference Barkus and Lewis16–Reference Barrantes-Vidal, Lewandowski and Kwapil18 the analyses were corrected for these variables, along with age and gender as other potential confounders. Schizotypal personality was measured with the Schizotypy Personality Questionnaire-Brief (SPQ-B). Reference Raine and Benishay19 Cannabis use was assessed with one question regarding the frequency of consumption: ‘never’, ‘once’, ‘monthly’, ‘weekly’ or ‘daily’ (this variable was then dichotomised into two categories: ‘not exposed to cannabis’: never, once; and ‘exposed to cannabis’: monthly, weekly, daily). Anxiety as a behavioural trait was assessed using the State–Trait Anxiety Inventory (STAI-T). Reference Spielberg, Gorsuch and Lushene20
Laboratory methods
Genomic DNA was extracted from peripheral blood cells using the Real Extraction DNA Kit (Durviz SLU, Valencia, Spain), or from buccal mucosa on a cotton swab using the BuccalAmp DNA Extraction Kit (Epicentre Biotechnologies, Madison, Wisconsin, USA). The rs6265 SNP (Val66Met) of the BDNF gene was determined using the Taqman 5′ exonuclease assay (Applied Biosystems) and genotyped using Applied Biosystems (AB) TaqMan technology. The probe for genotyping the rs6265 was ordered through the TaqMan SNP Genotyping assays (code C_11592758_10) AB assay-on-demand service. The final volume of the polymerase chain reaction was 5 ml, which contained 10 ng of genomic DNA, 2.5 ml of TaqMan Master Mix, and 0.125 ml of 40x genotyping assay. The cycling parameters were as follows: 95°C for 10 min followed by 40 cycles of denaturation at 92°C for 15 s and annealing/extension at 60°C for 1 min. Polymerase chain reaction plates were read on an ABI PRISM 7900HT instrument with SDS v2.1 software (Applied Biosystems).
Statistical analyses
Multiple linear regressions were conducted using STATA 10.0 for Windows. Separate models were tested for CAPE positive and CAPE negative as dependent variables. For the first hypothesis the independent variables of interest were childhood abuse, childhood neglect and the BDNF-Val66Met polymorphism. Schizotypal personality, cannabis use, trait anxiety, gender and age were included in the model as covariates. For the second hypothesis, two-way interaction effects between childhood abuse and the BDNF-Val66Met polymorphism and childhood neglect and the BDNF-Val66Met polymorphism were added to the model, as described for the first hypothesis. Since the Met/Met genotype (n = 29) has a much lower frequency than the Val/Met and Val/Val genotypes, the genotypes for this polymorphism were included in the analyses as a binary variable (Met allele carriers and Val homozygotes).
Results
Descriptive statistics
In order to obtain the prevalence of psychotic-like experiences in the current sample, CAPE scores were recoded to 0 (never, sometimes) and 1 (often, almost always). The resulting prevalence rate indicated that psychotic-like experiences were quite frequent. Specifically, 40.7% of the sample often or almost always experienced at least one positive psychotic-like experience; similarly, 47.6% reported experiencing at least one negative psychotic-like experience often or almost always.
The prevalence of childhood adversity was evaluated by recoding the answers to 0 (never true) and 1 (rarely true, sometimes true, often true and very often true). Thus, 1 indicates that the individual was exposed at least once to the adverse event. In the current sample, 25.5% of the individuals were exposed to childhood abuse and 32.2% to childhood neglect. More details of the distribution of dimensions in the sample can be found elsewhere. Reference Aguilera, Arias, Wichers, Barrantes-Vidal, Moya and Villa8
Genotype information was available for 470 individuals. The genotype frequencies for the BDNF-Val66Met polymorphism were: Val/Val: 60% (n = 282); Val/Met: 33.8% (n = 159); and Met/Met: 6.2% (n = 29). These frequencies did not differ from others described in previous studies conducted in White individuals. Reference Egan, Kojima, Callicott, Goldberg, Kolachana and Bertolino21 Hardy–Weinberg equilibrium was verified for the present population (χ2 = 1.05, d.f. = 2, P = 0.59).
The final sample consisted of 411 individuals for whom all the variables included in the models were available.
Specificity of the impact of childhood adversity on psychotic-like experiences
We found a main effect of childhood abuse on positive psychotic-like experiences (β = 0.16, s.e. = 0.05, P = 0.002) and a marginally significant effect of childhood abuse on negative psychotic-like experiences (β = 0.11, s.e. = 0.06, P = 0.055) (Table 1). Childhood neglect did not have a direct influence on either positive or negative psychotic-like experiences. Furthermore, no main effect was found for the BDNF-Val66Met polymorphism on either dimension of psychotic-like experiences.
Gene–environment interaction between the BDNF-Val66Met polymorphism and childhood adversity with respect to subsequent psychotic-like experiences
A significant gene–environment interaction was detected between BDNF Met carriers and childhood abuse with regard to positive psychotic-like experiences (β = 0.27, s.e. = 0.10, P = 0.004). In this
Table 1 Main effects of childhood abuse, childhood neglect and the BDNF-Val66Met polymorphism (Val/Val v. Met carriers) on positive and negative psychotic-like experiences, correcting for age, gender, schizotypal personality, cannabis use and trait anxiety
| Positive psychotic-like experiencesa | Negative psychotic-like experiencesb | |||||
|---|---|---|---|---|---|---|
| β | s.e. | P | β | s.e. | P | |
| BDNF | –0.385 | 0.358 | 0.282 | 0.338 | 0.409 | 0.409 |
| Childhood abuse | 0.155 | 0.049 | 0.002 | 0.107 | 0.056 | 0.055 |
| Childhood neglect | –0.085 | 0.053 | 0.110 | –0.032 | 0.060 | 0.591 |
a R 2 = 0.31.
b R 2 = 0.32.
Values in bold are significant.
sample, individuals carrying the Met allele had higher scores on adult positive psychotic-like experiences when childhood abuse was present, as compared with participants carrying Val/Val homozygotes (Fig. 1). No significant gene–environment interaction was detected with respect to childhood neglect (β = –0.09, s.e. = 0.05, P = 0.110).
Discussion
This study shows that childhood adversity has a strong independent effect on positive psychotic-like experiences and a marginally significant effect on negative psychotic-like experiences, whereas childhood neglect was not associated with either dimension of psychotic-like experiences. The BDNF-Val66Met polymorphism shows a moderating effect between childhood abuse and the later development of positive psychotic-like experiences. These results are not confounded by the effect of gender, age, schizotypal personality, cannabis use or trait anxiety.
Childhood adversity and psychotic-like experiences
Several years ago it was postulated that light might be shed on the aetiology of psychosis by studying individuals who have psychotic symptoms without being in need of treatment. Reference Johns and van Os22 Broadly, there are two potential approaches to the measurement of psychotic symptoms in non-clinical samples: one would be to measure schizotypal traits as an attenuated form of psychotic symptoms, whereas the other would involve measuring in the general population the occurrence of those symptoms that are seen in individuals with psychosis. The latter approach assumes that experiencing ‘symptoms’ of psychosis is not inevitably linked with the clinical disorder. Thus, even though the prevalence of the clinical disorder is low, the prevalence of these ‘milder forms’
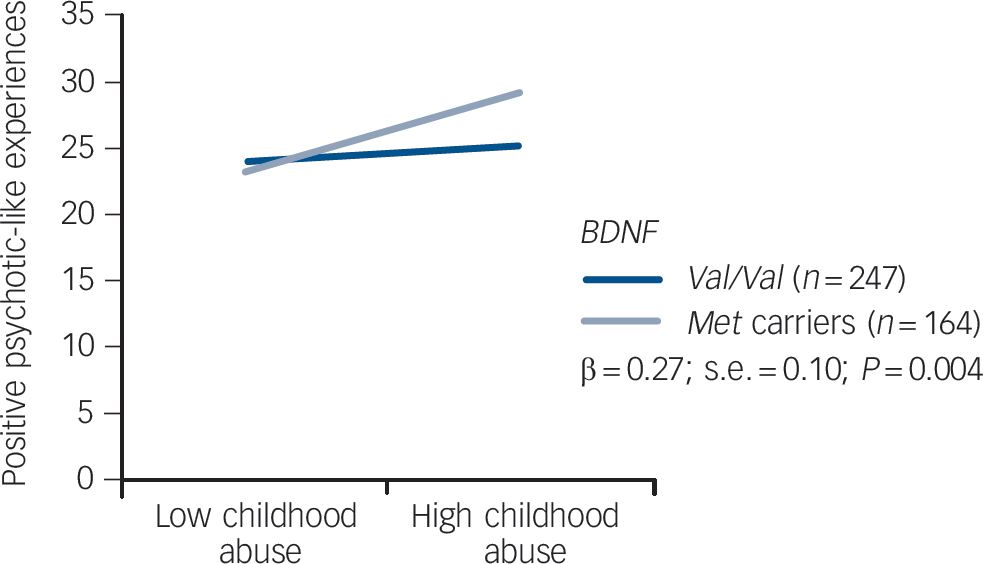
Fig. 1 Graphic respresentation of the interaction effect between childhood abuse and the BDNF-Val66Met polymorphism on positive psychotic-like experiences.
Corrected for age, gender, schizotypal personality, cannabis use and trait anxiety. Exposure to childhood abuse is moderated by the BDNF gene. Met carriers exposed to childhood abuse have significantly higher scores on positive psychotic-like experiences.
of psychosis, namely psychotic-like experiences, may be much higher. Reference Stefanis, Hanssen, Smirnis, Avramopoulos, Evdokimidis and Stefanis13,Reference Johns and van Os22 The rate of psychotic-like experiences in the present sample is in line with previous reports. Reference Johns and van Os22 For example, Barrett & Etheridge found that 30–40% of individuals from the general population reported the experience of hearing voices. Reference Barrett and Etheridge23 Similarly, in a sample of college students, 71% reported at least brief, occasional hallucinated voices during periods of wakefulness, whereas 39% reported hearing their thoughts spoken aloud. Reference Posey and Losch24
Regarding the aetiology of psychotic-like experiences, according to previous research, our findings support the role of childhood adversity as a risk factor underlying the development of psychotic-like experiences in the general population. Reference Kelleher, Harley, Lynch, Arseneault, Fitzpatrick and Cannon4–Reference Janssen, Krabbendam, Bak, Hanssen, Vollebergh and de Graaf6 Specifically, there was a strong association between childhood abuse and positive psychotic-like experiences and a trend towards an association between childhood abuse and negative psychotic-like experiences. These results fit well with recent models suggesting that adverse events, especially those characterised by abuse, may produce a psychological and/or biological vulnerability for the development of positive psychotic symptoms, including subclinical forms such as psychotic-like experiences. Reference Johns and van Os22,Reference Garety, Kuipers, Fowler, Freeman and Bebbington25,Reference Read, Perry, Moskowitz and Connolly26 It has been suggested that early abusive experiences may create an enduring cognitive vulnerability characterised by negative schematic models of the self and the world (for example beliefs about the self as vulnerable to threat, or about others as dangerous) that facilitate external attributions, which may ultimately lead to paranoid ideation. Reference Garety, Kuipers, Fowler, Freeman and Bebbington25 In this regard, current ideas about the biological consequences of childhood adversity lend even more credibility to the notion of an enduring psychological vulnerability. When exposure to stressors persists, the stress-induced glucocorticoid release can become chronic, leading to permanent changes in the hypothalamic–pituitary–adrenal (HPA) axis. This alteration of HPA functioning can lead to dysregulation of the dopaminergic system, which is generally thought to be involved in psychosis. Reference Van Winkel, Stefanis and Myin-Germeys1,Reference Heim, Newport, Heit, Graham, Wilcox and Bonsall27 Specifically, it has been suggested that stress-induced dysregulation of the HPA axis causes increased dopamine receptor densities and greater dopamine release. The dopaminergic system is important as regards the interpretation of stress and threat-related stimuli, and therefore, relevant to the development of positive psychotic symptoms such as paranoid ideation. Reference Read, Perry, Moskowitz and Connolly26
In our sample, childhood neglect was not significantly associated with psychotic-like experiences. Although this contrasts with some previous reports, Reference Vogel, Spitzer, Kuwert, Moller, Freyberger and Grabe28,Reference Gil, Gama, de Jesus, Lobato, Zimmer and Belmonte-de-Abreu29 a recent study by Fisher and colleagues Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan30 also found no impact of neglect on the expression of psychosis when controlling for the impact of abuse. Conversely, events characterised by abuse have shown the most robust association with psychotic symptoms. Reference Janssen, Krabbendam, Bak, Hanssen, Vollebergh and de Graaf6,Reference Whitfield, Dube, Felitti and Anda31,Reference Morgan and Fisher32 Moreover, it has been postulated that abusive experiences could have an aetiological significance in psychosis, Reference Harris and Cooper33 and research has described higher rates of abusive maltreatment than neglect among individuals with psychosis. Reference Hlastala and McClellan34 Hence, it may be that previous associations between psychosis and childhood adversity, where the latter included both abuse and neglect events, were inflated by the effect of abuse.
BDNF-Val66Met polymorphism, childhood adversity and psychotic-like experiences
Gene–environment interaction studies have shown exciting findings that made them appear to be promising mechanisms to understanding the joint effect between environmental and genetic factors in the aetiology of complex traits such as psychiatric symptoms. Reference Rutter, Moffitt and Caspi35 However, dismissal of gene–environment interaction studies has recently arisen mainly as a result of the failure to replicate; as has happened before with genetic association studies. Reference Munafo and Flint36 It has been argued that the lack of replication may be related to the greater number of potential statistical tests that are possible when interaction effects are included in any analysis, which greatly increases the risk of false positives that can be nominally significant but do not represent true insight. Reference Munafo and Flint36 To prevent this, the present study was developed with a priori hypothesis that guides the choice of the gene and the polymorphism and the environmental risk factor. Furthermore, several reasons were considered to explain why gene–environment interactions might be expected in the relationship between childhood adversity and psychosis. Human development is an environmentally dependent process in which individuals need to adapt to environmental hazards. However, it is implausible that genetic variants do not contribute to individual variation in response to the environment, since this response is associated with pre-existing individual differences in temperament, personality and psychophysiology, all of which are known to be under a certain degree of genetic influence. Reference Rutter, Moffitt and Caspi35 In this context, one genetic variant that is a candidate for moderating the association between childhood adversity and psychosis is the BDNF-Val66Met polymorphism. This polymorphism consists of a Val/Met single nucleotide polymorphism at position 66 in the BDNF gene, and it has been identified as a functional polymorphism. Reference Chen, Patel, Sant, Meng, Teng and Hempstead37 The Val variant is associated with higher neuronal BDNF secretory activity than is the Met variant. Additionally, the coexpression of Val and Met alleles in heterozygotes results in less efficient intracellular trafficking and processing, leading to decreased BDNF secretion. Reference Chen, Patel, Sant, Meng, Teng and Hempstead37 The secretion of BDNF is crucial for the growth and differentiation of developing neurons in both central and peripheral nervous systems, and BDNF is also implicated in the survival of neuronal cells in response to stress. Reference Van Winkel, Stefanis and Myin-Germeys1,Reference Chen, Jing, Bath, Ieraci, Khan and Siao7,Reference Chen, Patel, Sant, Meng, Teng and Hempstead37 Evidence from animal studies suggests that individuals carrying the Met/Met genotype are more likely to develop anxiety-related behaviours in response to stressful events. Reference Chen, Jing, Bath, Ieraci, Khan and Siao7 In humans, it has been shown that Met homozygotes and heterozygotes who have experienced childhood adversity could also be more genetically vulnerable to the development of affective symptoms, in comparison to Val homozygotes. Reference Aguilera, Arias, Wichers, Barrantes-Vidal, Moya and Villa8 However, the potential moderating effect of the BDNF-Val66Met polymorphism on the relationship between psychosocial stress and psychosis has not been widely explored. To the best of our knowledge, only Simons and colleagues Reference Simons, Wichers, Derom, Thiery, Myin-Germeys and Krabbendam11 have studied the relationship between minor stressful daily events, the BDNF-Val66Met polymorphism and paranoid experiences. These authors found that BDNF-Met allele carriers showed more social stress-induced paranoia than did individuals with the Val/Val genotype. The present results are in line with these findings. Specifically, we found that the impact of childhood abuse on the development of positive psychotic-like experiences was higher in those individuals carrying the Met allele. This provides evidence of a gene–environment interaction effect, whereby Met carriers would, genetically, be more vulnerable to the effects of childhood abuse than would Val homozygotes.
We believe that these findings are consistent with the hypothesised affective pathway to psychosis, which has been suggested to be preferentially underlying the positive symptoms of psychosis. Reference Van Winkel, Stefanis and Myin-Germeys1 As mentioned earlier, childhood adversity has been shown to alter the functioning of the HPA axis, which is one of the most important brain circuits involved in regulating adaptive responses to stress. In this context, the intrusive nature of abusive experiences may indicate that they are especially likely to dysregulate the HPA axis. This dysregulation would, in turn, result in increased dopamine release in mesolimbic brain areas, which has been frequently related to the expression of positive psychotic symptoms. Reference Van Winkel, Stefanis and Myin-Germeys1,Reference Bendall, Jackson, Hulbert and McGorry2
In summary, our results indicate that individuals carrying the Met allele, the variant associated with less BDNF secretion, would be more vulnerable, neurobiologically speaking, to the negative effects of early abusive experiences.
Strengths and limitations
Among the strengths of the present study it is worth noting that the results were not confounded by the effect of schizotypal personality traits, trait anxiety or cannabis use. Thus, the findings indicate that exposure to childhood abuse increases the risk of reporting adult psychotic-like experiences independently of any pre-existing schizotypal traits, which have also been shown to increase the likelihood of experiencing psychotic symptoms. Reference Barrantes-Vidal, Lewandowski and Kwapil18 Similarly, although the use of cannabis is a well-known environmental risk factor for psychotic-like experiences, Reference Arseneault, Cannon, Witton and Murray38 this did not confound the present results as the frequency of cannabis use was controlled for. As regards the inclusion of trait anxiety as a confounder, it has been found that the strong emotions associated with childhood adversity, such as anxiety and memories of the earlier experience, contribute to an increased risk of later psychotic symptoms. Reference Freeman and Garety39 However, as trait anxiety was controlled for, we can rule out the possibility that the occurrence of psychotic-like experiences was linked to the anxiety associated with abusive events experienced in childhood. Overall, the present research design follows the recommendations of a systematic and critical review by Bendall et al Reference Bendall, Jackson, Hulbert and McGorry2 in that it includes confounders based on previous research into childhood adversity and psychosis.
Despite these strengths, the present study does have a number of limitations. First, the cross-sectional design prevents a robust test of causal associations, although a priori hypotheses were clearly defined and guided all the subsequent analyses as mentioned earlier. Second, the retrospective measure of childhood adversity may constitute an inherent source of bias. That said, the CTQ has been validated and is considered a reliable measure of childhood adversity, Reference Bernstein, Stein, Newcomb, Walker, Pogge and Ahluvalia15 as well as being recommended in the critical review by Bendall and colleagues Reference Bendall, Jackson, Hulbert and McGorry2 as a reliable tool for measuring childhood abuse. Third, although the current findings are in line with those reported by Simons et al, Reference Simons, Wichers, Derom, Thiery, Myin-Germeys and Krabbendam11 the studies are not directly comparable since the outcomes and environmental risk factors analysed were different. Studies examining similar hypothesis but that differ in the exact variables analysed or the instruments used to measure such variables can also account for inconsistencies in the results and therefore, failure to replicate. Fourth, although the sample size is similar to that used in previous and similar studies, Reference Kelleher, Harley, Lynch, Arseneault, Fitzpatrick and Cannon4,Reference Simons, Wichers, Derom, Thiery, Myin-Germeys and Krabbendam11 it can be still considered relatively small. In the light of these limitations, our findings should be considered with caution and need replication in larger samples.
Implications
Our findings suggest a specific relationship between childhood abuse and positive psychotic-like experiences in the general population. The results also provide evidence for a gene–environment interaction effect underlying individual behavioural differences in response to childhood abuse; specifically, Met carriers are more likely to report positive psychotic-like experiences in the presence of childhood abuse compared with Val homozygotes. These results now require replication as they may have important implications for future research into the aetiological mechanisms operating between childhood adversity and later psychosis.
Funding
This study was supported through research projects funded by the Ministry of Science and Innovation ( and ) and the Institute of Health Carlos III, CIBER of Mental Health (CIBERSAM) and also by the Comissionat per a Universitats i Recerca del DIUE of the Generalitat de Catalunya (). S.A. thanks the Institute of Health Carlos III for her PhD grant (FI00272).





eLetters
No eLetters have been published for this article.