Naturalistic follow-up studies of up to 27 years of patients with borderline personality disorder have reported that the overall suicide rate for this group of patients is high (about 9%) and the overall death rate, other than by suicide, is higher than the general population. Little change is seen in affective disturbance over time. Reference McGlashan1–Reference Plakun, Burkhardt and Muller4 Prospective studies, likely to be more reliable than other types of follow-up studies, Reference Gunderson, Shea, Skodol, McGlashan, Morey and Stout5 have raised concerns about the definition and classification of personality disorders and the long-term course of these disorders, Reference Links, Heslegrave and van Reekum6–Reference Skodol, Pagano, Bender, Shea, Gunderson and Yen8 with one study reporting 88% of patients in full remission at 10-year follow-up. Reference Zanarini, Frankenburg, Hennen, Bradford Reich and Silk7 Follow-up studies of patients that have been treated with specific psychological therapies in randomised controlled trials (RCTs) are relatively rare and tend to be relatively short term to date, although good outcomes have been reported. Reference Bateman and Fonagy9,Reference Chiesa, Fonagy and Holmes10 We previously reported the findings of an RCT of 106 patients with borderline personality disorder who participated in the BOSCOT (Borderline Personality Disorder Study of Cognitive Therapy) trial. Patients were randomised to 30 sessions of individual cognitive–behavioural therapy for personality disorders (CBT–PD) over 1 year in addition to their usual treatment or to treatment as usual (TAU) alone. Reference Davidson, Norrie, Tyrer, Gumley, Tata and Murray11–Reference Davidson14 At 1-year post-therapy, CBT–PD was superior to TAU in terms of a reduction in suicidal acts, anxiety, positive symptom distress and dysfunctional beliefs. Mean total costs per patient in the (CBT–PD) group were also lower than for patients receiving TAU.
We now report the 6-year follow-up of patients from the original BOSCOT trial that took place in three centres across the UK (trial registration: ISRCTN86177428). We examined:
-
(a) longer-term outcome of BOSCOT participants who met criteria for borderline personality disorder in 2002, half of whom were scheduled to receive 30 sessions of CBT–PD in addition to TAU;
-
(b) longer-term stability of a diagnosis of borderline personality disorder in a UK-treated sample and change in diagnostic criteria;
-
(c) prognostic indicators of good and poor outcome;
-
(d) the economic impact of borderline personality disorder on health and social services over 6 years.
Our expectation was that all patients would have continued to improve over time and that there would not be a differential treatment effect in favour of CBT–PD over the average follow-up period of 6 years.
Method
The follow-up study received ethical approval in each of the three centres. The ethics committees originally restricted the number of letters inviting potential participants to attend a follow-up interview to two. Later, permission was given to extend the number of letters to three.
Tracking and randomisation
Regardless of randomised treatment group or attendance at therapy, all participants who attended a final assessment by research assistants at 24 months post-randomisation (or 1 year after the end of the randomised intervention period) in the BOSCOT study were given the opportunity to sign a record form that would give permission to the research team to contact them ‘at some point in the future’ for follow-up. Participants were not committing to take part in the follow-up; rather they were agreeing to be invited to participate. Of the 106 individuals originally randomised, 1 had died of natural causes, 2 people declined to sign the form and a further 8 withdrew consent for contact, leaving 95 available for tracking. Death registers the General Register Office for Scotland and the National Statistics Office in England were checked twice during the follow-up period (in October 2007 and October 2008), revealing two deaths. This resulted in the possible follow-up of 93 participants. Contact details were traced for all the remaining 93 potential participants. Overall, 8 participants declined follow-up and 9 did not respond, resulting in 76 participants interviewed (n = 76/93, 82%). This is 72% of the original 106 BOSCOT participants. We offered payment of £25 to all participants as part of the protocol to attend the follow-up interview.
Follow-up interview and measures
The study used the same measures as the original BOSCOT study. Reference Davidson, Norrie, Tyrer, Gumley, Tata and Murray11,Reference Davidson, Tyrer, Gumley, Tata, Norrie and Palmer12 All measures were administered in one appointment in mental health resource centres or in the participant's home if the participant preferred. Appointments lasted about 2 h and all participants had previously given informed written consent.
To determine the remission rate of borderline personality disorder, participant's diagnostic status was measured by the Structured Clinical Interview for DSM–IV Axis II Personality Disorders (SCID–II). Reference First, Gibbon, Spitzer, Williams and Benjamin15 One assessor (H.T.) was a senior clinician, highly experienced in using the SCID–II. The other assessors were graduate psychologists, were trained by a senior member of the team to administer the SCID–II. Diagnostic assessments made by the graduate psychologists were reviewed by senior clinicians, masked to the patient's details.
Acts of self-harm or suicide were measured using the Acts of Deliberate Self-Harm Inventory. Reference Davidson14 This is a structured interview measure which asks participants to recall suicide attempts or events of self-harm, in this instance since the date of their 24-month appointment. When the patient had not been seen at 24 months, the period covered was from the planned date of the 24-month appointment.
To determine the extent of current psychiatric symptoms, the Beck Depression Inventory (BDI), Reference Beck, Steer and Brown16 Spielberger State–Trait Anxiety Inventory (STAI) Reference Spielberger, Gorsuch and Lushene17 and Brief Symptom Inventory (BSI) Reference Derogatis18 were employed. Participant's beliefs thought to be related to personality disorder were measured using the Young Schema Questionnaire (YSQ). Reference Young19 Social functioning was measured by the Social Functioning Questionnaire (SFQ) Reference Tyrer, Nur, Crawford, Karlsen, McLean and Rao20 and the Inventory of Interpersonal Problems – Short form 32 (IIP–32). Reference Horowitz, Alden, Wiggins and Pincus21
The costing analysis was undertaken from a broad perspective to evaluate the impact of the treatment on a number of different parties, including patients, the National Health Service (NHS), Social Services and other providers of care. The main health outcome for the cost-effectiveness analysis was the quality-adjusted life-year (QALY), assessed using the EuroQol (EQ–5D), 22 and the Client Service Receipt Inventory (CSRI) Reference Knapp and Beecham23 for the 6 months before follow-up interview. The EQ–5D questionnaire is a standardised generic instrument for measuring health-related quality of life and now forms part of the Reference Case for cost-effectiveness studies submitted to the National Institute for Health and Clinical Excellence (NICE) in the UK. Reference Brazier, Tumur, Holmes, Ferriter, Parry and Dent-Brown24 Data on treatment from the end of the original trial to follow-up date were also obtained using hospital records. These data provide information on in-patient and out-patient treatment across the period from year 2 to 6 years. A sample of case notes (10%) was cross-checked for accuracy by an independent assessor and no discrepancies were noted.
Masking
The research assistants did not know to which treatment group participants had been allocated in the BOSCOT trial.
Statistical analysis
All analyses presented follow the intention-to-treat principle (participants were analysed according to their original randomised allocation, irrespective of treatments received post-randomisation). Since we could only analyse individuals who were alive at 6 years, consented to follow-up, and were contactable and provided usable data, this is a modified intention-to-treat analysis of 76 of the original 106 randomised participants. The same statistical methodology is described in the analysis of the main BOSCOT results. Reference Davidson, Norrie, Tyrer, Gumley, Tata and Murray11 In brief, the difference between the randomised groups for the outcome of number of suicide attempts was modelled using a repeated measures linear model (main effects models, with treatment group and time as fixed effects, and participant as a random effect, with adjustment for pre-specified baseline (pre-randomisation) covariates, were used after first checking for a treatment × time interaction). The baseline covariates used in the adjustment were the same as those specified in the original study. Reference Davidson, Norrie, Tyrer, Gumley, Tata and Murray11 This model was also the basis of the prognostic model for the number of suicide attempts. The binary outcome of suicidal attempts (Yes/No) was modelled using logistic regression. The impact of missing data was explored using Rubin's multiple imputation strategy under an assumption of data missing at random. There was no adjustment for multiple comparisons and, given the large number of comparisons made on the secondary outcomes, this should be borne in mind when interpreting the tests of significance for individual items. A 0.05 level of significance was used throughout. All statistical analyses were conducted using SAS 9.0.1 for Windows (SAS Institute, Cary, North Carolina, USA).
Results
The 76 participants' average length of follow-up was 5.82 years (range 5.4–6.4) from baseline. There was no statistical difference in follow-up rates between the CBT–PD and TAU groups (n = 43/54, 80% v. n = 33/52, 63% respectively; Fisher exact test P = 0.085). Of the two patients who had died by suicide during the follow-up period, one had been randomised to CBT–PD and the other to TAU. The patient who died of natural causes during the trial had been in the TAU group. Only three patients received further CBT during the follow-up period (i.e. in years 3–6). It is unlikely that this was CBT–PD as specified in our original protocol. No other patients reported or, from information gathered from case notes, received formal psychotherapy during the follow-up period except for one patient who had received CBT–PD, who then attended a mentalisation-based therapy programme at a day hospital followed by out-patient follow-up and support.
Cohort baseline and follow-up characteristics
Patients' baseline characteristics have been described previously. Reference Davidson, Tyrer, Gumley, Tata, Norrie and Palmer12 In brief, the average age of the 106 patients randomised was 32 years, 84% were female, 80% had never married, about half had left school at 16 and all were of White ethnicity. The mean (s.d.) time spent in psychiatric hospital in the 12 months prior to baseline was 24.2 (47.5) days and the mean (s.d.) number of years since first act of self-harm was 14.8 (10.0) years. Just under half of the sample (47%) had contact with legal or law enforcement agencies in the 6 months prior to randomisation. Overall, 36% of participants were reported as living alone, 68% were unemployed and 84% were receiving benefits, with about half of these receiving a severe disablement allowance. For those with 6-year follow-up described in this paper, there were no statistically significant differences evident between the randomised groups (n = 43 CBT–PD and n = 33 TAU) in terms of baseline characteristics.
Suicide attempts
In the original RCT, the CBT–PD intervention took place over the first 12 months post-randomisation, after which there was an additional 12 months of follow-up. Table 1 provides information on the number of suicide attempts for the total periods under consideration (i.e. years 1, 2 and 6 cumulatively). The original treatment effect is maintained over an average of 6 years follow-up: a difference of 1.26 suicide attempts over the following 5 years (95% CI –0.06 to 2.58), with the extra variability in the data meaning this change is just failing to achieve statistical significance at P = 0.061 (using an analysis adjusted for baseline covariates). The 6-year follow-up group of 76 patients had very similar results at 2 years, with a treatment effect in favour of CBT–PD of 1.18 suicide attempts over 2 years, significant at P = 0.0085 (for the whole cohort the treatment effect was 0.93 suicide attempts).
Table 1 Number of suicide attempts at 1, 2 and 6 years (cumulative averages over entire period specified)

| Time | TAU (n = 33): mean (s.d.) | CBT–PD (n = 43): mean (s.d.) | Adjusteda mean difference TAU – CBT–PD (95% CI) | P |
|---|---|---|---|---|
| 1 year | 1.22 (2.67) | 0.69 (1.14) | 0.47 (–0.15 to 1.10) | 0.13 |
| 2 years | 2.09 (3.58) | 0.93 (1.58) | 1.18 (0.31 to 2.06) | 0.0085 |
| 6 years | 3.03 (4.16) | 1.88 (3.19) | 1.26 (–0.06 to 2.58) | 0.061 |
In addition, we examined whether those in the CBT–PD group were more likely to have no suicide attempts compared with those in the TAU group. Over the 6-year period, 73% (n = 24/33) in the TAU group had made at least one suicide attempt compared with 56% (n = 24/43) in the CBT–PD group (adjusted odds ratio 0.37, 95% CI 0.10–1.38, P = 0.13) This is an observed 17% absolute decrease (23% relative reduction) in the number of individuals attempting suicide in favour of the CBT–PD group. However, owing to the small numbers, the confidence interval around this fall is wide, and it is not a statistically significant finding.
In terms of self-harm (non-suicidal) there was little evidence of a difference between the groups. However, it was clear that the overall rate of self-harm declined in both groups, from an average of 4.88 episodes per month in the first year to about 1.10 per month in the following 5 years.
Other clinical outcome measures
For measures of depression, anxiety, general psychopathology, social functioning, quality of life and dysfunctional attitudes, there were no statistically significant differences between the groups during follow-up (Table 2). Considering the data without respect to randomised treatment, in aggregate they show the natural history of participants with a diagnosis of borderline personality disorder over 6 years. In general, there was improvement in these measures.
Table 2 Other clinical outcomes (baseline and 6-year follow-up)a

| CBT–PD (n = 43): mean (s.d.) | TAU (n = 33): mean (s.d.) | Adjusted mean difference CBT–PD–TAU (95% CI) | ||||
|---|---|---|---|---|---|---|
| Outcome | Baseline | 6 years | Baseline | 6 years | P b | |
| BDI total | 42.6 (10.1) | 26.5 (16.5) | 43.2 (10.1) | 26.2 (17.5) | –0.58 (–8.45 to 7.29) | 0.88 |
| BSI global severity | 2.68 (0.57) | 1.75 (1.02) | 2.38 (0.80) | 1.68 (1.09) | –0.24 (–0.70 to 0.23) | 0.32 |
| EQ–5D thermometer | 40.6 (19.9) | 53.3 (22.4) | 50.6 (24.4) | 56.2 (25.6) | 1.76 (–9.74 to 13.2) | 0.76 |
| EQ–5D weighted HSV | 0.46 (0.37) | 0.52 (0.38) | 0.54 (0.37) | 0.61 (0.37) | –0.05 (–0.22 to 0.12) | 0.58 |
| IIP–32 total | 72.4 (15.1) | 53.1 (23.7) | 64.9 (16.5) | 48.7 (24.6) | –3.12 (–14.5 to 8.23) | 0.58 |
| SFQ total | 15.3 (4.14) | 10.3 (4.98) | 15.1 (3.80) | 11.2 (5.00) | –1.07 (–3.49 to 1.36) | 0.38 |
| State–Anxiety total | 54.9 (12.5) | 45.7 (13.5) | 51.9 (11.9) | 48.2 (13.0) | –5.29 (–11.3 to 0.69) | 0.082 |
| Trait–Anxiety total | 66.1 (7.87) | 55.1 (13.3) | 65.2 (7.42) | 56.5 (13.6) | –4.13 (–9.64 to 1.37) | 0.14 |
| Youth Schema Questionnaire | ||||||
| Total | 4.07 (0.60) | 3.09 (1.03) | 3.77 (0.76) | 3.16 (1.12) | –0.28 (–0.89 to 0.32) | 0.35 |
| Emotional deprivation | 4.60 (1.15) | 3.76 (1.41) | 3.98 (1.58) | 3.44 (1.45) | 0.13 (–0.52 to 0.77) | 0.70 |
| Abandonment | 4.57 (1.29) | 3.09 (1.47) | 4.53 (1.38) | 3.47 (1.94) | –0.59 (–1.41 to 0.24) | 0.16 |
| Mistrust/abuse | 4.79 (1.00) | 3.73 (1.61) | 4.42 (1.61) | 3.68 (1.81) | –0.26 (–0.99 to 0.47) | 0.48 |
| Social isolation | 4.80 (1.04) | 3.49 (1.60) | 4.27 (1.39) | 3.78 (1.75) | –0.71 (–1.43 to 0.00) | 0.051 |
| Defective/shame | 4.40 (1.08) | 3.13 (1.20) | 4.05 (1.15) | 3.48 (1.30) | –0.54 (–1.10 to 0.02) | 0.058 |
| Failure | 4.22 (1.61) | 2.98 (1.63) | 4.06 (1.59) | 3.54 (1.76) | –0.63 (–1.37 to 0.12) | 0.10 |
| Dependence/incompetence | 3.91 (1.27) | 2.94 (1.34) | 3.49 (1.14) | 3.07 (1.40) | –0.36 (–1.00 to 0.27) | 0.26 |
| Vulnerable harm/illness | 4.23 (1.22) | 3.36 (1.64) | 3.94 (1.34) | 3.45 (1.60) | –0.28 (–1.04 to 0.49) | 0.47 |
| Enmeshment | 2.31 (1.47) | 1.90 (1.22) | 2.47 (1.41) | 1.86 (1.07) | 0.27 (–0.34 to 0.88) | 0.37 |
| Subjugation | 4.18 (1.16) | 2.95 (1.31) | 3.90 (1.29) | 3.42 (1.69) | –0.63 (–1.31 to 0.04) | 0.067 |
| Self-sacrifice | 4.00 (1.40) | 3.62 (1.40) | 3.88 (1.45) | 3.67 (1.27) | –0.14 (–0.68 to 0.40) | 0.61 |
| Emotional inhibition | 3.96 (1.36) | 3.21 (1.43) | 3.64 (1.44) | 3.25 (1.51) | –0.12 (–0.78 to 0.54) | 0.72 |
| Unrelenting standards | 4.08 (1.28) | 3.49 (1.39) | 3.86 (1.43) | 3.83 (1.34) | –0.52 (–1.12 to 0.09) | 0.092 |
| Entitlement | 2.96 (1.10) | 2.68 (1.13) | 2.29 (1.14) | 2.36 (1.14) | –0.07 (–0.62 to 0.48) | 0.80 |
| Insufficient self-control | 4.50 (1.26) | 3.22 (1.53) | 4.01 (1.43) | 3.25 (1.46) | –0.05 (–0.80 to 0.71) | 0.90 |
Change in diagnosis
At 6 years, 54% of the sample no longer met diagnostic criteria for borderline personality disorder: 56% (n = 24/43) of the CBT–PD group and 52% (n = 17/33) of the TAU group. There was no difference between the groups in terms of those who continued to meet diagnostic criteria (P = 0.44). Figure 1 illustrates the percentage change in the individual criteria for borderline personality disorder diagnosis for the group as a whole.
Prognostic indicators of good and poor outcome
Defining poor outcome as any suicide attempt in the follow-up period, we examined the baseline predictors of good and poor outcome (Table 3). From all the variables known to be of prognostic importance pre-randomisation, only having special needs at school was specifically associated with the presence of any suicide attempts during the 6-year follow-up.
Table 3 Baseline (pre-randomisation) predictors of any suicide attempt (yes/no) at any time in the extended study period of 6 yearsa

| Covariate | Odds ratio | 95% CI | P |
|---|---|---|---|
| Treatment (CBT–PD v. TAU) | 0.37 | 0.10–1.38 | 0.14 |
| Number of suicide attempts in 12 months prior to randomisation | 1.42 | 0.90–2.23 | 0.13 |
| Age at randomisation | 0.98 | 0.91–1.06 | 0.65 |
| Age at first self-harm | 1.09 | 0.98–1.20 | 0.10 |
| Female | 1.85 | 0.34–10.2 | 0.48 |
| Single | 0.32 | 0.06–1.91 | 0.21 |
| Left school at 16 | 1.45 | 0.37–5.76 | 0.60 |
| Special needs | 10.2 | 1.56–67.3 | 0.015 |
| Lives alone | 1.16 | 0.30–4.43 | 0.83 |
| Been involved with police | 0.96 | 0.26–3.53 | 0.96 |
| Unemployed | 2.94 | 0.77–11.3 | 0.12 |
| Self-harm (high v. low) | 3.42 | 0.67–17.4 | 0.14 |
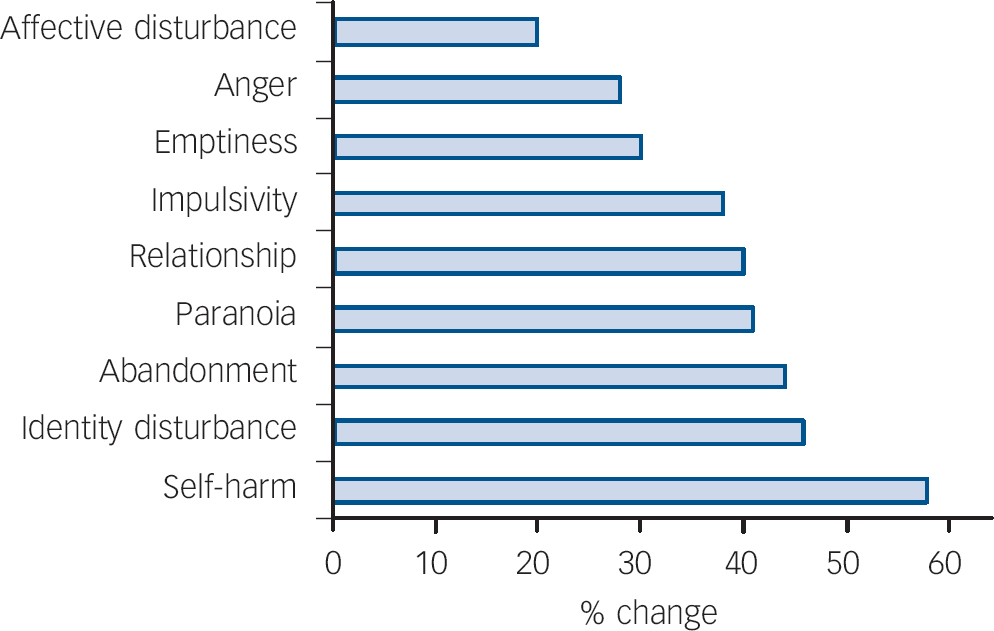
Fig. 1 Percentage change in borderline personality disorder criteria endorsed from baseline to 6-year follow-up.
Economic impact of borderline personality disorder on the NHS/Social Services over 6 years
Overall quality of life scores for the entire group remained poor and continued to lie within a similar range to values reported for other severe mental health populations such as severe schizophrenia (mean EQ–5D scores at 6 years: 0.56, s.d. = 0.38). On average, patients in the CBT–PD group continued to report a slightly lower quality of life than the TAU group at 6-year follow-up. However, the difference between the two groups remained small and did not approach conventional levels of statistical significance, regardless of whether an adjustment was made for baseline EQ–5D scores. The mean differences reported at 6-year follow-up between the groups were virtually identical to those reported at 2-year follow-up. Overall quality of life scores remained higher than the baseline measurements reported at the start of the main BOSCOT study, suggesting that some of the improvement in EQ–5D scores reported during the 24-month BOSCOT study were maintained over the longer-term follow-up.
Service utilisation and costs (illustrating usual NHS treatment)
The treatment patients received over the 6-year follow-up, with details of the number of contacts patients had with services during this period by treatment group and the associated cost, is described in Tables 4 and 5. This represents usual treatment (TAU) that is delivered by the NHS. Information on pharmacotherapy was not obtained. Both groups received a range of mental health and general practitioner services. Use of hospital services remained high in both groups with about 54% of all individuals having received in-patient treatment and almost two-thirds having utilised accident and emergency (A&E) treatment during the follow-up period. With the exception of in-patient and A&E utilisation, no particularly large differences were observed between the treatment groups. However, the mean length of hospitalisation was markedly lower in the CBT–PD group than for the TAU group (10.81 v. 60.97 days respectively). Although a similar proportion of patients in both groups attended A&E, both the mean and median number of attendances were higher in the TAU group, a difference that was not evident during the main BOSCOT study.
Table 4 Follow-up resource utilisation by group

| TAU | CBT–PD | Unit cost or range, £ | ||||||
|---|---|---|---|---|---|---|---|---|
| Service | Mean (s.d.) | Median (IQR) | Used by, % | Mean (s.d.) | Median (IQR) | Used by, % | Unit | |
| Hospital services | ||||||||
| In-patient | 60.97 (180.59) | 1 (0–16) | 51 | 10.81 (19.29) | 1 (0–11) | 56 | Day | 219–659 |
| Out-patient | 13.21 (14.51) | 11 (0.5–21.5) | 76 | 13.49 (18.02) | 9 (1–19) | 86 | Attendance | 55–148 |
| Day hospital | 7.15 (25.42) | 0 (0–0) | 12 | 4.79 (31.41) | 0 (0–0) | 2 | Attendance | 84–86 |
| Emergency room | 8.12 (24.22) | 3 (0–4) | 64 | 3.91 (7.67) | 1 (0–4) | 65 | Attendance | 69–79 |
| Community day servicesa | ||||||||
| Day care centre | 0.21 (1.22) | 0 (0–0) | 3 | 0.23 (1.23) | 0 (0–0) | 7 | Day | 33 |
| Drop-in centre | 3.3 (13.12) | 0 (0–0) | 15 | 6.35 (19.73) | 0 (0–0) | 19 | Session | 21 |
| Sheltered workshop | 0 (0–0) | 0 (0–0) | 0 | 0.60 (3.97) | 0 (0–0) | 2 | Attendance | 43 |
| Primary and communitya | ||||||||
| GP (surgery visit) | 4.82 (5.84) | 3 (1.5–5.5) | 97 | 5.71 (6.65) | 3 (1–10) | 95 | Visit | 19 |
| GP (home visit) | 0.91 (3.59) | 0 (0–0) | 18 | 0.65 (3.07) | 0 (0–0) | 16 | Visit | 59 |
| Practice nurse | 3.88 (11.35) | 1 (0–2) | 58 | 2.12 (4.28) | 1 (0–2) | 54 | Visit | 14 |
| Counsellor | 0.12 (0.55) | 0 (0–0) | 6 | 0.84 (3.93) | 0 (0–0) | 7 | Visit | 33 (per hour) |
| District nurse | 2.73 (15.67) | 0 (0–0) | 3 | 0.02 (0.15) | 0 (0–0) | 2 | Visit | 20 |
| CPN/case manager | 2.91 (5.58) | 0 (0–4) | 33 | 3.21 (5.86) | 0 (0–5) | 37 | Visit | 28 |
| Social worker/care manager | 2.06 (6.05) | 0 (0–0.5) | 24 | 1.42 (4.57) | 0 (0–0) | 19 | Visit | 89 (per hour) |
| Occupational therapist | 0.91 (4.21) | 0 (0–0) | 9 | 0.63 (2.59) | 0 (0–0) | 9 | Visit | 35 |
| Advocate | 0.12 (0.70) | 0 (0–0) | 3 | 0.09 (0.48) | 0 (0–0) | 5 | Visit | 20–35 |
| Home help/care worker | 5.18 (20.99) | 0 (0–0) | 6 | 0.63 (3.67) | 0 (0–0) | 7 | Visit | 7 |
| Other | 26.67 (94.60) | 4 (1–13) | 82 | 7 (12.55) | 3 (1–6) | 79 | Visit | 7–35 |
| Accommodation,a community (non-hospital) | 5.52 (31.68) | 0 (0–0) | 3 | 4.23 (27.75) | 0 (0–0) | 2 | Day | 69 |
| Criminal justice servicesa | ||||||||
| Arrests | 0.09 (0.29) | 0 (0–0) | 9 | 0.05 (0.21) | 0 (0–0) | 5 | Arrest | 1353 |
| Magistrate Court | 0.30 (1.10) | 0 (0–0) | 12 | 0.12 (0.76) | 0 (0–0) | 2 | Appearance | 564 |
| Crown Court | 0 (0–0) | 0 (0–0) | 0 | 0 (0–0) | 0 (0–0) | 0 | Appearance | 9214 |
| Prison services | 0 (0–0) | 0 (0–0) | 0 | 0 (0–0) | 0 (0–0) | 0 | Day | 86 |
Table 5 Follow-up costs by group

| TAU | CBT–PD | Mean difference (95% CI), £ | Adjusteda mean difference (95% CI), £ | |
|---|---|---|---|---|
| £ Mean (s.d.) | £ Mean (s.d.) | |||
| Hospital services | 16 658 (42 425) | 5015 (6150) | –11 643 (–29 401 to –441) | –6731 (–19 792 to 1091) |
| Community day services | 175 (513) | 247 (571) | 72 (–164 to 315) | 49 (–171 to 280) |
| Primary/community care | 1199 (1755) | 885 (850) | –313 (–1012 to 214) | –252 (–978 to 324) |
| Accommodation | 381 (2186) | 292 (1915) | –88 (–1249 to 613) | 387 (–27 to 1219) |
| Criminal justice services | 325 (782) | 142 (563) | –183 (–506 to 106) | –178 (–523 to 112) |
| Total | 18 737 (43 998) | 6582 (6913) | –12 155 (–32 743 to –870) | –6472 (–18 578 to 781) |
Cost of services
The average cost for patients over the course of the follow-up was £11 860 (s.d. = £29 824) for the sample (n = 76) as a whole (Table 5). Costs of all hospital services comprised the largest component of cost. On average, the mean hospital costs incurred by those in the TAU group were higher than in the CBT–PD group (£16 658 v. £5015, mean difference £11 643; 95% CI £441–29 401) over the follow-up period. This is reflected in the difference in total costs for the treatment groups (TAU £18 737 v. CBT £6582, mean difference £12 155; 95% CI £870–£32 743). After adjustment for baseline differences in cost of service use, the magnitude of the mean difference in total costs is smaller, although still in favour of CBT–PD (£6472, 95% CI –£781 to £18 578). However, neither the differences in the cost of hospital services or total costs were found to be statistically significant after adjustment for baseline differences and the associated confidence intervals were large, indicating considerable uncertainty about the central estimates.
Outliers
Examination of resource use of individual patients indicated that two patients had a major influence on the overall mean estimates. Between them, these two individuals (both in the TAU group) accounted for 54% of all in-patient days and 44% of all A&E attendances. Excluding these patients from the analyses changes the pattern of A&E use in favour of TAU (2.39 v. 3.91 for CBT–PD), but the mean length of hospitalisation remains in favour of CBT–PD (10.81 v. 22.10 days for TAU). After adjustment for baseline costs, the differences in mean costs remained nonsignificant. Although the magnitude of these differences was much smaller than the estimates including these patients, the cost estimates were still in favour of CBT–PD (mean difference in cost of hospital services £913, 95% CI –£2802 to £6133; mean difference in total costs £749, 95% CI –£3452 to £6337).
Impact of attrition (loss to follow-up) on the outcome of number of suicide attempts
Of the 106 participants who took part in the original trial, 30 participants did not take part in the longer-term follow-up. Of these, 19 were from the TAU group and 11 from the CBT–PD group. This is not a formally statistically significant difference (Fisher exact test P = 0.085, chi-squared test P = 0.064). Several approaches were utilised to investigate the impact of missing data. The multiple imputation models based on the assumption of data missing at random reproduced the original findings (data available from the authors on request).
Discussion
Comparison with other studies
Just over half the patients who met criteria for borderline personality disorder at entry into the original study no longer did so 6 years later. This finding is similar to those of other longer-term follow-up studies Reference Zanarini, Frankenburg, Hennen, Bradford Reich and Silk7,Reference Skodol, Pagano, Bender, Shea, Gunderson and Yen8 in which patients became less symptomatic over time, no longer meeting criteria but continuing to show serious dysfunction. However, the McLean Study of Human Development that examined the course of borderline personality disorder over 10 years Reference Zanarini, Frankenburg, Hennen, Bradford Reich and Silk7 found that 68.6% of patients no longer met diagnostic criteria at 6 years. Our findings also do not appear as positive in terms of change in diagnosis over 8 years for patients treated with mentalisation-based therapy in a ‘partial hospitalised setting’, Reference Bateman and Fonagy9 but ours was a larger group of patients who were likely to show more variability and received only 1 year of therapy. The differences in percentage recovered between studies may reflect real differences in how the cohorts or randomised groups have been treated or may reflect differences in sample characteristics or natural variability in the course of the disorder. All our patients had received either in-patient psychiatric services or an assessment in A&E, or had self-harmed (either suicidal act or self-mutilation) in the previous 12 months. Very few patients received further psychological therapy following the CBT–PD offered during the trial and we can therefore be relatively certain that the effects seen are due to the original therapy in combination with the natural course of the disorder. In addition, compared with those who received TAU, the patients who received CBT–PD continued to show a greater reduction in the number of in-patient days and suicidal acts over the 6-year follow-up. There are two ways to interpret this finding. First, there is no evidence that the CBT–PD delivered in the first 12 months accrues additional benefit in years 3–6, or second, there is evidence that the benefit accrued in the first 2 years is not dissipated in years 3–6. That is, there is no rebound effect and no indication that the good achieved has been undone, with the participants given CBT–PD deteriorating over time. We argue that this is consistent with CBT–PD producing a lasting benefit in those responding to CBT–PD, with another subgroup who did not benefit from CBT–PD. Having special needs at school was predictive of carrying out any suicidal act over the 6-year period. This group (18% of the original group) may require more treatment and support in the longer term.
Course of borderline personality disorder
The findings add to the evidence that the course of borderline personality disorder is better than previously recognised, even for those who have received extensive hospitalisation and were suicidal 6 years before. Although we found that three people had died, two by suicide, just over half of our sample no longer met diagnostic criteria for the disorder at 6-year follow-up. The gains of the CBT–PD over the TAU group in reduction of suicidal behaviour seen after 1 year were maintained at 6 years, and the cost of in-patient care was three times less in the CBT–PD than the TAU group. The savings in costs contrast with data from a related study, Prevention Of Parasuicide with Manual Assisted Cognitive behaviour Therapy (POPMACT), in which patients with borderline personality disorder treated with a brief form of CBT had greater costs associated with this treatment after 1 year than those with other personality disorders. Reference Tyrer, Tom, Byford, Schmidt, Jones and Davidson25 The better results obtained with the more intensive CBT specific to personality disorder (CBT–PD) support the recommendations of the recently published guidelines on the treatment of borderline personality disorder from NICE that short-term psychotherapy is not appropriate for borderline personality disorder but that a more structured long-term treatment is preferable. 26 The cost per patient in the CBT–PD group also compared well with the equivalent costs of other forms of psychotherapy for borderline personality disorder even when allowing for the longer period of study. Reference van Asselt, Dirksen, Arntz, Giesen-Bloo, van Dyck and Spinhoven27
Although our design did not allow investigation of mechanisms of change with therapy, cognitive change was evident at 1-year post-treatment in that there was a highly significant difference between the groups in terms of dysfunctional beliefs (P = 0.0064). Reference Davidson, Norrie, Tyrer, Gumley, Tata and Murray11 The YSQ Reference Young19 used to assess patient's beliefs consists of several subscales and differences between the groups were not evident on all of these subscales. At 6 years, the total mean score of the subscales shows no significant difference between the groups. However, we do show that there are trends in terms of continuing differences between the groups on some subscales (social isolation (0.051), defectiveness and shame (0.058) and subjugation (0.067)) suggesting that some differences may continue to be maintained, although these are no longer statistically significantly at 6 years.
As in other follow-up studies, Reference Skodol, Pagano, Bender, Shea, Gunderson and Yen8 we found that CBT–PD altered impulsive behaviours but only a fifth of patients showed improvement in affective disturbance; quality of life remained poor. It may be that 1 year in therapy was not sufficient to alter affective disturbance. Cognitive–behavioural therapy for personality disorder, at least in theory, should be able to alter mood disturbance and this in turn may alter perceived quality of life. Future trials might consider more specifically targeting this following a reduction in self-harming behaviours.
Health costs across follow-up
The use of CBT–PD did not demonstrate a statistically significant cost-effective advantage based on the results of our follow-up study. Although no information on comorbidity or the use of prescription drugs was collated, there are no major imbalances in resource utilisation to suggest that comorbidity or drug prescribing differed either across the original randomised groups or in the subset of the 76 patients who were followed up. However, despite the lack of formal statistical differences reported between the groups, the total costs continued on average to be lower in the CBT–PD group after adjustment for both baseline differences as well as the potential impact of the two high-cost participants. These findings demonstrate the potential for continued long-term cost-offsets that accrue following the initial provision of CBT–PD.
Limitations
No information on comorbidity and prescribed drug use was obtained across the trial and follow-up, and no formal assessment of interrater agreement was carried out on SCID–II diagnosis. In addition, follow-up was not obtained in 30 out of 106 patients. Severe restrictions were placed on the research group by ethics committees in terms of following up patients in the longer term, with only a limited number of invitations to participate being permissible. The sensitivity analyses carried out, using statistical models that assume data were missing at random (multiple imputation), showed that the findings were robust to this pattern of missing data.









eLetters
No eLetters have been published for this article.