The hypothesis that psychological factors influence blood pressure is at least 100 years old. Descriptions of ‘polycythemia hypertonica’ Reference Geisböck1 and of ‘hypertension’ Reference Moschcowitz2 have insinuated that there might be a history of emotional stress behind the origin of these terms. Whether symptoms of anxiety and depression contribute to the development of hypertension has been addressed in several studies, but with inconclusive results. A few studies using change in mean blood pressure as outcome Reference Goldberg, Comstock and Graves3–Reference Shinn, Poston, Kimball, St Jeor and Foreyt7 found mostly no effect.
We recently reported an inverse cross-sectional association of anxiety and depression with blood pressure in a large, community-based population. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 We designed the present study to estimate prospectively the effect of anxiety and depression on change in blood pressure 11 years later within the same population.
Method
Participants
In the Nord-Trøndelag Health Study (HUNT study), all inhabitants in the county of Nord-Trøndelag aged 20 years and older were invited to participate in a general health study that was conducted twice: in 1984–86 (HUNT–1) and 1995–97 (HUNT–2). Data were obtained from physical examinations, blood samples and questionnaires that covered demographic characteristics, somatic illnesses, somatic and mental symptoms, medication, lifestyle and health-related behaviour. Reference Holmen, Midthjell, Bjartveit, Hjort, Lund-Larsen, Moum, Næss and Waaler9,Reference Holmen, Midthjell, Krüger, Langhammer, Holmen, Bratberg, Vatten and Lund-Larsen10
Among participants aged 20–89 years in the two surveys, 60 143 of the HUNT–1 participants and 60 799 of the HUNT–2 participants Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 had valid data on anxiety/depression and blood pressure. These two comparable cross-sectional samples were used for the purpose of cross-validation. The inclusion criteria for our 11-year longitudinal study were valid data on anxiety, depression and blood pressure in both surveys. Of the 60 143 HUNT–1 participants, 57 471 were 20–78 years old; 9708 of these individuals died or moved out of the county during follow-up. Of the remaining 47 763 individuals, 76.5% participated in HUNT–2 with valid data, giving a study population of 36 530 participants aged 20–78 years at baseline (31–89 years old at follow-up). Compared with participants (n=36 530), those who did not complete the study (n=11 233) among eligible individuals were older (51 v. 44 years) and more often men (49.7 v. 47.4%), had higher mean blood pressure (141/86 v. 131/83 mmHg) and higher symptom scores of anxiety/depression (mean z-score=0.07 (s.d.=1.08) v. −0.02 (s.d.=0.97); P<0.001 for all comparisons). However, there was no interaction between age or gender and the association of interest. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 Consequently, we did not expect non-completers to bias our results. The Norwegian Data Inspectorate and The Regional Committee for Ethics in Medical research approved the study.
Measures of anxiety and depression
Twelve questions on anxiety and depression were included in the baseline questionnaire, consisting of a one-dimensional anxiety and depression symptom index (the ADI–12 Index) that correlated strongly (r=0.82) with the Hopkins Symptoms Checklist–25 in a subsample re-examined 2 years after baseline screening. Reference Tambs and Moum11 The test–retest correlation over 2 years for the ADI–12 Index was considered good (r=0.66). Reference Tambs and Moum11 Five of the ADI–12 items corresponded with ICD–10 12 criteria of depressive episode (code F32), and three items corresponded with ICD–10 criteria of generalised anxiety disorder (code F41.1). Two items were related to feelings of being under pressure, one to the use of tranquillisers or sleeping pills, and one to being more aware of responsibilities than others.
The Hospital Anxiety and Depression Scale (HADS) was employed at follow-up. Reference Mykletun, Stordal and Dahl13 The HADS is a self-report questionnaire comprising 14 four-point Likert-scaled items, 7 for anxiety and 7 for depression. Reference Bjelland, Dahl, Haug and Neckelmann14 Cross-sectional analyses in the same population indicated that HADS-defined anxiety and depression, respectively, were similarly associated with blood pressure. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 Consequently, one-dimensional measures for symptoms of anxiety and depression were used at both baseline and follow-up, and z-scores of both measures were used to compare mean symptom levels.
Symptom load of anxiety and depression at baseline was used both as a continuous measure and categorically as a dichotomy with cut-offs at the 90th percentile. Change in symptom load from baseline to follow-up (difference in z-scores between baseline and follow-up) was used as a continuous measure and categorically as 10-percentile groups (0–10, 11–20,… 91–100th percentile). Percentiles above the median indicated a relative increase in symptom load and below the median indicated a relative decrease.
Blood pressure measurements
Specially trained nurses measured blood pressure in seated participants after 4 min (baseline) or 2 min (follow-up), with the cuff placed on the right upper arm and with the arm resting on a table. At baseline, blood pressure was measured using calibrated mercury manometers with standard cuff size. The first pulse sound (Korotkoff's phase I) was registered as systolic blood pressure and the level at which the pulse disappeared (phase V) as diastolic blood pressure. The measurements were repeated after 2 min and the second reading was used in this study. At follow-up, blood pressure was measured with a Dinamap 845XT (Criticon, Florida, USA) based on oscillometry. Cuff size was adjusted after measuring the arm circumference. Blood pressure was measured automatically three times at 1 min intervals. The mean of the second and third reading was used in this study.
Outcome measures
The outcome measures were change in mean systolic or diastolic blood pressure (the participant's blood pressure at follow-up minus blood pressure at baseline), and systolic or diastolic hypotension (defined as age- and gender-stratified blood pressure ≤10th percentile) or hypertension (≥90th percentile) at follow-up. Reasons for using age- and gender-stratified percentiles rather than fixed blood pressure values have been described previously. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8
Statistical analysis
First, we used linear regression models to examine the association of symptom loads of anxiety and depression at baseline and change in symptom load from baseline to follow-up with change in mean systolic or diastolic blood pressure. Effects were reported as unstandardised regression coefficients (B=mmHg per standard deviation increase in symptoms of anxiety and depression at baseline or from baseline to follow-up). Additionally, we performed gender-stratified analyses, and repeated analyses after excluding individuals taking antihypertensive or antidepressant medication. In separate analyses we examined the association between individual anxiety and depression items at baseline and change in blood pressure.
Second, we used logistic regression models to predict systolic or diastolic hypotension (defined as age- and gender-stratified blood pressure ≤10th percentile) at follow-up, when individuals with low systolic or diastolic blood pressure (≤30th percentile) at baseline were excluded. We used separate analyses with anxiety and depression as continuous and categorical measures, as described above. For the purpose of predicting hypertension (blood pressure ≥90th percentile) at follow-up, we excluded individuals with high blood pressure (≥70th percentile) at baseline.
All regression models were adjusted for age (5-year categories as dummy coded variables), gender, education (three levels), and baseline systolic or diastolic blood pressure. In the fully adjusted linear models, we further included hypertension among siblings (dichotomy), angina pectoris, myocardial infarction, stroke, diabetes mellitus (never, follow-up only, or both), smoking status, use of antihypertensive medication (never, baseline only, follow-up only, or both) and body mass index (baseline and change, both continuous).
Third, we displayed graphically the unadjusted association of change in symptom load of anxiety and depression with change in blood pressure. Effects were displayed with 95% confidence intervals.
Finally, for the purpose of cross-validation, we performed cross-sectional analyses applying HUNT–1 data, aiming to replicate the associations previously reported from HUNT–2 data. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 We used logistic regression models with systolic and diastolic blood pressure (encoded in age- and gender-stratified percentiles), and anxiety and depression scores above the 90th percentile both at baseline and follow-up. Data were analysed using SPSS version 14.0 for Windows.
Results
Characteristics of the sample included for longitudinal analyses (n=36 530) are listed in Table 1. Mean systolic blood pressure increased during follow-up, whereas mean diastolic blood pressure remained almost unchanged. The baseline and follow-up measurements correlated strongly for both systolic (r=0.63, P<0.001) and diastolic (r=0.49, P<0.001) blood pressure and for anxiety and depression symptom scores (r=0.46, P<0.001). The changes in anxiety and depression scores, and in systolic and diastolic blood pressure during follow-up, were normally (bell-shaped) distributed.
Table 1 Baseline and 11-year follow-up characteristics of participants (n=36 530)

| Variable | |
|---|---|
| Age at baseline, years: mean (s.d.) | 44.3 (13.8) |
| Men, % | 47.4 |
| Education at baseline, % | |
| ≤9 years | 46.3 |
| 10-12 years | 42.6 |
| ≥13 years | 11.1 |
| Medical history, % | |
| Angina pectoris | |
| Baseline and follow-up | 1.9 |
| Follow-up only | 6.0 |
| Myocardial infarction | |
| Baseline and follow-up | 0.9 |
| Follow-up only | 3.9 |
| Stroke | |
| Baseline and follow-up | 0.5 |
| Follow-up only | 2.2 |
| Diabetes mellitus | |
| Baseline and follow-up | 1.0 |
| Follow-up only | 3.4 |
| On antihypertensive medications, % | |
| Baseline only | 1.2 |
| Follow-up only | 8.4 |
| Both | 5.1 |
| On antidepressant medications,a % | |
| Follow-up only | 3.3 |
| Hypertension among siblings, % | |
| Baseline only | 12.3 |
| Smokers, % | |
| Baseline only | 9.2 |
| Follow-up only | 4.0 |
| Both | 22.4 |
| Blood pressure, mmHg: mean (s.d.) | |
| Baseline | |
| Systolic | 131.2 (19.2) |
| Diastolic | 82.6 (11.0) |
| Change from baseline to follow-up | |
| Systolic | 9.6 (18.1) |
| Diastolic | -0.3 (11.7) |
| Body mass index, kg/m2: mean (s.d.) | |
| Baseline | 24.9 (3.6) |
| Change from baseline to follow-up | 1.8 (2.3) |
Effect of anxiety and depression at baseline
Baseline anxiety and depression predicted a relative decrease in blood pressure. Baseline level of anxiety and depression was associated with a decrease in mean systolic (B=–0.32, P<0.001) and diastolic (B=–0.17, P=0.002) blood pressure. The associations were similar in men and women, and further adjustment for the other covariates listed in Table 1 did not change the results (data not shown). Excluding individuals on antidepressant medication did not reduce the decrease in systolic (B=–0.32, P<0.001) and diastolic (B=–0.18, P=0.001) blood pressure. When individuals on antihypertensive medication were excluded, the corresponding values were B=–0.41, P<0.001 and B=–0.18, P=0.002.
In logistic regression models where individuals with low systolic or diastolic blood pressure (<30th percentile) at baseline were excluded, anxiety and depression predicted hypotension (blood pressure <10th percentile) 11 years later (Table 2). Similar findings were obtained without any exclusions and when individuals below the 10th, 20th, 40th or 50th percentiles were excluded (results not shown); however, the highest odds ratios were observed when individuals with baseline systolic or diastolic blood pressure <30th percentile were excluded (Table 2). Conversely, after similar successive exclusions of individuals with high baseline blood pressure, we did not find anxiety and depression significantly associated with hypertension (blood pressure >90th percentile) at follow-up, except for diastolic blood pressure when individuals with baseline diastolic blood pressure >70th percentile were excluded (Table 3).
Table 2 Relationship between baseline anxiety/depression and low blood pressure at follow-up after exclusion of participants with baseline hypotensiona

| Low systolic blood pressure (<10th percentile)b at follow-up | Low diastolic blood pressure (<10th percentile)b at follow-up | |||||
|---|---|---|---|---|---|---|
| ORc | 95% CI | P | ORc | 95% CI | P | |
| Baseline anxiety/depression score | ||||||
| Continuous measure (per s.d. increase) | 1.10 | 1.04-1.17 | 0.001 | 1.07 | 1.01-1.12 | 0.015 |
| ≥90th percentile | 1.30 | 1.08-1.57 | 0.005 | 1.14 | 0.96-1.36 | 0.129 |
Table 3 Relationship between baseline anxiety/depression and high blood pressure at follow-up after exclusion of participants with baseline hypertensiona

| High systolic blood pressure (>90th percentile)b at follow-up | High diastolic blood pressure (>90th percentile)b at follow-up | |||||
|---|---|---|---|---|---|---|
| ORc | 95% CI | P | ORc | 95% CI | P | |
| Baseline anxiety/depression score | ||||||
| Continuous measure (per s.d. increase) | 0.98 | 0.92-1.04 | 0.445 | 0.95 | 0.90-1.00 | 0.059 |
| ≥90th percentile | 0.91 | 0.75-1.11 | 0.358 | 0.83 | 0.69-0.99 | 0.041 |
Effect of change in anxiety and depression
Change in symptom load of anxiety and depression from baseline to follow-up was inversely associated with change in mean systolic (B=–0.34, P<0.001) and diastolic (B=–0.12, P=0.026) blood pressure. In the fully adjusted models, the effect was weaker for systolic (B=–0.27, P=0.001) and not statistically significant for diastolic blood pressure (B=–0.09, P=0.105).
Figure 1 shows a dose–response decrease in systolic blood pressure, when change in mean blood pressure from baseline to follow-up was calculated per 10th percentile of change in symptom load of anxiety/depression from baseline to follow-up. Individuals with the greatest increase (91–100th percentile change) in symptoms of anxiety and depression had a significantly lower increase in systolic blood pressure (8.1 v. 10.4 mmHg, P<0.001), compared with individuals with the greatest decrease (0–10th percentile change) in anxiety and depression. However, this inverse association was not found for diastolic blood pressure.
Effect of individual anxiety/depression items at baseline
In separate analyses we found that most individual anxiety and depression items at baseline were associated with a decrease in mean blood pressure during follow-up (results not shown), which is in line with the main result of this paper.
Supplementary cross-sectional findings
The cross-sectional inverse association of systolic blood pressure with anxiety and depression symptom scores above the 90th percentile was equivalent at baseline and follow-up (Fig. 2), despite use of different measures for blood pressure, and anxiety and depression. Similarly, the association of diastolic blood pressure with symptoms of anxiety and depression was almost identical for the two surveys (results not shown).
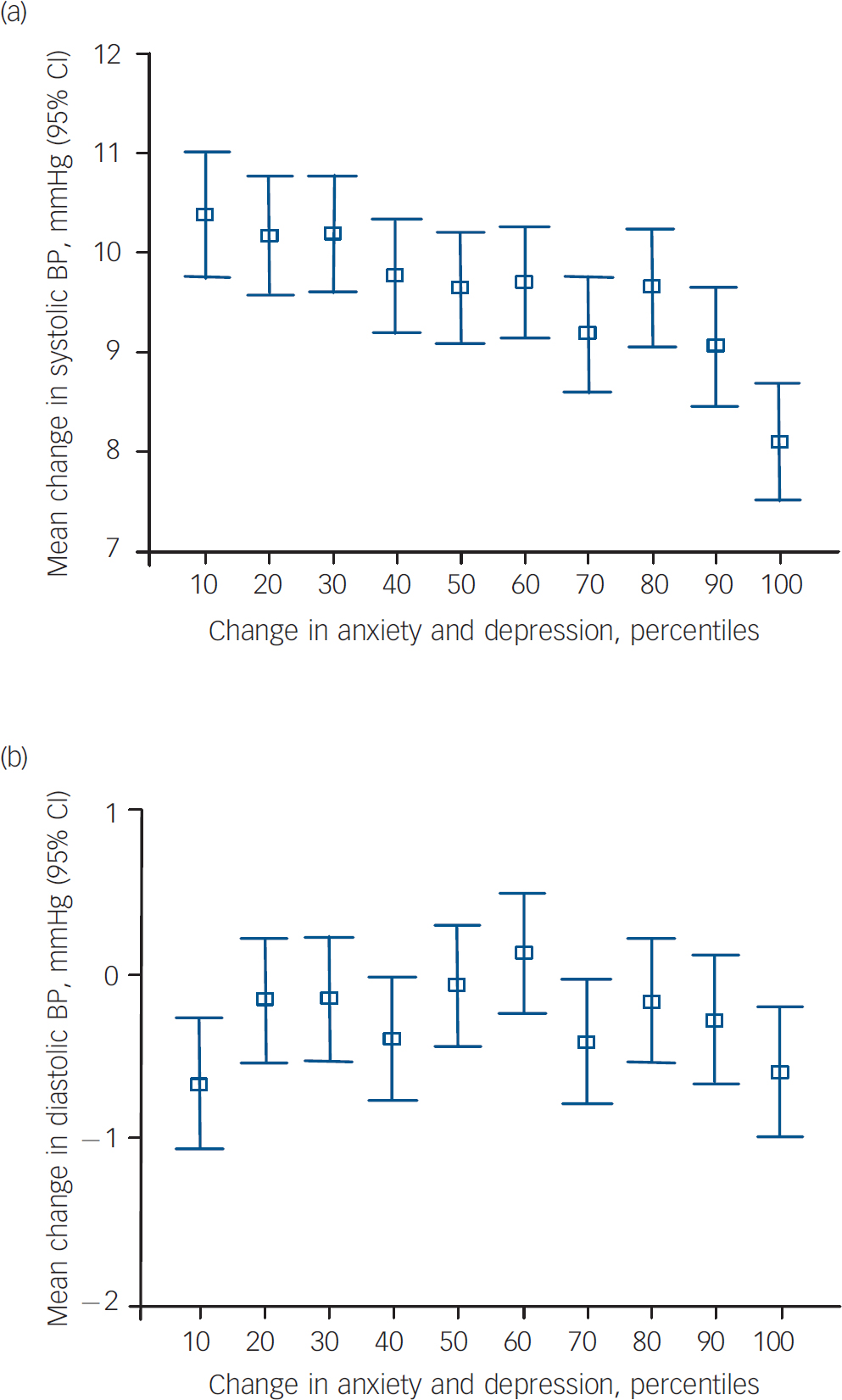
Fig. 1 Effect of change in symptom load of anxiety and depression (follow-up minus baseline level) on blood pressure (follow-up minus baseline blood pressure) over 11 years.
(a) Systolic and (b) diastolic blood pressure (BP). Change above the 50th percentile indicates a relative increase, whereas change beneath the 50th percentile indicates a relative decrease in symptom load from baseline to follow-up.
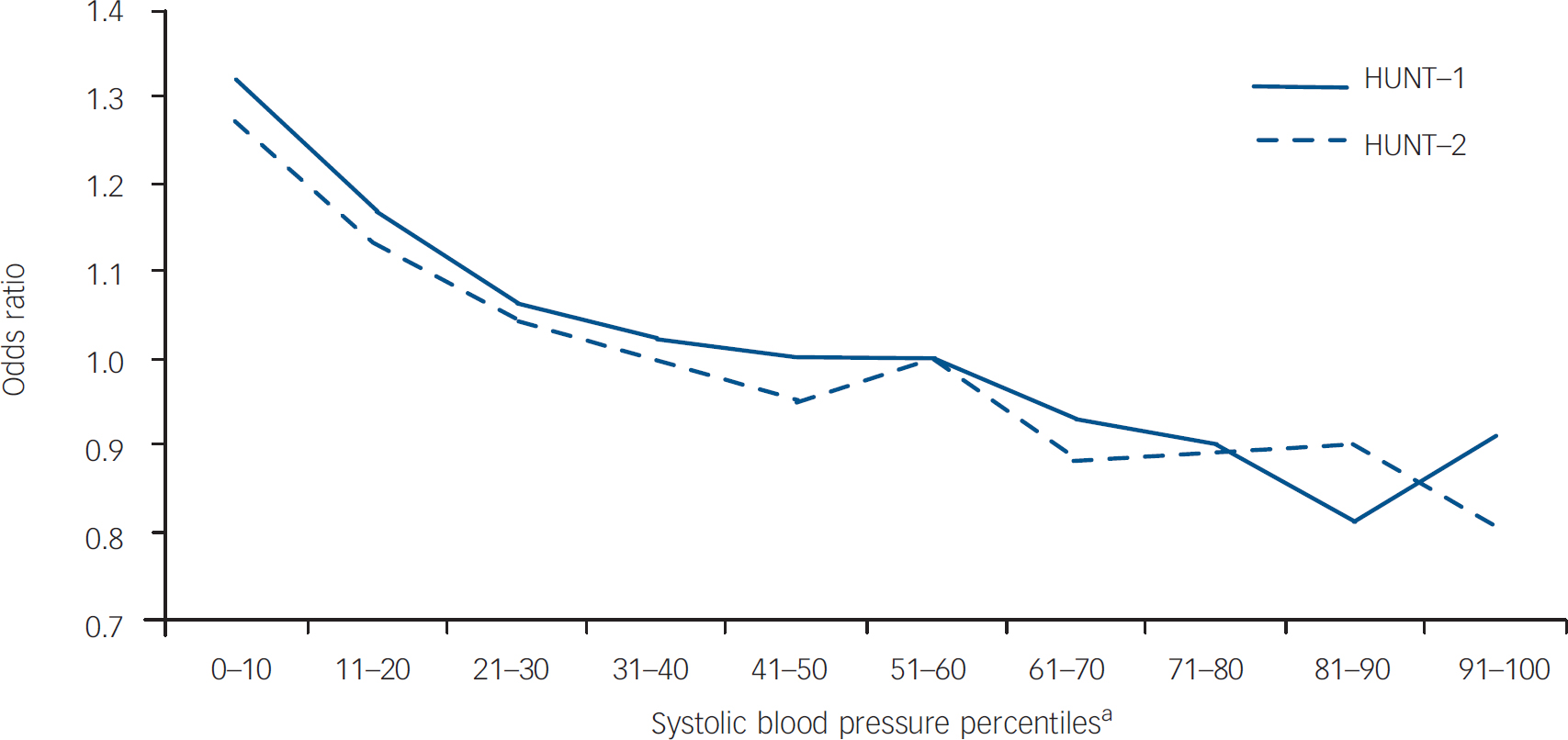
Fig. 2 Cross-sectional associations between systolic blood pressure and anxiety and depression in HUNT–1 and HUNT–2.
Odds ratio from logistic regression analyses, outcomes being scores above the 90th percentile of the Anxiety and Depression Symptom Index–12 in HUNT–1 (n=60 143) and the Hospital Anxiety and Depression Scale in HUNT–2 (n=60 799), adjusted for age, gender and educational level. The 51–60th percentile systolic blood pressure was reference group. a. Stratified for age and gender.
Discussion
We found that symptoms of anxiety and depression were associated with decrease in blood pressure. Both the increase in symptom load from baseline to follow-up and a high baseline symptom load predicted a decrease in blood pressure. These associations were found in both genders, were independent of baseline blood pressure, age and other risk factors usually associated with hypertension, and were not explained by the use of antidepressant or antihypertensive medication.
Other studies
Our findings are in contrast to earlier reports that suggested a link between anxiety and an increase in mean systolic but not diastolic blood pressure, Reference Markovitz, Matthews, Wing, Kuller and Meilahn5 and that neither anxiety Reference Sparrow, Garvey, Rosner and Thomas4,Reference Räikkönen, Matthews and Kuller6,Reference Shinn, Poston, Kimball, St Jeor and Foreyt7 nor depression Reference Goldberg, Comstock and Graves3,Reference Shinn, Poston, Kimball, St Jeor and Foreyt7 had any effect on mean systolic and diastolic blood pressure. However, these studies had smaller sample sizes and were prone to selection biases; the only positive association (between anxiety at baseline and increase in systolic but not diastolic blood pressure) was found in a sample of 468 middle-aged women. Reference Markovitz, Matthews, Wing, Kuller and Meilahn5 Moreover, the results of ten studies employing blood pressure above a cut-off level or use of antihypertensive medication as outcomes are conflicting: four found that anxiety predicted hypertension Reference Jonas, Franks and Ingram15–Reference Somova, Connolly and Diara18 and three that depression predicted hypertension, Reference Jonas, Franks and Ingram15,Reference Jonas and Lando16,Reference Davidson, Jonas, Dixon and Markovitz19 whereas four found no effect of anxiety Reference Sparrow, Garvey, Rosner and Thomas4,Reference Räikkönen, Matthews and Kuller6,Reference Shinn, Poston, Kimball, St Jeor and Foreyt7,Reference Yan, Liu, Matthews, Daviglus, Ferguson and Kiefe20 and four found no effect of depression. Reference Räikkönen, Matthews and Kuller6,Reference Shinn, Poston, Kimball, St Jeor and Foreyt7,Reference Yan, Liu, Matthews, Daviglus, Ferguson and Kiefe20,Reference Levenstein, Smith and Kaplan21 Some of the positive associations have been found only in subsamples according to gender Reference Jonas and Lando16 or ethnicity. Reference Somova, Connolly and Diara18,Reference Davidson, Jonas, Dixon and Markovitz19 A 2-year follow-up study in elderly people found that low blood pressure was a risk factor for, but not a consequence of, depression. Reference Paterniti, Verdier-Taillefer, Geneste, Bisserbe and Alpérovitch22
In contrast, three cross-sectional studies among the elderly found an association between high anxiety and depression and low blood pressure, Reference Barrett-Connor and Palinkas23–Reference Jorm25 consistent with our previous report Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 and with another large population-based study of young adults. Reference Herva, Räsänen, Miettunen, Timonen, Läksy, Veijola, Laitinen, Ruokonen and Joukamaa26
Strengths and limitations
Previously, only two studies of middle-aged women with small sample sizes Reference Markovitz, Matthews, Wing, Kuller and Meilahn5,Reference Räikkönen, Matthews and Kuller6 have examined the effect of increasing anxiety or depression on change in blood pressure, based on measurements both at baseline and follow-up. In contrast, most longitudinal studies have only assessed the association of anxiety or depression at baseline and blood pressure measured from months to many years later. Our study analysing change in anxiety and depression in relation to change in blood pressure over a decade in a large population is methodologically more advanced than most other studies.
Another strength is that our study covered a large unselected adult population within a geographical area with a high participation rate. Reference Holmen, Midthjell, Bjartveit, Hjort, Lund-Larsen, Moum, Næss and Waaler9,Reference Holmen, Midthjell, Krüger, Langhammer, Holmen, Bratberg, Vatten and Lund-Larsen10 As blood pressure varies greatly with gender and age, the use of mean blood pressure and age- and gender-stratified percentiles is better for assessing change than traditional cut-off values. Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 Furthermore, we had a long follow-up period and data on relevant covariates.
This study has some limitations. First, anxiety and depression were measured with different instruments at baseline and follow-up. Although the HADS at follow-up is a well-established screening instrument in epidemiology, Reference Bjelland, Dahl, Haug and Neckelmann14 the ADI–12 Index used at baseline is less established. However, several items of the two scales overlapped with high correlations between them and with comparable associations with age (data not shown). In addition, the ADI–12 Index has previously reported strong correlations with the Hopkins Symptoms Checklist–25. Reference Tambs and Moum11 Of great interest is that the cross-sectional associations between blood pressure and anxiety and depression were almost identical at baseline and at follow-up (Fig. 2), indicating no major problems applying different psychometrics.
Second, different methods of measuring blood pressure were used at baseline and follow-up. However, as these two methods were found to give similar results, Reference Lund-Larsen27 it is unlikely that this could influence the associations we have observed.
Third, because most of the participants were White, the extent to which the results can be generalised to other ethnic groups is uncertain.
Possible mechanisms and future studies
Our data do not elucidate the mechanism behind the findings. The cross-sectional Reference Hildrum, Mykletun, Stordal, Bjelland, Dahl and Holmen8 and longitudinal analyses included many covariates, but they explained very little of the association. Similarly, the individual-item analyses did not reveal any pattern suggesting mechanisms for the association. There is, however, considerable evidence suggesting that symptoms of anxiety and depression are associated with alterations in the hypothalamic–pituitary–adrenal system, Reference Ströhle and Holsboer28 and some indications of abnormal autonomic nervous function in depression. Reference Scalco, Scalco, Azul and Lotufo Neto29 In the past two decades, numerous studies have suggested that neuropeptide Y, one of the most abundantly expressed neuropeptides, has important functions in these systems and exhibits effects in various domains such as food intake, blood pressure and mental symptoms. A recent review has shown that patients with depression have altered levels of neuropeptide Y and that cerebrospinal fluid levels of neuropeptide Y have been found to be inversely associated with anxiety scores in these patients. Reference Karl and Herzog30 Another review highlights its anxiolytic and antidepressant-like effects. Reference Carvajal, Dumont and Quirion31 Regarding the cardiovascular system, neuropeptide Y in the brain seems to suppress sympathetic activity and decrease blood pressure, Reference Matsumura, Tsuchihashi, Fujii and Iida32 whereas in the peripheral nervous system it induces vasoconstriction, Reference Pons, Lee, Li and Kitlinska33 which may be of a transient nature. Reference Kellogg34 Although the effects of neuropeptide Y and related peptides on vascular regulation are only partly understood, Reference Matsumura, Tsuchihashi, Fujii and Iida32 it seems reasonable that they are involved both in the well-known acute stress-induced increase in blood pressure and in the long-term inverse association between anxiety and depression and blood pressure that we found. More work is needed to explore the differences between the relationship of ongoing v. acute psychological distress on blood pressure and the underlying biological pathways.
Acknowledgements
The HUNT study is a collaboration between the HUNT research centre at the Faculty of Medicine, Norwegian University of Science and Technology, the Norwegian Institute of Public Health, and the Nord-Trøndelag County Council. B.H. has received grants from Mid-Norway Regional Health Trust, Jonn Nilsen's Legacy, and H. Lundbeck, Norway.








eLetters
No eLetters have been published for this article.