Preventing suicide is a global health priority; it is a significant cause of death in developed and developing countries among key population groups, including young people, men in middle age, and people in later life.1 Self-harm and self-injury have also been identified as increasing in many countries over recent years.Reference Brunner, Kaess, Parzer, Fischer, Carli and Hoven2 There are more than 100 000 presentations per year at hospitals in England, UK, although this underestimates the numbers because most episodes of self-harm do not reach clinical services and remain in the community.3, Reference Borges, Nock, Abad, Hwang, Sampson and Alonso4 There is a strongly evidenced connection between an episode of self-harm or self-injury, repetition and suicide completion; an episode of self-harm increases the chance of suicide completion up to 100-fold,Reference Kendall, Taylor, Bhatti, Chan and Kapur5, Reference Hawton, Bergen, Cooper, Turnbull, Waters and Ness6 thus it is a strong predictor of future suicide attempts.Reference Cox, Stanley, Melhem, Orquendo, Birmaher and Burke7, Reference Wilkinson, Kelvin, Roberts, Dubicka and Goodyer8 The North American literature distinguishes between suicide attempts and non-suicidal self-injury (NSSI) on the basis of intention to die,Reference Crosby, Ortega and Stevens9 whereas in the UK and Europe, the term ‘self-harm’ is used to include any non-fatal act of harm against the self, irrespective of motivation or method, and so the term ‘suicide attempt’ is subsumed within the term ‘self-harm’ in this literature.3, Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Townsend10, Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Hazell11 In this review we use the UK terminology self-harm, as defined above to include suicide attempts, as well as reporting the terminology used by trial authors, including NSSI and the older term, ‘parasuicide’.
Psychological therapies are increasingly important for providing interventions for people at risk of suicide or repeated self-harm, but good-quality evidence for the effectiveness of interventions remains low, especially from randomised controlled trials (RCTs), despite recently increased numbers of trials in this area.3, Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Townsend10, Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Hazell11 It is important to know how specific interventions reduce risks and episodes, and which are effective with which groups of people. This review seeks to evaluate the effectiveness of one intervention, psychoanalytic (or psychodynamic) psychotherapy. Psychoanalytic psychotherapy has a misleading reputation for not being ‘evidence-based’, a reflection of a historic view that it is not amenable to scientific evaluation. A number of recent systematic reviews and meta-analyses attest to the existence of trials evaluating its effectiveness with regard to a range of conditions, including depression, anxiety, somatoform disorders and borderline personality disorder, and for different approaches, including longer- and short-term therapy, for adults and children and adolescents.Reference Ougrin, Tranah, Stahl, Moran and Asarnow12–Reference Leichsenring and Klein18 Conclusions from these reviews are that effect sizes are largely similar to those of other therapies, such as cognitive–behavioural therapy, whereas an emerging feature of psychoanalytic psychotherapy trials is that benefits are sustained and can demonstrate superiority at longer-term follow-up.Reference De Maat, de Jonghe, de Kraker, Leichsenring, Abbass and Luyten19, Reference Fonagy, Rost, Carlyle, McPherson, Thomas and Fearon20 This is the first systematic review and meta-analysis of RCTs evaluating this form of intervention for suicidal behaviour, self-harm and self-injury. This review seeks to assess whether psychoanalytic psychotherapy is effective in preventing suicide through reducing self-harm (including suicide attempts), reducing symptoms and characteristics linked with known risk factors for suicide/self-harm, and to assess possible adverse effects associated with these interventions. To be consistent with recommendations from prior reviews,Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Hazell11 we examine effects for suicide attempts, NSSI and self-harm separately, and we explore potential mediators of treatment effects, including type and duration of treatment.
Method
The review protocol is registered with The International Prospective Register of Systematic Reviews (PROSPERO) under identifier CRD42018108483. Studies were identified through searches in six bibliographical databases (from January 1970 to March 2017): PubMed, PsycINFO, Psycharticles, CINAHL, EMBASE and the Cochrane Central Register of Controlled Trials. Search terms used were: ‘psychoanalytic psychotherapy’, ‘mentalisation based therapy’, ‘transference-focused psychotherapy’, ‘cognitive analytic therapy’, ‘psychodynamic psychotherapy’ with suicid*, ‘self-harm’, ‘self-mutilation’ and ‘self-injury’. The reference lists of all relevant papers known to the investigators were checked, as were the reference lists of major reviews that were known to the investigators or found by the electronic searches (Fig. 1).Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Townsend10, Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Hazell11, Reference Ougrin, Tranah, Stahl, Moran and Asarnow12, Reference Abbass, Kisely, Town, Leichsenring, Driessen and De Maat13, Reference Fonagy16, Reference Leichsenring and Rabung17, Reference Knekt, Lindfors, Laaksonen, Renlund, Haaramo and Härkänen21–Reference Leichsenring, Abbass, Luyten, Hilsenroth and Rabung26
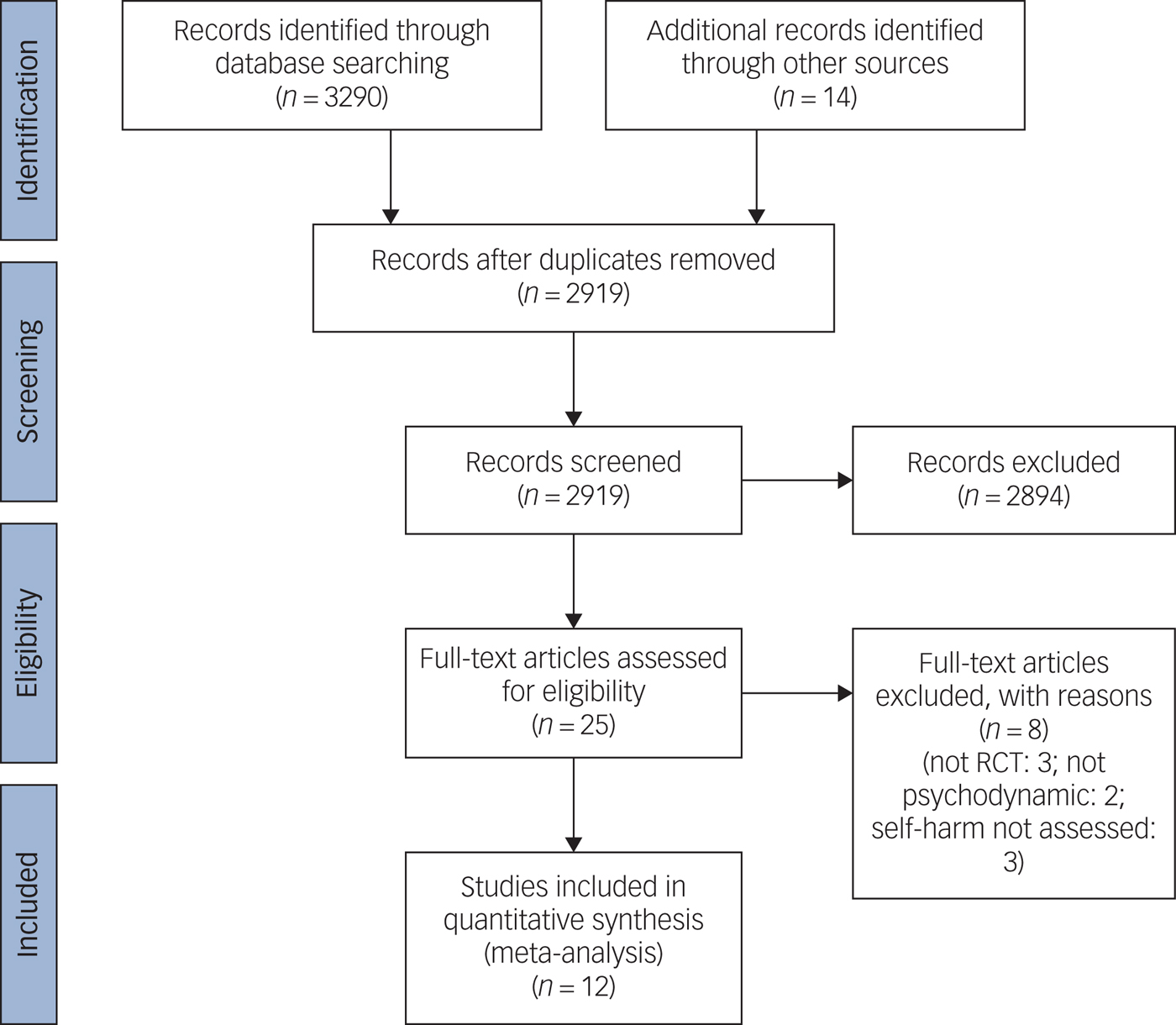
Fig. 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2009 flow diagram.
Studies included had to be RCTs (including cluster-randomised and crossover trials) comparing psychoanalytic psychotherapy of suicidal behaviour, self-harm or self-injury with treatment as usual (TAU), routine psychiatric care, enhanced usual care, placebo or any other comparison, including with a different psychological therapy. Samples included children, adolescents and adults in any setting. The primary outcome measure in this review was the occurrence of repeated self-harm, which, according to the National Institute for Health and Care Excellence definition, means we will assess both suicide attempts and self-injuries,3 including follow-up at intervals up to 18 months post-treatment. Secondary outcomes were depression, anxiety, psychosocial functioning and hospital admissions. Where a trial measured the same outcome (for example, depression) in two or more ways, we used the most common measure across trials in any meta-analysis, but we also report scores from the other measures in the text of the review.
We defined the intervention as therapy that was psychoanalytic or psychodynamic in nature, of any duration, aimed at reducing or preventing repetition of suicide attempts, self-harm and self-injury, and reducing suicidal intent, ideation and thoughts.
Data from included trials were extracted by two authors (A.G. and S.B.) independently of each other, using a standardised extraction form (adapted from the Cochrane Data Extraction and Assessment Template 2011, available at https://training.cochrane.org/sites/training.cochrane.org/files/public/uploads/resources/downloadable_resources/English/Collecting%20data%20-%20form%20for%20RCTs%20only.doc). Where the same study had more than one article written about the outcomes, we treated all articles as one study and presented the results only once. We used data from all identified and selected trials to draw funnel plots (size of study versus effect size),Reference Midgley and Kennedy27 to attempt to detect the possibility of publication bias.
Statistical analysis
Standardised mean differences (SMDs) were used for continuous data and odds ratios for binary data, with accompanying 95% confidence intervals, using the random effects DerSimonian and Laird method. For subgroup comparisons, we used fixed-effects models. Before groups were compared, we first synthesised the results within the groups before comparing at the group level. All analyses were conducted with Stata version 14.2. Heterogeneity between studies was measured with the I 2 statistic. We used the following values to denote relative importance of heterogeneity: 0–40% (unimportant), 30–60% (moderate), 50–90% (substantial) and 75–100% (considerable), as is the guidance in the Cochrane Handbook.Reference Egger, Davey Smith, Schneider and Minder28 Where the value fell into one of the overlapping regions (e.g. between 30% and 40%), we used the confidence interval for I 2 or P-value from the χ 2 test to determine the category of importance. We used the Grading of Recommendations and Evaluation (GRADE) approach to summarise the quality of evidence.
Results
We identified 3290 citations by using the search strategy described above. Additionally, 14 papers were identified by searching references. After removing duplicates, the overall number of citations remaining was 2919. Of these, 2894 were excluded after screening and a further 9 were excluded after reading full texts. The 17 papers included reported from 12 studies. All studies included were described as RCTs. All but one study used a simple randomisation procedure, based on individual allocation to the intervention and control groups. One trialReference Higgins, Green, Higgins and Deeks29 randomised clinicians in blocks rather than participants. The main characteristics of the studies are summarised in online Supplementary Table 1 available at https://doi.org/10.1192/bjp.2019.33 (included studies), and Supplementary Table 2 (excluded studies). Eight excluded studies are listed in Supplementary Table 2. Three were excluded because the research design was not RCT,Reference Ougrin, Zundel, Ng, Banarsee, Bottle and Taylor30–Reference Korner, Gerull, Meares and Stevenson32 two were excluded because the intervention was judged not to be psychodynamicReference Kvarstein, Pedersen, Urnes, Hummelen, Wilberg and Karterud33, Reference Farrell, Shaw and Webber34 and three were excluded because outcomes for self-harm were not assessed.Reference Diamond, Wintersteen, Brown, Diamond, Gallop and Shelef35–Reference Jørgensen, Freund, Baye, Jordet, Andersen and Kjølbye37
Description of studies
Twelve studies were included.Reference Higgins, Green, Higgins and Deeks29, Reference Monroe-Blum and Marziali38–Reference Reneses, Galián, Serrano, Figuera, Del Moral and López-Ibor53 Characteristics of the trials are shown in Supplementary Table 1. The total number of randomised participants was 999. Some studies excluded some participants who dropped out in their data analysis,Reference Bateman and Fonagy44, Reference Chanen, Jackson, McCutcheon, Jovev, Dudgeon and Yuen45, Reference Doering, Horz, Rentrop, Fischer-Kern, Schuster and Benecke47, Reference Gregory, Remen, Soderberg and Ploutz-Snyder49, Reference Guthrie, Kapur, Mackway-Jones, Chew-Graham, Moorey and Mendel51, Reference Ougrin, Boege, Stahl, Banarsee and Taylor52 and thus the total number of participants analysed was 939. Samples ranged from 30 (24 after excluding those who dropped out in the analysis) to 134, with means of 76.8 randomised and 72.2 analysed.
Studies were conducted in out-patient and community settings (nine studies), a combination of accident and emergency and out-patient,Reference Higgins, Green, Higgins and Deeks29 accident and emergency and patients’ homes,Reference Gregory, DeLucia-Deranja and Mogle50 and an in-patient setting.Reference Amianto, Ferrero, Pierò, Cairo, Rocca and Simonelli39 Studies were conducted in several countries: the UK,Reference Higgins, Green, Higgins and Deeks29, Reference Amianto, Ferrero, Pierò, Cairo, Rocca and Simonelli39, Reference Bateman and Fonagy43, Reference Rossouw and Fonagy54, Reference Gregory, DeLucia-Deranja and Mogle50, Reference Reneses, Galián, Serrano, Figuera, Del Moral and López-Ibor53 USA,Reference Chanen, Jackson, McCutcheon, Jovev, Dudgeon and Yuen45, Reference Gregory, Remen, Soderberg and Ploutz-Snyder49 EuropeReference Monroe-Blum and Marziali38, Reference Clarkin, Levy, Lenzenweger and Kernberg46, Reference Doering, Horz, Rentrop, Fischer-Kern, Schuster and Benecke47, Reference Ougrin, Boege, Stahl, Banarsee and Taylor52 and Australia.Reference Bateman and Fonagy44 Nine studies were on adult samples and threeReference Higgins, Green, Higgins and Deeks29, Reference Bateman and Fonagy44, Reference Reneses, Galián, Serrano, Figuera, Del Moral and López-Ibor53 were on adolescents aged <18 years. All studies except oneReference Monroe-Blum and Marziali38 had a majority of female participants, and one studyReference Clarkin, Levy, Lenzenweger and Kernberg46 recruited only females. Overall, female participants outnumbered males by a ratio of 4:1, which happens to reflect self-harm gender disparities found in the prevalent literature.
A range of controls was used in these studies; no waiting list or crossover designs were used. TAU of various kinds was used in six trialsReference Higgins, Green, Higgins and Deeks29, Reference Amianto, Ferrero, Pierò, Cairo, Rocca and Simonelli39, Reference Clarkin, Levy, Lenzenweger and Kernberg46, Reference Gregory, DeLucia-Deranja and Mogle50, Reference Ougrin, Boege, Stahl, Banarsee and Taylor52, Reference Reneses, Galián, Serrano, Figuera, Del Moral and López-Ibor53 and enhanced usual care was used in four studies.Reference Monroe-Blum and Marziali38, Reference Bateman and Fonagy43, Reference Bateman and Fonagy44, Reference Gregory, Remen, Soderberg and Ploutz-Snyder49 Two trials compared psychoanalytic psychotherapy with another psychological therapy: schema-focused therapy,Reference Doering, Horz, Rentrop, Fischer-Kern, Schuster and Benecke47 and dialectical behaviour therapy and supportive therapy.Reference Chanen, Jackson, McCutcheon, Jovev, Dudgeon and Yuen45
In all included studies, the intervention used core psychoanalytic methods to increase awareness and self-reflection; to manage, regulate or contain emotions; and to effect change through the therapeutic relationship. However, there were differences of approach, intensity and duration of the intervention and differences between types of study population (age, number of previous episodes of self-harm). We identified subgroups for the purposes of making comparisons for population (adult or adolescent), acute or chronic self-harm, duration of therapy (short term <40 sessions or longer term >40 sessions) and comparators (TAU, enhanced TAU or another intervention). Additionally, we assessed the experience of therapists and their training in and adherence to the intervention.
Primary outcomes
Suicide attempts
There was an overall significant treatment effect for psychoanalytic psychotherapy compared with TAU on the number of patients who attempted suicide in three studies at 12-month follow-up (three studies: n = 276, pooled odds ratio 0.469; 95% CI 0.274–0.804; I 2 = 0.0) (Fig. 2). There was no significant treatment effect for psychoanalytic psychotherapy on the number of suicide attempts (episodes) at 12-month follow-up (two studies: n = 238; SMD = −0.235; 95% CI −0.502 to 0.033; I 2 = 8.6) (Fig. 3).
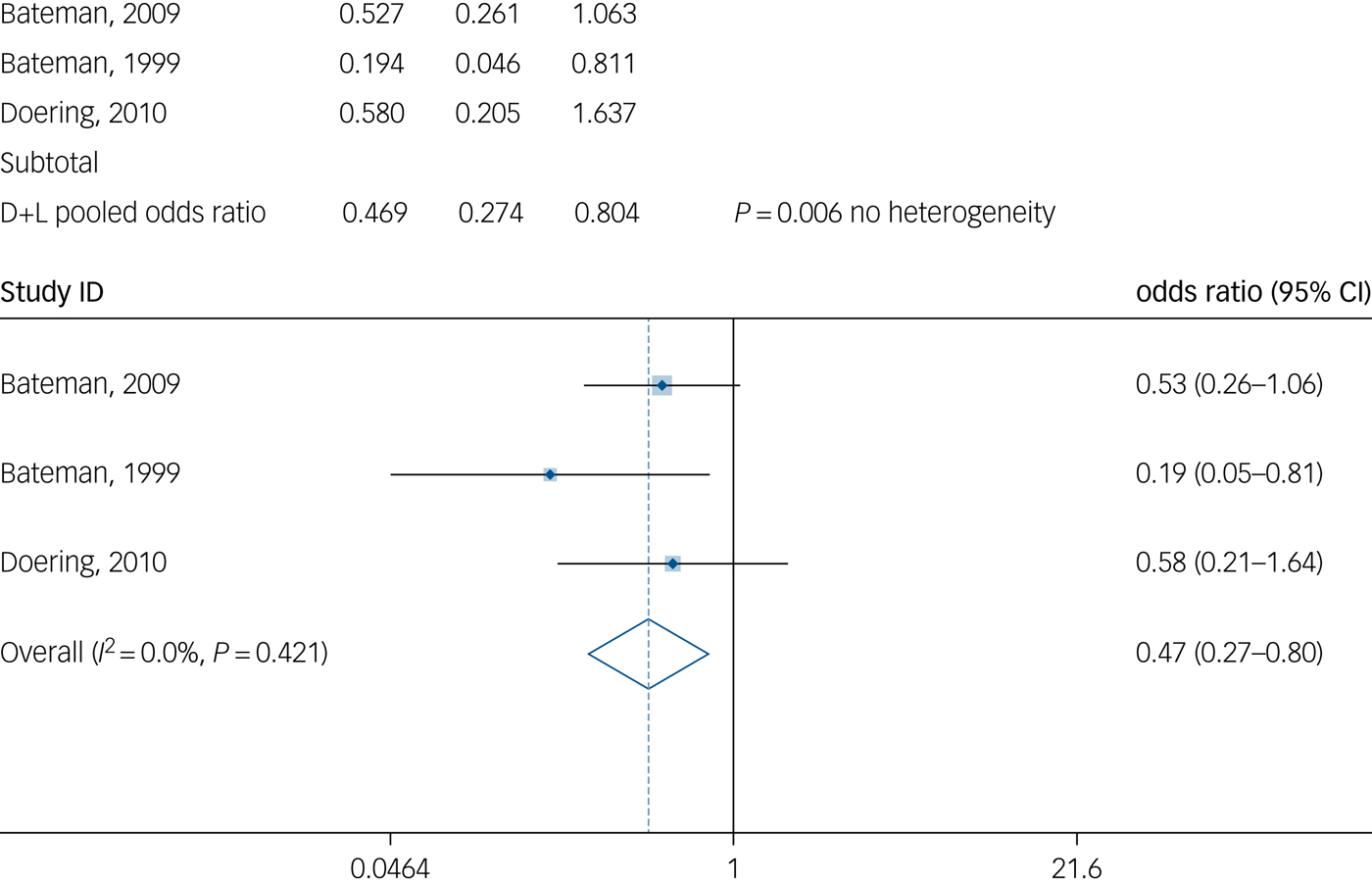
Fig. 2 Number of patients who attempted suicide at 12-month follow-up.

Fig. 3 Number of suicide attempts (counts) at 12-month follow-up.
Self-harm
There was evidence of a significant treatment effect for psychoanalytic psychotherapy on the number of patients who repeated self-harm (i.e. self-harm and suicide attempts combined) by the 6-month follow-up (two studies: n = 125; odds ratio 0.27; 95% CI 0.109–0.668; P = 0.005; I 2 = 82.7%) (Fig. 4). High heterogeneity should be noted. However, at 12-month follow-up there was no evidence of a significant treatment effect for psychoanalytic psychotherapy on the number of patients who repeated self-harm (three studies: n = 278; odds ratio 0.581; 95% CI 0.236–1.426; I 2 = 63.6%). Similarly, there was no evidence of significant treatment effect for psychoanalytic psychotherapy on self-harm episodes in this period (rather than the number of patients who repeated self-harm) at 12-month follow-up on the basis on data from three studies (three studies: n = 273; SMD = −0.149; 95% CI 0.388–0.089; I 2 = 0.0%) (Fig. 5).

Fig. 4 Number of patients attempting suicide and self-harming at 6-month follow-up.
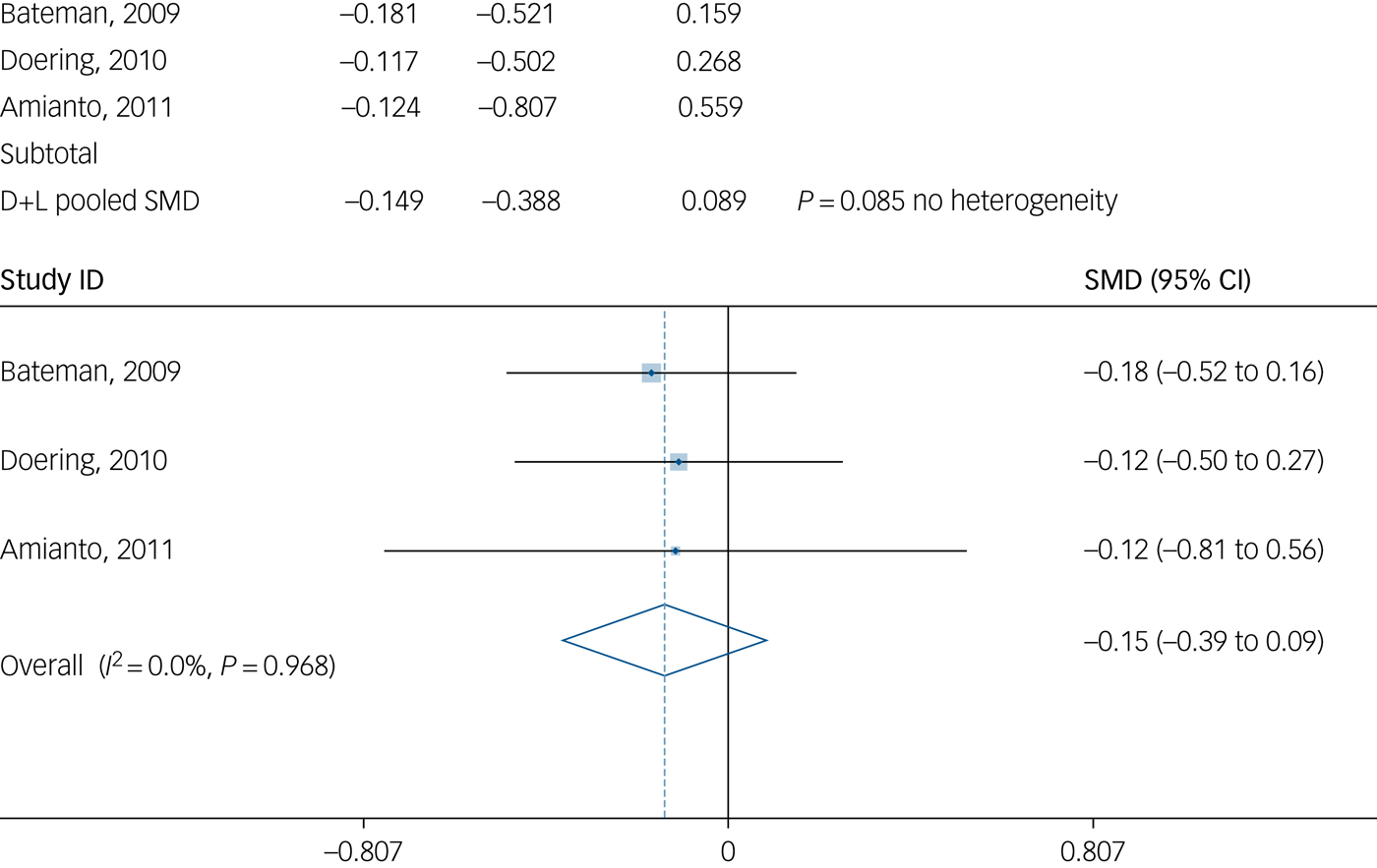
Fig. 5 Number of self-harm incidents at 12-month follow-up.
Secondary outcomes
Depression
Data on depression scores obtained using the Beck Depression Inventory at 6-month follow-up did not suggest a significant treatment effect for psychoanalytic psychotherapy (two studies: n = 172; SMD = −0.273; 95% CI −0.615 to 0.069; I 2 = 0.0%). There was no overall evidence to suggest a significant treatment effect for psychoanalytic psychotherapy at 12-month follow-up (three studies: n = 172; SMD = −0.357; 95% CI −1.048 to 0.335; I 2 = 85.2%).
Anxiety
There was no overall evidence of a significant treatment for psychoanalytic psychotherapy at 12-month follow-up in anxiety state (temporary state of anxiety) assessed by the Spielberger State-Trait Anxiety Inventory (two studies: n = 142; SMD = −0.350; 95% CI −1.458 to 0.757; I 2 = 87.8%). It ought to be noted that significant heterogeneity was found. As for anxiety trait (long-term anxiety), there was no evidence to suggest a treatment effect for psychoanalytic psychotherapy at 12-month follow-up (two studies: n = 142; SMD = 0.018; 95% CI −0.311 to 0.347; efficacy at 12 months, I 2 = 0.0%).
Psychosocial functioning
Psychosocial functioning was assessed by the Social Adjustment Scale. There was evidence of an overall moderate treatment effect for psychoanalytic psychotherapy at the 18-month follow-up assessment (three studies: n = 207; SMD = −0.620; 95% CI −1.210 to −0.030; I 2 = 23.6%). However, psychoanalytic psychotherapy was not found to have a significant effect on psychosocial functioning when that was assessed by the Global Assessment of Functioning Scale (GAS) in two trials at 12-month follow-up (two studies: n = 139; SMD = 0.269; 95% CI 0.068–0.606; I 2 = 0.0%). Overall, psychoanalytic psychotherapy did not show an effect on improved psychosocial functioning as assessed by GAS at 18-month follow-up (two studies: n = 169; SMD = 0.401; 95% CI −0.034 to 0.837; I 2 = 34.5%).
Admissions
There was evidence of a significant treatment effect for psychoanalytic psychotherapy on the reduction of number of admissions at the 12-month follow-up assessment (two studies: n = 238; SMD = −0.505; 95% CI −0.763 to −0.246; I 2 = 0.0%). However, there was no evidence of a treatment effect for psychoanalytic psychotherapy in reducing the number of admissions at 6-month follow-up in two trials (two studies: n = 253; SMD = −0.291; 95% CI −0.592 to 0.011; I 2 = 23.6%). Pooled analysis of three trials at 12-month follow-up assessment suggested no overall evidence of a significant treatment effect for psychoanalytic psychotherapy in reducing the length of admissions in days (three studies: n = 273; SMD = −0.268; 95% CI −0.563 to 0.028; I 2 = 27.9%).
Differences between subgroups
We found no evidence of significant differences between studies of different populations (adult or adolescent), self-harm histories (acute or chronic) or for long- and short-term interventions (treatment for >1 year or <1 year). In all comparisons, heterogeneity was low (I 2 < 30%). For comparisons of studies with different comparators (TAU and enhanced TAU), heterogeneity was also low (I 2 < 30%).
Quality of the studies
Bias was detected in the domain of performance and detection bias, with five trials being at high risk for blinding of participants, although this can be problematic in trials of this nature. Overall we judged the majority of the 12 studies to be at low risk of bias. There was inadequate information to make a satisfactory risk of bias judgement for the majority of trials (9 out of 12) for selected reporting bias (for detailed ratings see Supplementary Table 3). Using funnel plots, we checked for publication bias in three groups of outcomes: those reported as means, those reporting counts and those with binary outcomes. In all cases the plots revealed significant asymmetry, suggesting publication bias. This was confirmed by the Egger test (studies reporting means: bias, −4.86; t = −3.04; P = 0.008; studies reporting counts: bias, 2.74; t = 2.83; P = 0.016; and studies reporting binary outcomes: bias, −1.78; t = −2.10; P = 0.048) (Fig. 6). Applying the GRADE system, we classified the quality of evidence overall as moderate.
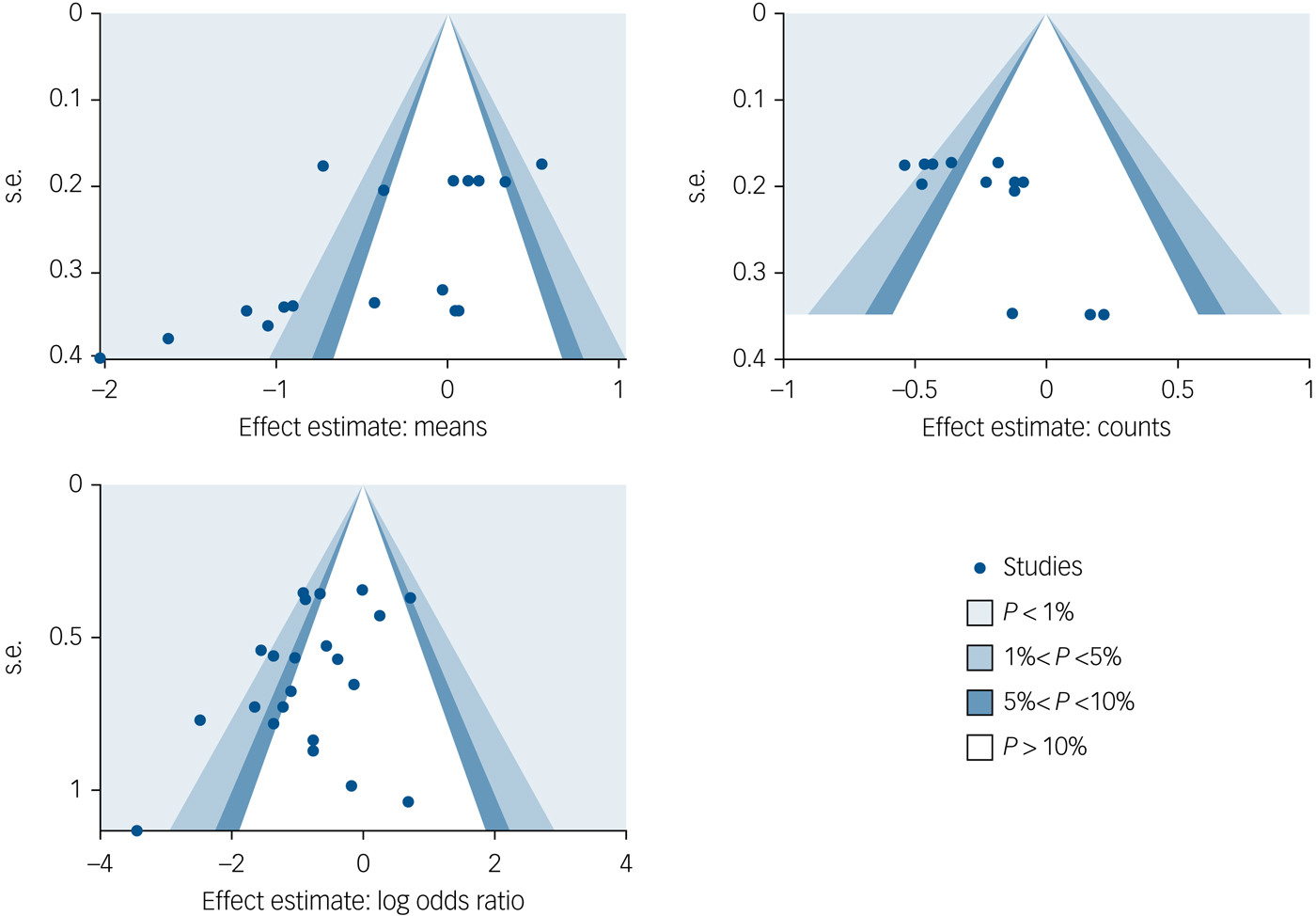
Fig. 6 Publication bias: funnel plots.
All studies used a manual/protocol. Delivering therapists ranged from expert (two studies) to moderate training and experience (eight studies), to low experience and qualifications (two studies). In six studies, training to use the intervention was high, three studies were moderate and three studies low; supervision and fidelity measures were high in seven studies, moderate in four studies and low in one study.
Discussion
This systematic review seeks to provide an estimation of the effectiveness of psychoanalytic psychotherapies compared with TAU and with other interventions for reducing suicide attempts and self-harm. This included the evaluation of whether such interventions had a positive effect on proximal risk factors for suicide attempts and self-harm (such as depression and anxiety), for reduction of psychosocial problems and for reduction of length of hospital admissions associated with suicide and self-harm. We also evaluated the quality of the evidence base and the presence of publication bias.
The finding in relation to the primary outcomes was that there was some evidence for a significant treatment effect for the number of patients attempting suicide (pooled odds ratio, 0.468 with 276 participants) at 12-month follow-up. There was also some evidence for a small significant effect for the reduction of self-harm (defined here to include suicide attempts and self-injuries) at 6-month follow-up (odds ratio, 0.27 with 149 participants), and it is noted there is high heterogeneity for this result. There was no evidence for a significant treatment effect for self-harm or suicidal episodes, nor the number of patients repeating self-harm at 12-month follow-up. Although other studies of psychoanalytic psychotherapy show that differences are sustained at longer-term follow-up, we were not able to pool findings from studies for the effects at longer term, i.e. ≥18 months. The clinical implication is that psychoanalytic psychotherapy has benefit over comparators for self-harm 6 months after treatment ends, but not at 12 months; for suicide attempts the evidence is in favour of the intervention at 12 months.
We did not find overall a significant treatment effect for improvement of depression or anxiety symptoms in studies of psychoanalytic psychotherapy at 6-month and 12-month follow-up. The findings were similar in relation to both anxiety state (temporary anxiety) and anxiety trait (long-term anxiety), with no overall significant treatment effect for psychodynamic therapies at either 12 months or 18 months.
We looked for improvements in psychosocial functioning in patients who received psychoanalytic psychotherapy. Studies used different outcome measures, so data could only be pooled where the same measurement instrument had been used. Studies that used the Social Adjustment Scale found evidence of an overall moderate treatment effect at 18-month follow-up, based on three studies with an SMD of −0.620 and 207 participants. However, the studies that used GAS as the measurement tool for psychosocial functioning found no overall significant treatment effect.
Finally, we considered whether psychoanalytic psychotherapy reduced the number of hospital admissions or the length of admissions. There was no effect in reducing the number of admissions at 6 months, although there was a significant effect at 12-month follow-up (two studies: SMD = −0.505 with 238 participants). There was no overall evidence of reduction in the number of days spent in hospital at 12-month follow-up.
We explored how differences of population, histories of self-harm, types of comparator and types of psychodynamic therapy affected the results. We found no significant heterogeneity between studies for different populations, in terms of age (adult versus adolescent), self-harm history (acute versus chronic) and duration of therapy (>1 year or <1 year) Despite different nomenclatures, all the interventions applied psychoanalytic principles to improve awareness, emotion regulation and relationships, and to effect change through the therapeutic relationship.
Quality of the evidence
Risk of bias was unclear for several domains in most of the studies, particularly in relation to reporting bias (selective reporting), where 9 of the included 12 studies were rated as ‘unclear’. Risk of bias was considered low for the significant majority of studies in relation to selection bias, performance and detection bias (with the exception of blinding of participants, which has inherent difficulties in researching psychotherapeutic interventions), and attrition bias. Applying the GRADE system, we classified the quality of evidence as moderate. The possibility of significant publication bias was found, although the funnel plot asymmetry could be due to the different populations sampled in the studies. Our analyses were based on a limited number of trials overall and we were unable to conduct other sensitivity analyses because of the lack of power of potential comparisons.
Limitations
The review is based on a limited number of studies. The interventions that were investigated in the trials, despite being selected for inclusion because they met the descriptor for psychoanalytic psychotherapy, were diverse in relation to intensity, content and duration of treatment. We addressed this through comparing outcomes for subgroups for age, extent of self-harm and duration of therapy, and found no significant heterogeneity. However, it is difficult to identify which specific components had a therapeutic effect. This is further complicated by inconsistency of taxonomies of psychoanalytic psychotherapies, reflecting an apparent predisposition in the field for the constant invention of new labels for similar interventions; despite this, all interventions adhered to principles for psychoanalytic psychotherapy. Likewise, divergence in the way outcomes were measured and recorded, and variations in inclusion and exclusion criteria present challenges for the systematic reviewer. This includes the different definitions of self-harm used in various geographical areas. We had hoped to include suicidal ideation in the review but this is not reported in most studies, and in the few studies where it was reported there was no standardisation of measurement, so this was not possible. Finally, studies did not address patients’ experiences of therapy.
Implications for practice
Our systematic review of the effectiveness of psychoanalytic psychotherapy in reducing suicidal and self-harming behaviour provides some preliminary evidence that psychoanalytic psychotherapy can reduce the number of patients attempting suicide. There is some evidence that suicide attempts are reduced up to 12-month follow-up, and self-harm is reduced in the short term (6-month follow-up), but we found no evidence that psychoanalytic psychotherapy reduces self-harm more than the comparators at 12 months. An implication is that psychoanalytic psychotherapy can be used to aim to reduce self-harm more effectively up to 6 months after the end of treatment; the finding shows that comparators ‘catch up’ by 12 months. Further studies with longer-term follow-up (18 and 24 months) are needed to understand this better. Where we were able to pool findings at 18-month follow-up, for psychosocial functioning, we did find some evidence of an effect in favour of the intervention, which is consistent with other studies for psychoanalytic psychotherapy.Reference Abbass, Kisely, Town, Leichsenring, Driessen and De Maat13, Reference Driessen, Hegelmaier, Abbass, Barber, Dekker and Van15
There is some evidence of effectiveness in some risk factors for suicidal and self-harming behaviour. Psychoanalytic psychotherapy has a positive impact on psychosocial functioning, and thus on reducing problems, and reduces length of in-patient admissions. We note that meta-analyses of psychological therapies for self-harm and suicide reach broadly comparable conclusions, with some evidence for reducing repeated self-harm/suicide attempts and some reduction of associated risk factors together with findings where no evidence is found in favour of the interventions.Reference Hawton, Witt, Taylor Salisbury, Arensman, Gunnell and Hazell11 Hence, this review suggests that service providers could consider the use of psychoanalytic psychotherapy as an intervention that could be offered to individuals at risk of, or with a history of, suicidal or self-harming behaviour. No cost data were available with the trials included in the review, save one,Reference Bateman and Fonagy41 but these psychoanalytic psychotherapy interventions include structured, manualised approaches; in their Cochrane review of short-term psychoanalytic therapies, Abbass et al Reference Abbass, Kisely, Town, Leichsenring, Driessen and De Maat13 note that where psychoanalytic therapies are manualised and short term, these can be relatively inexpensive and might be a prudent first-line intervention before more extensive interventions are considered. It must be noted, however, that longer-term psychoanalytic psychotherapy is beginning to demonstrate effectiveness for a number of conditionsReference Driessen, Hegelmaier, Abbass, Barber, Dekker and Van15 (in accordance with this review),Reference Amianto, Ferrero, Pierò, Cairo, Rocca and Simonelli39, Reference Bateman and Fonagy43, Reference Clarkin, Levy, Lenzenweger and Kernberg46 and thus its value should not be underestimated.
Future research
Our systematic review and meta-analysis suggest that psychoanalytic psychotherapy is potentially effective in the treatment of suicidal and self-harming behaviours, and in reduction of some of the risk factors for these behaviours. However, given the relatively small number of RCTs meeting the criteria for inclusion in the analysis and the presence of bias in these studies, including potential publication bias, there is a need for further high-quality research. Future studies should also focus on specific diagnostic and problem categories to provide practitioners with evidence with which to consider these treatments for specific populations. Studies should also examine specific treatment factors and their contributions to outcomes across therapy models. Studies should ensure that follow-up is conducted over the longer term, up to at least 24 months after the end of treatment.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjp.2019.33.









eLetters
No eLetters have been published for this article.