Geographical variation in the prevalence of common mental disorders has been observed for many years in Britain (Reference Lewis and BoothLewis & Booth, 1992; Reference Weich, Lewis and JenkinsWeich et al, 2001). Traditionally this variation has been attributed to differences in the population composition rather than in the contextual characteristics. The advent of the statistical technique of multi-level analysis has made it possible to investigate the effect on mental health of both compositional and contextual variables in the same model. The few studies carried out so far have generally found negative results for the effect of place (Reference Duncan, Jones and MoonDuncan et al, 1995; Reference Weich, Twigg and HoltWeich et al, 2003a ; further details available from G.L. on request). From the risk factors studied, measures of aggregate deprivation failed to reach statistical significance after adjustment for the individual-level (compositional) variables (Reference Reijneveld and ScheneReijneveld & Schene, 1998; Reference Weich, Twigg and HoltWeich et al, 2003b ). However, this is a relatively new field and further research is required. In the present study we investigated whether differences in mental health in Wales would persist after taking into account the individual characteristics. We also tested the hypothesis that individuals living in more deprived areas would have worse mental health.
METHOD
Description of the data-set
The 1998 Welsh Health Survey (National Assembly for Wales, 1999) was a cross-sectional postal survey carried out in Wales with the aim of collecting information on various aspects of the physical and mental health of adults aged 18 years and over living in Wales. The research instrument used in the survey included the Short-Form 36 health survey (SF–36) (Reference Ware and SherbourneWare & Sherbourne, 1992). The sample was drawn from electoral registers of the 22 regional unitary authorities of Wales. Small authorities were slightly oversampled to achieve the required sample size. The current study included 26 710 individuals who had data on the SF–36. The response rate was 60%, with a range across regions of between 50.4% in Wrexham and 65.4% in Powys. The main fieldwork was carried out between May and August 1998.
Information on Wales
Wales occupies a broad peninsula on the western side of Great Britain, with a total area of 20 760 square kilometres and a population of approximately 2.9 million in 2001. The average population density is lower than that in England but in the industrialised south is comparable to other highly populated areas in Britain. The median population (mid-year estimates in 2001) in the 22 regional unitary authorities was 122 850, with a range between 55 900 in Merthyr and 305 200 in Cardiff.
Measures
Assessment of common mental disorders
The main outcome used in the present study was psychiatric morbidity, as measured by the mental health index included in the SF–36. The SF–36 (Reference Ware and SherbourneWare & Sherbourne, 1992) is an instrument widely used to assess the health status of patients and it has also been used in community studies. The psychometric properties of the SF–36 were tested in a study in the UK general population and the mental health index showed good internal consistency (Cronbach's α=0.83; Reference Jenkinson, Coulter and WrightJenkinson et al, 1993). In addition, a study carried out in Wales compared the mental health index with the 12-item General Health Questionnaire (GHQ–12), an instrument commonly used to assess common mental disorders in the community, and found it to be comparable (Reference Winston and SmithWinston & Smith, 2000).
The mental health index is a set of five questions asking about the presence of negative (three questions) or positive (two questions) feelings during the past 4 weeks. The five questions used for the index are:
-
(a) Have you been a very nervous person?
-
(b) Have you felt so down in the dumps that nothing could cheer you up?
-
(c) Have you felt calm and peaceful?
-
(d) Have you felt downhearted and low?
-
(e) Have you been a happy person?
Each of the questions has six response categories ranging from ‘all of the time’ to ‘none of the time’. For the purposes of the present paper we reversed the order of scoring for the three negative questions and therefore a higher score on the index represents greater psychiatric morbidity. We then transformed the raw scores (ranging from 5 to 30) on a scale from 0 (no morbidity) to 100 (high morbidity). In our analysis we used the transformed scores as a continuous variable. It should be noted that this simple instrument assumes that common mental disorders represent a single dimension. Several epidemiological studies have confirmed the usefulness of this assumption for the common mental disorders of depression or anxiety (Reference Goldberg and HuxleyGoldberg & Huxley, 1992).
Individual characteristics
Information on the following individual-level variables was available: age, gender, marital status (coded in four categories: single; divorced; widowed; married/living as couple), employment status (coded in four categories: employed full-time or part-time; unemployed or unable to work because of long-term disability; retired; economically inactive), the Registrar General's social class based on the participant's present or most recent occupation (coded in five categories: I/II; III, non-manual; III, manual; IV/V; missing values), and housing tenure status (either owner or tenant).
Deprivation at the authority level
Levels of deprivation across regions were estimated with the Welsh Index of Multiple Deprivation (National Assembly for Wales, 2004). This is a composite measure developed by the local government data unit with the aim of modelling levels of deprivation in Wales and supporting policy development and targeting of resources. The data used in the derivation of the index are based on direct measures of deprivation at the small-area level (the electoral division level). Data from the following domains were included: income, employment, health, education, housing and geographical access to services. Detailed information for the derivation of this index is given elsewhere (National Assembly for Wales, 2004). For the purposes of the present paper we used the average electoral division rank. This was a number between 104 for the most deprived area and 708 for the least deprived area. For easier interpretation of the index we subtracted the actual score from 1000 and therefore the new score has a median of 558 and a range of 292–896, with a higher score meaning a higher level of deprivation. The 22 regions were categorised further into three groups according to their deprivation score, as follows: low level of deprivation (scores of 292–490), middle level of deprivation (491–651) and high level of deprivation (652–896). The cut-offs chosen were the 25th (490) and 75th (651) percentiles of the transformed score on the deprivation index.
Statistical analysis
Analyses were carried out with MLWin software (Reference Rasbash, Brown and GoldsteinRasbash et al, 2001). The score on the mental health index was used as the continuous dependent variable in a hierarchical linear regression model. The estimation procedure applied was the restricted iterative generalised least-squares method (Reference GoldsteinGoldstein, 1995), which leads to unbiased estimates of the random parameters. The P values were based on Wald's test (two-sided). Our strategy for the analysis consisted first of fitting a simple variance component model (null model) to identify the two components of variation: that between regions (level 2 variance) and that between individuals within a region (level 1 variance). The next step was to include all level 1 variables in the model. The level 1 variables were entered as fixed effects, which assumes that they are related to the mental health index in the same way across level 2 units. The degree to which the estimated level 2 variance decreased after entering the explanatory level 1 variables indicated how well the model explained the between-region variance. To examine whether deprivation at the regional level was associated independently with the mental health of the individuals, we first entered the deprivation variable into the null model (to obtain crude estimates) and then adjusted for all level 1 variables. The deprivation index was entered as a categorical variable, using dummy variables for the categories of middle and high level of deprivation. We also explored graphically whether differences in mental health between regions persisted after taking into account the individual characteristics and regional deprivation, by plotting the 22 residuals in the null model after adjustment for individual variables and after adjustment for both individual variables and regional deprivation.
RESULTS
A greater proportion of the participants were female (54.8%, n=14 629), married/living as a couple (66.4%, n=17 730) and employed full-time/part-time (51.9%, n=13 851). The mental health index had a mean of 27.96 (s.d.=18.97).
Table 1 shows the hierarchical structure of the data and the crude regional averages of the mental health index. Regions have been arranged in rank order of their social deprivation indices. There are differences between regions, with a high average of 32.7 (s.d.=20.5) in Blaenau Gwent and a low of 25.1 (s.d.=17.6) in Monmouthshire. There is a strong relationship between the rank order of regional deprivation and the rank order of the mental health index, with Spearman's ρ=0.60 (P=0.003).
Table 1 The hierarchical structure of the data-set
| Level 2: local unitary authorities (n=22) | Welsh Index of Multiple Deprivation1 (rank) | Level 1: individuals (n=26710) | Mean (s.d.) MHI2 score (rank) |
|---|---|---|---|
| Monmouthshire | 292 (1) | 863 | 25.1 (17.6) (2) |
| Vale of Glamorgan | 365 (2) | 1062 | 25.8 (17.3) (6) |
| Flintshire | 434 (3) | 1307 | 26.8 (18.3) (10) |
| Powys | 455 (4) | 1132 | 25.3 (18.3) (4) |
| Cardiff | 490 (5) | 2884 | 28.4 (18.9) (14) |
| Ceredigion | 496 (6) | 890 | 26.0 (18.0) (8) |
| Conwy | 505 (7) | 958 | 25.9 (18.2) (7) |
| Denbighshire | 535 (8) | 879 | 26.2 (19.1) (9) |
| Swansea | 537 (9) | 2061 | 27.3 (18.9) (11) |
| Newport | 553 (10) | 1118 | 29.1 (19.0) (16) |
| Wrexham | 558 (11) | 934 | 28.1 (19.5) (13) |
| Bridgend | 570 (12) | 1127 | 28.6 (18.2) (15) |
| Pembrokeshire | 595 (13) | 1034 | 25.2 (18.0) (3) |
| Torfaen | 597 (14) | 908 | 31.1 (20.4) (20) |
| Gwynedd | 627 (15) | 1076 | 25.4 (17.1) (5) |
| Isle of Anglesey | 639 (16) | 888 | 25.0 (17.1) (1) |
| Carmarthenshire | 651 (17) | 1281 | 27.5 (18.6) (12) |
| Rhondda Cynon Taff | 734 (18) | 1980 | 30.2 (19.4) (18) |
| Caerphilly | 843 (19) | 1426 | 30.9 (20.2) (19) |
| Neath Port Talbot | 845 (20) | 1245 | 29.2 (19.7) (17) |
| Blaenau Gwent | 884 (21) | 874 | 32.7 (20.5) (22) |
| Merthyr Tydfil | 896 (22) | 783 | 32.6 (21.0) (21) |
Null model
The intercept-only model is presented in Table 2. The constant value of 27.85 (s.e.=0.51) represents the average mental health score across regions. This value does not remain constant across regions and the random effect variances are presented. Most variance occurs at level 1 (individuals) and only 1.47% of the total (unexplained) variance occurs at level 2 (95% CI 0.56–2.38). Although small, this amount of variation at the regional level is statistically significant (P=0.002).
Table 2 Variance and percentage of total unexplained variance at the individual and regional level in mental health index scores1 (Welsh Health Survey, 1998)

| Null model | Model 1 (null+individual variables2) | Model 2 (model 1+regional deprivation3) | |
|---|---|---|---|
| Variance (standard error) | |||
| Level 2 (regions) | 5.31 (1.68) | 3.15 (1.04) | 1.56 (0.56) |
| P=0.002 | P=0.002 | P=0.005 | |
| Level 1 (individual) | 355.25 (3.07) | 315.67 (2.77) | 315.67 (2.77) |
| Total unexplained variance | 360.56 | 318.82 | 317.23 |
| % of unexplained variance at level 2 (95% Cl) | 1.47% (0.56-2.38) | 0.99% (0.35-1.63) | 0.49% (0.14-0.84) |
| % of unexplained variance at level 1 (95% Cl) | 98.53% (96.86-100) | 99.01% (97.31-100) | 99.50% (97.80-100) |
Inclusion of individual characteristics and regional deprivation
Model 1 in Table 2 shows the degree to which the two variances are decreased after entering the individual characteristics into the model. It can be seen that the total unexplained variance at level 2 is reduced by 32.6% but is still significant. Further adjustment for regional deprivation (model 2) led to a 50% reduction in the total unexplained variance at level 2, but this remained significant (P=0.005).
Association between regional deprivation and common mental disorders
Table 3 shows the association between level 2 deprivation and scores on the mental health index before and after adjustment for individual-level socio-demographic characteristics. It can be seen that the regional deprivation level is associated with common mental disorders, even after adjustment for the characteristics of individuals (likelihood ratio test=13.6 on 2 d.f.; P=0.001).
Table 3 Association between psychiatric morbidity1 and regional deprivation in 26 710 subjects residing in 22 regions of Wales, UK

| Two-level regression parameter (standard error) | ||
|---|---|---|
| Unadjusted | Adjusted for individual-level variables2 | |
| Deprivation score3 | ||
| Low | Reference | Reference |
| Middle | 0.79 (0.83) | 0.17 (0.72) |
| High | 4.72 (0.98) | 3.11 (0.86) |
Regional residuals
Figure 1 presents the specific residuals for the 22 regions in the null model, after adjustment for individual characteristics (model 1) and after adjustment for both individual characteristics and regional deprivation (model 2). The residuals represent departures of each region from the average score on the mental health index, predicted by the fixed part of the multi-level model. A positive residual means that this particular region is associated with a higher morbidity. In the null model, 13 out of the 22 residuals were significantly different from zero. Adjustment for individual variables did not have a significant impact on regional mental health differences because 12 regions still had significant residuals. After adjustment for regional deprivation, regional differences were reduced substantially and only seven regions had residuals significantly different from zero. This effect was more evident in regions where the crude association between deprivation and common mental disorders was high, such as Rhondda Cynon Taff, Caerphilly, Blaenau Gwent and Merthyr.
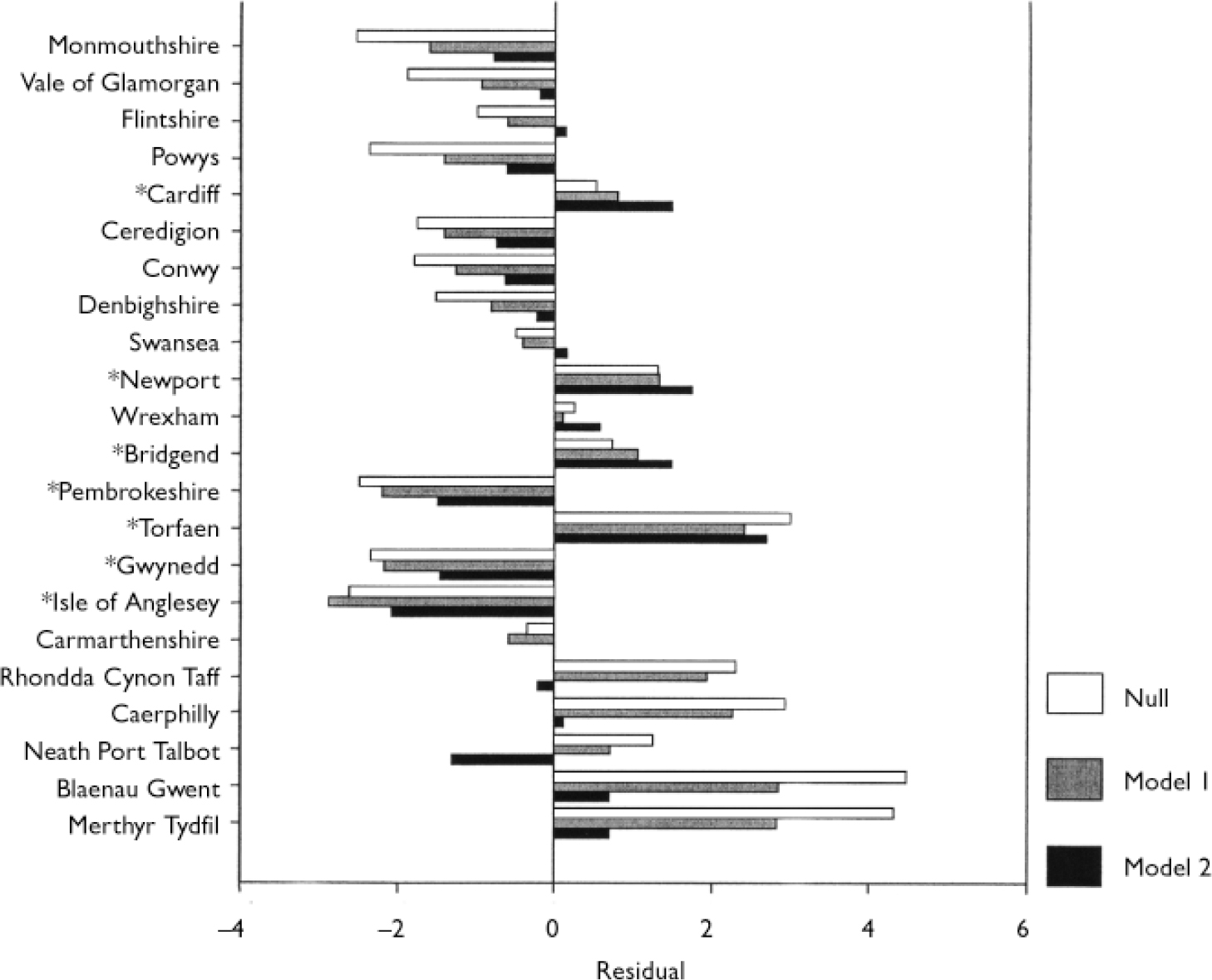
Fig. 1 Mental health differences across the 22 regions of Wales, UK. The bars show the residuals from a two-level linear regression in the null model, after adjustment for individual socio-demographic characteristics (model 1) and after additional adjustment for regional deprivation (model 2). Significant residuals in the full model (model 2) are noted by asterisks.
DISCUSSION
Main findings
In this cross-sectional postal survey we found significant differences in psychiatric morbidity, as measured by a brief self-completed questionnaire, between the 22 administrative regions of Wales. These differences persisted (although they were reduced) after taking into account the characteristics of the individuals. Regional deprivation was associated independently with psychiatric morbidity and explained part of the variation at the regional level.
Limitations of the study
Certain limitations should be considered before interpreting these results. First, it has been pointed out by others that there is a lack of theory on the mechanisms that link area of residence and health in general, or mental health in particular (Reference Macintyre, Ellaway and CumminsMacintyre et al, 2002; Reference O'CampoO’Campo, 2003). The study of the effects of area of residence on mental health is so limited that our study is mainly exploratory in nature. Although we hypothesised that a measure of deprivation at the regional level would be associated with common mental disorders, our finding should be interpreted more as a preliminary effort that can help the generation of new hypotheses, rather than as an indication that this specific factor might ‘explain’ mental health differences across regions. Second, we used large administrative areas as our higher level of aggregation, and our analysis included only two levels. We did not have data on other intermediate levels, such as the electoral ward. However, for the specific hypothesis of our study this design is adequate. Third, the cross-sectional design is certainly limited and issues related to reverse causality and duration of exposure can be dealt with only by longitudinal designs. Fourth, we assessed common mental disorders in a crude way, using a simple five-item self-reported measure. Although this measure has been found to be comparable with other similar instruments, such as the GHQ–12, a degree of random misclassification will be inevitable and may have biased our results in either direction. Finally, this was a postal survey with an average response rate of 60%. The most likely effect of this relatively low response is type II errors, but if there were an association between regional deprivation, common mental disorders and probability of response to the survey, the results could be biased in either direction.
Area effects
Previous research that aimed to investigate the effect of area of residence on mental health has observed generally that, once individual characteristics have been taken into account, the amount of variation attributed to the higher levels is very small and not significant (Reference Duncan, Jones and MoonDuncan et al, 1995; Reference Weich, Twigg and HoltWeich et al, 2003a ; further details available from G.L. on request). Our own estimates are somewhat higher and statistically significant. A number of reasons may explain this discrepancy: the choice of instruments to measure psychiatric morbidity (other studies mainly have used the General Health Questionnaire) may have contributed to this diffference; and the power of previous studies to find a statistically significant difference may have been compromised by the choice of the higher level. With regard to the latter, it has been argued (Reference Snijders and BoskerSnijders & Bosker, 1999; Reference Diez RouxDiez Roux, 2004) that the power to detect the higher level variance component is influenced by the number of individual observations in each group. A greater number of higher level groups with relatively few individual observations per group will yield large standard errors and may have insufficient power to detect a significant variance component at this level (although it will maximise the power to detect an association between a higher level risk factor and the individual outcome). It is interesting to note that most previous studies have used either the postcode or the electoral ward as the higher level and this resulted in a small number of observations per group in the range of 14–23 persons. In contrast, our own study had a mean of 1214 individual observations per region. The study by Duncan et al (Reference Duncan, Jones and Moon1995) used the regions in Britain as the higher level but this study failed to find a significant result even in the null model.
Our study consisted of two levels of analysis whereas previous studies included a third intermediate level, most commonly the household level, and this may be a further reason for our significant results (or the non-significant results of previous studies) on the variation attributed to the higher levels. It should be noted that previous studies had selected more than one individual per household and this made necessary the inclusion of the household level to take account of the clustering of observations. In our own study only one individual per household was selected. Failure to include the household level in multi-level studies of mental health has been criticised in the past (Reference Weich, Twigg and HoltWeich et al, 2003b ). However, inclusion of an intermediate level will also increase the chances of overadjustment, which is considered an important problem in multi-level research (Reference Diez RouxDiez Roux, 2004). For example, if the effects of area of residence on individual mental health are mediated through unknown household factors, then inclusion of this level will reduce the reported associations at the higher level (Reference Davey Smith, Hart and WattDavey Smith et al, 1998).
All studies that have investigated the effect of area of residence on several health outcomes generally have found small size effects, in the range of 1–5% of the total (unexplained) variance (Reference Boyle and WillmsBoyle & Willms, 1999). Our own result of 0.9% confirms these findings. Do these small figures have any public health importance? To answer this question one should take into account the possible ways in which a higher level context may affect an individual outcome. Blakely & Woodward (Reference Blakely and Woodward2000) have discussed this issue in detail. Contextual factors may have a direct effect on individual mental health or they may influence other intervening variables that mediate their effect. It has been argued that a direct effect is not possible because it will require a final reduction to an individual process. However, as Blakely & Woodward (Reference Blakely and Woodward2000) rightly point out, such reductionism is not helpful in public health terms because knowledge of one component of a causal chain may be sufficient for public health interventions. In addition, modifications of higher level risk factors are more efficient from a public health perspective compared with interventions that target individuals. Certainly, further research is needed to understand better what constitutes an adequate amount of explained variation (Reference Boyle and WillmsBoyle & Willms, 1999).
Association of deprivation with mental health
Our hypothesis that an index of regional deprivation would be associated with common mental disorders was confirmed in this data-set. The few previous studies that have investigated the same issue generally have found negative results, after taking into account the individual characteristics (Reference Reijneveld and ScheneReijneveld & Schene, 1998; Reference McCullochMcCulloch, 2001; Reference Weich, Twigg and HoltWeich et al, 2003b ). As mentioned before, the choice of levels of analysis and the problems of overadjustment may have contributed to this discrepancy. In addition, selection bias could be an alternative explanation. Individuals select the places they live and the (unidentified) individual factors that influence this selection may be responsible for the reported association. The resulting bias, however, could be in either direction (Reference Duncan, Magnuson and LudwigDuncan et al, 2004).
Regional residuals
Analysis of the 22 regional residuals (Fig. 1) may shed more light on the reported association between regional deprivation and common mental disorders. The residuals reflect the unexplained variability between regions and from Fig. 1 several points can be made. First, adjustment for the individual variables generally had little effect on reducing the differences between regions. In contrast, further adjustment for regional deprivation had a significant effect and only 7 out of 22 regions had residuals significantly different from zero. Second, for most regions, adjustment for deprivation reduced the value of the residual. This effect was more evident in regions where there was a strong association between deprivation and common mental disorders. It can be seen from the figure that for Merthyr, Blaenau Gwent, Caerphilly and Rhondda Cynon Taff regional deprivation explained most of the variation. Third, for some regions (e.g. Cardiff and Newport) adjustment for regional deprivation had the opposite effect and the value of the residual was increased, indicating that other higher level variables, possibly related to the urban environment (Reference Weich, Twigg and HoltWeich et al, 2003b ), may be more relevant. Fourth, Pembrokeshire, Gwynedd and the Isle of Anglesey differed in that they had significant negative residuals even though they had more than the average regional deprivation. Whether this discrepancy is owing to the rural/urban difference in rates of common mental disorders is not known, but certainly requires further research.
Interpretation of the association between regional deprivation and common mental disorders is not easy. Regional deprivation is most probably a proxy for other unmeasured regional attributes and the pathways involved are likely to be complex and include feedback loops (Reference Diez RouxDiez Roux, 2004). Longitudinal studies may be of particular importance. However, clarification of these pathways will certainly require a combination of methods, both qualitative and quantitative.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ Mental health differences between regions in Wales persisted even after adjustment for individual characteristics.
-
▪ An index of regional deprivation was found to be associated independently with common mental disorders, even after adjustment for individual-level variables.
-
▪ Although the effect of area of residence on mental health appears to be small, it may be important from a public health perspective.
LIMITATIONS
-
▪ Research into the effect of area of residence on mental health is still limited and our study is mainly of an exploratory nature.
-
▪ The contextual effects may vary with the number of levels used and our choice of levels may have influenced our results in either direction.
-
▪ Common mental disorders were assessed with a simple five-item questionnaire and this may have resulted in measurement bias.
Acknowledgements
The study was funded by the National Assembly for Wales. However, the views. expressed in this report are those of the authors alone. We thank Dr Kate. Chamberlain of the Welsh local government data unit for providing us with. information on the Welsh Index of Multiple Deprivation.







eLetters
No eLetters have been published for this article.