Emergency department presentations for self-harm and attempted suicide are increasing in a number of countries, including the USA, UK and New Zealand. Reference Larkin and Beautrais1–Reference Gibb and Beautrais4 Those who present to hospital with self-harm are at increased risk of a range of negative outcomes, including further self-harm and death. Reference Crandall, Fullerton-Gleason, Aguero and LaValley5–Reference Owens, Horrocks and House7 A systematic review found repetition rates for self-harm after an index hospital visit for non-fatal self-harm were 16% within the first year and 23% within 4 years; the rate of suicide in the 9 years following self-harm was almost 7%. Reference Owens, Horrocks and House7 These high rates of morbidity and mortality in those presenting with self-harm have prompted the development of interventions to reduce the risk of further suicidal behaviour following a hospital self-harm presentation. Interventions shown to significantly reduce further suicidal behaviour include follow-up telephone calls, Reference De Leo, Dello Buono and Dwyer8,Reference Vaiva, Vaiva, Ducrocq, Meyer, Mathieu and Philippe9 cognitive therapy Reference Brown, Ten Have, Henriques, Xie, Hollander and Beck10 and psychodynamic interpersonal therapy. Reference Guthrie, Kapur, Mackway-Jones, Chew-Graham, Moorey and Mendel11 However, some of these interventions are time consuming and costly to deliver. An easily administered, low-cost alternative is the ‘postcard’ intervention, first proposed by Motto, Reference Motto12,Reference Motto and Bostrom13 and more recently evaluated by Carter. Reference Carter, Clover, Whyte, Dawson and D'Este14,Reference Carter, Clover, Whyte, Dawson and D'Este15 Carter's trial consisted of eight postcards mailed to participants during the 12 months following their hospital admission for self-poisoning. In a randomised controlled trial (RCT), the postcard intervention almost halved the number of readmissions for self-poisoning in the intervention group in the 12 months following the index admission, with this reduction maintained for 24 months after the index admission. However, the benefits of the postcard intervention appeared to be confined to a relatively small subsample of participants. Specifically, the reduction in readmission rates in the intervention group appeared to be almost entirely the result of a large reduction in the number of repeat visits among women who were frequent self-poisoning repeaters. These results suggested that the effectiveness of the postcard intervention may be confined to selected subgroups of individuals who self-harm (female frequent emergency department attenders, people who live alone and/or are socially isolated); further trials are necessary to establish the effectiveness of the intervention in different patient groups.
The aim of our study was to examine whether a postcard intervention reduced self-harm re-presentations to the psychiatric emergency service in a sample of individuals presenting to this service in Christchurch, New Zealand, following an episode of self-harm.
Method
Study population
The recruitment population consisted of all individuals aged 16 and older who presented to psychiatric emergency services at Christchurch Hospital, New Zealand, following self-harm or attempted suicide during the period 1 August 2006 to 6 April 2007. The psychiatric emergency service is an acute psychiatric service affiliated with Christchurch Hospital and its staff see all individuals presenting to the Christchurch Hospital emergency department with self-harm or suicide attempts. Christchurch Hospital emergency department is the sole emergency department in the greater Christchurch area, serving a population of approximately 500 000 people.
Eligible patients were those who presented to the psychiatric emergency service following self-harm or attempted suicide, were normally resident at a New Zealand address, and were able to speak English sufficiently well to understand the study. Written informed consent was obtained from all participants prior to commencement of the study. The study was approved by the Upper South B Regional Ethics Committee. Eligibility for the study was assessed by the psychiatric emergency service's clinicians based on a psychiatric interview conducted as part of standard practice, which included mental status examination, psychiatric history and questions about current and previous suicide attempts and self-harm. Prior to enrolling individuals in the study, dedicated research staff who were not psychiatric emergency service clinicians checked eligibility by reviewing the department's records.
Intervention
Participants were randomised 1:1 by research staff into two groups (treatment as usual; treatment as usual plus the postcard intervention) using predetermined computer-generated random numbers. The psychiatric emergency service clinicians were masked to treatment allocation. Treatment as usual consisted of crisis assessment and referral to in-patient community-based mental health services. The intervention consisted of a series of six ‘postcards’ sent by mail during the 12 months following the participant's index presentation for suicide attempt or self-harm. The text and format of the postcard were based on those used by Carter and colleagues. Reference Carter, Clover, Whyte, Dawson and D'Este14,Reference Carter, Clover, Whyte, Dawson and D'Este15 The postcard read: ‘It has been a short time since you were here at PES (Psych Emergency), and we hope things are going well for you. If you wish to drop us a note we would be happy to hear from you'. (We used six rather than the eight postcards Carter used for several reasons: no strong justification has been presented for eight postcards; we were seeking to establish the minimum number of postcards that would be effective so that the intervention could be translated to a real-world situation in which secretarial staff would send the postcards routinely, and, based on consultation with Carter, who suggested earlier postcards might be the effective element, we decreased the number of later, and thereby, overall, postcards).
Postcards were printed on A4 paper and posted in a plain sealed envelope to the participant's residential address. Postcards were posted at the following times after the index presentation: 2 and 6 weeks; 3, 6, 9 and 12 months. The envelope included a return address so that undelivered postcards could be returned. The return address consisted only of a code and a post office box number so that the source of the letter could not be identified from the outside of the envelope. When a postcard was returned research staff endeavoured to obtain the participant's new address using both the contact details that the participant had provided at the index interview, and contact details from the departmental records. If a new address was found for the participant, the letter was re-sent to the new address. If no new address could be found for the participant, the letter was not re-sent.
Sample size and power
Initial power calculations, based on estimated re-presentation rates of 20% for the control group and 12% for the intervention group, yielded a required sample size of 700 (350 per group) in order to detect differences at the P<0.05 level with 80% power. Recruitment was therefore commenced with a planned sample size of 700. However, after 8 months of recruitment, inspection of preliminary results revealed a larger than anticipated difference between intervention and control groups in the rate of re-presentation to the psychiatric emergency service for further self-harm. In addition, over the first 8 months of the trial there had been ongoing difficulties with recruitment procedures, with clinical staff reluctant to recruit participants to the trial. Therefore, consideration was given to stopping the trial early. The P required for overall type I error of 0.05 with one interim test was calculated to be 0.015 using the Fleming, Harrington and O'Brien boundary. Reference Fleming, Harrington and O'Brien16 Comparison of the rate of further self-harm in the intervention and control groups revealed that the difference was significant at P<0.001 (mean number of further psychiatric emergency service visits per 100 people: 14.4 v. 33.3, odds ratio (OR) = 0.43). Therefore, the trial was stopped after 8 months of recruitment with a sample size of 327.
Measures
Demographic data
Baseline demographic information including age, gender, marital status and method of self-harm was collected as part of the standard procedures of the psychiatric emergency service.
History of self-harm
Participants' hospital medical records were reviewed to identify any presentations to Christchurch Hospital emergency department for self-harm in the 12 months prior to the index presentation.
Outcome measures
Re-presentations for self-harm were assessed by monitoring two sources of re-presentation information. First, psychiatric emergency service records were checked daily by research staff to identify attendances by study participants. Second, participants' hospital medical records were reviewed at the conclusion of the 12-month follow-up period to identify visits to Christchurch Hospital emergency department for self-harm in the year following the index presentation. Three measures of re-presentation were calculated from these data: re-presentations to psychiatric emergency service, re-presentations to Christchurch Hospital emergency department and total re-presentations to either the psychiatric emergency service or emergency department.
Assignment and masking
Randomisation was based on a random number sequence available only to research staff. The number sequence was computer-generated in SAS 9.1 for Windows using a uniform distribution to generate a sequence of random numbers between 0 and 1. Numbers of 0.5 or above were classified as the intervention group; numbers below 0.5 were classified as the control group. Randomisation was performed post-recruitment and post-consent by research staff who were not involved in the recruitment or clinical care of participants. Participants' randomisation status was not conveyed to clinical or data-collection staff. Clinical staff assisted participants to complete the forms required to enrol in the study. Completed forms were forwarded to research staff daily. Research staff then allocated participants to the control or intervention group based on the pre-generated random number sequence. In order to prevent duplicate enrolments, clinical staff checked details of eligible individuals against a list of participants who had already enrolled in the study. This list was updated daily. Participant details were checked against the list again by research staff prior to randomising participants.
Statistical analysis
All statistical analysis was performed in SAS 9.1 for Windows. The results of the trial were analysed using the intention-to-treat design. Comparisons of rates of re-presentation in the control and intervention groups were conducted by fitting a Poisson regression in which the number of re-presentations was modelled as a function of randomisation status. Comparisons of the proportions of individuals re-presenting in the control and intervention groups were conducted by fitting a logistic regression in which the log odds of re-presentation was modelled as a function of randomisation status. Adjustments for prior self-harm were made by including the number of prior self-harm presentations as a covariate in the regression model. Covariate-adjusted re-presentation rates were calculated using the methods described by Lee. Reference Lee17
Results
Participant flow and follow-up
A total of 541 people were eligible for the study during the recruitment period. Of these, 327 were enrolled (a recruitment rate of 60.4%); 153 participants were randomised to the intervention group and 174 randomised to the control group. For the majority of participants, self-harm involved self-poisoning (n = 250 (76.7%); cutting: n = 47 (14.4%); hanging: n = 11 (3.4%); vehicle exhaust carbon monoxide poisoning: n = 6 (1.8%); motor vehicle crash: n = 6 (0.9%); other methods: n = 9 (2.7%)). Figure 1 summarises the flow of participants through the study.
Analysis
Table 1 compares self-harm re-presentations for the intervention and control groups over the 12-month follow-up period. The intervention and control groups are compared on two re-presentation measures: the proportion of participants re-presenting at least once for self-harm during the follow-up period; and the total number of self-harm re-presentations per 100 people over the follow-up period. For each measure, re-presentation was assessed in three ways: re-presentations to the psychiatric emergency service; re-presentations to the emergency department; and total re-presentations to either the psychiatric emergency service or emergency department.
Table 1 Re-presentation for self-harm in the 12 months following the index presentation

| Intervention | Control | P | OR (95% CI) | IRR (95% CI) | |
|---|---|---|---|---|---|
| Re-presentation for self-harm, % | |||||
| To psychiatric emergency service | 15.0 | 23.6 | < 0.06 | 0.57 (0.33-1.01) | — |
| To emergency department | 25.5 | 27.0 | > 0.75 | 0.92 (0.56-1.52) | — |
| Total (psychiatric emergency service or emergency department) | 25.5 | 28.2 | > 0.58 | 0.87 (0.53-1.43) | — |
| Number of self-harm re-presentationsa | |||||
| To psychiatric emergency service | 23.5 | 51.1 | < 0.0001 | — | 0.46 (0.31-0.68) |
| To emergency department | 53.6 | 71.8 | < 0.04 | — | 0.75 (0.56-0.99) |
| Total (psychiatric emergency service or emergency department) | 56.9 | 78.2 | < 0.03 | — | 0.73 (0.56-0.95) |
The postcard intervention was not associated with a significant reduction in the proportion of participants re-presenting to the emergency department (OR = 0.92, P>0.75) or in the total proportion of participants re-presenting to either the psychiatric emergency service or the emergency department (OR = 0.87, P>0.58). The intervention was, however, associated with a significant reduction in the proportion of participants re-presenting to the psychiatric emergency service (OR = 0.57, P<0.06). When re-presentation was measured using the total number of re-presentations over the 12-month follow-up period, the intervention was associated with a significant reduction in the number of re-presentations to psychiatric emergency service (incident risk ratio, IRR = 0.46, P<0.0001). The intervention was also associated with reductions in the total number of re-presentations to the emergency department (IRR = 0.75, P<0.04) and to either the psychiatric emergency service or the emergency department (IRR = 0.73, P<0.03), although the significance of these effects was marginal due to P exceeding the adjusted boundary P value of 0.015.
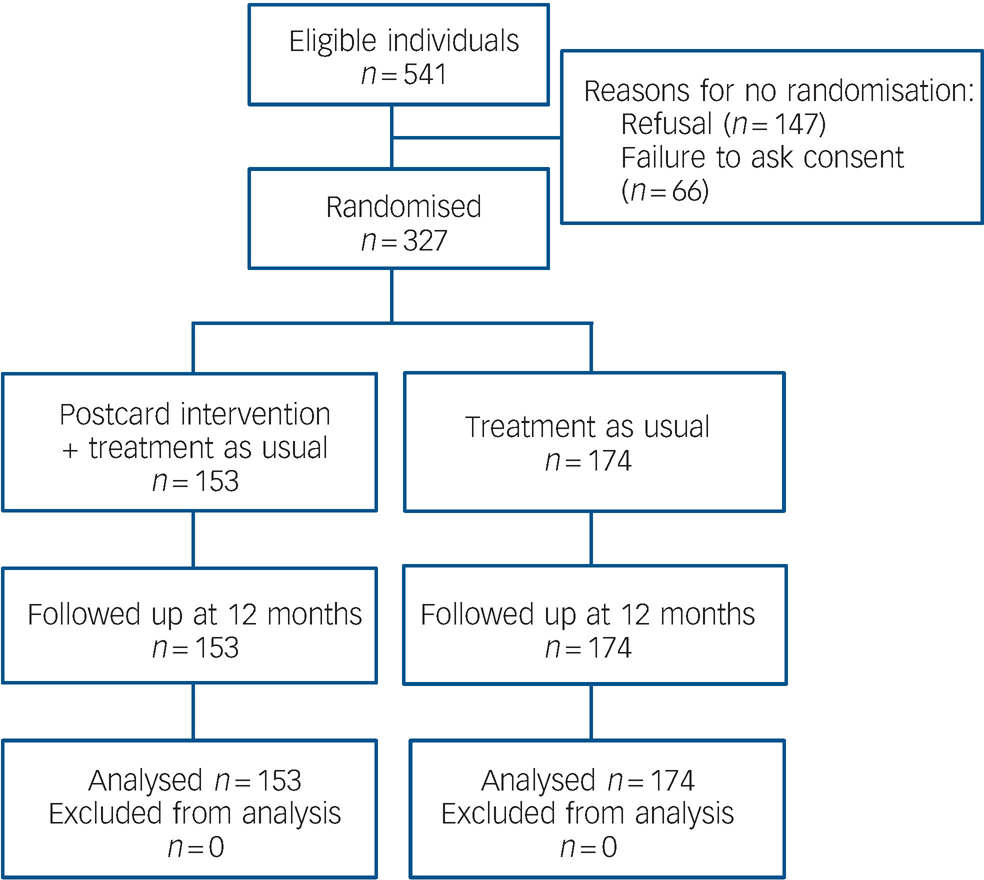
Fig. 1 Flow of participants through the trial
Although the results in Table 1 indicated that the intervention was associated with a reduction in the total number of self-harm re-presentations in the 12-month follow-up period, it is important to consider whether this difference arises from pre-existing differences between the two groups. Table 2 compares the control and intervention groups on a series of demographic and background factors, reporting P for significance from a t-test for independent means (for the continuous measures) or a chi-squared test for independence (for the dichotomous measures).
Table 2 Comparison of control and intervention groups at the time of the index presentation

| Intervention | Control | P | |
|---|---|---|---|
| Age, years: mean | 33.8 | 33.9 | > 0.92 |
| Female, % | 70.4 | 62.3 | > 0.12 |
| Married/de-facto, % | 31.0 | 29.3 | > 0.73 |
| Self-poisoning, % | 75.0 | 78.2 | > 0.50 |
| Visit for self-harm in past 12 months, % | 15.8 | 19.4 | > 0.39 |
| Number self-harm visits in past 12 months, mean | 0.31 | 0.61 | < 0.07 |
| Number of nights in hospital, mean | 0.90 | 0.98 | > 0.73 |
There were no significant differences between the intervention and control groups in age, gender, marital status, method of self-harm, length of hospital stay or history of attendance for self-harm in the 12 months prior to the index presentation (all P>0.12). However, there was a significant difference between the groups in the number of prior attendances for self-harm in the previous 12 months (P<0.07), with the number of prior attendances being lower in the intervention than in the control group.
The results in Table 2 suggest that the reduced number of re-presentations for self-harm in the intervention group reported in Table 1 may reflect a pre-existing tendency for those in the intervention group to have lower numbers of prior hospital attendances for self-harm. Therefore, we adjusted re-presentation rates in Table 1 for the total number of hospital attendances for self-harm in the 12 months prior to study entry.
Table 3 shows the proportion of participants re-presenting, and the adjusted total number of re-presentations, in the 12-month follow-up period in the control and intervention groups, adjusted for number of hospital visits for self-harm in the 12 months prior to study enrolment. Adjusting for the number of prior hospital visits for self-harm reduced, and in many cases removed, the effect of the intervention on re-presentation for self-harm. After adjustment, there was no significant difference between control and intervention groups in the proportion of participants re-presenting with self-harm to the psychiatric emergency service (OR = 0.64, P>0.13), to the emergency department (OR = 1.04, P>0.88) or to either the psychiatric emergency service or the emergency department (OR = 0.97, P>0.91). Furthermore, the intervention was not associated with a reduction in the total number of re-presentations for self-harm to the emergency department (IRR = 1.10, P>0.52) or to either the psychiatric emergency service or the emergency department (IRR = 1.07, P>0.64). The intervention was associated with a reduction in the total number of re-presentations to the psychiatric emergency service (IRR = 0.65, P<0.04), but the significance of this effect must be considered marginal because the P for significance exceeds the adjusted boundary P value of 0.015.
Table 3 Re-presentation for self-harm in the 12 months following the index presentation, adjusted for prior self-harm

| Intervention | Control | P | OR (95% CI) | IRR (95% CI) | |
|---|---|---|---|---|---|
| Re-presentation for self-harm, % | |||||
| To psychiatric emergency service | 16.2 | 22.5 | > 0.13 | 0.64 (0.36-1.15) | |
| To emergency department | 26.6 | 26.0 | > 0.88 | 1.04 (0.62-1.73) | |
| Total (psychiatric emergency service or emergency department) | 26.6 | 27.2 | > 0.91 | 0.97 (0.58-1.62) | |
| Number of self-harm re-presentationsa | |||||
| To psychiatric emergency service | 28.7 | 44.1 | < 0.04 | 0.65 (0.43-0.98) | |
| To emergency department | 67.2 | 61.0 | > 0.52 | 1.10 (0.82-1.49) | |
| Total (psychiatric emergency service or emergency department) | 71.1 | 66.4 | > 0.64 | 1.07 (0.80-1.43) |
Discussion
The results of this RCT suggested that a postcard intervention did not significantly reduce self-harm re-presentations in individuals presenting to a psychiatric emergency service following an index episode of self-harm. Although unadjusted results suggested that the postcard intervention reduced the total number of self-harm re-presentations in the 12 months following the index presentation, comparison of control and intervention groups revealed that the intervention group had lower rates of self-harm presentations in the 12 months prior to trial entry. Adjusting for this pre-existing difference in prior self-harm removed the apparent effect of the intervention. These results suggest that any reduction in rates of further self-harm presentations in the intervention group in this trial could be explained by pre-existing differences between the control and intervention groups in their history of self-harm. When these pre-existing differences were accounted for, the postcard intervention did not reduce the rate of self-harm re-presentations in the 12 months following the index presentation. A marginally significant reduction in the number of re-presentations to the psychiatric emergency service was not substantiated by measures of re-presentation taken from hospital records.
Comparison with previous studies
The results of this study contrast with those from a previous RCT conducted by Carter and colleagues Reference Carter, Clover, Whyte, Dawson and D'Este14,Reference Carter, Clover, Whyte, Dawson and D'Este15 who reported that a postcard intervention reduced the total number of self-poisoning re-presentations by almost half in the 12 months following the index presentation, with this effect persisting for 24 months. The findings from our trial suggested that a very similar intervention did not reduce further self-harm re-presentations in the 12 months following the index presentation. Several possibilities may account for this discrepancy. The first is that the postcard intervention is more effective following self-poisoning than following other types of self-harm. The sample of participants in Carter's study was restricted to those presenting with self-poisoning, whereas the sample used in our study included those presenting with any method of self-harm. However, although individuals presenting with any method of self-harm were eligible for our study, the final sample consisted primarily (77%) of self-poisoning presentations. Analyses (not presented here) of only those who self-poisoned in our study found no significant reduction in re-presentations among those receiving the intervention.
Another possibility is that differences in treatment procedures and healthcare structures between the two study sites may have resulted in the intervention being differentially effective in the two different settings. Although Carter's study did not reveal the mechanism of action of the intervention, the authors suggested that postcards may be effective by enhancing a sense of social connectedness. The ability of the postcard intervention to increase feelings of social connectedness may be influenced by the overall treatment model, the level of support already available, and other similar factors that could be expected to vary across treatment settings. Therefore, it is possible that the effectiveness of the postcard intervention depends on the characteristics of the treatment setting, and the intervention may not effectively reduce further self-harm presentations in all settings.
Implications
This study highlights the importance of cross-checking key outcome measures in RCTs using multiple data sources. The results of this study suggested that the postcard intervention was associated with a reduction in the number of re-presentations to psychiatric emergency service for self-harm. However, cross-checking psychiatric emergency service data against hospital medical records suggested that re-presentations recorded in the psychiatric emergency service data were only a subset of the total re-presentations to the psychiatric emergency service and the emergency department. When these additional visits were considered, results suggested that the postcard intervention did not reduce the total number of re-presentations for self-harm.
This study also highlights the importance of testing for the possibility of pre-existing differences between control and intervention groups, even when apparently adequate randomisation and masking procedures have been used. Our study demonstrates that, in some cases, the apparent effects of an intervention may be explained by pre-existing differences in background characteristics between control and intervention groups.
Initial trial results and early stopping
A feature of this trial is that it was stopped early in response to interim data that suggested that the postcard intervention was associated with a large and statistically significant reduction in the number of self-harm re-presentations to the psychiatric emergency service. However, the final trial results contrasted with these interim findings and provided no evidence that the intervention significantly reduced the total number of self-harm re-presentations. This discrepancy between the interim and final results appears to be as a result of two factors. First, the interim data only assessed re-presentations to the psychiatric emergency service and did not include information about re-presentations to the emergency department. Cross-checking the psychiatric emergency service data with the emergency department data at the time of the final analysis revealed that re-presentations recorded in the psychiatric emergency service data were only a subset of the total number of re-presentations. Second, the interim data were not adjusted for history of self-harm because information about prior presentations for self-harm was not available at the time that recruitment was stopped. Had these additional sources of data been available at the time of the interim analysis, the outcome of the decision about early stopping may have been different. This suggests, therefore, that decisions regarding the early stopping of RCTs should be based on the widest range of data available, including baseline data that may indicate pre-existing group differences, and outcome data from multiple sources to enable cross-checking.
Staff reluctance to initiate change
Another reason for stopping this trial early was the reluctance of clinical staff to recruit individuals to the trial. We suspect this was part of a more generic institutional reluctance to change, and highlights the types of problems to be faced in conducting research projects in real-world settings.
Limitations
A limitation of this study was that, despite apparently strong randomisation and masking procedures, there remained a pre-existing difference between intervention and control groups in the history of prior hospital visits for self-harm. There is no apparent reason for this difference, given that individuals were randomised post-consent and all clinical and data collection staff were masked to participants' allocations. As in previous studies of hospital presentations for self-harm for example, see Carter et al Reference Carter, Clover, Whyte, Dawson and D'Este15 and Hall et al, Reference Hall, O'Brien, Stark, Pelosi and Smith18 the distribution of prior self-harm presentations in this study was skewed, with most participants having no prior presentations, and a small number of participants having a very high number of prior presentations. This distribution means that the inclusion of a very small additional number of individuals with high-frequency self-harm in one experimental group can have a substantial effect on overall rates of prior self-harm in that group. For this reason, it may be useful for future trials to adopt a stratified randomisation procedure, such as that used by Vaiva et al, Reference Vaiva, Vaiva, Ducrocq, Meyer, Mathieu and Philippe9 in which participants are split into two strata (low number of prior self-harm presentations and high number of prior self-harm presentations) prior to randomisation, and the randomisation process is then completed separately for each stratum.
It could be suggested that given the decision to terminate the study early, the present findings are as a result of the study being underpowered, and that had recruitment continued according to the original design, clear benefits of the intervention might have been observed. However, the findings from the reduced sample suggest that any possible benefits of the intervention were at best very modest and in most cases non-existent. It seems unlikely this conclusion would alter even with a substantially larger sample.
These limitations notwithstanding, the results of the current study suggest that the postcard intervention did not reduce self-harm re-presentations among those presenting to a general hospital psychiatric emergency service following self-harm. The results of further trials of postcard interventions may help to clarify whether this type of intervention effectively reduces self-harm re-presentations, and the specific patient groups and treatment settings in which the intervention is most effective.
Funding
This study was supported by grants from the Canterbury District Health Board and the Accident Compensation Corporation (ACC). S.J.G. was supported by a University of Otago Postgraduate Publishing Bursary.
Acknowledgements
We gratefully acknowledge the assistance of the staff from Psychiatric Emergency Services of the Canterbury District Health Board.







eLetters
No eLetters have been published for this article.