Whenever a new treatment concept is introduced, psychiatrists and other mental health professionals discuss the consequences for their own profession (Reference Brown, Crawford and DarongkamasBrown et al, 2000). Some fear the unknown, role blurring and the erosion of traditional professional practices whereas others hope for better teamwork, more flexible roles and better patient care (Reference RodenhauserRodenhauser, 1996; Reference OnyettOnyett, 1999; Reference Herrman, Trauer and WarnockHerrman et al, 2002). The main issue, however, seems to concern the tasks and responsibilities of psychiatrists in relation to other mental health professionals. Despite their legally assessed position in different countries (i.e. the Mental Health Act 1983 in the UK, the ‘law BIG’ in The Netherlands), psychiatrists have conflicting views on their responsibilities (Kennedy & Griffiths, Reference Kennedy and Griffiths2001, Reference Kennedy and Griffiths2002); other mental health professionals also have conflicting ideas about the responsibilities of psychiatrists (Reference Herrman, Trauer and WarnockHerrman et al, 2002). Hence, discussions between professional unions seldom lead to consensus, with members of each particular profession considering their contribution to patient care as more important than that of other professions (Reference Herrman, Trauer and WarnockHerrman et al, 2002). The distribution of tasks between psychiatrists and other mental health professionals has rarely been investigated and no standard has been developed (Reference Eveland, Dever and SchafEveland et al, 1998; Reference Faulkner, Scully and ShoreFaulkner et al, 1998; Reference Ivey, Scheffler and ZazzaliIvey et al, 1998; Reference Tyrer, Al-Muderis and GulbrandsenTyrer et al, 2001).
More agreement may help governments in workforce planning and mental healthcare institutions to organise a more appropriate distribution of tasks. This may be especially important when setting up new forms of collaboration, e.g. between mental health and social care (Reference Exworthy and PeckhamExworthy & Peckham, 1998). Increased clarity may also help patients in their search for the best equipped professional for their problems. Although the assignment of patients to professionals in mental healthcare often depends on pragmatic arguments such as availability, and on traditions at institutional, local or even national levels (Reference Hutschemaekers and NeijmeijerHutschemaekers & Neijmeijer, 1998; World Health Organization, 2001; Reference Druss, Marcus and OlfsonDruss et al, 2003), most professionals believe that their decisions are related to the task to be performed and the patients' problems.
The current pilot study was designed to outline this ‘collective sense of the profession’ of the relationship between patient characteristics and the tasks to be performed by psychiatrists and other professionals.
METHOD
We used an adapted form of the RAND appropriateness method, a formal group judgement method (Reference Brook, Chassin and FinkBrook et al, 1986; Reference Park, Fink and BrookPark et al, 1986; Reference Chassin and HopkinsChassin, 1989). This is a modified Delphi procedure in which a multidisciplinary expert team defines treatment options (indications) and patient characteristics (indicators). Consequently, professionals make an independent judgement of the appropriateness of indications given a specific set of indicators. In the current study the indications were defined as the contribution of a specific discipline to the diagnostic and treatment tasks given specific patient indicators. The indicators were described in written model cases of psychiatric patients. The whole judgement procedure consisted of four steps: (1) the selection of disciplines for the indications; (2) the choice of the indicators for the construction of a set of case descriptions; (3) the recruitment of the judges; and (4) the judgement procedure (Fig. 1).
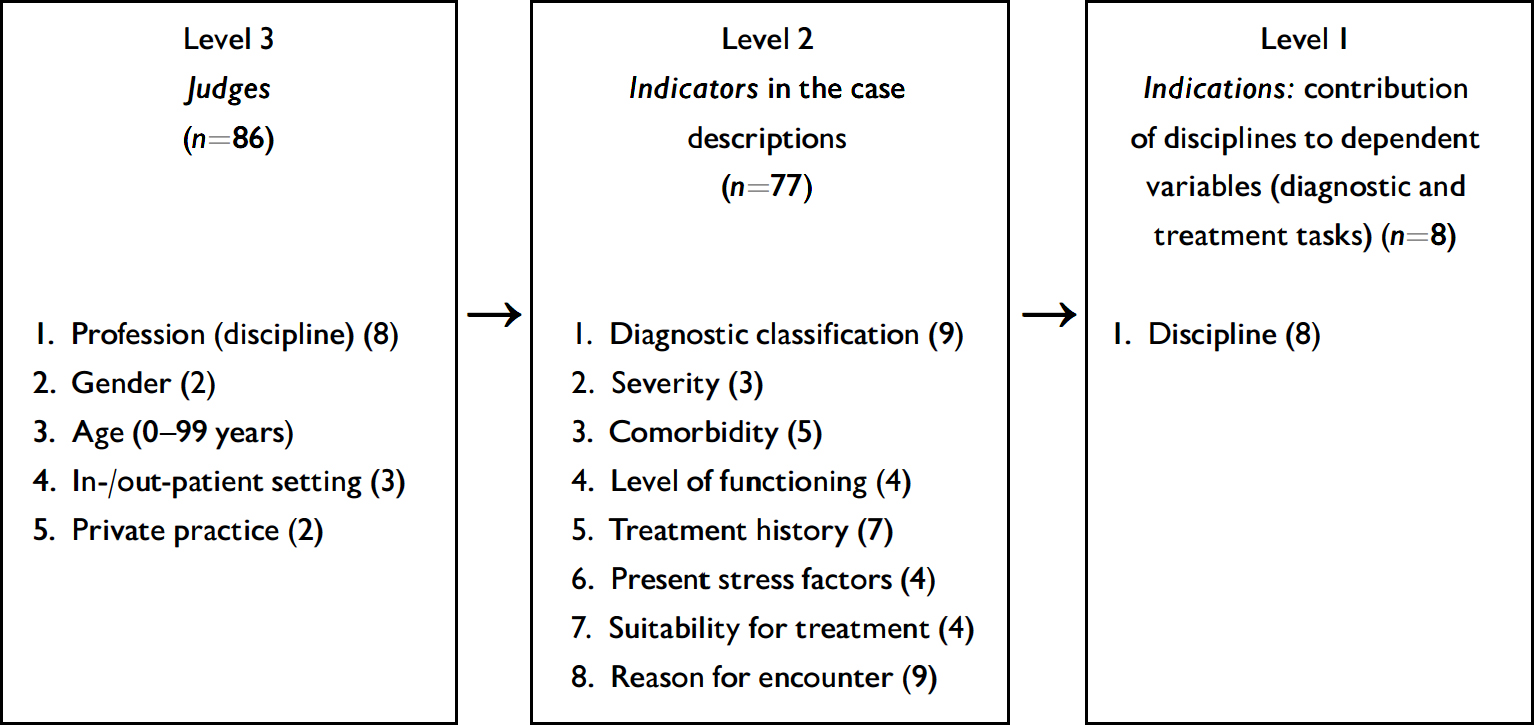
Fig. 1 Elements of the judgement procedure leading to the nested data-set construction. Number of categories in parentheses. The number of indicator combinations was reduced to 77 by orthoplan.
The indications
The indications were defined as the contribution of a specific discipline to the diagnostic and treatment tasks (cure and care). Therefore, a selection of the disciplines that were included in the judgement procedure was needed. Apart from the psychiatrist, we selected seven other formally recognised disciplines: general physicians, psychiatric nurses, psychotherapists, psychologists, social workers, group leaders (called here social pedagogic workers) and non-verbal therapists such as art and movement therapists.
The indicators
The selection of indicators (patient characteristics) for the construction of case descriptions was performed by an expert team of eight experienced clinicians, one from each of the selected disciplines. In a Delphi procedure consisting of two rounds, the experts reached agreement on eight different patient characteristics as indicators for the distribution of tasks between various disciplines. The selected indicators (with the number of categories in parentheses) were: diagnostic classification (9), severity (3), level of social/role functioning (4), comorbidity (5), treatment history (7), stress factors (4), suitability for treatment (4) and reason for seeking help (9).
A case description was constructed by the unique combination of the different categories of each indicator. Using these indicators we were able to describe the broad range of mental health patients between the ages of 18 and 65 years who are usually seen in psychiatric wards, community mental health services and private practices. Descriptions of forensic psychiatric patients and those with severe substance misuse were excluded. A typical case description is a patient with moderate depression with a comorbid personality disorder who has not received prior treatment, who has a sufficient level of social role functioning, with chronic stressors, poor suitability for treatment and striving for symptom reduction.
By permutation of all the patient characteristics it was possible to generate 544 320 different case descriptions. In order to reduce the judgement task to a manageable size we used ‘orthoplan’ (SPSS, 1998). Orthoplan produces an orthogonal array of indicator combinations. This reduced the number of combinations to 77, while guaranteeing that the indicators were equally distributed in this sample and the effect of each indicator still could be evaluated. However, one disadvantage of this procedure is that interactions between patient characteristics and other variables cannot be analysed systematically.
The recruitment of the judges
We recruited the judges from the disciplines that were selected for the indications. The members of the expert panel assessed the following selection criteria for the judges: they must be working in mental healthcare, have experience with the processes of indication/assessment and treatment planning, and be representative and authoritative members or opinion leaders of their professional group. Each member of the expert team invited at least ten members of his/her professional group to rate the model cases, taking into account variation in work setting, years of experience and gender. In total, 102 professionals were invited to participate in the panel of judges, from which 86 (84%) agreed to participate (10 or 11 respondents for each profession). Non-response was not selective for setting, experience or gender.
The judgement procedure
We asked the judges to rate each case description on the defined indications: the contribution of the eight selected disciplines to diagnosis and treatment. The judges had to rate the contribution of their own and seven other disciplines to these two tasks for the 77 case descriptions. Each task was rated on a five-point scale as follows: 1, no contribution; 2, small contribution; 3, partial contribution in collaboration with other disciplines; 4, considerable contribution; 5, complete contribution (no other disciplines required). Each judge had to give a total of 77 ratings (case descriptions) on 8 disciplines and 2 tasks, amounting to a total of 1232 judgements. The actual number of usable judgements was 104 422 (99%).
Analysis
Because the design of the study was nested, we had to perform multilevel analyses of variance. Figure 1 shows how this nested data-set was constructed from the judgement procedure. According to the way the data-set was constructed, we had three levels in the analyses: the indications that were judged (level 1), the indicators in the case descriptions (level 2) and the judges (level 3). Subsequently the fixed variables were added as follows: first the characteristics of the judges, then the various indicators, and finally, at the lowest level, the disciplines in the indications being judged. Each subsequent model started with the significant variables of the previous model. Two separate analyses were carried out for the two dependent variables, i.e. ratings on the contributions to diagnostic tasks and to treatment tasks. Because almost all variables (see Fig. 1) were variables at a nominal level, we had to construct dummy variables for the various categories.
RESULTS
Multilevel analyses
We performed multilevel analyses in order to investigate to what degree the variance of the judgements on the indications (contribution of different disciplines to diagnostic and treatment tasks) could be explained by the indicators (characteristics of the case descriptions). The results are shown in Tables 1 and 2.
Table 1 Relationship between the dependent variable ‘contribution to diagnosis’ and the judge variables, the indicators in the case descriptions, and the disciplines in the indications (standard error in parentheses)

| Model | ||||
|---|---|---|---|---|
| Intercept only | Judge model | Indicator model | Indication model | |
| Intercept | 2.59 | 1.97 | 1.99 | 3.54 |
| Fixed judge variables | ||||
| Gender | 0.24 (0.09) | 0.24 (0.09) | 0.24 (0.09) | |
| Discipline | ||||
| Psychiatrist | ||||
| General physician | 0.47 (0.15) | 0.47 (0.15) | 0.47 (0.15) | |
| Psychotherapist | −0.11 (0.15) | −0.11 (0.15) | −0.11 (0.15) | |
| Psychologist | −0.04 (0.15) | −0.04 (0.15) | −0.05 (0.15) | |
| Social worker | 0.62 (0.16) | 0.62 (0.16) | 0.62 (0.16) | |
| Psychiatric nurse | 0.27 (0.14) | 0.27 (0.14) | 0.27 (0.14) | |
| Non-verbal therapist | 0.33 (0.16) | 0.33 (0.16) | 0.33 (0.16) | |
| Pedagogic worker | 0.41 (0.16) | 0.41 (0.16) | 0.41 (0.16) | |
| Fixed indicators | ||||
| Diagnostic classification | ||||
| Borderline personality disorder | ||||
| Problems with identity | −0.05 (0.03) | −0.05 (0.02) | ||
| Interpersonal problems | −0.02 (0.03) | −0.02 (0.02) | ||
| Dissociative, somatoform or eating disorder | 0.01 (0.02) | 0.01 (0.02) | ||
| Anxiety disorder | −0.02 (0.02) | −0.02 (0.02) | ||
| Affective disorder | −0.04 (0.02) | −0.04 (0.02) | ||
| Psychosis | −0.10 (0.02) | −0.10 (0.01) | ||
| Schizophrenia | −0.08 (0.02) | −0.09 (0.02) | ||
| Organic psychosyndrome | −0.10 (0.02) | −0.10 (0.02) | ||
| Comorbidity | ||||
| No comorbidity | ||||
| Somatic problems | 0.03 (0.02) | 0.03 (0.01) | ||
| Personality disorder | 0.03 (0.02) | 0.04 (0.01) | ||
| Addiction | 0.03 (0.02) | 0.03 (0.01) | ||
| Combined somatic and psychological problems | 0.07 (0.02) | 0.07 (0.01) | ||
| Stress factors | ||||
| No stress factors | ||||
| Chronic stress factors, long-term difficulties | −0.04 (0.02) | −0.04 (0.01) | ||
| Traumatising stress factors | −0.03 (0.02) | −0.04 (0.01) | ||
| Evoking life events | −0.03 (0.02) | −0.03 (0.01) | ||
| Reason for encounter | ||||
| Out-patient care | ||||
| Symptom reduction | −0.05 (0.02) | −0.05 (0.02) | ||
| Increase understanding | −0.04 (0.02) | −0.04 (0.02) | ||
| Support | 0.03 (0.02) | 0.03 (0.02) | ||
| Exercise | −0.02 (0.02) | −0.02 (0.02) | ||
| In-patient care or day care | 0.05 (0.02) | 0.06 (0.01) | ||
| Crisis intervention | 0.00 (0.02) | 0.00 (0.01) | ||
| Resocialisation/rehabilitation | 0.04 (0.02) | 0.04 (0.01) | ||
| Long-term in-patient care | 0.09 (0.02) | 0.09 (0.02) | ||
| Self-help | −0.03 (0.04) | −0.03 (0.03) | ||
| Fixed indications | ||||
| Discipline | ||||
| Psychiatrist | ||||
| General physician | −1.62 (0.02) | |||
| Psychotherapist | −1.32 (0.02) | |||
| Psychologist | −1.03 (0.02) | |||
| Social worker | −1.88 (0.02) | |||
| Psychiatric nurse | −1.44 (0.02) | |||
| Non-verbal therapist | −2.51 (0.02) | |||
| Pedagogic worker | −2.57 (0.02) | |||
| Random | ||||
| Judge | 0.19 (0.03) | 0.13 (0.02) | 0.13 (0.02) | 0.13 (0.02) |
| Indicators | 0 | 0 | 0 | 0 |
| Indications | 1.44 (0.01) | 1.44 (0.01) | 1.44 (0.01) | 0.84 (0.00) |
| Fit | 167 592.1 | 167 558 | 167 451 | 139 193 |
Table 2 Relationship between the dependent variable ‘contribution to treatment’ and the judge variables, the indicators in the case descriptions, and the disciplines in the indications (standard error in parentheses)
| Model | ||||
|---|---|---|---|---|
| Intercept only | Judge model | Indicator model | Indication model | |
| Intercept | 2.71 | 2.0 | 1.953 | 2.68 |
| Fixed judge variables | ||||
| Gender | 0.28 (0.10) | 0.28 (0.10) | 0.28 (0.10) | |
| Discipline | ||||
| Psychiatrist | ||||
| General physician | 0.39 (0.17) | 0.39 (0.17) | 0.39 (0.17) | |
| Psychotherapist | −0.12 (0.17) | −0.12 (0.17) | −0.12 (0.17) | |
| Psychologist | −0.01 (0.17) | −0.01 (0.17) | −0.01 (0.17) | |
| Social worker | 0.73 (0.18) | 0.73 (0.18) | 0.73 (0.18) | |
| Psychiatric nurse | 0.22 (0.16) | 0.22 (0.16) | 0.22 (0.16) | |
| Non-verbal therapist | 0.24 (0.19) | 0.24 (0.19) | 0.24 (0.19) | |
| Pedagogic worker | 0.76 (0.18) | 0.76 (0.18) | 0.76 (0.18) | |
| Fixed indicators | ||||
| Diagnostic classification | ||||
| Borderline personality disorder | ||||
| Problems with identity | −0.03 (0.04) | −0.03 (0.04) | ||
| Interpersonal problems | −0.08 (0.04) | −0.08 (0.04) | ||
| Dissociative, somatoform or eating disorder | 0.08 (0.03) | 0.08 (0.03) | ||
| Anxiety disorder | 0.02 (0.03) | 0.02 (0.03) | ||
| Affective disorder | −0.01 (0.03) | −0.01 (0.03) | ||
| Psychosis | −0.10 (0.03) | −0.10 (0.03) | ||
| Schizophrenia | −0.11 (0.03) | −0.11 (0.03) | ||
| Organic psychosyndrome | −0.03 (0.03) | −0.03 (0.03 | ||
| Comorbidity | ||||
| No comorbidity | ||||
| Somatic problems | 0.02 (0.02) | 0.02 (0.02) | ||
| Personality disorder | 0.02 (0.02) | 0.02 (0.02) | ||
| Addiction | 0.03 (0.02) | 0.03 (0.02) | ||
| Combined somatic and psychological problems | 0.07 (0.02) | 0.07 (0.02) | ||
| Reason for encounter | ||||
| Out-patient care | ||||
| Sympton reduction | −0.12 (0.03) | −0.12 (0.03) | ||
| Increase understanding | −0.04 (0.03) | −0.04 (0.03) | ||
| Support | 0.03 (0.03) | 0.03 (0.03) | ||
| Exercise | −0.01 (0.03) | −0.01 (0.03) | ||
| In-patient care or day care | 0.16 (0.03) | 0.16 (0.03) | ||
| Crisis intervention | −0.01 (0.03) | −0.01 (0.03) | ||
| Resocialisation/rehabilitation | 0.12 (0.03) | 0.12 (0.03) | ||
| Long-term in-patient care | 0.19 (0.03) | 0.19 (0.03) | ||
| Self-help | −0.08 (0.05) | −0.08 (0.05) | ||
| Fixed indications | ||||
| Discipline | ||||
| Psychiatrist | ||||
| General physician | −1.05 (0.02) | |||
| Psychotherapist | −0.62 (0.02) | |||
| Psychologist | −0.38 (0.02) | |||
| Social worker | −0.87 (0.02) | |||
| Psychiatric nurse | −0.26 (0.02) | |||
| Non-verbal therapist | −1.29 (0.02) | |||
| Pedagogic worker | −1.37 (0.02) | |||
| Random | ||||
| Judge | 0.25 (0.04) | 0.16 (0.03) | 0.16 (0.03) | 0.16 (0.03) |
| Indicators | 0.19 (0.01) | 0.19 (0.01) | 0.18 (0.01) | 0.21 (0.01) |
| Indications | 1.55 (0.01) | 1.55 (0.01) | 1.55 (0.01) | 1.30 (0.01) |
| Fit | 178 382.6 | 178 345 | 178 163 | 170 076 |
In the multilevel model for the judgement of the diagnostic tasks, the significant judge characteristics (shown in Table 1) explained 3.7% of the total variance, the indicators did not explain any variance at all and the fixed variable ‘disciplines in the indications’ explained 36.8% of the total variance. In the multilevel model for the judgement of the treatment tasks, the significant judge variables explained 4.5% of the total variance, the indicators explained 0.5%, and the disciplines in the indications 12.6% of the total variance. This means that the ratings that were given on the contribution of diagnostic and treatment tasks were mainly influenced by the ideas about the disciplines under judgement, were less influenced by the characteristics pertaining to the judges and were almost independent of the characteristics given in the case descriptions.
Both models show signs of interaction effects. The diagnostic model improved slightly after adding the significant indications (χ2=107, d.f.=24), although the indications did not explain any variance. Table 2 shows in the last model (the indication model) an increase of the random variance on the level of indicators from 0.18% to 0.21%, which may be due to some interaction effects between discipline and the case characteristics.
We conclude that, contrary to our expectations, neither the ratings on the disciplinary contribution to diagnostic tasks, nor the ratings of the contribution to treatment tasks were primarily associated with the indicators in the case descriptions. In order to explain this unexpected result we returned to the raw data.
The disciplines that were judged
Figure 2 shows the mean ratings that the judges gave to the different disciplines for the contribution to diagnostic and treatment tasks. There is a clear ranking order between the various disciplines for both tasks. The psychiatrist is considered to have the highest contribution in both tasks, and the non-verbal therapists and pedagogic workers the lowest. Psychiatrists, for example, received a mean rating of 4.14 for diagnostic tasks, indicating that psychiatrists were almost always seen as being capable of performing all diagnostic tasks without the aid of other mental health professionals.
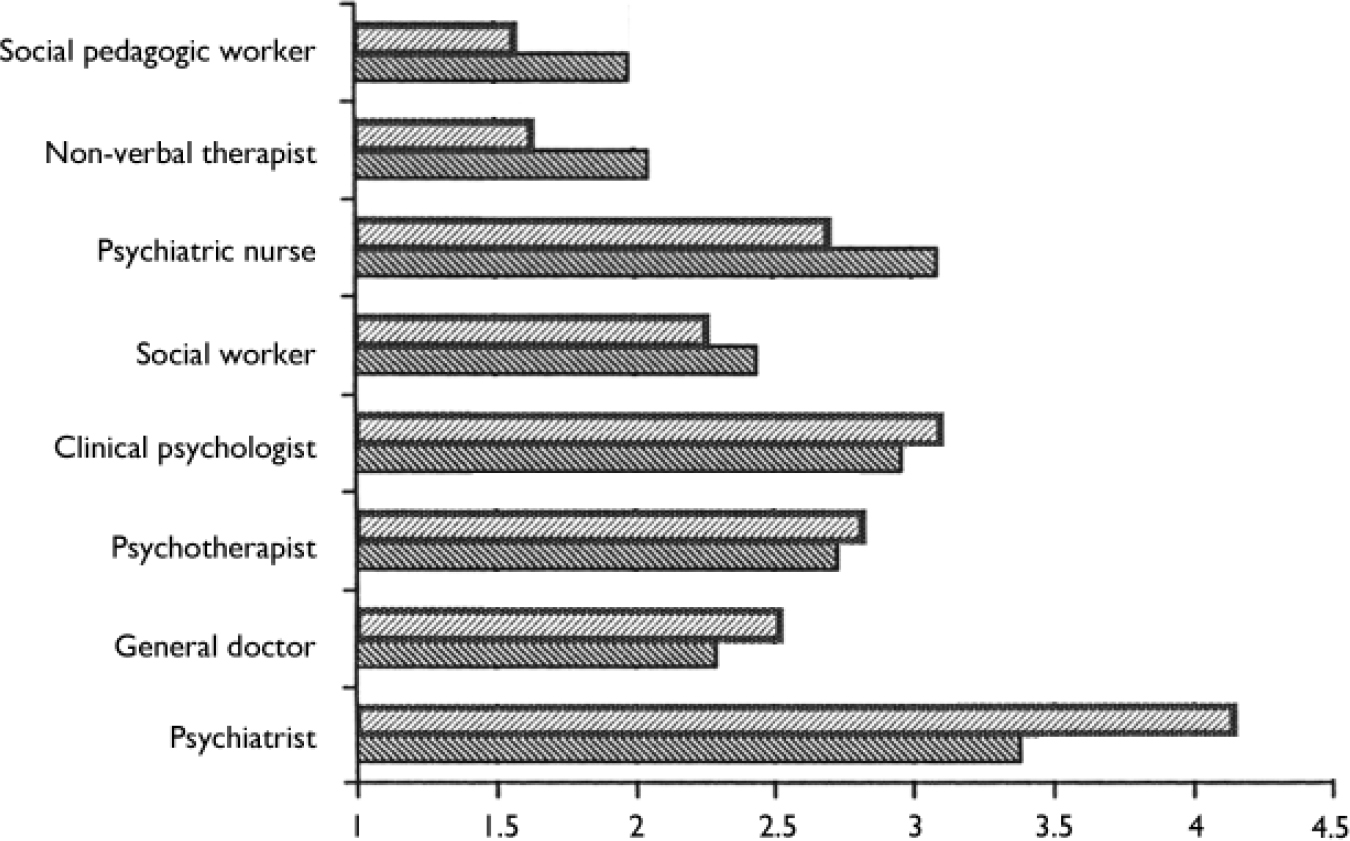
Fig. 2 Mean ratings on diagnostic and treatment tasks for the eight disciplines: 1, no contribution; 5, complete contribution; ▨ treatment; ▧ diagnosis.
The judges
Of the five fixed variables belonging to the factor ‘judge’, the sub-factor ‘discipline’ was the most significant in the explained variance. This indicates that professionals belonging to the same discipline judged identically and that professionals of different disciplines could be distinguished. Figure 3 presents the ratings that professionals gave to their own discipline compared with the ratings other professionals gave them on their contribution to treatment. Most of the professional groups claimed a broader domain of interventions than other disciplines attributed to them. One exception was the rating psychiatrists gave to themselves, which was identical to those given by other professionals.
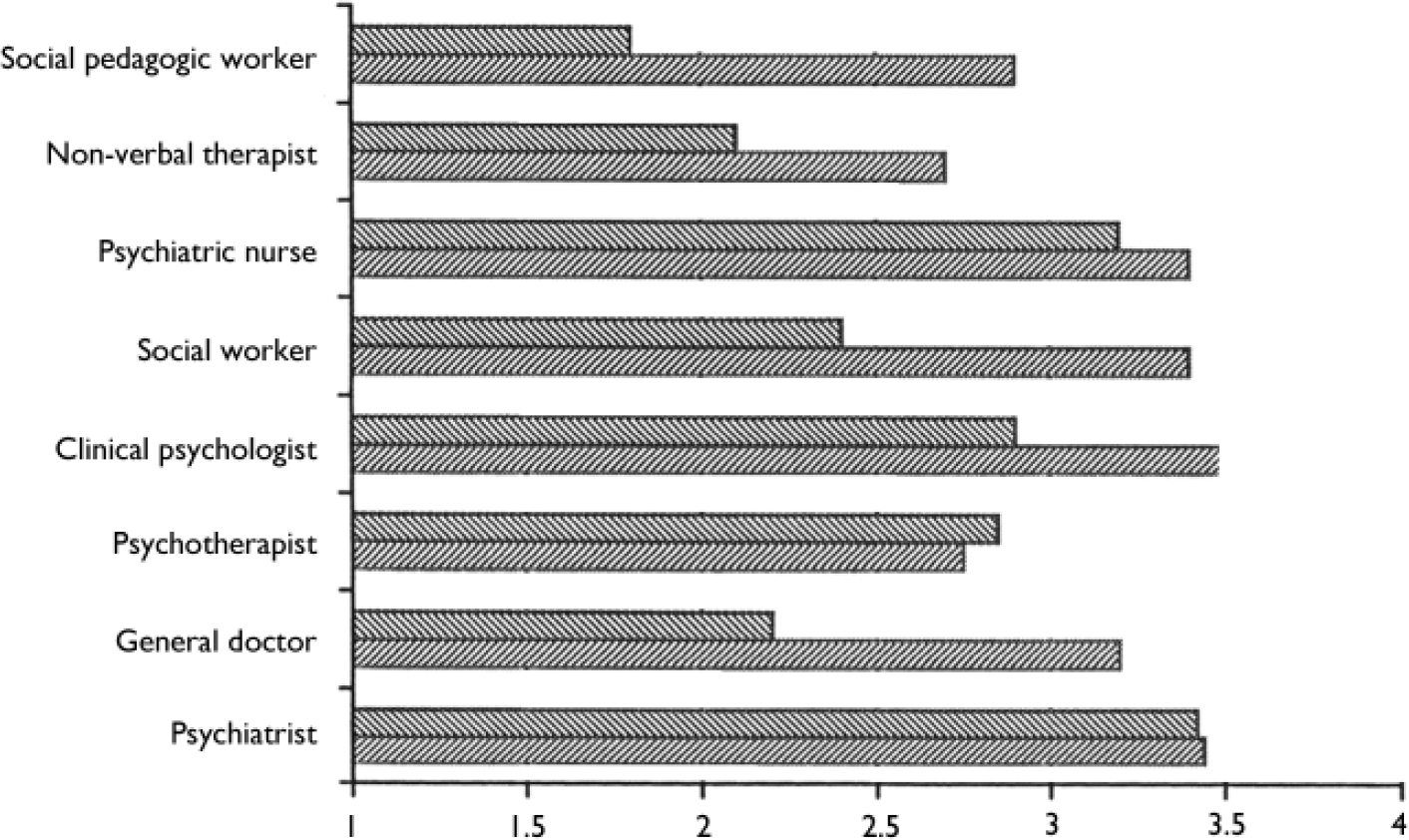
Fig. 3 Mean ratings on treatment tasks. Contribution of disciplines judged by professionals of the same discipline and of other disciplines. 1, no contribution; 5, complete contribution; ▨ own rating; ▧ discipline rated by others.
The indicators in the case descriptions
The results on the indicators were the most complex to understand. Only at the fixed-effect level did some variables gain significance: ‘diagnostic classification’, ‘comorbidity’ and ‘reasons for encounter’. The increased random effect after the addition of ‘discipline’ at level three (indications) points to interaction effects between indicators in the case descriptions and disciplines. The orthoplan sampling of the combinations of indicators made it impossible to analyse these interaction effects in detail.
An example of an interaction effect that may have occurred is shown in Fig. 4: the contribution to treatment by each discipline for three diagnostic categories, ‘schizophrenia’, ‘mood disorder’ and ‘interpersonal problems’. First, we see the main trends as shown in Fig. 2: psychiatrists were rated as having the highest contribution and social pedagogic workers the lowest to treatment tasks. Second, a smaller trend is apparent, indicating that the average contribution of disciplines changes with the severity of the problems of the patients. The contributions of the social pedagogic worker, the psychiatric nurse and the psychiatrist increase with the severity of the diagnosis. The contributions of the non-verbal therapist and the social worker are more or less the same for all three diagnostic groups. The contributions of the clinical psychologist and the psychotherapist decrease with the severity of the diagnosis. This pattern corroborates our suggestion of an interaction effect.
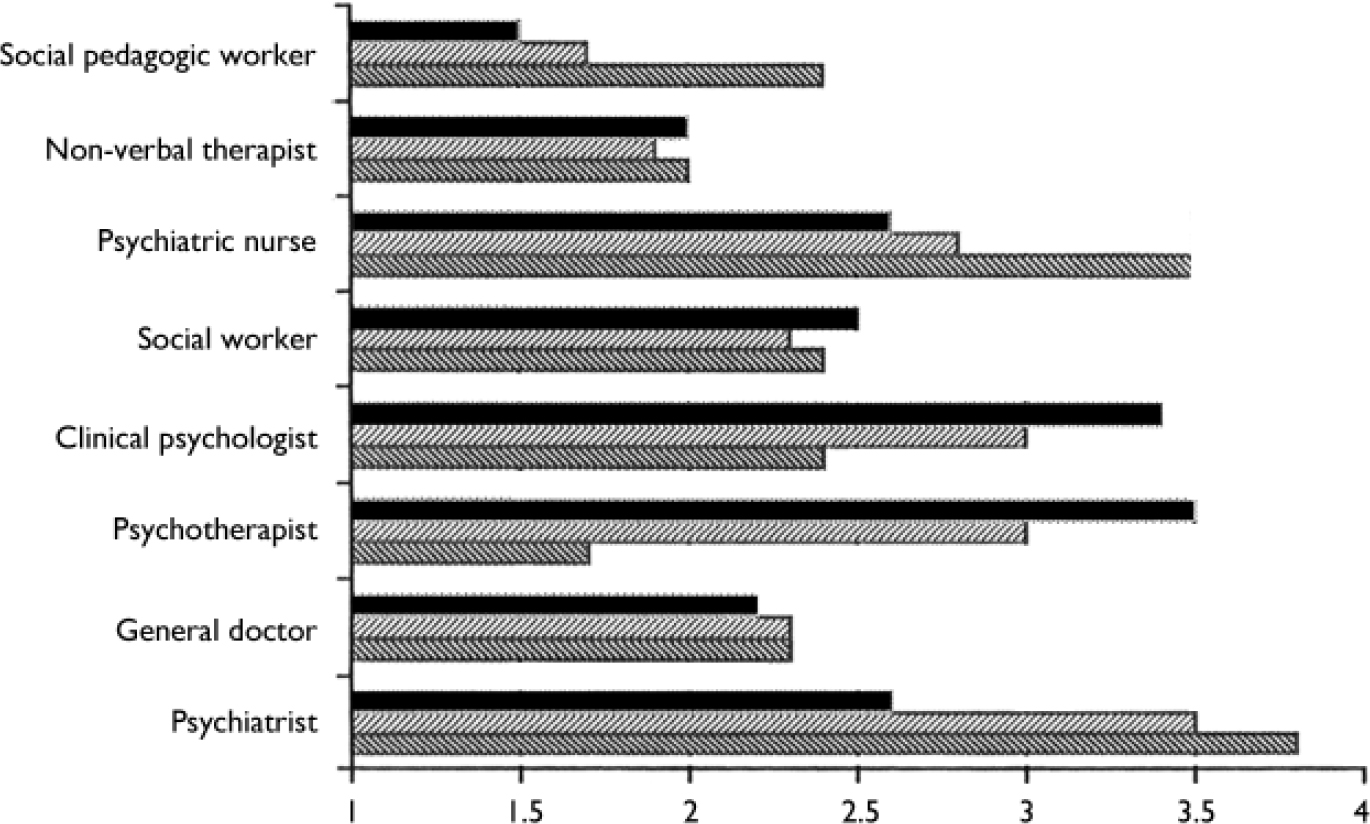
Fig. 4 Mean ratings on treatment tasks for eight disciplines for three diagnostic categories in the case descriptions. 1, no contribution; 5, complete contribution, ▨ schizophrenia; ▧ mood disorder; ▪ interpersonal problems.
DISCUSSION
The results from the current study reveal the existence of an implicit standard for the contribution of the psychiatrist and other disciplines towards diagnostic and treatment tasks in mental healthcare. The role of the psychiatrist is much less controversial than often presumed. Regardless of their disciplines, the judges were unambiguous about the tasks and responsibilities of the psychiatrist. Psychiatrists themselves do not overestimate their role, a fact corroborated by the other disciplines. However, contrary to our expectation, this standard did not show a convincing relationship with specific patient characteristics. In contrast, we found that the rated contribution depended mostly on an a priori ranking order of disciplines.
Limitations
It is possible that these unexpected results are at least partly an artefact of the study design. In the judgement procedure the operationalisation of the dependent and the independent variables was crucial. The dependent variables were limited to the contribution of professionals towards two tasks: diagnosis and treatment. More tasks might have led to more differentiation between disciplines. Also the choice of eight broad disciplines may mean that not enough room was left for the nuances of sub-specialties and also that the indicators in the case descriptions may not have been specific enough to allow clear judgements.
In addition, we do not know the extent of the influence of the way the tasks were rated. The categories of the five-point scale anticipated a double judgement on the part of the judges: they had to give an absolute judgement on the contribution of a specific discipline to diagnostic and treatment tasks as well as giving a relative judgement (the appropriate contribution given the contribution of other disciplines).
Although we cannot exclude the fact that other operationalisations would have led to other results, the large difference between the explained variance by the three main factors - judges, indicators and indications - is so overwhelming that we doubt whether this main result of the study would have changed with other study criteria. In addition, as we cannot compare our results with results from other studies, we can only consider, with some caution, the possible implications of our findings.
Agreement on the tasks to be performed by psychiatrists
The results show that the judgement of the contribution towards care by eight professional groups is quite transparent. Almost all of the random variance was on the level of the indications. Among the fixed variables ‘disciplines in the indications’ explained most of the variance. Psychiatrists hold the position of always having to carry out the most important role, whereas the contribution of pedagogic workers is seen as quite modest. Psychologists should make a substantial contribution to diagnostic tasks whereas psychiatric nurses have a substantial role in treatment tasks. The main conclusion of this study is, therefore, that the collective sense of professionals concerning the tasks of various disciplines is defined and very strong.
Lack of agreement on the shop floor remains
The agreement concerning the distribution of tasks between psychiatrists and other mental health professionals was not expected, considering the differences in task distribution between disciplines in the mental healthcare institutes (Reference Hutschemaekers and NeijmeijerHutschemaekers & Neijmeijer, 1998). Nor does the agreement fit with the competition between professional unions and related professional struggles (Reference AbbotAbbot, 1988; Reference Herrman, Trauer and WarnockHerrman et al, 2002).
It is possible that the current procedure of judgements may have decontextualised and depoliticised the judgements of tasks where the immediate risk for the position of their own discipline was not taken into consideration by the judges. It is also possible that the competition between disciplines has less to do with diagnostic and treatment tasks than with other tasks, such as team coordination or case management (Sainsbury Centre for Mental Health, 1997). Finally, our data do not indicate the ideal composition of mental healthcare teams (number and numeric proportions of disciplines) or the way such a team should function (Reference Hutschemaekers and NeijmeijerHutschemaekers & Neijmeijer, 1998). Further research is needed to explain the lack of agreement on the shop floor, and the strong agreement found in this study.
Images of professions
The most unexpected finding of this study is the lack of clear relationships between the assigned contribution of disciplines to diagnostic or treatment tasks and the different indicators in the case descriptions. It is hard to understand on what other sources professionals have relied in this judgement procedure. Perhaps these sources consist of more or less generalised images that professional groups have of each other. If this is the case, our data provide insight into the nature of these images. First, given the lack of specific relations with patient characteristics, we may assume that these images are not very specific. Second, these images do not seem strongly tied to specific clinical settings. The large differences between the distribution of disciplines in the field of work are at least not reflected in the ratings of the judges. Third, and most astonishingly, professional groups only partially differ in the images they have of each other. Their ratings show that they use one broad set of shared images. These images therefore fit what is called in social psychology a cultural value or a social presentation (Reference Moscovici, Farr and MoscoviciMoscovici, 1984).
Power or expertise?
In this study we aimed to provide more clarity on how the contributions of aligned tasks between psychiatrists and other disciplines are seen. Although we feared a lack of agreement due to professional competition, we actually found strong agreement, probably also due to a lack of specific images on the expertise of disciplines in relation to the needs of patients. How, therefore, should these results be interpreted? One possible interpretation is that the distribution of tasks has to do more with responsibility or power than with specific expertise, simply because most interventions in mental healthcare can be performed by several disciplines. This would imply that there is only a moderate link between disciplines and specific expertise. Another interpretation is that psychiatrists as well as the other professionals in mental healthcare have insufficiently learned to recognise and use the specific expertise of other mental healthcare professionals. An example of this specificity could be the distinction between generalists and specialists. In general healthcare, for example, more distinction is made between interventions in primary care and interventions in specialised healthcare.
If indeed a lack of recognising and using differences is a viable explanation for the results presented here, a conclusion of this study could be that professions in mental healthcare should focus more on differentiation. This would mean that psychiatrists, as well as other professionals, should focus more on their core competencies in relation to specific patient groups.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
▪ There is large agreement on the role and tasks of psychiatrists in mental healthcare; the presupposed competition between professional groups is less important than often assumed.
-
▪ The assigned contribution of disciplines to diagnostic and treatment tasks is only marginally related to the characteristics and the demands of the patient.
-
▪ Mental health professionals, including psychiatrists, seem to have rather vague notions about the specific expertise of the most important disciplines in mental healthcare.
LIMITATIONS
-
▪ A vignette to study only partly reflects real practice.
-
▪ Operationalisation of the judgement procedure (the patient characteristics, the tasks and disciplines to be rated) may have influenced the results.
-
▪ Statistical selection of the patient characteristics for the case descriptions did not allow the analysis of interactions.









eLetters
No eLetters have been published for this article.