Improved relapse prevention has been identified as a priority for treatment research Reference Hollon, Munoz, Barlow, Beardslee, Bell and Bernal1 in depression, because a significant proportion of people with depression experience a chronic or recurrent life course. Reference Judd2,Reference Scott3 Prospective longitudinal studies identify partial recovery following acute treatment as an important risk factor for full-episode relapse. Reference Judd2,Reference Fava4-Reference Paykel, Ramana, Cooper, Hayhurst, Kerr and Barocka6 Moreover, residual subsyndromal symptoms are common, with a third of individuals not responding fully to acute treatment. Chronicity is also associated with substantial distress, high rates of comorbidity, marked functional impairments, and increased healthcare utilisation. Reference Hollon, Munoz, Barlow, Beardslee, Bell and Bernal1,Reference Scott3,Reference Paykel, Ramana, Cooper, Hayhurst, Kerr and Barocka6,Reference Cornwall and Scott7 Although randomised controlled trials (RCTs) of cognitive-behavioural therapy (CBT) for chronic depression demonstrate that it is effective at reducing subsequent depressive relapses over 4-6 years, Reference Fava, Grandi, Zielezny, Canestrari and Morphy8-Reference Kocsis, Gelenberg, Rothbaum, Klein, Trivedi and Manber12 standard models of CBT seem to be less efficacious in achieving early remission in chronic depression, Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10,Reference Kocsis, Gelenberg, Rothbaum, Klein, Trivedi and Manber12 and comorbid anxiety and other impairments remain problematic. One potential way to improve the efficacy of CBT for residual or chronic depression is to adapt it to specifically address core residual symptoms such as depressive rumination, Reference Watkins, Scott, Wingrove, Rimes, Bathurst and Steiner13,Reference Watkins14 defined as repetitive thinking about the causes, meanings and implications of depressed feelings, symptoms, problems and upsetting events. Reference Nolen-Hoeksema15,Reference Watkins16 This study reports the first phase II RCT of rumination-focused CBT, building on an encouraging multiple baseline case series. Reference Watkins, Scott, Wingrove, Rimes, Bathurst and Steiner13 We modified CBT to target rumination because rumination: (a) remains elevated after remission from depression; Reference Nolen-Hoeksema15,Reference Riso, du Toit, Blandino, Penna, Dacey and Duin17,Reference Roberts, Gilboa and Gotlib18 (b) is associated with less treatment response; Reference Ciesla and Roberts19,Reference Schmaling, Dimidjian, Katon and Sullivan20 and (c) prospectively predicts the onset, severity and duration of depression. Reference Watkins16 The primary aim of our study was to test the hypothesis that rumination-focused CBT provides added benefit to treatment as usual (TAU) in reducing residual symptoms of depression. This is a stringent test as previous RCTs Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10,Reference Kocsis, Gelenberg, Rothbaum, Klein, Trivedi and Manber12 failed to find any acute benefit of adding CBT to pharmacotherapy in treating residual depression. The secondary aim was to test the hypothesis that rumination-focused CBT reduces rumination significantly more than TAU, i.e. acts on its intended target. The third aim was to test whether change in rumination mediates any treatment effect of rumination-focused CBT.
Method
The study was approved by the UK National Health Service South London and Maudsley Research Ethics Committee and was conducted in community mental health teams and psychological treatment services in South East London and Devon, UK. Consecutive referrals to out-patient services for depression and on the waiting list for psychological therapies were approached and those who met inclusion criteria and gave written informed consent to participate were randomly allocated to TAU alone or to TAU plus rumination-focused CBT. Randomisation was performed by an off-site researcher using computer-generated random numbers, and stratified according to gender and the duration of the index episode of major depression (< v.≥1 year). All participants were assessed by research staff masked to treatment allocation at intake baseline assessment (Time 1 (T 1)) and again 6 months later (post-intervention, Time 2 (T 2)). The trial has been registered (ISRCTN22782150).
Inclusion criteria were: aged >18, meeting criteria for medication-refractory residual depression as defined previously: Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 (a) meeting DSM-IV criteria 21 for major depression within the past 18 months but not in the past 2 months; (b) residual symptoms reaching at least 8 on the 17-item Hamilton Depression Rating Scale for Depression (HRSD) Reference Hamilton22 and 9 on the Beck Depression Inventory (BDI-II); Reference Beck, Steer and Brown23 (c) taking antidepressant medication at a therapeutic dose as recommended by the British National Formulary 24 and/or equivalent to 125 mg of amitriptyline for at least 8 weeks continuously during the current episode and within the past 2 months. Exclusion criteria were: a history of bipolar disorder, psychosis, current drug or alcohol dependence, intellectual disability, organic brain damage and concurrent psychotherapy at point of entry to the study. There were no exclusion criteria with respect to comorbid anxiety disorders or Axis II diagnoses.
Outcome measures
Severity of residual depressive symptoms was the primary outcome measure. Treatment response was defined as ≥50% decrease in baseline HRSD. Secondary outcome measures were change between T 1 and T 2 in self-reported rumination, number of comorbid psychiatric diagnoses and number of individuals meeting criteria for remission (defined as HRSD <8 and BDI <9 at termination) and relapse (defined as a participant meeting DSM-IV criteria for a new episode of major depression at any point between T 1 and T 2).
Primary outcome measures
Hamilton Depression Rating Scale for Depression. The HRSD Reference Hamilton22,Reference Williams25 is a standardised clinical interview developed to assess severity of depression that combines scoring individual's answers with direct observation of the person (range 0-52). A clinical psychologist experienced in the use of the HRSD trained the research assistants. Masked rating of randomly selected recorded interviews indicated excellent interrater reliability between the study interviewer(s) and masked rater, all kappa coefficient (κ)>0.8.
Beck Depression Inventory. The BDI-II Reference Beck, Steer and Brown23 is a 21-item self-report instrument developed to measure severity of depression in adults and adolescents. Higher scores represent greater depression severity (range 0-63), and minimal, mild, moderate and severe symptom severity ranges have been specified.
Secondary outcome measures
The Structured Clinical Interview for DSM-IV. The Structured Clinical Interview for DSM-IV (SCID) Reference Spitzer, Williams, Gibbon and First26 was used to ensure that participants met the study criteria and to examine whether diagnostic status changed across the course of therapy. Current and past history of Axis I and Axis II diagnoses were assessed by an experienced clinician or a trained research worker at T 1 and T 2. All comorbid diagnoses identified at intake were reassessed at study end using the relevant SCID modules. An experienced clinical psychologist with formal training in the use of the SCID trained the two research staff. To examine interrater reliability for diagnosis of depression, a random selection of audio recordings of diagnostic interviews were coded by a masked rater: the kappa coefficient for agreement between the study interviewer and masked rater was 0.9, suggesting excellent agreement.
Ruminative Response Scale of the Response Styles Questionnaire. The Ruminative Response Scale of the Response Styles Questionnaire (RRS) Reference Nolen-Hoeksema and Morrow27 consists of 22 items that assess ruminative responses to sad and depressed mood. Participants rate the frequency that they use unhelpful ruminative strategies, and higher scores suggest higher levels of rumination (range 22-88).
Interventions
Rumination-focused CBT
Rumination-focused CBT is a manualised CBT treatment, consisting of up to 12 individual sessions scheduled weekly or fortnightly. The therapy is theoretically informed by experimental research indicating that there are distinct constructive and unconstructive forms of rumination. Reference Watkins16 It is designed to coach individuals to shift from unconstructive rumination to constructive rumination, through the use of functional analysis, experiential/imagery exercises and behavioural experiments. These adaptations mean that rumination-focused CBT differs from standard CBT for depression, which focuses on modifying the content of individual thoughts, by having a greater emphasis on directly modifying the process of thinking. For example, rumination-focused CBT incorporates the functional-analytic and contextual principles and techniques of behavioural activation, Reference Jacobson, Martell and Dimidjian28 but explicitly and exclusively focused on rumination (for further details see Watkins et al Reference Watkins, Scott, Wingrove, Rimes, Bathurst and Steiner13 and Watkins Reference Watkins14 ). Within behavioural activation and rumination-focused CBT, rumination is conceptualised as a form of avoidance, and functional analysis is used to facilitate more helpful approach behaviours. Rumination-focused CBT also uses functional analysis to help individuals realise that their rumination about negative self-experience can be helpful or unhelpful and to coach them in how to shift to a more helpful style of thinking. In addition, patients use directed imagery to recreate previous mental states when a more helpful thinking style was active, such as memories of being completely absorbed in an activity (for example ‘flow’ or ‘peak’ experiences), which act directly counter to rumination.
Treatment was provided by four doctoral level clinical psychologists, one psychiatrist and one British Association for Behavioural and Cognitive Psychotherapies accredited CBT therapist, who had all received at least 12 months prior supervision in CBT, one of whom was the developer of rumination-focused CBT (E.R.W.), and four of whom had been therapists during the previous case series. Each therapist received rumination-focused CBT supervision every 2 weeks from E.R.W. with detailed feedback to maintain adherence and competence. Sessions were audiotaped to facilitate therapist supervision and to check on therapist adherence and competence. As no validated competency assessment tool is available for rumination-focused CBT, the supervisor used a brief checklist of treatment fidelity against the treatment protocol (scored 1 if rumination-focused CBT was the dominant therapeutic approach; 0 if other therapy modes predominant). All sessions reviewed by E.R.W. were scored 1.
Treatment as usual
For all participants in the trial, TAU consisted of ongoing maintenance antidepressant medication and out-patient clinical management. Because participants in the trial were already on the waiting list (typically for 3-6 months) for psychological treatment, it was expected that some would commence therapy between T 1 and T 2. However, as no participant in the TAU group would receive rumination-focused CBT, we did not exclude any of those who commenced therapy from any analyses.
Statistical analysis
The trial is reported in accord with the updated CONSORT guidelines for parallel group RCTs. Reference Schulz, Altman and Moher29 Level of residual depressive symptoms (primary outcome) was compared between treatment condition using a mixed models between-group analysis of covariance (ANCOVA) with treatment condition (TAU v. TAU + rumination-focused CBT) as the independent variable; baseline depressive symptoms as the covariate; and post-treatment depressive symptoms as the dependent variable. The analysis was performed according to the principle of intention-to-treat (i.e. all participants according to and included in random allocation). We calculated the sample size required based on the outcomes from the previous case series for rumination-focused CBT for residual depression Reference Watkins, Scott, Wingrove, Rimes, Bathurst and Steiner13 (mean pre- to post-intervention change in HRSD 9), and for the TAU condition from the existing RCT of CBT for residual depression Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 (mean change in HRSD 2.8), giving an estimate of between-group effect size (Cohen's d.) of 1. With alpha set at 0.05 to obtain 85% power, a sample size of 15 was required in each group. Assuming drop out of 20%, this requires a total sample for randomisation of 40. The data analysis approach was decided a priori using ANCOVA to counter potential baseline variance that may influence results.
As no differences in baseline covariates between conditions were noted, analyses were performed with adjustment for baseline depressive symptoms only. For the small subset of participants with missing data (n = 2 for symptoms, n = 3 for rumination), we used last observation carried forward (LOCF) to impute missing data. Sensitivity analyses compared the LOCF analysis with a participant-completer analysis (no imputation) to explore the impact of imputation of data losses on primary outcome analyses: the analyses were unaffected by data imputation (i.e. similar findings for participant-completer and LOCF analyses). All analyses were undertaken using SPSS version 16 for Windows.
Results
Patient flow
Figure 1 shows the participant flow from screening to follow-up. The main reasons for potentially eligible individuals not participating were that they did not meet the study criteria (17, 27%) or they declined to participate (4, 6.3%). The main reasons for not meeting study criteria were: currently meeting criteria for an episode of major depression (9, 53%); not taking a recommended therapeutic dose of antidepressant medication for at least 8 weeks (3, 17.6%); not having an episode of major depression in the past 18 months (3, 17.6%); and having a diagnosis of bipolar disorder (2, 13%). The sample can be characterised as a group of people with residual depression, treated pharmacologically in primary care, who were referred to specialist secondary care services for psychological treatment.
Forty-two people (11 London; 31 Devon) who agreed to participate and met the inclusion criteria were randomised to either TAU (n = 21) or to TAU + rumination-focused CBT (n = 21). At intake the type of antidepressant medication used was as follows: selective serotonin or serotonin-noradrenaline reuptake inhibitors (n = 38, 90%), tricyclic antidepressants (n = 2, 5%), monoamine oxidase inhibitors (n = 2, 5%); prescribed medications were not significantly different across the two groups. Seven participants in the TAU group (33%) commenced psychological treatment between T 1 and T 2 and two individuals were lost to follow-up. In the rumination-focused CBT arm, one participant failed to attend any rumination-focused CBT (the individual started a course of CBT from their local service between recruitment and initial contact from the trial therapist), but otherwise rates of adherence to rumination-focused CBT were high, with no one dropping out and participants on average attending 11 out of the 12 sessions offered.
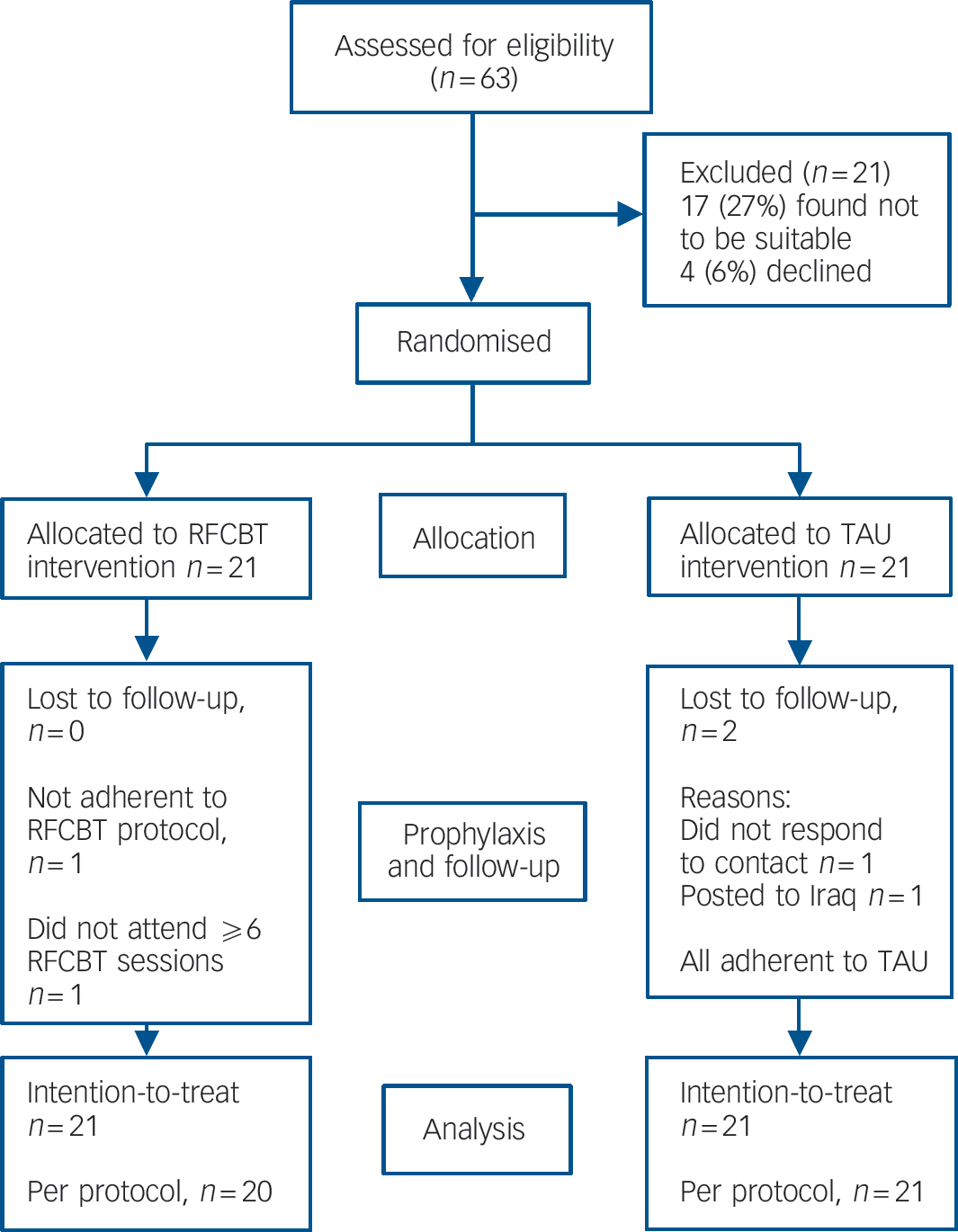
Fig. 1 CONSORT flow diagram.
RFCBT, rumination-focused cognitive-behavioural therapy; TAU, treatment as usual.
Participant characteristics
Table 1 shows participant characteristics of the intention-to-treat sample for both the rumination-focused CBT and TAU groups. The mean rumination score at baseline is consistent with that found in chronic depression. Reference Riso, du Toit, Blandino, Penna, Dacey and Duin17 The clinical characteristics indicate that the sample has a high level of comorbid mental disorders and a history of recurrent depression.
Primary outcomes
As shown in Table 2, the rumination-focused CBT group reported significantly fewer residual depressive symptoms post-intervention compared with the TAU group, after covarying initial level of baseline symptoms, for both BDI-II (F = 11.34, d.f. = 1,39, P = 0.002, η p 2 = 0.225) and HRSD (F = 7.68,, d.f. = 1,39, P = 0.009, η p 2 = 0.165).
Secondary outcomes
As predicted, depressive rumination post-intervention, covarying for baseline levels, was significantly lower in the rumination-focused CBT group than the TAU group (F = 6.87, d.f. = 1,38, P = 0.013, η p 2 = 0.15). There was a significant effect of treatment condition on rates of treatment response (TAU 26% v. rumination-focused CBT 81%; χ2 = 9.92, P<0.001); rates of remission (TAU 21% v. rumination-focused CBT 62%; χ2 = 5.24, P<0.05) and rates of relapse between baseline and post-intervention assessments (TAU 53% v. rumination-focused CBT 9.5%; χ2 = 6.89, P<0.01).
The number of comorbid Axis II diagnoses at study end, covarying for initial rates, was significantly less in the rumination-focused CBT group than the TAU group (TAU: mean
Table 1 Demographic and psychiatric characteristics of rumination-focused cognitive–behavioural therapy (CBT) and treatment as usual intention-to-treat sample
| Treatment as usual group (n = 21) | Rumination-focused CBT group (n = 21) | |
|---|---|---|
| Demographic characteristics | ||
| Female, n (%) | 10 (48) | 14 (67) |
| White, n (%) | 20 (95) | 20 (95) |
| Age, years: mean (s.d.) | 45.24 (9.35) | 43.05 (11.09) |
| Marital status, n (%)a | ||
| Single | 3 (14) | 3 (16) |
| Married or cohabiting | 16 (76) | 13 (68) |
| Separated, divorced, widowed | 2 (10) | 3 (16) |
| Level of education, n (%)b | ||
| No educational qualifications | 1 (5) | 1 (5) |
| Some school qualifications | 7 (33) | 4 (20) |
| High school/vocational qualification | 9 (43) | 8 (40) |
| University degree/professional qualification | 4 (19) | 7 (35) |
| Job status, n (%)b | ||
| Unemployed | 3 (14) | 2 (10) |
| Full-time work | 11 (52) | 8 (40) |
| Part-time work | 2 (10) | 5 (25) |
| Household | 2 (10) | 4 (20) |
| Retired | 3 (14) | 1 (5) |
| Psychiatric characteristics | ||
| Hamilton Rating Scale for Depression score, mean (s.d.) | 12.19 (2.80) | 13.29 (3.32) |
| Beck Depression Inventory-II score, mean (s.d.) | 28.29 (7.63) | 30.76 (8.17) |
| Rumination Scale of Response Style Questionnaire score, mean (s.d.) | 57.88 (8.52) | 56.40 (11.92) |
| Previous episodes of major depression, mean (s.d.) | 4.84 (3.02) | 5.43 (2.93) |
| Length of current episode, months: mean (s.d.) | 7.57 (6.13) | 9.14 (6.30) |
| Number of comorbid Axis I diagnoses | 1.86 (1.24) | 2.05 (0.92) |
| Number of comorbid Axis II diagnoses | 0.89 (1.33) | 0.81 (0.98) |
a Two participants in the rumination-focused CBT group declined to report marital status.
b One participant in the rumination-focused CBT group declined to report educational and job status.
Table 2 Mean (s.d.) scores on outcome measures at baseline assessment and post-intervention assessment for rumination-focused cognitive–behavioural therapy (RFCBT) group and treatment as usual (TAU) group
| Baseline | Post-treatment | Mean difference in change scoresa (95% CI) | Effect sizeb | |||
|---|---|---|---|---|---|---|
| Measure | TAU | RFCBT | TAU | RFCBT | ||
| Hamilton Rating Scale for Depression | 12.19 (2.80) | 13.29 (3.32) | 9.05 (5.25) | 5.48 (5.15) | 4.67 (0.28–9.05) | 0.94 |
| Beck Depression Inventory-11 | 28.29 (7.63) | 30.76 (8.17) | 20.71 (10.84) | 12.71 (11.37) | 7.57 (1.86–19.08) | 1.11 |
| Rumination Scale of Response Style Questionnaire | 59.17 (8.55) | 58.45 (12.34) | 54.38 (11.02) | 44.50 (12.86) | 9.16 (–3.4–21.73) | 0.65 |
a Mean difference in change scores: change on outcome measure from baseline to post-treatment for rumination-focused cognitive–behavioural therapy minus change in outcome measures from baseline to post-treatment for treatment as usual.
b Between-group effect size for change in symptoms (Cohen's d where d = M1–M2/σpooled, σpooled = √[(σ1 2 + σ2 2)/2]. (M1 is the mean change on outcome measure from baseline to post-treatment for rumination-focused cognitive–behavioural therapy; M2 is the mean change in outcome measures from baseline to post-treatment for treatment as usual). Large effect sizes were defined as ≥0.80.
0.67 (s.d. = 0.97); rumination-focused CBT: mean 0.24 (s.d. = 0.44); F = 5.93; d.f. = 1,39, P = 0.02, η p 2 = 0.132). There was also a similar but non-significant trend for fewer comorbid Axis I disorders in the rumination-focused CBT group than the TAU group at follow-up (TAU: mean 1.05 (s.d. = 0.97); rumination-focused CBT: mean 0.62 (s.d. = 0.86), P = 0.068).
Mediational analysis
The rationale for rumination-focused CBT predicts that reduced rumination mediates the effects of treatment condition on the primary outcome. We undertook separate regression equations to test Baron & Kenny's criteria for mediation. Reference Baron and Kenny30 We found that: change in rumination was significantly associated with change in depressive symptoms (BDI: adjusted R 2 = 0.46, β = 0.69, t = 5.73, P<0.001; HRSD: adjusted R 2 = 0.41, β = 0.66, t = 5.29, P<0.001), and remained so even when treatment condition was entered into the regression equation (BDI: adjusted R 2 = 0.61, β = 0.66, t = 5.25, P<0.001; HRSD: adjusted R 2 = 0.48, β = 0.67, t = 4.75, P<0.001). When change in rumination was entered into the regression equation, treatment condition was no longer a significant predictor of change in depressive symptoms (BDI: β = –0.06, t = –0.46, P = 0.65; HRSD: β = –0.37, t = –0.24, P = 0.81). Sobel tests were then used to statistically investigate the effect of rumination on the relationship between treatment condition and change in symptoms, which indicated that rumination was a significant mediator of the effect of treatment condition on depressive symptoms (HRSD: z = 2.20, P = 0.03; BDI: z = 2.53, P = 0.01).
Discussion
The aim of this study was to provide the first pilot RCT to explore whether rumination-focused CBT may be a potentially efficacious treatment for residual depression. As predicted, participants in the rumination-focused CBT group improved significantly more than those in the TAU group. Although combined pharmacotherapy and psychological treatments are widely recommended for depression, additional gains from combined treatment have been modest in residual depression. Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10,Reference Kocsis, Gelenberg, Rothbaum, Klein, Trivedi and Manber12 Our findings are therefore encouraging as they suggest that focusing on one aspect of residual depression - rumination - in addition to ongoing antidepressant medication, may yield improvement in depressive symptoms in a medication-refractory group.
Treatment effects on acute residual depressive symptoms
The outcomes on depressive symptoms found for 12 sessions of rumination-focused CBT (remission rates of 62%; between-treatment effect sizes of 0.94-1.1) compare favourably with 20 sessions of CBT Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 (remission rates of 25%; between-treatment effect size of 0.3) in identically defined samples of participants with residual depression. Moreover, we found that the addition of a psychological intervention beneficially augmented pharmaco-therapy, unlike the recent trial conducted by Kocsis et al. Reference Kocsis, Gelenberg, Rothbaum, Klein, Trivedi and Manber12 Although we have to be cautious when comparing between differently powered studies, the outcomes for our TAU condition closely match the outcomes for the TAU arm in the Paykel et al Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 trial. In the absence of a definitive RCT of rumination-focused CBT with a larger sample and a longer follow-up, we tentatively suggest that these results raise the possibility that the modifications made to CBT in rumination-focused CBT may engender better treatment outcomes in residual depression. This interpretation is consistent with recent evidence that behavioural activation, an important element of rumination-focused CBT, had better outcomes for treatment of severe depression than CBT in a recent large scale RCT. Reference Dimidjian, Hollon, Dobson, Schmaling, Kohlenberg and Addis31 However, a direct comparison of rumination-focused CBT v. standard CBT in a large scale trial, using a similar design to that comparing behavioural activation v. CBT Reference Dimidjian, Hollon, Dobson, Schmaling, Kohlenberg and Addis31 is necessary to test the possibility that rumination-focused CBT leads to better outcomes than CBT.
Treatment effects on relapse prevention
Since residual symptoms tend to predict relapse Reference Judd, Paulus, Zeller, Fava, Rafanelli and Grandi5,Reference Paykel, Ramana, Cooper, Hayhurst, Kerr and Barocka6,Reference Cornwall and Scott7 and interventions that target residual symptoms tend to produce better outcomes over long-term follow-ups, Reference Fava, Rafanelli, Grandi, Canestrari and Morphy9,Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 the finding that adding rumination-focused CBT to TAU reduces residual symptoms also suggests that rumination-focused CBT may reduce future relapse. Consistent with this, over the time scale of the study, there was significantly less relapse into episodes of major depression in the rumination-focused CBT condition than the TAU condition, suggesting that participation in rumination-focused CBT was protective against relapse.
Treatment effects on comorbidity
Rumination-focused CBT was also effective in reducing a range of Axis I and II comorbidity (for example generalised anxiety disorder reduced from 11 participants meeting criteria at baseline to 1 post-intervention). This reduction across comorbid disorders is consistent with the hypothesis that rumination is a transdiagnostic process, which plays a causal role in the development of psychopathology across a range of disorders. Reference Ehring and Watkins32,Reference Harvey, Watkins, Mansell and Shafran33
Mechanisms of the treatment effect
Consistent with the proposed target of the treatment, rumination-focused CBT was found to significantly reduce rumination from levels found in people with current depression down to more normative levels. Moreover, using Baron & Kenny's Reference Baron and Kenny30 criteria for mediation, change in rumination was found to be a mediator of the effects of treatment condition on reduction in depressive symptoms. This finding is consistent with the proposed mechanism of action of rumination-focused CBT. However, more recent criteria Reference Kraemer, Wilson, Fairburn and Agras34 propose that one also needs to demonstrate that there is change in the mediator before there is change in the outcome variable. Without this, one cannot rule out the possibility of backward causality in which change in the mediator (rumination) is a consequence of treatment outcome (reduced depression) rather than a contributor to that outcome. The current study assessed depression and rumination concurrently, so we cannot rule out the possibility that change in depressive symptoms led to change in rumination. Moreover, we note a further caveat in that the Baron & Kenny approach has been criticised for its failure to account for issues of confounding, with better methods proposed recently. Reference Emsley, Dunn and White35 Nonetheless, the current finding is a necessary step in determining whether change in rumination mediates the effect of rumination-focused CBT - a failure to satisfy Baron & Kenny's Reference Baron and Kenny30 criteria would clearly have argued against this.
This study does not address the active elements whereby the addition of rumination-focused CBT to TAU further reduces residual symptoms. The logic underpinning the therapy is that rumination-focused CBT works by engendering the ability to recognise pathological rumination and coaching an ability to adopt more functional styles of processing as an alternative to unhelpful rumination. However, the active ingredients could include any or none of the elements shared with CBT (for example Socratic questioning), any or none of the elements shared with behavioural activation (for example functional analysis), any or none of the elements unique to rumination-focused CBT (for example using functional analysis and/or experiential/imagery exercises to induce new styles of thinking), and any or none of the non-specific effects of providing a structured treatment, giving a plausible treatment rationale, providing hope, normalising symptoms and increased one-to-one attention from a supportive therapist. The current RCT was designed to mitigate threats to internal validity when evaluating whether rumination-focused CBT has a direct influence on depressive symptoms and was successful in this intention. However, it was not designed to investigate construct validity (i.e. to determine what aspect of rumination-focused CBT contributes to treatment outcome). Nonetheless, the failure of CBT to provide additive benefit to TAU in reducing acute residual symptoms in a sample meeting the same inclusion and exclusion criteria Reference Paykel, Scott, Teasdale, Johnson, Garland and Moore10 raises the possibility that elements found in rumination-focused CBT but not in CBT may underpin the improved treatment outcomes (for example functional analysis; targeting processing style). Process-outcome research explicitly focused on examining mechanisms of change (for example a dismantling study examining the behavioural activation components of rumination-focused CBT v. cognitive/experiential elements of rumination-focused CBT v. non-specific attention control) is needed to resolve the question of which elements actively underpin outcome. Reference Watkins14
Limitations of the study
This study has several limitations in addition to the inability to determine the temporal relationship between rumination and depression, and the absence of attention control conditions to examine construct validity, as noted above. First, this trial used a small sample as the first RCT of rumination-focused CBT, limiting our power to detect differences between groups and the generalisability of our results, although the treatment effect size is large enough to suggest that this is a reliable effect even with the small sample. Second, ideally, trial participants would have been followed for up to 2 years post-intervention to examine whether rumination-focused CBT reduced rates of relapse relative to TAU in the long term. However, resource constraints meant that this was not feasible and attrition of the control group (who were awaiting therapy) began within the first 6 months of the trial, making it unlikely we would have a therapy-free control group at longer follow-up. Third, we did not prevent participants in the TAU condition from receiving psychotherapy, and, thus, this group was somewhat heterogeneous, although, if anything, participants in the TAU arm receiving psychotherapy provides a more robust test of whether rumination-focused CBT adds treatment benefit to TAU. Fourth, therapist effects (for example different levels of experience between E.R.W. and other therapists) may have moderated treatment outcomes, but the study was underpowered to examine this.
Rumination-focused CBT and residual depression
In conclusion, this pilot phase II RCT tentatively indicates that rumination-focused CBT offers added benefit to the treatment of medication-refractory residual depression - the most common presentation of depression in secondary care Reference Scott3 - both in reducing acute symptoms and in preventing onset of another episode of major depression. The findings raise the possibility that a treatment targeting rumination utilising behavioural activation principles may have better efficacy than standard CBT for depression in this population. Moreover, these results indicate that it is possible to directly reduce depressive rumination, and that this reduction mediates the effects of rumination-focused CBT on concurrent change in depressive symptoms. Nonetheless, as the first exploratory trial, there is a need for further RCTs to replicate these findings in other settings based on the extant effect sizes observed in this study and to examine cost-effectiveness in a fully powered phase III trial.
Funding
This trial was funded by a Young Investigators Grant to E.R.W. from the National Alliance for Research into Schizophrenia and Depression (NARSAD), with J.S. as mentor.
Acknowledgements
We are grateful to the people who participated in the trial and to the physicians and other healthcare staff who enabled the trial, especially the research workers (Sandra Kennell-Webb, Yanni Malliaris) and therapists on the trial.






eLetters
No eLetters have been published for this article.