The course of unipolar affective disorder is now recognised to show not only clear-cut episodes of major disorder, but also considerable periods of inter-episode lower-level symptoms (Reference Paykel, Ramana and CooperPaykel et al, 1995; Reference Judd, Akiskal and MaserJudd et al, 1998), with continuity between major and minor symptoms and subtypes. In bipolar disorder, whereas milder forms such as bipolar II disorder and cyclothymic disorder are well recognised, there has been less study of subthreshold symptoms between major episodes. Two of us (Reference Kennedy, Abbott and PaykelKennedy et al, 2003) recently reported a 10-year longitudinal follow-up study of symptom levels in unipolar depression. The present paper reports the first UK longitudinal study of bipolar disorder, using similar methods.
METHOD
Sample
The sample was from a randomised controlled trial of cognitive therapy previously reported in detail (Reference Scott, Paykel and MorrissScott et al, 2006). At five sites (Cambridge, Glasgow, Liverpool, Manchester and Preston), including both inner-city and more-rural areas, all eligible patients with bipolar disorder were recruited from general adult psychiatry services that served defined geographical catchment areas. Participants were given oral and written information and gave written informed consent. Ethical approval was given by the North-East Multicentre Research Ethics Committee in the UK.
Inclusion criteria were:
-
(a) age 18 years or more;
-
(b) history of bipolar I affective disorder meeting DSM-IV criteria (American Psychiatric Association, 1994);
-
(c) history of two or more episodes of illness meeting DSM-IV criteria for mania, hypomania, major depressive disorder or mixed affective disorder, one of which must have been within 12 months of recruitment;
-
(d) currently, or in past 6 months, contact with mental health services.
Exclusion criteria were:
-
(a) bipolar disorder secondary to an organic cause;
-
(b) continuous illicit substance misuse;
-
(c) currently meeting DSM-IV criteria for mania (these patients were included after symptoms improved and patients with current hypomania or a mixed affective episode were included);
-
(d) rapid-cycling bipolar disorder (more than four episodes alternating in the past year with less than a month between);
-
(e) severe borderline personality disorder with suicidal ideation or intent in the past 3 months;
-
(f) current systematic psychological treatment for bipolar disorder;
-
(g) inability to read and write English.
Treatment and follow-up
Participants were randomised by minimisation, to receive in equal proportions either treatment as usual from their usual catchment-area mental health teams, or treatment as usual plus cognitive therapy from trained therapists in up to 20 sessions over 26 weeks. All patients were followed up if possible for a further 12 months to a total of 18 months (72 weeks), irrespective of recurrence or drop-out from the controlled trial.
Outcome measures
Research assistants masked to treatment condition conducted baseline assessment interviews before randomisation and then every 8 weeks for 72 weeks. Training was undertaken for a preliminary 3 months, including joint monthly meetings with audiotaped practice interviews reviewed and re-rated, and differences were discussed and resolved. Reliability was subsequently assessed.
Baseline data included: diagnoses made using the Structured Clinical Interview for DSM-IV Axis I disorders (SCID; Reference First, Spitzer and GibbonFirst et al, 1997) and DSM-IV (American Psychiatric Association, 1994); background information collected to cover a range of socio-demographic, life-history and clinical variables; baseline ratings made on the repeated measures.
Repeated ratings each 8 weeks employed an interview combining SCID, DSM-IV criteria, cross-sectional ratings on the 17-item Hamilton Rating Scale for Depression (HRSD; Reference HamiltonHamilton, 1960) and the Bech-Rafaelsen Mania Rating Scale, Modified Version (MAS; Reference Licht and JensenLicht & Jensen, 1997) and other data.
Longitudinal severity ratings of symptom levels were made at baseline for the current week and at follow-up interviews for each week since the last assessment (8 weeks), based on the LIFE-II Longitudinal Interval Follow-up Evaluation (LIFE-II; Reference Keller, Lavori and FriedmanKeller et al, 1987; Reference Keller, Lavori and KaneKeller et al, 1992). Two LIFE scores were rated, one for mania and one for depression, and each used a six-point scale where 1=no symptoms. The criteria used for these ratings are shown in Table 1. Rating scores could be assigned simultaneously for mania and depression if mixed symptoms were present. For analysis, a further rating of overall severity with the most-severe rating for either mania or depression was used, irrespective of which. For analysis these were grouped into four levels: 1=no symptoms; 2=minor symptoms; 3,4=sub-syndromal symptoms; 5,6=major disorder. Interrater reliability on the LIFE and other measures was assessed by the method of Bland & Altman (Reference Bland and Altman1986) as used for repeatability, on 110 joint ratings from tapes. For the depression rating only 3.6% (4 out of 110), and for the mania rating 2.7% (3 out of 110), of rating pair differences from their joint means were outside Bland & Altman's acceptable range of 2 s.d. of the distributions of these differences. The mean differences were –0.01 for depression and +0.26 for mania, both with an s.d. of 0.62.
| Score | Cue | Rating-point definition |
|---|---|---|
| 6 | Definite, severe | Meets DSM–IV criteria for definite major depressive episode or manic episode, and either prominent psychotic symptoms or extreme impairment in functioning. |
| 5 | Definite | Meets DSM–IV criteria for definite major episode but no prominent psychotic symptoms and no extreme impairment in functioning. (For depression, HRSD score probably 17 or above. For mania, MAS probably 15 or more.) |
| 4 | Marked | Does not meet definite DSM–IV criteria for depressive or manic episode, but major symptoms of the disorder, and some functional impairment. (For depression, HRSD probably between 13 and 16.) |
| 3 | Partial remission | Considerably less psychopathological impairment than full criteria, and less than in score 4. Some clear evidence of symptoms of the disorder, but with no more than moderate impairment in functioning. (For depression, HRSD probably between 9 and 12.) |
| 2 | Minor symptoms | Presence of symptoms of the disorder in relatively mild degree. (For depression HRSD probably between 5 and 8.) |
| 1 | Usual self | Patient has no residual symptoms of the disorder. Significant symptoms from some other condition or disorder may or may not remain: if so, this should be recorded under that condition or disorder. (For depression, HRSD probably 4 or less. For mania, MAS probably less than 7.) |
LIFE, Longitudinal Interval Follow-up Evaluation–II; HRSD, Hamilton Rating Scale for Depression; MAS, Bech–Rafaelsen Mania Rating Scale, modified version
1. Separate ratings were made for depression and mania. Reproduced scale is slightly abridged, with rating scale cue scores for depression and mania combined. HRSD and MAS scores were specified as rough guidelines only
2. For analysis these levels were grouped to four: 1=no symptoms; 2=minor symptoms; 3,4=sub-syndromal symptoms; 5,6=major disorder
Data analyses
Overall trial outcome showed no significant differences between the treatment groups on recurrence, LIFE scores or other key rating variables (Reference Scott, Paykel and MorrissScott et al, 2006). The analyses in this paper combine the two treatment groups, and are based on LIFE ratings, using the three scores respectively for depression, mania and overall severity, each grouped according to the four levels described in the previous section. To avoid overemphasis of small fluctuations, LIFE scores were averaged over the four weekly ratings to provide a monthly rating, and means were rounded to the nearest integer (0.5 rounded up), for grouped analyses. Data were analysed using the Statistical Package for the Social Sciences for Windows, version 11.0. Group differences were tested for significance by two-tailed t-tests, with the 5% level accepted. Predictor analyses were by univariate logistic regressions.
RESULTS
Sample characteristics
In total, 253 patients were included in the main controlled trial, derived from 1260 patients available for initial screening; the major cause of loss was failure to meet inclusion criteria, and also some non-consent for the controlled trial (Reference Scott, Paykel and MorrissScott et al, 2006). For the analyses reported here, to avoid bias in later ratings owing to selective loss of participants with early drop-out and subsequent missing ratings, the sample was reduced by eliminating 49 individuals who lacked all subsequent ratings at any point before 40 weeks (including 17 missing all ratings after baseline, and 8 lacking all ratings after 8 weeks). Other missing ratings were not imputed, but percentages and means were based on available ratings.
The remaining 204 patients were of mean age 42.0 years (s.d.=11.0); 133 (65%) were women; 101 (50%) were of social class Registrar General classification Classes I-III (non-manual); 133 (65%) were not in bipolar episode at inclusion; 52 (26%) were in a major depressive episode; and 19 (9%) were in a hypomanic or mixed episode. DSM-IV diagnoses of most recent episodes were depressive 107 (52%), manic 66 (32%) and hypomanic 31 (15%). Participants had had a median of 11 previous bipolar episodes (depression median 5, mania median 4); 67 (33%) had received a lifetime diagnosis of a comorbid non-bipolar disorder; 89 (44%) had a history of previous substance misuse or dependence; and 179 (88%) were receiving receiving mood stabilisers (lithium or anticonvulsants) at baseline.
Comparison of the 49 patients omitted with the 204 included, on the variables later used in predictor analyses, showed some differences significant at the 5% level. Excluded patients had significantly higher baseline scores on the LIFE overall and depression scores, HRSD total score and MAS mania score, and shorter time since resolution of last episode; and fewer of them were receiving mood stablisers.
Symptom levels over 18 months
Table 2 shows the mean percentages of total months at the four grouped symptom levels over the 18 months, separately for participants in episode at baseline (depression, hypomania, mixed) and not in episode. Individuals in episode tended to spend more time at all symptomatic levels, and less time asymptomatic, than those not in baseline episode. For people in episode initially, on the overall rating 28% of months were asymptomatic, 22% at minor symptom level, 33% at substantial sub-syndromal level and 17% at major symptom level. Regarding people not initially in episode, 55% of months were asymptomatic, 19% at substantial sub-syndromal level and 6% had major symptoms. Consistently, in both groups, about three times as much time was spent with depressive symptoms as with manic symptoms. When the two episode groups were combined (not shown in the table), a mean of 47% of months were asymptomatic, 20% at minor symptom level, 23% at sub-syndromal level and 10% at major symptom level.
Table 2 Mean percentages of months spent at LIFE symptom levels over 18 months

| Percentage of months at level | Depression In episode at baseline | Mania In episode at baseline | Overall severity In episode at baseline | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No (n=143) | Yes (n=61) | No (n=143) | Yes (n=61) | No (n=143) | Yes (n=61) | ||||
| No symptoms (I) Mean (s.d.) | 60.9 (32.3) | 33.7 (27.6) *** | 86.6 (16.4) | 75.7 (24.9) *** | 55.2 (33.4) | 28.3 (25.7) *** | |||
| Minor symptoms (2) Mean (s.d.) | 18.2 (15.4) | 23.1 (15.7) * | 8.1 (10.9) | 13.4 (14.8) * | 19.3 (16.2) | 22.1 (16.4) | |||
| Sub-syndromal | |||||||||
| symptoms (3/4) Mean (s.d.) | 16.4 (18.2) | 30.3 (21.0) *** | 3.9 (6.5) | 7.6 (10.2) * | 19.2 (19.7) | 33.0 (19.7) *** | |||
| Major disorder (5/6) Mean (s.d.) | 4.6 (9.9) | 13.2 (14.5) *** | 0.9 (2.8) | 2.5 (8.8) | 6.4 (11.4) | 16.9 (18.7) *** | |||
LIFE, Longitudinal Interval Follow-up Evaluation – II
* P < 0.05, v. not in episode, by t-test
** P < 0.001
*** P < 0.001
Because patients excluded from analysis (n=49) had characteristics suggesting a worse prognosis, a further analysis was undertaken, including them where possible. This is shown in the data supplement to the online version of this paper, with scores for the reported sample of 204 patients for comparison. For the overall severity rating, inclusion of the omitted individuals would have rendered about 4% fewer months asymptomatic, largely because of more months at major level, at least in the earlier, less biased months.
There was no unipolar comparison group in the present study, but a comparison was available from a 10-year follow-up study (Reference Kennedy, Abbott and PaykelKennedy et al, 2004), by using only patients with at least one previous episode in that study. These people spent a mean of 52% of follow-up months asymptomatic, 20% at LIFE sub-syndromal symptom levels, 15% with minor symptoms and 13% at major depressive disorder level. These findings are very similar to overall severity for those not in episode in the present study, appropriate for comparison since unipolar index major episodes had been up to 10 years earlier. This suggests that when mania and depression are combined, symptom levels are similar to unipolar disorder.
Changes over time
Figure 1 plots the four symptom levels over time on the overall LIFE severity score, separately for participants initially not in episode and in episode. Levels remained approximately constant in those individuals not in episode at baseline. Those in baseline episode showed a gradual improvement, with a greater proportion of time spent at lower symptom levels; however, even after 18 months they tended to spend less asymptomatic time than those not in baseline episode. As shown in the figures, only a minority of the patients rated as in episode at baseline scored at the major symptom level during the first month. This was because the others had improved since the episode, but not for sufficient time (8 weeks) to meet the DSM-IV criteria for being out of episode.
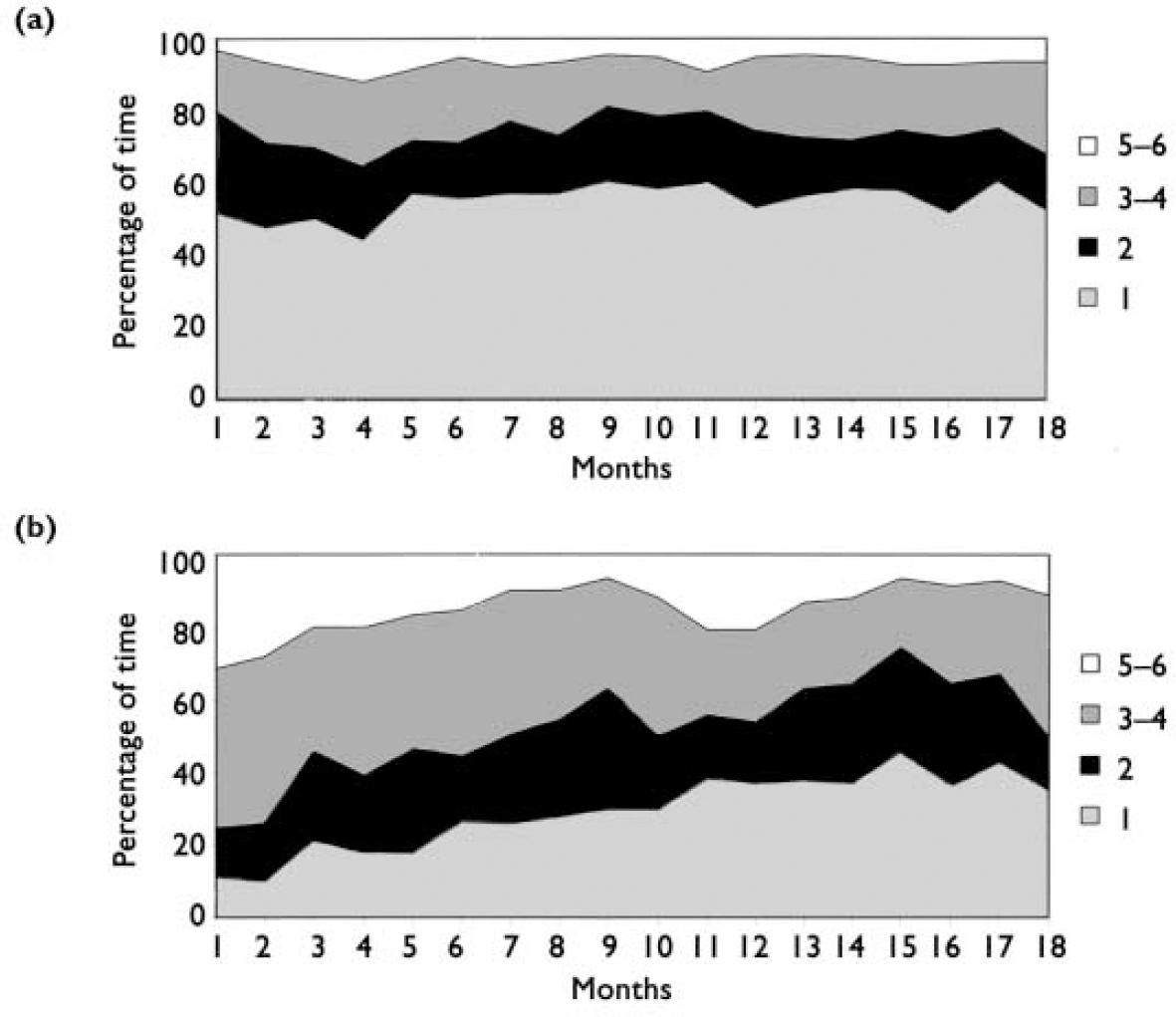
Fig. 1 Overall LIFE scores over 18 months. LIFE, Longitudinal Interval Follow-up Evaluation-II. Boxes indicate scores. (a) Participants not in episode at baseline. (b) Participants in episode at baseline. Baseline scores (week 0) are for that week, not 4 weeks.
Variability in symptom level
Table 3 shows the extent of changes in the grouped symptom levels during the 18-month follow-up period. Over the 18 months there were means of 5.4 changes in depression level, 3.0 changes in mania and 6.0 changes in overall severity level. Only 6% of participants remained at a constant level of overall severity throughout the follow-up. Since these changes were in levels averaged over 4 weeks, this reflects a considerable tendency to change levels. When examined separately, participants not in episode at baseline had a mean of 5.7 changes and participants in episode had a mean of 6.6 changes.
Table 3 Numbers of participants showing changes in monthly LIFE symptom levels over 18 months
| Changes in scores at: | Changes in depression levels | Changes in mania levels | Changes in overall severity levels | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| One level | 18 | 8.8 | 67 | 32.8 | 13 | 6.4 | |||
| Two levels | 47 | 23.0 | 59 | 28.9 | 41 | 20.1 | |||
| Three levels | 76 | 37.3 | 58 | 28.4 | 75 | 36.8 | |||
| All four levels | 63 | 30.9 | 20 | 9.8 | 75 | 36.8 | |||
| Total | 204 | 100 | 204 | 100 | 204 | 100 | |||
| Mean of changes (s.d.) | 5.4 (3.5) | 3.0 (3.1) | 6.0 (3.4) | ||||||
LIFE, Longitudinal Interval Follow-up Evaluation – II
Again, a partial unipolar comparison is provided by data from Kennedy et al (Reference Kennedy, Abbott and Paykel2004). In that study monthly changes were less frequent, at a mean of two annually. Although in that retrospective study some changes might have been missed, and symptoms may tend to stabilise over the longer term, these findings suggest greater variability in bipolar disorder.
Judd et al (Reference Judd, Akiskal and Schettler2002) reported changes in level weekly, so these were also examined. Over the entire sample there was a mean of 9.4 week-by-week changes in depression level and 5.4 in mania. For participants in episode at baseline, the mean changes were depression 11.3 and mania 7.2; for those not in episode, the mean changes were depression 8.6 and mania 4.6.
Changes in polarity on the averaged monthly ratings during the study were infrequent. Only three patients showed changes from a major level of one pole to a major level of the other. A larger number, 20 patients, showed changes from sub-syndromal levels in one direction to the other (12 individuals changing once, 7 twice and 1 three times). However, when weekly changes were examined, in order to compare with Judd et al (Reference Judd, Akiskal and Schettler2002) 34 (17%) participants showed changes from a major level at one pole to a major level at the other, allowing up to 8 weeks between changes, and 15 of these people showed more than one change. Such fluctuations therefore, although not infrequent, tended to be brief.
Predictors of time spent at different symptom levels
In order to examine whether predictors for subsyndromal and major symptoms were the same or different, two separate sets of analyses were undertaken to predict length of occurrence, respectively, of sub-syndromal symptoms (overall LIFE levels 3, 4) and of symptoms at major level (overall LIFE levels 5, 6). Logistic regression was used, since outcome distributions were skewed. For each analysis the outcome measure was dichotomised to short and long at the median length: for sub-syndromal symptoms, 21% of follow-up months (n above=93, below=111): for major symptoms, any (n=103) v. none (n=101). A reduced set of 15 predictor variables was derived from initial and background variables, to focus on those likely to be of relevance from the earlier literature but eliminating variables with substantial overlap, low frequency or unreliability.
Significant predictors were very similar in the two analyses. More time at both symptom levels was predicted significantly by more previous episodes, shorter time since resolution of the last episode, and higher baseline HRSD and LIFE scores. Significantly more time at one level and a trend (P<0.10) for the other was predicted by higher social class, last episode depressive rather than manic, higher baseline MAS and history of substance misuse. Family history of affective disorder in a first-degree relative predicted shorter time with major symptoms (P<0.05), possibly owing to chance. Only one variable, being in episode at baseline, predicted in opposite directions for the two outcomes, predicting longer time with major symptoms and shorter time with sub-syndromal symptoms, possibly because of the time spent with major disorder shortly after baseline. There was no significant prediction by gender, current age, age at first episode, lifetime comorbid diagnosis or being on a mood stabiliser at baseline.
DISCUSSION
This longitudinal study is the first of its kind reported in UK patients with bipolar disorder. It has found that sub-syndromal symptoms constitute a considerable clinical element over time, present for twice as long as major symptoms. Patients not in episode at baseline did better than those in episode, but spent only half the time completely free of symptoms. Changes of symptom level were frequent. Predictors of substantial sub-syndromal symptoms were similar to those of major symptoms, predominantly related to greater severity and previous history.
The study methods had some advantages. Symptoms were evaluated more frequently than in most similar studies, by trained interviewers using established rating scales to anchor the LIFE ratings. Although they all had had an illness episode in the past year, more than half of the participants were not in episode at baseline. Most follow-up studies start in an episode, weighting outcomes towards adverse, except in the very long term. Furthermore, the sample was large and from diverse centres.
There were also some limitations. Participants were selected for a cognitive therapy trial, albeit one aiming at wide inclusion. Criteria excluded patients wtih first episodes, mania until improved and recent rapid cycling, and there were some trial refusals. Some of these weight towards more recurrence and some against it. Biases in trial recruitment tend to produce better-prognosis patients, but in this study outcome was relatively poor. Overall, the participants were probably representative of patients with bipolar disorder in the care of National Health Service mental health services, but did not represent those not requiring this care.
Comparisons with other studies
Although minor forms of the bipolar spectrum without major episodes, such as cyclothymia and bipolar II disorder, are well recognised (Reference AkiskalAkiskal, 1983a ), there has been considerably less attention paid to subthreshold symptoms between major episodes.
The major most directly comparable US study (Reference Judd, Akiskal and SchettlerJudd et al, 2002) reported on longitudinal state over 13 years in 146 patients with bipolar I disorder, using weekly LIFE scores but based on retrospective ratings, initially 6-monthly and later annually. Patients were asymptomatic about 50% of the time, spent about 15% of the time at sub-syndromal level, another 20% with minor symptoms, and only 12% of weeks with major disorder. These findings are comparable with those for our patients not in episode at baseline. In both studies depressive symptoms predominated over manic and hypomanic symptoms, and changes in symptom levels over time were frequent. Judd et al (Reference Judd, Akiskal and Schettler2002) found six changes in weekly ratings per year.
Morriss (Reference Morriss2002) has reviewed the limited additional literature on inter-episode subclinical symptoms in bipolar disorder, using studies with less systematic longitudinal assessment. Inter-episode symptoms, often fluctuating and sometimes prodromal to relapse, have been reported in a number of studies (Reference Molnar, Fava and ZieleznyMolnar et al, 1987; Reference Dion, Tohen and AnthonyDion et al, 1988; Reference Keller, Lavori and KaneKeller et al, 1992; Reference Gitlin, Swendsen and HellerGitlin et al, 1995; Reference Keitner, Solomon and RyanKeitner et al, 1996). Recently Joffe et al (Reference Joffe, Macqueen and Marriott2004) found that 50% of the time over a year or more, patients with bipolar I and II disorder were euthymic, 41% were depressed and only 6% manic. Studies have also pointed to considerable associated social disability. We will report on impaired social adjustment in the present study separately.
Few studies have examined predictors of subthreshold symptoms separately. Nolen et al (Reference Nolen, Luckenbaugh and Altshuler2004), combining major and lesser symptoms, found severity of depression and mania predicted by more previous depressive and manic episodes respectively; and mania only was predicted by comorbid substance misuse, which is somewhat similar to our study. Our main finding was that predictors of sub-syndromal symptoms and of major disorder were essentially the same, in spite of the theoretical possibility that longer periods of one might leave less time for the other. This suggests that major and sub-syndromal symptoms are part of the same continuous phenomenon, which is also strongly supported by the frequent changes in levels over the range.
There is more extensive literature on residual and sub-syndromal symptoms in unipolar affective disorder and on lower-grade subtypes, including dysthymic disorder (Reference AkiskalAkiskal, 1983b ), recurrent brief depression (Reference Angst, Merikangas and ScheideggerAngst et al, 1990) and sub-syndromal depression (Reference Judd, Rapaport and PaulusJudd et al, 1994). It has become clear that similar subthreshold symptoms occur following and between major depressive episodes (Reference Paykel, Ramana and CooperPaykel et al, 1995; Reference Judd, Akiskal and MaserJudd et al, 1998), with considerable continuity between major and minor forms. Our comparison with the Kennedy et al (Reference Kennedy, Abbott and Paykel2004) follow-up study suggests that symptom levels tend to be similar over time in bipolar and unipolar disorder, but that variability is greater in the former.
Therapeutic implications
Our findings underline the need for careful monitoring of the mental state of people with bipolar disorder, and for continuation and maintenance treatment, particularly for those who have had an episode in the past year.
There have been very few treatment studies to target sub-syndromal symptoms. Keller et al (Reference Keller, Lavori and Kane1992) reported a controlled trial in which patients with bipolar disorder received lithium doses at higher plasma levels of 0.8-1.0 mmol/l or lower levels of 0.4-0.6 mmol/l. Both inter-episode sub-syndromal symptoms and major relapses were reduced. This study merits replication and greater attention in treatment recommendations. Some other studies have shown benefit on symptom ratings or affective morbidity, but without separating morbidity due to major relapse. These include trials of lithium, valproate (Reference Bowden, Calabrese and McElroyBowden et al, 2000) and lamotrigine (Reference Bowden, Calabrese and SachsBowden et al, 2003).
There have been limited attempts to examine effects of cognitive-behavioural therapy (CBT) and other psychological therapies on symptoms rather than relapse. Scott et al (Reference Scott, Garland and Moorhead2001), in a small pilot controlled trial, found significant benefit on symptom self-ratings in patients receiving CBT. However, in the large controlled trial from which the present sample was derived, CBT did not produce any benefit on LIFE scores. Lam et al (Reference Lam, Watkins and Hayward2003) found limited effect of CBT on symptom ratings and larger effects on relapse prevention. Miklowitz et al (Reference Miklowitz, George and Richards2003) also reported some benefit on mood symptom ratings from family-focused psychoeducation. Again, these analyses have not distinguished symptoms during relapse from inter-episode symptoms.
The findings of high prevalence of inter-episode sub-syndromal symptoms in bipolar disorder, confirmed in the present study, mandate greater vigilance in clinical practice in detecting and treating these to obtain a symptom-free state, and point to the needs for these issues to be incorporated into treatment guidelines, and for further therapeutic trials aimed at ameliorating these symptoms.
Acknowledgements
We thank R. Bentall, P. Kinderman, A. J. Johnson and S. Palmer, members of the multicentre trial of Cognitive Therapy for Bipolar Disorders, staff at the Biostatistics Office at the Christie Hospital, and the patients who participated in the study. The study was supported by the Medical Research Council.







eLetters
No eLetters have been published for this article.