The operations of the US military since 2001 have raised important concerns about the psychological costs of intense and repeated deployments. Reference Hoge, Auchterlonie and Milliken1-Reference Smith, Wingard, Ryan, Kritz-Silverstein, Slymen and Sallis3 Military personnel deployed for combat operations are frequently exposed to traumatic events and, predictably, those returning from the operations in Iraq and Afghanistan have evidenced increased rates of post-traumatic stress disorder (PTSD). Reference Hoge, Auchterlonie and Milliken1,Reference Smith, Ryan, Wingard, Slymen, Sallis and Kritz-Silverstein2 Unfortunately, it is difficult to accurately assess the psychological cost of deployment in these samples. Reference Litz and Schlenger4 Although previous studies have made important advances in our understanding of deployment-related trauma reactions, with few exceptions Reference Engelhard, van den Hout, Weerts, Hox and van Doornen5,Reference Rona, Hooper, Jones, Iversen, Hull and Murphy6 little prospective research among population-based samples exists to explain how trauma symptoms vary across time. These earlier studies have typically relied on convenience samples, which potentially introduce sampling bias and limit generalisability; use of assessment data that may be vulnerable to reporting bias; and cross-sectional research designs that cannot distinguish trauma reactions from pre-existing symptoms.
The current investigation attempted to fill this knowledge gap by using data from a large population-based sample of military personnel, the Millennium Cohort Study, followed prospectively over nearly a decade. Reference Ryan, Smith, Smith, Amoroso, Boyko and Gray7 A previous study using data from this cohort identified new-onset PTSD symptoms in 7.6-8.7% of deployers who reported combat experiences, compared with 1.4-2.1% of deployers who did not report combat experience. Reference Smith, Ryan, Wingard, Slymen, Sallis and Kritz-Silverstein2 What is not yet known, however, is how post-traumatic stress varies from preto post-deployment, the extent that different trajectories of post-traumatic stress might capture that variation and the predictors that might best inform those trajectories. To address these questions, we examined pre-post trajectories of post-traumatic stress from participants who had deployed at least once in support of these operations.
To identify the trajectories, we employed latent growth mixture modelling (LGMM). Traditional statistical approaches used to examine mental health over time assume a single homogeneous distribution of change. Reference Duncan, Duncan and Strycker8 Recent advances suggest that responses to potential trauma are heterogeneous and explained by a finite set of longitudinal trajectories, Reference Bonanno9 including chronically elevated post-traumatic stress following the event, continuous symptom elevations that preceded the event and elevated pre-deployment (baseline) symptoms followed by steady improvement. This previous research has also repeatedly demonstrated resilient outcomes characterised by a stable trajectory of healthy adjustment (for example little or no symptoms preto post-event). Reference Bonanno, Wortman, Lehman, Tweed, Haring and Sonnega10 Latent growth mixture modelling is well-suited to capture these trajectories because it explicitly assumes outcome heterogeneity. Reference Muthen and Kaplan11 Of note, LGMM has been used effectively to identify prototypical trajectories following different types of potential trauma, including traumatic injury, Reference DeRoon-Cassini, Mancini, Rusch and Bonanno12 natural disaster, Reference Norris, Tracy and Galea13 disease epidemic, Reference Bonanno, Ho, Chan, Kwong, Cheung and Wong14 bereavement Reference Mancini, Bonanno and Clark15 and life-threatening medical procedures. Reference Lam, Bonanno, Mancini, Ho, Chan and Hung16 A recent study mapped trajectories of PTSD symptoms prospectively in a sample of US soldiers deployed on a 6-month NATO-led peacekeeping mission. Reference Dickstein, Suvak, Litz and Adler17 Four distinct trajectories were found in this sample, with 84% categorised in a resilient pattern of low-stable post-traumatic stress from preto post-deployment. Surprisingly absent was a chronic PTSD pattern, which was attributed in part to the fact that peacekeepers experience less exposure to war-related trauma than is normally the case for combat veterans.
Pre-deployment and follow-up data from the Millennium Cohort Study, the largest longitudinal military study, were used to investigate the trajectories of post-traumatic stress symptoms among service members prior to and after deployment.
Method
Population and data sources
The Millennium Cohort Study began collection of self-reported health data in 2001, just prior to the start of military operations in Iraq and Afghanistan. Invited participants to the first panel were randomly selected from US military personnel serving in October 2000, oversampling for women; those previously deployed to Bosnia, Kosovo or Southwest Asia; and reserve and national guard members. Participants are surveyed every 3 years throughout a 21-year planned follow-up period. Detailed descriptions of methodology for the Millennium Cohort Study are available elsewhere. Reference Ryan, Smith, Smith, Amoroso, Boyko and Gray7,Reference Gray, Chesbrough, Ryan, Amoroso, Boyko and Gackstetter18
Of the 77 047 consenting participants who enrolled in the study's first panel (36% baseline response rate), 55 021 (71%) completed the first follow-up (2004-2006) and 54 790 (71%) completed the second follow-up questionnaire (2007-2008). The Defense Manpower Data Center supplied demographic and deployment-related data obtained from electronic personnel files.
This study examined the first panel of participants who completed all three questionnaires as two separate subpopulations: (a) those who had their first complete deployment in support of the operations in Iraq and Afghanistan between baseline and the first follow-up and did not deploy again before April 2009 (single deployers); and (b) those who had their first deployment in support of the operations in Iraq and Afghanistan between baseline and the first follow-up and deployed at least once more in support of the same operations thereafter (multiple deployers).
This research has been conducted in compliance with all applicable federal regulations governing the protection of human subjects in research (Protocol NHRC.2000.0007).
Primary outcome
Post-traumatic stress was assessed at all three time points using the PTSD ChecklistCivilian Version (PCL-C). Reference Weathers, Huska and Keane19 The PCL-C is a 17-item self-reported measure of PTSD symptoms requiring participants to rate the severity of each symptom during the previous 30 days on a Likert scale. Post-traumatic stress scores were examined continuously, ranging from 17 to 85 points (higher scores indicating more symptoms or greater severity).
Covariates
The following covariates were assessed pre-deployment (baseline). Using the Short Form 36-Item Health Survey for Veterans (SF-36V), the Physical Component Summary (PCS) score was used as a continuous measure to assess physical health. Reference Ware and Sherbourne20 Higher scores reflected more favourable health status. History of life stress was assessed as a continuous measure by applying the points and scoring mechanisms of the Holmes and Rahe Social Readjustment Rating Scale. Reference Holmes and Rahe21 Each affirmative response to a stressful event, such as divorce, major financial problems and violent assault, was weighted Reference Holmes and Rahe21 and summed, so higher scores reflected higher stress levels. Two binary variables were used to assess alcohol consumption. Men who reported drinking more than 14 alcoholic drinks per week and women more than 7 drinks per week were considered to be heavy drinkers. Men consuming 5 or more drinks per occasion or day and women who reported 4 or more were considered binge drinkers. Reference Jacobson, Ryan, Hooper, Smith, Amoroso and Boyko22 Based on questions that assessed lifetime smoking habits, participants were classified as never smokers, past smokers or current smokers. Reference Smith, Ryan, Wingard, Patterson, Slymen and Macera23
Combat experience was assessed as a score from 0 to 5 based on the number of affirmative responses to personal exposure in the 3 years before response to the follow-up questionnaire to: witnessing a person's death due to war, disaster or tragic event; instances of physical abuse (torture, beating, rape); dead and/or decomposing bodies; maimed soldiers or civilians; and prisoners of war or refugees. Reference Smith, Wingard, Ryan, Kritz-Silverstein, Slymen and Sallis3 Injury status was derived from the Joint Theater Trauma Registry, a database established in 2002 and maintained by the US Army Institute of Surgical Research. It contains medical information on military personnel who have sustained either non-combat or combat-related injuries during deployment. For single deployers, participants were categorised as injured if an injury was recorded in the Joint Theater Trauma Registry between the baseline and first follow-up. All other participants were categorised as injured if an injury was recorded between their baseline and second follow-up questionnaire.
Statistical analyses
Separate LGMM for single and multiple deployers, using the Mplus statistical modelling programme, was conducted. Reference Muthen and Kaplan11 Latent growth mixture modelling began with a single-class growth model and then added classes to examine improvements in model fit. Reference Muthén24,Reference Nylund, Asparouhov and Muthen25 The final model solution was determined by a combination of fit statistics, conceptual rationale and interpretability. Reference Muthen and Kaplan11,Reference Muthén24,Reference Nylund, Asparouhov and Muthen25
We examined each data-set separately in three steps. First, we identified a single-class growth model without covariates. Second, we compared oneto five-class unconditional LGM models (no covariates) by assessing relative fit with conventional indices (Table 1), which penalise more complex models when they fail to provide a better fit to the data. Reference Muthén24-Reference Lo, Mendell and Rubin26 To ensure that the restricted populations, which excluded participants with missing data, were representative of the larger, unrestricted populations, we compared the unconditional models of the restricted populations with the unrestricted populations. Third, consistent with recommendations for correct model specification, the LGMM was extended to include predictors of class membership in a conditional model. This step is increasingly recommended, Reference Muthén24 since the absence of significant relationships between theoretically relevant covariates and class membership can indicate an incorrect local solution. As recommended, Reference Muthen and Kaplan11 we examined covariates based on their conceptual relevance and performance in preliminary univariate testing. Finally, multinomial logistic regression analyses were nested within the LGMM to examine predictors of class membership.
Results
Of the 77 047 participants, 46 438 completed both follow-up questionnaires. Among those participants, 7272 had missing outcome information and 2946 had incomplete covariate data and hence were excluded, leaving 36 220 participants. Of these eligible participants, there were 7787 participants who had their first complete deployment between their baseline and first follow-up questionnaire. For 3393 of these participants, this was their only deployment until April 2009 (i.e. single deployers). The remaining 4394 participants deployed one or more times thereafter (i.e. multiple deployers).
Characteristics of single deployers, multiple deployers, and all other panel one members are presented in online Table DS1.
Notably, single and multiple deployers were proportionately more likely to be male, active duty, air force members, deploy longer, experience more combat, screen positive for binge drinking, and have lower stress compared with the other panel one participants (P<0.05).
The examination of the unconditional models for the unrestricted (including those with missing outcome or covariate data) and restricted (no missing data) populations indicated no significant difference in the resulting trajectory solutions. Fit statistics for oneto five-class unconditional models (no covariates) showed relative improvements in fit going from two to five classes (Table 1). However, especially with large sample sizes that can accommodate more fine-grained distinctions among classes, fit statistics may suggest theoretically unsound class solutions. The four-class model for single deployers produced a viable, theoretically defensible solution. The five-class model was unparsimonious and unviable because it split one class into two parallel classes, creating a very small class (1.6%), and failed to converge when covariates were included in the model. Accordingly, we chose the four-class solution as optimal. Nested analyses of the four-class single-deployer solution indicated improved fit when the intercept variance was unconstrained (random effect) and when the following covariates were included: age, marital status, education level, service branch, pay grade, PCS, combat experience, smoking status, heavy drinking and binge drinking. Figure 1 shows that the majority of single deployers were assigned to a class with consistently low symptoms (low-stable, 83.1%). Other classes were characterised by low pre-deployment symptoms with elevated and worsening post-traumatic stress after deployment (worsening-chronic, 6.7%), moderate pre-deployment post-traumatic stress that decreased steadily after deployment (moderate-improving, 8.0%), and elevated post-traumatic stress at all measurement points (high-stable, 2.2%). Slope estimates were significantly non-zero for the worsening-chronic post-traumatic stress (28.27, standard error (s.e.) = 2.05, P<0.001) and moderate-improving (–8.86, s.e. = 1.24, P<0.001). The slope for the low-stable group was small, but also significant due to the group's large size and small standard error (1.64, s.e. = 0.14, P<0.001). The slope for the high-stable group was non-significant (–5.07, s.e. = 5.50, P = 0.36).
Among single deployers, those with worsening-chronic, high-stable or moderate-improving post-traumatic stress had a lower PCS score, indicating worse physical health than the low-stable group (Table 2). Interestingly, heavy drinkers had three times greater odds of experiencing high-stable than low-stable post-traumatic stress, but also threefold odds of moderate-improving post-traumatic stress symptoms. The worsening-chronic and highstable groups had more combat experiences than the low-stable
TABLE 1 Fit indices for one- to five-class unconditional growth mixture models for single and multiple deployers

| Fit indices | 1 class | 2 classes | 3 classes | 4 classes | 5 classes |
|---|---|---|---|---|---|
| Single deployers (n = 3393) | |||||
| Akaike information criterion | 71 637.96 | 69 472.81 | 68 532.31 | 67 784.48 | 66 735.33 |
| Bayesian information criterion | 71 693.12 | 69546.36 | 68 611.99 | 67 882.55 | 66 864.05 |
| Sample size-adjusted Bayesian information criterion | 71 664.52 | 69 508.23 | 68 570.69 | 67 831.71 | 66 797.32 |
| Entropy | 0.98 | 0.98 | 0.97 | 0.97 | |
| Lo-Mendell-Rubin likelihood ratio test, P | <0.001 | <0.05 | 0.29 | <0.05 | |
| Bootstrap likelihood ratio test, P | <0.001 | <0.001 | <0.001 | <0.001 | |
| Multiple deployers (n = 4394) | |||||
| Akaike information criterion | 89 371.29 | 86 409.24 | 84 755.68 | 83 830.92 | 83 038.46 |
| Bayesian information criterion | 89 428.78 | 86 485.90 | 84 851.51 | 83 945.90 | 83 172.61 |
| Sample size-adjusted Bayesian information criterion | 89 400.18 | 86 447.77 | 84 803.85 | 83 888.74 | 83 105.88 |
| Entropy | 0.98 | 0.98 | 0.97 | 0.97 | |
| Lo-Mendell-Rubin likelihood ratio test, P | <0.001 | <0.01 | 0.10 | 0.74 | |
| Bootstrap likelihood ratio test, P | <0.001 | <0.001 | <0.001 | <0.001 | |
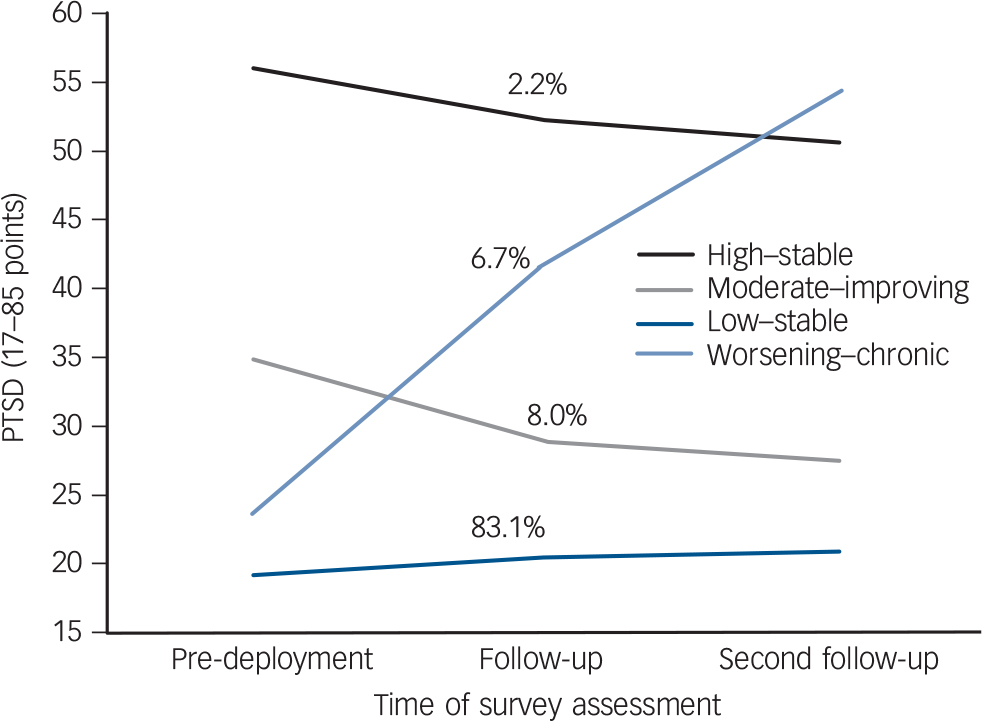
Fig. 1 Conditional model (including covariates) of post-traumatic stress over time among 3393 Millennium Cohort participants with a single deployment between baseline (pre-deployment) and first follow-up.
Post-traumatic stress disorder (PTSD) assessed using the PTSD ChecklistCivilian Version.
group. The worsening-chronic group was more likely to be in the army and have a high-school education or less than the low-stable group.
Similarly to the single deployers, the four-class unconditional model for multiple deployers produced a viable and parsimonious solution, whereas the five-class model again created a very small class (1.3%) and again failed to converge when covariates were included. Thus the four-class solution was selected as optimal. Nested analyses of the four-class solution for multiple deployers indicated improved fit when both the intercept and slope variance were unconstrained and when the following covariates were included: age, education level, service branch, pay grade, combat experience, current smoking and heavy drinking. Figure 2 shows that the majority of multiple deployers were again assigned to a low-stable class (84.9%). Other classes included worsening-chronic (4.5%), moderate-improving (8.5%) and high-improving (2.2%) trajectories. Slope estimates were significantly non-zero for the worsening-chronic post-traumatic stress (31.35, s.e. = 1.78, P<0.001) and high-improving (–15.32, s.e. = 2.94, P<0.001) classes. The slopes were relatively small but also significant for the low-stable (1.29, s.e.= 0.10, P<0.001) and moderate-improving (–4.84, s.e. = 0.84, P<0.001) classes.
TABLE 2 Adjusted odds of class membership, single and multiple deployers a
| Single deployers, OR (95% CI) (n = 3393) | Multiple deployers, OR (95% CI) (n = 4394) | |||||
|---|---|---|---|---|---|---|
| Classes | Worsening–chronic | High–stable | Moderate–improving | Worsening–chronic | High–improving | Moderate–improving |
| Physical component summary b | 0.95 (0.93–0.97) | 0.91 (0.89 – 0.94) | 0.96 (0.94–0.98) | |||
| Education | ||||||
| High school or less | Reference | Reference | Reference | Reference | Reference | Reference |
| More than high school | 0.67 (0.45–0.99) c | 0.55 (0.29–1.02) | 0.71 (0.52–0.97) | 0.66 (0.40 –1.08) | 0.70 (0.36–1.34) | 0.55 (0.41–0.74) |
| Combat experience b | 1.44 (1.31–1.59) | 1.25 (1.02–1.52) | 1.06 (0.97–1.17) | 1.71 (1.53–1.91) | 1.24 (1.05–1.46) | 1.09 (1.01–1.18) |
| Service branch | ||||||
| Navy/coast guard, marine corps, air force | Reference | Reference | Reference | Reference | Reference | Reference |
| Army | 2.57 (1.65–3.99) | 0.96 (0.46–2.03) | 0.92 (0.66–1.29) | 1.78 (1.17–2.69) | 0.98 (0.55–1.76) | 1.08 (0.82–1.43) |
| Pay grade | ||||||
| Enlisted | Reference | Reference | Reference | Reference | Reference | Reference |
| Officer | 0.44 (0.26–0.73) | 0.61 (0.25–1.51) | 0.42 (0.26–0.70) | 0.38 (0.22–0.67) | 0.43 (0.18–1.00) | 0.51 (0.35–0.76) |
| Heavy drinking | ||||||
| No | Reference | Reference | Reference | Reference | Reference | Reference |
| Yes | 1.65 (0.98–2.78) | 3.14 (1.57–6.28) | 3.08 (2.08–4.58) | 1.64 (0.98–2.74) | 1.83 (0.96–3.48) | 2.03 (1.41–2.94) |
| Binge drinking | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 1.12 (0.77–1.63) | 0.89 (0.40–1.96) | 1.25 (0.89–1.74) | |||
| Smoking status | ||||||
| Current smoker | Reference | Reference | Reference | |||
| Never smoker | 0.66 (0.42–1.05) | 0.43 (0.21–0.85) | 0.77 (0.53–1.14) | |||
| Past smoker | 0.51 (0.30–0.87) | 0.58 (0.30–1.10) | 0.76 (0.50–1.15) | |||
| Current smoker | ||||||
| No | Reference | Reference | Reference | |||
| Yes | 1.08 (0.69–1.68) | 1.97 (1.22–3.17) | 1.71 (1.30–2.26) | |||
| Age b | 1.03 (1.00–1.05) | 1.01 (0.97–1.06) | 0.98 (0.96–1.01) | 1.00 (0.97–1.03) | 0.95 (0.91–0.98) | 1.00 (0.98–1.01) |
| Marital status | ||||||
| Divorced | Reference | Reference | Reference | |||
| Never married | 1.89 (0.79–4.51) | 1.92 (0.56–6.57) | 1.05 (0.57–1.91) | |||
| Married | 1.59 (0.71–3.55) | 1.17 (0.40–3.41) | 0.73 (0.42–1.27) | |||
a Empty spaces in table indicate that a given covariate did not improve fit and was not included in the model.
b Measured continuously; relative odds based on one-unit increments.
c Bolding indicates significance based on a P < 0.05 criterion in adjusted analyses.
Multiple deployers in the moderate-improving and worsening-chronic groups were more likely to be enlisted service members and to report greater combat experience compared with low-stable participants (Table 2). Participants in the moderateimproving class were more likely to have a high-school education or less, report current smoking and screen positive for heavy drinking when compared with the low-stable group. Worsening-chronic post-traumatic stress participants had greater odds of being in the army compared with the low-stable group.
Discussion
Main findings
Our trajectory analyses of the Millennium Cohort data addressed many of the key methodological limitations of previous studies on deployed military personnel and revealed several noteworthy findings. First, across both the singleand multiple-deployer samples, the proportion exhibiting a stable trajectory of low post-traumatic stress preto post-deployment, or resilience, was exceptionally prevalent (83.1% and 84.9% respectively). High proportions of resilience have been reported across a range of trauma and disaster studies. Reference Bonanno9,Reference Bonanno, Wortman, Lehman, Tweed, Haring and Sonnega10,Reference Bonanno, Ho, Chan, Kwong, Cheung and Wong14 The fact that the proportions were even higher in the current investigation was not altogether surprising. The exemplary resilience in these studies might be expected, given the level of preparedness and training common to US military personnel. Prior experience and training have generally been associated with favourable outcomes in
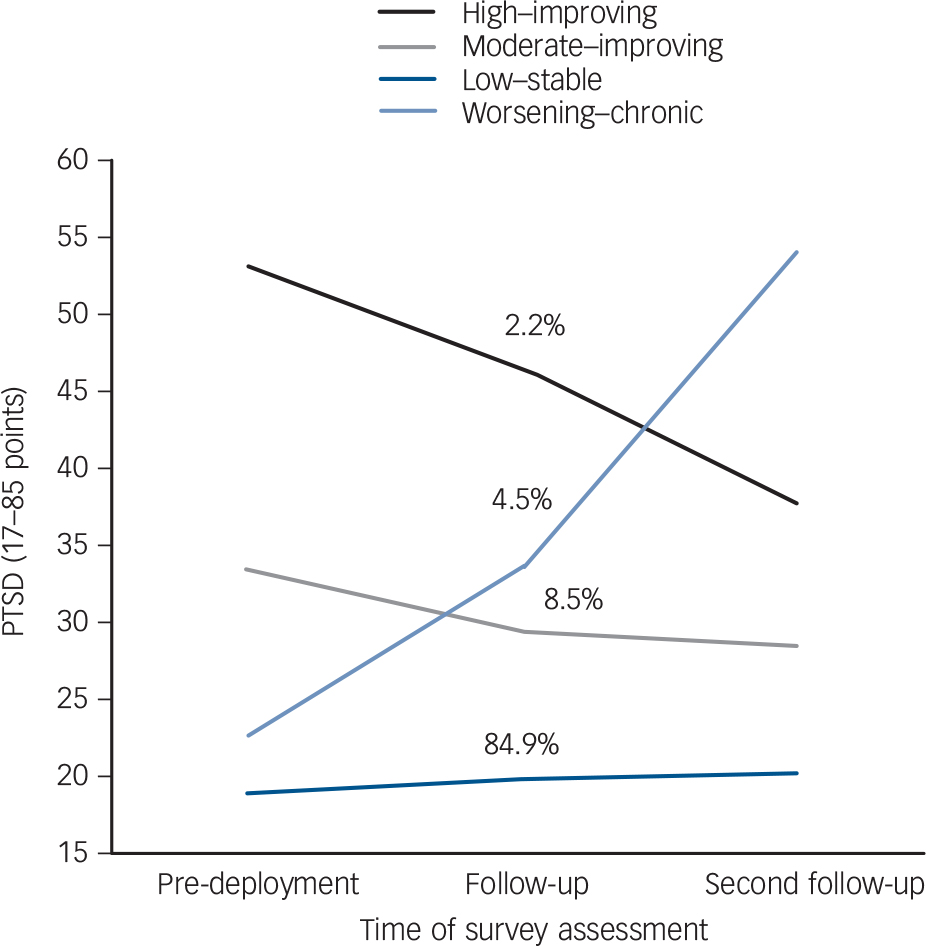
Fig. 2 Conditional model (including covariates) of posttraumatic stress over time among 4394 Millennium Cohort participants with multiple deployments.
Post-traumatic stress disorder (PTSD) assessed using the PTSD Checklist-Civilian Version.
populations at risk for trauma exposure, Reference Dougall, Herberman, Delahanty, Inslicht and Baum27 presumably because they increase perceptions of control and self-efficacy, help shape constructive appraisals and facilitate regulation of physiological and emotional reactions. Reference Whealin, Ruzek and Southwick28 Similar levels of resilience were reported in the prospective study of United Nations peacekeepers. Reference Dickstein, Suvak, Litz and Adler17
Extending previous population-based military studies, the proportion exhibiting worsening-chronic post-traumatic stress was relatively modest (6.7% of single deployers and 4.5% of multiple deployers). Several factors highlighted in recent reviews Reference Richardson, Frueh and Acierno29,Reference Sundin, Fear, Iversen, Rona and Wessely30 help explain these findings. First, many studies have assessed symptoms based on a screening tool using four items and in proximity to deployment, whereas these analyses are based on a 17-item assessment with an average of 2.7 years between questionnaire responses. Second, the Millennium Cohort is a population-based sample including all service branches as well as reserve and national guard. Studies of Department of Veterans Affairs populations that report higher levels of PTSD only account for a minority of veterans who self-select to receive treatment. In addition, elevated levels of PTSD symptoms have been associated with seeking medical compensation, whereas the endorsement of PTSD symptoms in the Millennium Cohort questionnaire was confidential and not tied to either monetary compensation or treatment. Reference Smith, Ryan, Wingard, Slymen, Sallis and Kritz-Silverstein2,Reference Frueh, Elhai, Grubaugh, Monnier, Kashdan and Sauvageot31 Finally, many studies Reference Hoge, Auchterlonie and Milliken1,Reference Hoge, Castro, Messer, McGurk, Cotting and Koffman32,Reference Kang and Hyams33 have used retrospective methods to assess the proportion of PTSD symptoms, which may create artificial associations between PTSD and deployment due to either recall or selection bias. The prospective design of this study assessed PTSD symptoms at time points before and after deployment.
The final models exhibited the same number and similar types of trajectories for single and multiple deployers. The most elevated post-traumatic stress scores pre-deployment represented only 2.2% of the study population in both single and multiple deployers. However, post-traumatic stress scores in multiple deployers showed greater improvement over time compared with single deployers. In addition, fewer service members experienced elevated post-traumatic stress, in general, among the multiple deployers. These findings may indicate that at least some service members who deploy multiple times may be able to participate in repeated deployments because they are healthier or perhaps they view themselves as physically and mentally fit for deployment.
Another interesting finding was that small but meaningful numbers of service members who experienced moderate or elevated pre-deployment post-traumatic stress showed some improvement in post-traumatic stress over time. This improvement pattern had been observed previously in the United Nations peacekeeper study, Reference Dickstein, Suvak, Litz and Adler17 as well as in prospective bereavement studies involving end-of-life caregivers. Reference Bonanno, Wortman, Lehman, Tweed, Haring and Sonnega10,Reference Schulz, Mendelsohn, Haley, Mahoney, Allen and Zhang34 It is important to note, however, that in our study these participants, particularly the high-improving group, were not entirely free of post-traumatic stress at follow-up.
Given that the vast majority of our study population exhibited a resilient pattern of low-stable post-traumatic stress scores, we were especially interested in predictors of this group. Compared with those experiencing low-stable post-traumatic stress, single deployers with all other stress patterns reported worse physical health and, with the exception of the moderate-improving class, experienced more combat. The latter is not surprising because combat experience has consistently been demonstrated as one of the strongest predictors of PTSD following deployment. Reference Hoge, Auchterlonie and Milliken1,Reference Smith, Ryan, Wingard, Slymen, Sallis and Kritz-Silverstein2,Reference Hoge, Castro, Messer, McGurk, Cotting and Koffman32,Reference Brewin, Andrews and Valentine35,Reference Foy, Sipprelle, Rueger and Carroll36
Among single deployers, the worsening-chronic post-traumatic stress class with elevated post-traumatic stress post-deployment was also more likely to be enlisted and in the army compared with the low-stable class. This is not unexpected since ground infantry, largely composed of army-enlisted personnel, would be most likely to experience combat. Among single deployers, service members exhibiting worsening-chronic post-traumatic stress were also more likely to be high-school or less educated, which is consistent with lower pay grade. Predictably, the worsening-chronic group also experienced the greatest level of combat.
The most prominent predictors of membership in the classes showing improvement in both single and multiple deployers included reporting heavy drinking and enlisted status at baseline compared with the low-stable groups. In multiple deployers, current smoking predicted membership in the improving symptoms class, and in both single and multiple deployers, the improving symptoms classes had significantly lower education than the low-stable groups. Although still reporting post-traumatic stress symptoms, it is possible that these improving groups were using alcohol or smoking as maladaptive coping mechanisms. Individuals reporting a pattern of pre-deployment heavy drinking may be more likely to use alcohol to self-medicate for post-traumatic stress symptoms. A recent study among adolescents exposed to traumatic events suggested that post-traumatic stress symptoms are associated with coping-related drinking motives. Reference Dixon, Leen-Feldner, Ham, Feldner and Lewis37 Additional factors that might foster improvements in post-traumatic stress over time are unit cohesion and social support. Supportive resources may mitigate the chronic effects of combat-related trauma, particularly among enlisted service members, because they provide opportunities to participate in community-based, healthcare provider or military command-directed reintegration programmes.
Membership in the high-stable (single deployers) and high-improving (multiple deployers) classes was predicted by similar variables, such as being a current smoker. In addition, both reported more combat experience than their moderate-improving and low-stable post-traumatic stress counterparts. Interestingly, heavy drinking was not a predictor of worsening post-traumatic stress after deployment but rather associated with moderate and elevated pre-deployment post-traumatic stress.
Strengths and limitations
Using Millennium Cohort data for this study had advantages. It provided a prospective assessment for both exposures and outcomes of interest, with an average of 2.7 years between assessments; it included members from all services and personnel from the national guard and reserves; sample sizes were sufficiently large to obtain statistically meaningful results; and the data allowed for adjustment of potential confounders that are otherwise difficult to obtain from sources other than self-report.
There were also a number of potential limitations to the study. As there was variability in the time from post-traumatic stress assessments to when participants started and ended deployment(s), sensitivity analyses were performed to test the possible effects of time from baseline (pre-deployment) to first deployment and time from last deployment to second follow-up on the trajectory assignments in both the singleand multiple-deployer populations. When entered separately into the final models as continuous variables, these variables did not increase fit for either the singleor multiple-deployer populations. We concluded, therefore, that the variability in time did not influence the trajectory solutions of the models.
In evaluating the data, we note that although the initial response rate to invitation in the Millennium Cohort Study was 36%, multiple studies of possible reporting and selection biases in baseline cohort data suggest reliable reporting, minimal response bias and a representative sample of military personnel, including deployers. Reference Smith, Ryan, Wingard, Slymen, Sallis and Kritz-Silverstein2,Reference Smith, Wingard, Ryan, Kritz-Silverstein, Slymen and Sallis3,Reference Ryan, Smith, Smith, Amoroso, Boyko and Gray7,Reference LeardMann, Smith, Smith, Wells and Ryan38-Reference Wells, LeardMann, Smith, Smith, Jacobson and Reed44 Several participants had missing data; however, trajectory solutions with and without missing data did not differ. It is possible that the use of self-reported symptom data to identify individuals with chronic post-traumatic stress might be less precise than medical diagnosis; however, previous studies using questionnaire instruments for PTSD have shown good agreement with medical diagnosis. Reference Smith, Smith, Jacobson, Corbeil, Ryan and Team40 Moreover, in some cases military personnel avoid seeking healthcare for mental disorders, which would likely lead to underreporting of post-traumatic stress using medical diagnoses. Reference Hoge, Castro, Messer, McGurk, Cotting and Koffman32
Another potential limitation was that because we measured adjustment solely in terms of post-traumatic stress, it is possible that our analyses failed to capture other forms of dysfunction. Also, in some cases, LGMM analyses may identify non-normality rather than true mixture distributions. We consider this possibility unlikely given the large representative sample, the high degree of accuracy in classifying participants into trajectories and the coherent pattern of covariate prediction for each of the trajectory patterns. Reference Muthén24
Implications
These data offer the first prospective view of post-traumatic stress in a large military population, with measurement of post-traumatic stress prior to deployment, and indicate that the vast majority of service members remained without significant post-traumatic stress symptoms prior to and following deployments. The next highest proportion of participants showed an improving trend despite having one or more deployments. Only a small minority of the participants exhibited persistent or worsening symptoms. The most prominent predictors of these groups with worsening or persistently high levels of post-traumatic stress are, for the most part, difficult to change (for example enlisted army service members who experience combat). Some programmes have been created and implemented to develop psychological resiliency (such as battlemind training) among these high-risk groups, however, perhaps more is needed in terms of preventive interventions for PTSD in these specific groups of deployers. Smoking, a modifiable behaviour, also predicted membership in many of the groups with moderate or high levels of post-traumatic stress. This finding further stresses the importance of programmes aimed at smoking cessation and the prevention of its initiation or resumption among military personnel, particularly those who experience higher levels of PTSD. We cannot easily revisit previous conflicts to measure their psychological cost. However, the current findings provide a rare glimpse at the natural history of post-traumatic stress symptoms in relation to recent military deployments and thus may also help illuminate the mental health burden of both past and future conflicts.
Funding
The Millennium Cohort Study is funded through the Military Operational Medicine Research Program of the US Army Medical Research and Materiel Command, Fort Detrick, Maryland. This represents report 11-08, supported by the Department of Defense, under work unit no. . The funding organisation had no role in the design and conduct of the study; collection, analysis, or preparation of data; or preparation, review or approval of the manuscript. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of the Army, Department of the Air Force, Department of Defense, Department of Veterans Affairs or the US government. Resources from the VA Puget Sound Health Care System supported E.J.B.'s involvement in this research.
Acknowledgements
We thank Scott L. Seggerman from the Management Information Division, Defense Man-power Data Center, Seaside, California. We also thank Michelle LeWark from the Naval Health Research Center. We thank the professionals from the US Army Medical Research and Materiel Command, especially those from the Military Operational Medicine Research Program, Fort Detrick, Maryland. We appreciate the support of the Henry M. Jackson Foundation for the Advancement of Military Medicine, Rockville, Maryland. We are indebted to all the members of the Millennium Cohort for their participation in this important project. In addition to the authors, the Millennium Cohort Study Team includes Melissa Bagnell, Gina Creaven, James Davies, Nisara Granado, Dennis Hernando, Isabel Jacobson, Kelly Jones, Travis Leleu, Gordon Lynch, Jamie McGrew, Hope McMaster, Amanda Pietrucha, Amber Seelig, Beverly Sheppard, Besa Smith, Katherine Snell, Steven Speigle, Kari Sausedo, Martin White, James Whitmer, and Charlene Wong, from the Deployment Health Research Department, Naval Health Research Center, San Diego, California.







eLetters
No eLetters have been published for this article.