Introduction
Depression is a common mental health disorder that involves a variety of symptoms including loss of pleasure, fatigue, sleep difficulties, poor concentration, indecisiveness, feelings of worthlessness and suicidal thoughts (American Psychiatric Association, 2022).
The behavioural approach is a dominant model to understand and treat depression indicating there is an association between one’s environment and behaviour which evolve over time (Dimidjian et al., Reference Dimidjian, Martel, Addis, Herman-Dunn and Barlow2008). This approach focuses on ‘if–then’ contingencies: for example, if a person stays in bed then what are the consequences of this behaviour for their mood and quality of life? Reinforcement plays a central role in the behavioural approach to depression. Positive reinforcement involves the presence of a reinforcer which maintains or increases a behaviour, whereas negative reinforcement involves the removal of an aversive or unpleasant stimulus or circumstance to maintain or increase behaviour (Polenick and Flora, Reference Polenick and Flora2013). For example, staying in bed within the context of depression may be positively reinforced by feelings of comfort or receiving sympathy from others, although also may be negatively reinforced as it reduces exposure to social interactions that the individual finds unpleasant or anxiety-provoking.
Symptoms of depression can act as negative reinforcers (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001). For example, rumination or social isolation can temporarily reduce unpleasant feelings, causing these behaviours to be strengthened via negative reinforcement and become learned habits (Kanter et al., Reference Kanter, Busch, Weeks and Landes2008). This may provide temporary relief in the short-term but people are then less likely to engage with meaningful or pleasurable activities, which ultimately maintains or increases depressive symptoms, resulting in a negative cycle (Carvalho and Hopko, Reference Carvalho and Hopko2011; Jacobson et al., Reference Jacobson, Martell and Dimidjian2001). Ageing is also an important consideration within the behavioural model (Polenick and Flora, Reference Polenick and Flora2013). Aspects of ageing, which may include neurocognitive difficulties such as memory decline, can negatively reinforce symptoms of depression such as avoidance. Individuals may seek to escape or avoid social interactions if memory problems (such as forgetting names of acquaintances or repeating stories) have resulted in feelings of shame, anxiety or embarrassment. The removal of an unpleasant stimulus (negative emotions due to memory problems) maintains avoidance and subsequently reduces opportunities for the person to experience naturally positive reinforcers linked to socialising and increased activity. Therefore, behavioural theories predict that increases in negative reinforcement and decreases in positive reinforcement (combined with the impact of adverse life events) result in the maintenance of depression (Polenick and Flora, Reference Polenick and Flora2013).
The behavioural model stimulated the development of behavioural activation (BA) to treat depression (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001; Polenick and Flora, Reference Polenick and Flora2013). This approach involves the therapist and client working collaboratively to determine individualised activation strategies that will be reinforcing and pleasurable for the client to disrupt the factors maintaining depression (Dimidjian et al., Reference Dimidjian, Martel, Addis, Herman-Dunn and Barlow2008). Randomised controlled trials have demonstrated the effectiveness of BA in the treatment of depression. BA is argued to be as effective as ‘pure’ cognitive behavioural therapy (CBT), is more cost effective and can be delivered by low intensity workers (Richards et al., Reference Richards, Ekers, McMillan, Taylor, Byford, Warren, Barrett, Farrand, Gilbody, Kuyken, O’Mahen, Watkins, Wright, Hollon, Reed, Rhodes, Fletcher and Finning2016; Richards et al., Reference Richards, Rhodes, Ekers, McMillan, Taylor, Byford, Barrett, Finning, Ganguli, Warren, Farrand, Gilbody, Kuyken, O’Mahen, Watkins, Wright, Reed, Fletcher, Hollon and Woodhouse2017). A meta-analysis also revealed that BA is effective in depression treatment with effects maintained after 2- and 6-month follow-ups (Cuijpers et al., Reference Cuijpers, van Straten and Warmerdam2007). Pertinent to this article, a recent systematic review and meta-analysis indicated that BA significantly reduced depressive symptoms in older adults, indicating its suitability for this client group (Orgeta et al., Reference Orgeta, Brede and Livingston2017).
Despite the effectiveness of BA, studies have mainly focused on working age adults. This prompted adaptations to be considered when using BA with older adults (Pasterfield et al., Reference Pasterfield, Bailey, Hems, McMillan, Richards and Gilbody2014). These adaptations typically consider physical health (the impact of one’s physical health and carefully selecting activities appropriate to the person’s level of functioning), cognitive impairment (simplifying language and less demanding homework tasks), social support (social contact and considering family/role changes) and risk of suicide (past and present ideations). Evidence indicates that incorporating adaptations within BA, particularly physical health adaptations, can reduce depressive symptoms in older adults (Gilbody et al., Reference Gilbody, Lewis, Adamson, Atherton, Bailey, Birtwistle, Bosanquet, Clare, Delgadillo, Ekers, Foster, Gabe, Gascoyne, Haley, Hamilton, Hargate, Hewitt, Holmes, Keding and McMillan2017). While these adaptations can help professionals deliver more thoughtful interventions for older adults with depression, there are few published case studies applying such ideas to older adults with depression and co-occurring mild cognitive impairment (MCI).
Furthermore, when working with older adults with co-occurring depression and MCI, it is important to consider the contribution of other co-morbid factors such as physical health status and neurocognitive difficulties such as MCI or dementia (Orgeta et al., Reference Orgeta, Brede and Livingston2017). While definitions of MCI vary (Diaz-Mardomingo et al., Reference Diaz-Mardomingo, Garcia-Herranz, Rodriguez-Fernandez, Venero and Peraita2017), this presentation typically reflects objective evidence of impairment in one or more neurocognitive domain (memory, attention, etc.) alongside preserved daily functioning (Albert et al., Reference Albert, DeKosky, Dickson, Dubois, Feldman, Fox, Gamst, Holtzman, Jagust, Petersen and Snyder2011). A systematic review and meta-analysis found the prevalance of depression in individuals with MCI was 32% (Ismail et al., Reference Ismail, Elbayoumi, Fischer, Hogan, Millikin, Schweizer, Mortby, Smith, Patten and Fiest2017) and the prevelance of MCI in older adults ranges between 5 and 30% depending on age and severity (Overton et al., Reference Overton, Pihlsgard and Elmstahl2019). Practice guidelines for MCI (Petersen et al., Reference Petersen, Lopez, Armstrong, Getchius, Ganguli, Gloss, Gronseth, Marson, Pringsheim, Day, Sager, Stevens and Rae-Grant2018) recommend the treatment of reversible causes, which includes interventions targeting mood difficulties, lifestyle adaptations and promoting neurocognitive stimulation and adaptations. With respect to mood, a Cochrane review found CBT treatments (including BA) have small but positive effects on depression in people with MCI or dementia (Orgeta et al., Reference Orgeta, Brede and Livingston2017). However, the authors argued more evidence is needed to help determine which psychological treatments and change techniques are best for people with depression and MCI or dementia. Therefore, this case study outlines the delivery of individual BA with an older adult male with co-existent depression and MCI.
Case study
Presenting problem
Mr C was referred to his local Community Mental Health Team (CMHT) by his general practitioner (GP). He sought help for memory difficulties after noticing some problems with forgetfulness and short-term recall. Mr C completed an initial assessment with a consultant psychiatrist which resulted in a referral for a MRI scan; however, this was not administered due to Mr C experiencing claustrophobia. Mr C completed a cognitive screening tool, the Addenbrooke’s Cognitive Examination (ACE-III: Mathuranath et al., Reference Mathuranath, Nestor, Berrios, Rakowicz and Hodges2000), with the psychiatrist where his score (89/100) led to a working diagnosis of amnestic (memory-related) MCI. During this assessment, it was uncovered that Mr C was feeling depressed, reluctant to go out and very isolated. Therefore, it was hypothesised that his memory difficulties could be ascribed to his depressed mood in addition to MCI and he was subsequently referred for a psychological assessment. During the therapy assessment, Mr C disclosed a history of depression and described spending most of his time on the sofa, which was linked to reduced motivation and limited engagement with activities. Mr C previously received therapy via a local Improving Access to Psychological Therapies (IAPT) service (now known as NHS Talking Therapies) at ‘Step 2’. This involved low intensity guided self-help based on CBT principles. Mr C reported that he did not find this useful, discontinued the intervention and asked to be discharged. However, Mr C appeared willing to engage and was agreeable to completing a therapy intervention.
Detailed history and assessment of the problem
Mr C was born in the 1950s and grew up in England. His father left home when he was 9 months old and he was raised by his mother. Mr C left school with few GCSEs and completed an engineering apprenticeship before working for 5 years in a factory. Following this, he returned to college before moving into social care where he worked for 25 years. In his 50s, Mr C was promoted but struggled to manage difficult dynamics in his team, which resulted in what he described as a ‘nervous breakdown’, causing him to leave the post and experience his first episode of depression. This was when Mr C first entered therapy via NHS Talking Therapies but stated that he did not connect with the therapist as he could not grasp the rationale for discussions or homework tasks. After 6 months of sickness-related absence, Mr C elected to take early retirement in his late 50s.
Since retiring over 10 years ago, Mr C described difficulties adjusting. While he initially gained enjoyment from cycling, he had recently lost interest in this hobby and described feeling lethargic and lonely. These feelings appeared linked to his wife continuing to work, causing him to spend long periods alone. Mr C reported that his social interaction had recently decreased and he had started declining social invitations from friends. While Mr C’s mood lifted when his wife stopped working, she sustained a physical injury that prevented them from achieving their retirement plans (to complete cycling tours together), which further impacted on his mood. As a consequence of decreased exercise, Mr C reported feelings of fatigue and pain when he occasionally cycled, which led to him spending more time resting on the sofa following such excursions.
Mr C’s distress increased during the pandemic due to concerns about his wife returning to a key worker role and her subsequently contracting COVID-19. This left him feeling stressed, worried, isolated and having little to occupy his time. In response, Mr C’s motivation reduced and he developed sleep problems due to spending most of his day on the sofa. During the assessment, Mr C reported ongoing symptoms of depression because he was ‘frustrated’ and ‘disappointed’ with himself. He felt he should be doing more activities (such as cycling, seeing people and completing household tasks) but could not muster the motivation to complete these.
Mr C described a typical day as waking up, having breakfast and sitting on his sofa for several hours. Through the course of the assessment, it became evident that Mr C was not engaging with activities that would provide pleasure, achievement and social contact, causing a vicious cycle whereby he felt low and engaged in more avoidance behaviours. Mr C’s negative and self-critical thoughts also maintained his depression: for example, noting cognitions like ‘I hate myself for spending so much time on the sofa’. He also described ruminating (most commonly at night) where he would fixate on past regrets and behaviour linked to historic work stress.
Research suggests that older adults may minimise depressive symptoms: for example, attributing depressive symptoms such as anhedonia and loss of interest as part of normal ageing (Balsamo et al., Reference Balsamo, Cataldi, Carlucci, Padulo and Fairfield2018). This was evident during the assessment process with Mr C as he would frequently refer to his difficulties as ‘frustration’ rather than identifying with low mood or depression. Furthermore, Mr C’s self-reported depression was 4/10 (0 being no depression and 10 being extreme depression), which was lower than his scores on mood questionnaires.
Therapy goals
Mr C articulated three goals for therapy:
-
(1) To be able to complete spontaneous activities again, such as taking his wife for a meal or accepting social invitations.
-
(2) To get his ‘old life’ back, which would be evident by him cycling twice a week, spending more time with his wife and restarting photography.
-
(3) To reduce the amount of time spent on the sofa.
Outcome measures
Standardised measures were used to help monitor Mr C’s progress. These included the Clinical Outcomes in Routine Evaluation-10 (CORE-10: Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013) and the Patient Health Questionnaire (PHQ-9: Kroenke et al., Reference Kroenke, Spitzer and Williams2001). Both measures have been described as having acceptable reliability properties (Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013; Kroenke et al., Reference Kroenke, Spitzer and Williams2001) and are cited as useful measures for an older adult population (Barkham et al., Reference Barkham, Culverwell, Spindler and Twigg2005; Phelan et al., Reference Phelan, Williams, Meeker, Bonn, Frederick, LoGerfor and Snowden2010). During the therapy assessment, Mr C scored 23/40 on the CORE-10 (indicating ‘moderate to severe’ psychological distress) and 12/27 on the PHQ-9 (indicating ‘moderate depression’).
Given Mr C’s therapy goals, an idiosyncratic outcome measure was developed using an activity monitor to consider the percentage of time he spent on the sofa and engaging with meaningful activities. The activity monitor involved Mr C recording the activities he engaged with every hour, every day of the week. This activity monitor was introduced early in therapy and identified that Mr C was spending 63% of his waking hours on the sofa and only 20% of his time engaged in meaningful activities.
A repeat ACE-III was also administered a year after treatment completion. The ACE-III is a cognitive screening tool designed to help with early detection of dementia and differentiate between Alzheimer’s disease and frontotemporal dementia (Mathuranath et al., Reference Mathuranath, Nestor, Berrios, Rakowicz and Hodges2000). It is composed of tests of neurocognitive abilities including attention, orientation, memory, language, visual perception and visuospatial skills. Scores are out of 100 with higher scores indicating greater neurocognitive functioning (Bruno and Vignana, Reference Bruno and Vignaga2019). Given Mr C’s diagnosis of MCI, a repeat ACE-III was administered to help track progression in neurocognitive difficulties over time after receiving treatment for depression.
A risk assessment was completed during the psychology assessment and Mr C’s risk to self and others was assessed as low. Risk was further monitored via weekly administration of the PHQ-9 questionnaire, as item 9 asks about thoughts around death or harming oneself. Mr C scored 0 on this item each time this measure was completed.
Formulation
A psychological formulation was co-constructed with Mr C using principles of BA (see Fig. 1). Mr C was insightful about the precipitating factors for his current depressive episode, which included retirement, his wife’s physical health issues and stressors experienced during the pandemic. In response to these stressful events, Mr C responded by doing less which restricted his access to activities and positive reinforcers, causing him to experience low mood, tiredness, frustration and a diminished sense of purpose. Due to these feelings, Mr C’s mood was negatively reinforced by spending protracted periods of time on the sofa, sleeping more during the day, avoiding people or social interactions and rumination on past regrets. Ultimately, the increase in negative reinforcers and decrease in positive reinforcers left Mr C feeling depressed, which in turn resulted in a maintenance cycle, as illustrated in Fig. 1.
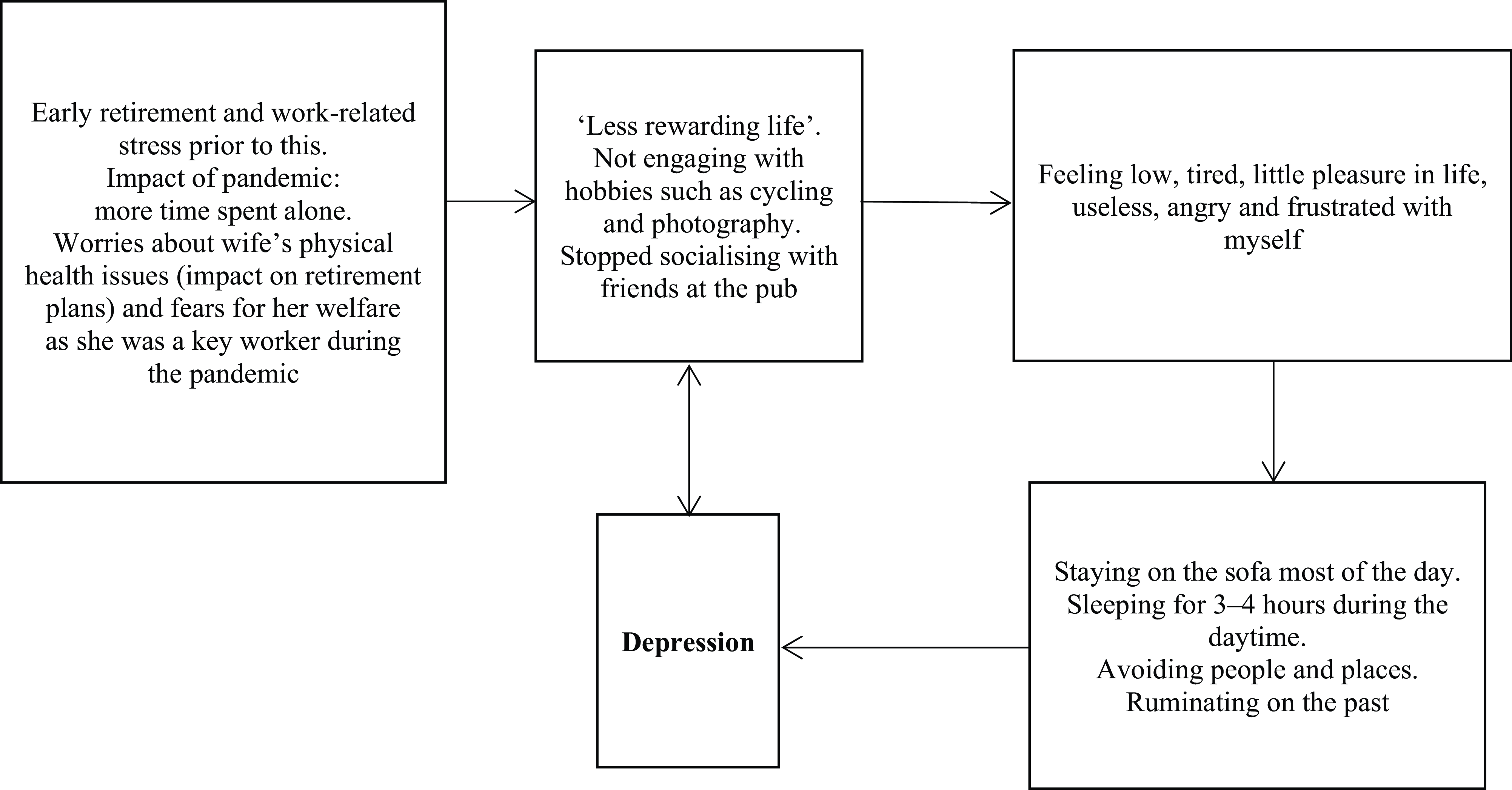
Figure 1. Maintenance cycle.
Research indicates that life transitions can be linked to depression (Moustafa et al., Reference Moustafa, Crouse, Herzallah, Salama, Mohamed, Misiak, Frydecka, Al-Dosari, Megreya and Mattock2020) and Mr C reported difficulties adjusting to retirement and the changes this caused in both his daily routine and valued social roles. According to psychosocial stage theory (Erikson and Erikson, Reference Erikson and Erikson1997), Mr C was navigating the developmental task of ‘ego integrity versus despair’ which involves reflecting back on one’s life experiences to integrate personal regrets with achievements. These reflections were important for supplementing the BA intervention, as Mr C described feelings of shame, anger and regret due to his ‘nervous breakdown’ and subsequent early retirement. When feeling low, Mr C would engage in excessive rumination about this difficult period of his life, causing him to notice self-critical thoughts. Research suggests that rumination plays an important role in maintaining depression (Nolen-Hoeksema, Reference Nolen-Hoeksema1991; Nolen-Hoeksema et al., Reference Nolen-Hoeksema, Wisco and Lyubomirsky2008; Sun et al., Reference Sun, Tan, Fan and Tsui2014) and Mr C’s tendency to dwell on past events appeared to lower his mood. As such, it was agreed with Mr C that therapy needed to also target these ruminative and self-critical processes alongside the behavioural formulation outlined above.
Within the assessment, attention was paid to how Mr C has historically coped with stressful events, and he described a tendency to ‘withdraw and retreat’ from activities and people when faced with adversity. These insights were helpful in understanding Mr C’s current avoidance patterns, as he described short-term relief and comfort when spending time on the sofa yet recognised this was not adaptive in the longer term.
In summary, Mr C’s presentation appeared linked to several stressful life events and role transitions, which were maintained by behavioural and cognitive processes that are known to exacerbate depression.
Course of therapy
Treatment rationale
National Institute for Health and Care Excellence (NICE) guidelines state treatment of a moderate to severe depression episode can involve individual CBT or BA (National Institute for Health and Care Excellence, 2022). Individual BA is recommended if the person’s depression results in social withdrawal and if inactivity increases (National Institute for Health and Care Excellence, 2022). Based on Mr C’s presentation and formulation, BA was deemed the most appropriate treatment.
Session outline
The BA intervention consisted of 12 weekly sessions and was guided by relevant treatment protocols (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001; Richards et al., Reference Richards, Rhodes, Ekers, McMillan, Taylor, Byford, Barrett, Finning, Ganguli, Warren, Farrand, Gilbody, Kuyken, O’Mahen, Watkins, Wright, Reed, Fletcher, Hollon and Woodhouse2017). The following sections provide a summary of the session content, difficulties encountered and adaptations made.
-
Co-construction of a formulation and BA psychoeducation (sessions 1–3) – specific examples were identified where Mr C felt depressed and the subsequent impact on his behaviour was explored. Psychoeducation and socialisation were provided around the ‘vicious cycle’ of depression, the BA model and the importance of activity monitoring to address low mood. The formulation highlighted how Mr C’s avoidance behaviour (which included protracted periods of time on his sofa) was reinforced due to this providing feelings of physical comfort (positive reinforcement) and enabling him to avoid unpleasant emotions that occurred within social situations due to his memory problems (negative reinforcement). Rumination and avoidance were conceptualised as learned habits that needed to be addressed to improve Mr C’s mood and self-esteem. The BA model was also useful in highlighting how Mr C’s retirement led to reduced exposure to positive reinforcers as well as noting the contribution of post-exercise fatigue in negatively reinforcing avoidance patterns (due to Mr C resting to avoid feeling muscle aches or pains but also becoming self-critical about his reduced fitness stamina).
-
Identifying meaningful activities (sessions 4–5) – an activity list was developed to agree tasks that would enable Mr C to achieve pleasure, achievement and social connection. These activities were suited to Mr C’s physical health ability to aid with adaptation of BA.
-
Activity monitoring and functional analysis (sessions 4–9) – during this phase, sessions began with reviewing Mr C’s weekly activity monitor and calculating the percentage of time spent on the sofa and engaging with activities during his waking hours. Functional analysis was used to identify avoidance patterns (negative reinforcement), and this was achieved using the TRAP/TRAC method (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001; Richards et al., Reference Richards, Ekers, McMillan, Taylor, Byford, Warren, Barrett, Farrand, Gilbody, Kuyken, O’Mahen, Watkins, Wright, Hollon, Reed, Rhodes, Fletcher and Finning2016); ‘T’ involved identifying triggers for unhelpful behaviours, ‘R’ involved the response (such as low mood or critical thoughts) and ‘AP’ was the avoidance pattern which typically involved Mr C retreating to the sofa. This highlighted clear examples of negative and positive reinforcement. For example, when retreating to the sofa, this was positively reinforced as Mr C spent time listening to music alone (addition of a stimulus). However, this was also negatively reinforced as Mr C disliked visiting places alone and sought to avoid situations where memory lapses evoked unpleasant emotions (e.g. forgetting his wallet when shopping or experiencing embarrassment due to losing the thread within social interchanges). To address this, ‘AC’ involved alternative coping strategies, such as Mr C spending time in the garden instead of the sofa. Mr C was further encouraged to notice the early warning signs of rumination or avoidance patterns and engage in more adaptive behaviours such as problem-solving, approaching tasks and practising relaxation exercises.
-
Proactive scheduling of activities (sessions 5–9) – the next phase of treatment involved scheduling meaningful activities that Mr C would engage in outside of the sessions. The therapist and Mr C started slowly by initially scheduling three activities and increasing the amount each week. The therapist and Mr C collaboratively reviewed agreed targets to ensure these were personally salient and realistic. Mr C was motivated to rate his achievement and pleasure associated with agreed activities, which helped to clarify the most helpful tasks for improving his mood. Activities were also adapted to ensure they met Mr C’s physical needs: for example, although Mr C wanted to cycle for extended periods, a shorter duration was agreed as more appropriate given his fitness levels and the role of post-exercise fatigue in maintaining avoidance.
-
Targeting unhelpful thinking patterns (sessions 9–11) – as Mr C reported experiencing self-critical thoughts and rumination, this was a necessary treatment focus that is often required within BA interventions (Richards et al., Reference Richards, Rhodes, Ekers, McMillan, Taylor, Byford, Barrett, Finning, Ganguli, Warren, Farrand, Gilbody, Kuyken, O’Mahen, Watkins, Wright, Reed, Fletcher, Hollon and Woodhouse2017). Second-wave CBT was utilised during this phase to help tackle self-critical thoughts and ruminative processes (Beck, Reference Beck1976). Second-wave CBT was used due to its emphasis on one’s thoughts and the role they play on emotion and behaviour. It became clear during discussion with Mr C that his thoughts and interpretation of events were negatively impacting him. Socratic questioning and guided discovery were used to identify the most affect-laden cognitions and the therapist helped Mr C develop compassionate statements he could say to himself when he noticed such thoughts.
-
Therapy blueprint and endings (sessions 11–12) – a therapy blueprint was collaboratively created. This involved identifying triggers to Mr C’s current depressive episode, revisiting the formulation, identifying factors that helped his mood, highlighting skills learnt in therapy, identifying future goals and considering how he may cope with future challenges or setbacks. The final session involved reviewing Mr C’s goals and progress as well as reflecting on endings.
Difficulties encountered
A difficulty encountered during the activity monitoring phase of therapy was that Mr C was unable to complete the activity monitor on two occasions. This left Mr C feeling frustrated and disappointed with himself, which had a counter-therapeutic effect of increasing his depressive symptoms. To overcome this, the therapist and Mr C revisited the BA formulation and rationale for using the activity diary before engaging in shared problem-solving about how to promote completion of this document. After discussing this with Mr C, it was agreed that the recording process would be simplified by making the form more visually appealing and monitoring activity over 2-hour periods (versus hourly recording). Memory strategies were used: for example, Mr C also elected to set himself reminders to prompt him to complete the activity monitor at set points throughout the day, which helped increase his engagement with this homework task.
Adaptations to therapy
Neurocognitive adaptations
Based on recommendations from the literature (Pasterfield et al., Reference Pasterfield, Bailey, Hems, McMillan, Richards and Gilbody2014; Todd and Smith, Reference Todd, Smith, Yeates and Ashworth2020), adaptations were made to assist with delivering BA with Mr C. Given Mr C’s diagnosis of MCI, the therapist provided a summary of the previous session at the beginning of each meeting and ensured there was adequate time left at the end of sessions to clarify key insights and agreed actions. Information was provided in small, manageable chunks and the therapist regularly checked Mr C’s understanding of the topics discussed. Behavioural techniques were emphasised to reduce neurocognitive load, hence BA was chosen rather than ‘pure CBT’. Mr C also benefited from having copies of therapy session recordings and Post-it notes to help remind him to complete his activity diary. While BA intervention treatment protocols (e.g. Jacobson et al., Reference Jacobson, Martell and Dimidjian2001) recommend between-session telephone contact to encourage homework compliance, it was agreed that between-session calls would be cognitively demanding for Mr C due to his MCI diagnosis. Instead, the therapist and client were able to implement strategies to overcome obstacles with activity monitoring as discussed earlier. Finally, written copies of key information discussed in therapy (such as the formulation diagram and core concepts such as TRAPs and TRACs) were provided to Mr C to support his understanding.
General and physical adaptations
Mr C was further encouraged to provide summaries of his own understanding of core concepts and homework tasks. Handouts were simplified and provided in bigger font to help Mr C feel less overwhelmed about reading or completing these. Scheduled activities were tailored to Mr C’s physical abilities to ensure these were realistically achievable and did not reinforce unhelpful patterns of inactivity linked to post-exercise fatigue. This was important because Mr C tended to set himself challenging targets that could have easily resulted in an experience of failure and increased self-criticism.
Outcomes
Over the course of treatment, Mr C’s PHQ-9 score improved from 12/27 to 3/27 at the end of therapy (see Fig. 2). The final score indicates ‘minimal depression’ and is below the clinical threshold for depression on the PHQ-9. A 5-point change in PHQ-9 score is deemed clinically significant and a score below 5 represents remission (Kroenke, Reference Kroenke2012; Kroenke et al., Reference Kroenke, Spitzer, Williams and Löwe2010). This suggests Mr C had a clinically significant change in depression and was in remission. There was a gradual reduction in Mr C’s PHQ-9 score each week, but there was a spike during session 7. The therapist hypothesised this was because Mr C struggled to complete the activity monitor that week, leading to a temporary increase in his depressive symptoms.
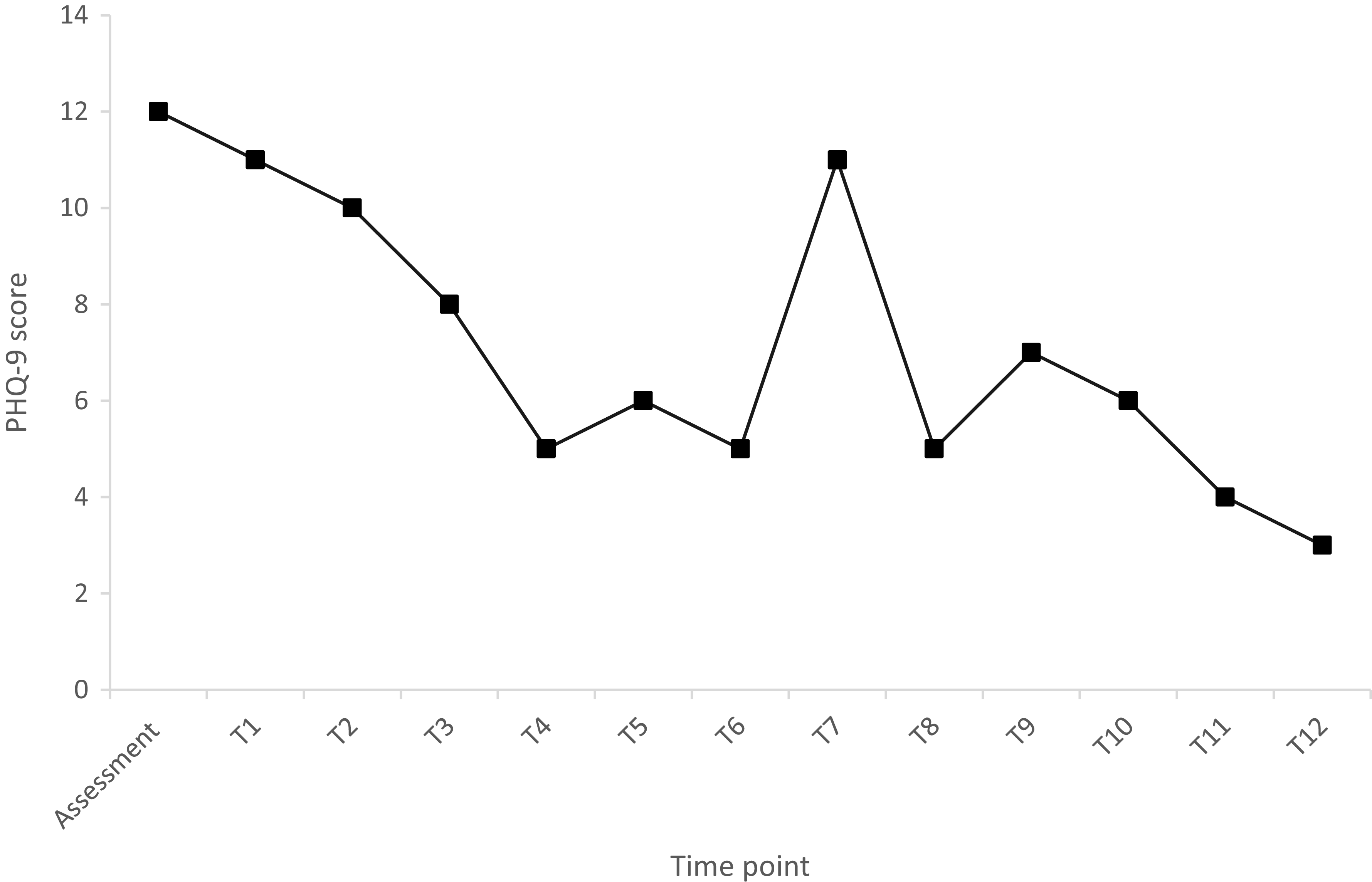
Figure 2. Change in PHQ-9 score.
Scores on the CORE-10 decreased by 16 points (from 23/40 to 7/40) over the course of treatment. This indicates a significant improvement in Mr C’s psychological distress (‘low’ distress following treatment versus ‘moderate to severe’ distress at baseline). A 6-point change in CORE-10 score is deemed clinically relevant, which indicates Mr C had a clinically significant change in psychological distress (Barkham et al., Reference Barkham, Bewick, Mullin, Gilbody, Connell, Cahill, Mellor-Clark, Richards, Unsworth and Evans2013).
Through activity monitoring, the therapist calculated the percentage of time Mr C spent on the sofa and engaging with activities at the start and end of therapy. This analysis revealed a decrease in the percentage of waking hours spent on the sofa from 63% to 45%. Furthermore, there was an increase from 20% to 42% in the percentage of Mr C’s waking hours spent engaging with agreed meaningful activities.
On a subjective level, Mr C reported feeling much better at the end of therapy and stated that his depression was ‘cured’. He articulated a sense of pleasure and achievement from reconnecting with hobbies, increasing his physical activity levels and spending more quality time with his wife. Mr C was able to achieve his goals. In particular, he reduced the time spent on the sofa, was able to engage in spontaneous activities (such as going for unscheduled bike rides) and reported getting his ‘old life back’ due to completing meaningful pursuits. Mr C was motivated throughout treatment, which was evident by him attending all sessions on time and his engagement with homework tasks.
Repeat neurocognitive screening
In addition to the psychological and self-report outcomes, a repeat ACE-III was administered 1 year after his initial assessment. Mr C’s scores remained static over this period (repeat ACE-III score of 88/100) and there was no progression of his MCI. Mr C reported that his depressive symptoms had improved, which he attributed to psychological treatment.
Discussion
The focus of this case study was addressing Mr C’s depression using BA and providing a single-case illustration of adapting BA within an older adult population, with neurocognitive impairment present. Outcome measures and subjective feedback indicated that Mr C’s depression and psychological distress greatly improved as a result of the therapeutic intervention, which was related to an increase in positively reinforcing activities and a decrease in negative reinforcers. These results affirm previous research (e.g. Orgeta et al., Reference Orgeta, Brede and Livingston2017) suggesting that BA is effective in reducing depressive symptoms in older people. This case study adds to the literature by identifying appropriate adaptations that can be helpful when delivering BA with an older adult with depression and co-occurring MCI.
Using behavioural theory to formulate and treat Mr C’s difficulties appeared to be effective and appropriate in treating his depression. More specifically, this approach enabled Mr C to recognise how an increase in negative reinforcers and decrease in positive reinforcers was maintaining his low mood. This enabled him to recognise the importance of proactively scheduling and completing meaningful activities to feel better, which is in accordance with BA principles.
An important finding was that Mr C’s scores on neurocognitive screening tests (ACE-III) remained static following BA treatment. Given the association between amnestic MCI and dementia (Albert et al., Reference Albert, DeKosky, Dickson, Dubois, Feldman, Fox, Gamst, Holtzman, Jagust, Petersen and Snyder2011), it was positive that Mr C’s memory difficulties remained stable after targeting reversible factors (in his case, depression). Furthermore, psychological therapy encouraged Mr C to modify lifestyle factors and his physical activity levels greatly increased. Given evidence suggesting a positive impact of exercise on MCI (e.g. Suzuki et al., Reference Suzuki, Shimada, Makizako, Doi, Yoshida, Ito, Shimokata, Washimi, Endo and Kato2013), this may have also influenced Mr C’s static scores on screening tests. Taken together, this case study supports the use of BA for older adults with depression and co-occurring MCI. This emphasises the need to consider therapy with older adults with neurocognitive impairment, as significant gains appear possible when interventions are appropriately selected and adapted.
Limitations from this case study arise. Firstly, the intervention pertains to a single case and the conclusions drawn may not generalise to other older adults with different presentations. Secondly, as Mr C was taking anti-depressants alongside therapy, it is difficult to conclude that the effects shown were solely attributable to the BA treatment. On balance, the combination of both medication and psychological intervention likely enabled the improvements seen in Mr C’s mood. Lastly, the goals developed could have been more specific and measurable. For example, the goal of reducing the amount of time spent on the sofa could have been enhanced by asking Mr C the percentage decrease he would like to obtain (for example, reducing time spent on the sofa by 20%) and stating a clear time frame to achieve this target. This limits the evaluation of outcomes in this case because the therapist was unsure whether the amount of time Mr C reduced on the sofa (18% reduction) was a meaningful achievement for Mr C. However, Mr C’s feedback indicated he was happy with the progress made in relation to this goal.
Alternative methods could have been utilised to enrich Mr C’s treatment. For example, during activity scheduling, graded task assignments could have been used to break down the activities into manageable components to help Mr C engage with them (Jacobson et al., Reference Jacobson, Martell and Dimidjian2001). With hindsight, this may have improved Mr C’s initial cooperation with homework tasks and increased his motivation to complete the activity monitor. However, this was difficult to achieve due to the therapist’s limited time on placement and Mr C still made good progress in achieving scheduled tasks despite the use of graded task assignments.
The adaptations made to BA for Mr C appeared to be effective; particularly in relation to his physical and neurocognitive abilities. Like many individuals, Mr C demonstrated a tendency to over-estimate what he could achieve, although therapy discussions were helpful in identifying a ‘just right’ challenge for him to complete. Negotiation of realistic targets was an important aspect of therapy with Mr C, and this may require particular consideration when delivering BA interventions with older people. Neurocognitive adaptations were important for increasing Mr C’s engagement in therapy as they appeared to promote his understanding of core concepts and improved his homework compliance. Overall, this case study suggests that BA with adaptations is an effective intervention to help treat depression in older adults with MCI.
Key practice points
-
(1) It is important to consider the role of cognitive impairment when treating depression to help identify useful adaptations to treatment protocols to support successful therapy delivery.
-
(2) BA is a promising approach for treating depression and co-existent MCI in older adults. Interventions should specifically target behavioural contingencies associated with neurocognitive difficulties (for example, avoidance being negatively reinforced and maintained due to individuals experiencing aversive emotional reactions to cognitive lapses when socialising).
-
(3) Neurocognitive adaptations for BA for depression and co-occurring MCI include offering frequent summaries, using memory aids (such as Post-it note reminders to help complete activity monitoring and other associated homework tasks) and providing information in small, manageable chunks to reduce neurocognitive load.
Data availability statement
Data availability is not applicable to this article due to the data pertaining to a single case and therefore to help maintain anonymity.
Acknowledgements
The authors would like to thank Mr C for his consent and being courageous to allow us to submit the case study for publication to help inform other therapists about the use of behavioural activation in the treatment of depression and MCI for older adults.
Author contributions
Saarim Aslam: Conceptualization (equal), Investigation (lead), Methodology (equal), Project administration (lead), Resources (lead), Visualization (equal), Writing - original draft (lead), Writing - review & editing (equal); Katy Lee: Conceptualization (equal), Investigation (supporting), Methodology (equal), Project administration (supporting), Resources (supporting), Supervision (lead), Writing - original draft (supporting), Writing - review & editing (equal).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The authors declare none.
Ethical standards
This case study complies with the ethical principles of psychologists and code of conduct as set out by the BABCP and BPS. Verbal and written informed consent were obtained from Mr C to submit this case report for publication.





Comments
No Comments have been published for this article.