Introduction
Post-traumatic stress disorder (PTSD) is a long-term mental health problem associated with high disability and poor wellbeing outcomes (Watkins et al., Reference Watkins, Sprang and Rothbaum2018). It is unlikely to remit spontaneously, but has very good recovery rates (over 75%) when treated in specialist services (Ehlers et al., Reference Ehlers, Clark, Hackmann, McManus, Fennell, Herbert and Mayou2003; Ehlers et al., Reference Ehlers, Hackmann, Grey, Wild, Liness, Albert, Deale, Stott and Clark2014). In the UK, first-line treatment for PTSD is within NHS Talking Therapies (NHS TT) services, where unfortunately it fares less well. NHS TT services show an average PTSD recovery rate of 37.8%, and as low as 15–20% in some services (Health and Social Care Information Centre, 2016; Murray, Reference Murray2017). This is notably lower than the overall NHS TT recovery rates of 50–60% across all disorders (Layard, Reference Layard2009). More recent data from 2019–2020 gives a UK-wide recovery rate of 42.2% for PTSD (Health and Social Care Information Centre, 2020), although this is only for individuals who completed treatment – so the overall recovery rate is likely to be lower.
NHS TT services are tasked with implementing NICE guidelines. As such, NHS TT services currently treat PTSD with either trauma-focused cognitive behavioural therapy (tfCBT) or eye-movement desensitisation and reprocessing (EMDR) – both evidence-based treatments (NICE, 2018). Data from 2021–2022 (NHS England Digital, 2022) indicate that in England the recovery rate following CBT for PTSD was 40.4%, with 61.8% of individuals showing reliable improvement, across 24,452 completed courses of therapy. Over the same period, the recovery rate for EMDR was 45.9% (63.1% improvement) across 5083 completed courses of treatment.
NICE guidelines (2018) identify four categories of trauma-focused CBT: prolonged exposure, cognitive processing therapy, cognitive therapy for PTSD (CT-PTSD), and narrative exposure therapy (NET). In the service described by the current study, and more generally in NHS TT services, the most prevalent of these tfCBT interventions is CT-PTSD, the treatment model based on Ehlers and Clark’s (Reference Ehlers and Clark2000) cognitive model of PTSD.
EMDR was originally developed based on clinical observations (Shapiro, Reference Shapiro2001) and has a less-established theoretical basis, although research has offered a number of potential cognitive explanations of the treatment, particularly with regard to mental imagery and working memory (Astill Wright et al., Reference Astill Wright, Horstmann, Holmes and Bisson2021; Holmes et al., Reference Holmes, James, Coode-Bate and Deeprose2009).
An early meta-analysis of studies directly comparing CBT and EMDR found that both were effective treatments for PTSD, with no grounds to favour either (Seidler and Wagner, Reference Seidler and Wagner2006). This – together with a relative lack of current evidence as to which individuals might find CBT or EMDR more effective (Shapiro, Reference Shapiro2012) – means it can be difficult to determine when each form of therapy should be used for specific individuals and groups. Current clinical recommendations only state that the choice of treatment be based on the client’s preference (NICE, 2018).
More recent meta-analyses have sought to further clarify the magnitude of treatment effects for CBT and EMDR in PTSD. A systematic review following Cochrane Collaboration guidelines found both tfCBT and EMDR to be well-supported and effective PTSD treatments, with less support for non-trauma-focused CBT (Lewis et al., Reference Lewis, Roberts, Andrew, Starling and Bisson2020). The network meta-analysis of PTSD trials which underlies the NICE guidelines (Mavranezouli et al., Reference Mavranezouli, Megnin-Viggars, Daly, Dias, Welton, Stockton, Bhutani, Grey, Leach, Greenberg, Katona, El-Leithy and Pilling2020) found ‘no evidence of differential effects between EMDR and other treatments’.
Khan et al. (Reference Khan, Dar, Ahmed, Bachu, Adnan, Kotapati, Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018) report a meta-analysis including 11 studies directly comparing CBT and EMDR, finding that EMDR performs better than CBT in reducing PTSD-specific and anxious symptoms, although the two forms of therapy did not differ in reducing depressive symptoms. A subset of four studies with follow-up after 3 months no longer showed any differences between the treatment modalities, although both remained effective. It is worth noting that the studies reviewed by Khan et al. (Reference Khan, Dar, Ahmed, Bachu, Adnan, Kotapati, Khan, Dar, Ahmed, Bachu, Adnan and Kotapati2018) used heterogeneous CBT protocols across studies – primarily (prolonged) exposure – with only one of the included studies being designated by the authors as using tfCBT (Jaberghaderi et al., Reference Jaberghaderi, Greenwald, Rubin, Zand and Dolatabadi2004, which showed no differences in treatment outcome between tfCBT and EMDR).
In summary, both tfCBT and EMDR have been shown in previous studies to be effective treatments for PTSD, which would support the NICE guideline recommendations that a choice of either is acceptable as first-line treatment for PTSD.
NHS TT recovery rates are based on composite measures which include anxious and depressive symptom scores, employed transdiagnostically across a range of disorders (Clark, Reference Clark2018; Gyani et al., Reference Gyani, Shafran, Layard and Clark2013). For PTSD, these recovery criteria (National Collaborating Centre for Mental Health, 2023) require symptom scores to decrease below clinical threshold on both a PTSD-specific questionnaire (the PCL-5 or IES-R) and a depression questionnaire (the PHQ-9). Binary indicators are helpful for determining service-level patterns in recovery, and in facilitating comparisons across different problems that people might be treated for in NHS TT services. However, collapsing across measures of PTSD symptoms and depression into a single ‘recovery’ measure may lose some detail regarding the nature of changes over the course of treatment for PTSD. Improved understanding of the presence, absence or extent of differential effects of PTSD-focused treatments across a range of symptom measures may stand to better inform services’ treatment planning.
On the basis of this background information, this service evaluation seeks to determine overall recovery rates for PTSD in a London NHS TT service, and how these may have changed over time. It will provide further detail regarding this question by examining symptom change scores across a range of symptom measures in addition to using binary recovery outcomes. Furthermore, this evaluation aims to compare the relative effectiveness of CBT (namely, CT-PTSD as implemented in this NHS TT service) and EMDR for treating PTSD.
By obtaining a better understanding of outcomes from each treatment modality in the service, clinicians will be able to better inform clients about treatment choice. Additionally, far fewer clinicians are trained in EMDR than tfCBT/CT-PTSD in the service. This is representative of the wider picture in UK mental health services (Farrell and Keenan, Reference Farrell and Keenan2013); a recent nationally funded programme (Health Education England, 2022) has aimed to increase the numbers of clinicians within mental health services who are trained in EMDR commensurate with the recently developed NHS EMDR curriculum (Health Education England, 2021) and EMDR competence framework (Roth et al., Reference Roth, Dudley and Pilling2020). Clarifying potential differences in who may benefit most from different treatment modalities will allow for better-informed service-level planning of clinician resources and clinical pathways.
Aims
-
To examine recovery rates for PTSD treatment in the service over time.
-
To compare recovery and symptom change for individuals with PTSD seen by the service across a range of symptom measures, including PTSD-specific symptom measures.
-
To determine whether there is any difference in effectiveness of treating PTSD in an NHS TT setting with CT-PTSD compared with EMDR.
Method
Sample
The current study took place in a London NHS TT service and consisted of a set of retrospective analyses of routinely collected data.
The IAPTUS interface was used to download all available recorded data of individuals treated for PTSD in the service. This gave 11 years of data between 2012 and 2023. All individuals whose data were used in these analyses had provided consent to their data being used for service evaluations. Downloading all available data for the service (as of May 2023) for individuals who had originally been given the IAPTUS problem descriptor of ‘post-traumatic stress disorder’ yielded a sample size of N=1696. Individuals whose problem descriptor was subsequently changed within the same treatment episode (e.g. to depression, health anxiety, etc.) were excluded from analyses, leaving a total sample size of N=1580.
Implementing CT-PTSD and EMDR in the service
All therapists delivering interventions in the service were either BABCP-accredited CBT practitioners (predominantly high-intensity CBT therapists or clinical psychologists), or trainees working towards these accreditations, supervised by BABCP-accredited supervisors. Therapists in the service who provided EMDR had additional specialist supervision from an EMDR accredited practitioner once per month, focused on PTSD cases. Other PTSD cases, who received tfCBT (namely, CT-PTSD), would be taken by therapists to their weekly supervision with their CBT supervisor. Therapists in the service would typically have more CBT cases than EMDR, so on balance cases should have received a similar amount of supervision regardless of treatment approach.
Service users included in the study were assigned a problem descriptor of PTSD via the triage system implemented in NHS TT services. Allocation to tfCBT or EMDR treatment was predominantly made on the basis of client choice, although it is also the case that clinicians in the current service may decide to explore EMDR as a possibility if the client has had tfCBT before. However, it was not possible to investigate this systematically with the data available.
Measures
Treatment outcomes were determined from the symptom measures below. ‘First’ or pre-treatment scores were recorded at the earliest point of contact that an individual completed the respective treatment measure. ‘Last’ scores were taken from the final treatment session where possible, otherwise they were taken from the final completed measure prior to an individual’s last treatment session. A small number of individuals in the dataset received follow-up reviews 1–3 months after ending treatment. To facilitate comparison between individuals in the dataset, final symptom measures used for treatment outcomes were taken from the final treatment session for all individuals rather than at follow-up.
PHQ-9 and GAD-7
All individuals seen in the service agree to complete weekly measures of depressive and anxious symptoms, indexed by the PHQ-9 and GAD-7 questionnaires, respectively (Gyani et al., Reference Gyani, Shafran, Layard and Clark2013). Both questionnaires use Likert-like ratings (ranging 0–3) to indicate the frequency of a range of symptoms over the past 2 weeks, and have been chosen for use in NHS TT services due to their well-documented reliability and validity, as well as being quick and relatively easy to complete (Kroenke et al., Reference Kroenke, Spitzer and Williams2001; Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006). The PHQ-9 ranges from 0 to 27, with a score of 10 used as a clinical threshold for depression, and ±6 points on the measure being taken as reliable change. The GAD-7 ranges from 0 to 21, with a score of 8 used as a clinical threshold, and ±4 points on the measure being taken as reliable change (National Collaborating Centre for Mental Health, 2023).
PTSD symptoms
Service users routinely completed PTSD symptom measure scores: either the PTSD Checklist for DSM-5 (PCL-5) or the Impact of Event scale-Revised (IES-R). Guidelines in the current service have shifted over the past 10 years from recommending use of the IES-R to use of the PCL-5, which is the currently recommended questionnaire for PTSD symptoms across NHS TT services (National Collaborating Centre for Mental Health, 2023). As a result, in the current dataset earlier treatment cases are more likely to have used the IES-R and later cases are more likely to use the PCL-5, which makes interpretation of findings more difficult.
PCL-5
The PCL-5 is a 20-item measure of distress due to PSTD symptoms (Weathers et al., Reference Weathers, Litz, Keane, Palmieri, Marx and Schnurr2013). Items are rated on 5-point Likert-like scales from 0 (not at all bothered/distressed) to 4 (extremely bothered/distressed), with total scores ranging from 0 to 80. A score of 32 or above indicates clinical caseness, and a change of ≥10 is taken to be indicative of reliable change (National Collaborating Centre for Mental Health, 2023).
IES-R
The IES-R is a 22-item measure of how bothered or distressed individuals are due to PTSD symptoms (Christianson and Marren, Reference Christianson and Marren2012), with each item rated on 5-point Likert-like scales from 0 (not at all) to 4 (extremely). Scores range from 0 to 88, with scores of 33 or above taken to indicate PTSD caseness.
Recovery
The data as downloaded from IAPTUS contained a binary indication of whether any given individual was recovered by the end of an individual treatment episode. According to NHS TT guidelines, this status should indicate PHQ-9 scores below 10 and a PCL-5 score below 32, or IES-R score below 33 (depending on which PTSD symptom measure was used). These IAPTUS-generated binary scores of recovery status by the end of treatment are used in Tables 2 and 3.
Table 1. Sample characteristics for the full sample (N=1580), as well as separately for service users who received CBT (namely CT-PTSD, n=794) and those who received EMDR (n=155)
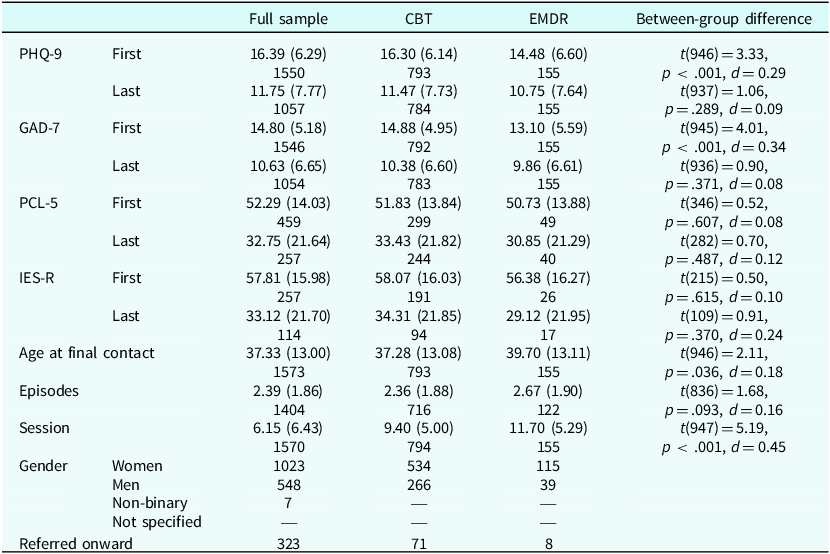
Scores are given as means (SD), with the bottom number in each cell giving the total number of valid datapoints (i.e. count) for that measure/figure. For example, the mean number of treatment sessions attended across the whole sample is 6.15 with an SD of 6.43, and these data are available for 1570 individuals in the sample.
NB. Specific numbers of individuals are not reported in cells where this figure would be <6, in order to prevent identification of specific individuals in line with Caldicott principles.
Table 2. Referral data and PTSD recovery rates (based on NHS TT criteria) broken down by year

Each cell gives the percentages of valid cases (i.e. where data were present), and absolute number of cases that this percentage represents. Cell counts of <6 are not reported, to prevent possible identification of individuals.
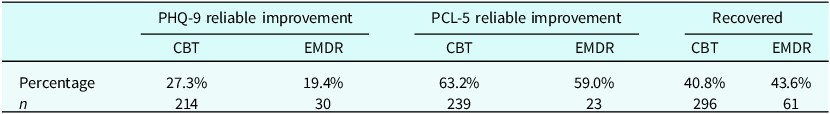
Table 3. Percentage recovery rates and reliable improvement (of valid/present data – based on NHS TT recovery criteria for PTSD) and their respective count data for CBT and EMDR treatment
Demographics
IAPTUS data contained self-reported gender, date of birth, last contact date, treatment modality, and total number of episodes of treatment with the service (which includes treatments for non-PTSD problems, as well as one-off community workshops and employment support as separate treatment instances). Each treatment instance for PTSD was recorded as a separate row in the dataset and given an individual participant code – so individuals who were treated multiple times for PTSD by the service occurred multiple times in the dataset. Sample characteristics are given in Table 1.
Number of treatment sessions was recorded for each treatment instance. This number of sessions excluded the individual’s initial triage(s) with the service, and so started with the first treatment session. Total number of sessions was recorded up to the final session for the recorded treatment modality.
Results
Descriptive statistics are given in Table 1.
In addition to 1:1 CBT (namely, CT-PTSD, n=794) and EMDR (n=155), service users had received a number of other treatments: counselling (n=15), computerised CBT (n=6), group CBT (n=5), NET (n<6), dynamic interpersonal therapy (DIT) (n<6), or a wellbeing workshop (n<6). A further 585 individuals received no treatment – either due to not attending sessions, being referred onto other services, declining treatment, or not being found suitable for the service. The ‘referred onward’ count in Table 1 includes all individuals formally referred to another service – this includes individuals referred onwards after completing therapy, after early termination of planned therapy, or those referred onwards after an initial triage/assessment with the current service.
Individuals who received CBT had significantly higher pre-treatment PHQ-9 and GAD-7 scores than those who received EMDR. The CBT group were also significantly younger than the EMDR group by a small margin. On average, individuals who received EMDR completed significantly more sessions of therapy than those who received CBT; this figure is inclusive of all individuals in both groups who did not complete a course of treatment.
Recovery
Recovery rates across a range of measures are shown in Table 2 (for the sample as a whole) and Table 3 (broken down across CBT/EMDR treatments). Table 3 also gives proportions of the sample of individuals who received CBT versus EMDR who showed reliable improvement in depression and PTSD symptoms. All indices of recovery and reliable change are taken from NHS TT guidelines (National Collaborating Centre for Mental Health, 2023).
Chi-squared tests indicated that the recovery rates in Table 3 did not differ significantly between those who received CBT versus EMDR: χ2(1)=0.32, p=.575, nor did the proportions of individuals who showed reliable improvement in PTSD symptoms as indexed by the PCL-5 across the treatment modalities: χ²(1)=0.25, p=.615. However, the two groups did differ significantly in the proportion of individuals who showed reliable improvement in depression symptoms, with a greater proportion of individuals receiving CBT showing reliable improvement in PHQ-9 scores than those receiving EMDR: χ²(1)=4.24, p=.039.
Symptom changes
Table 4 shows the proportion of the sample who showed (reliable and non-reliable) improvement or deterioration for each of the measures where there are published NHS TT reliable change indices (namely the PHQ-9, GAD-7 and PCL-5).
Table 4. Proportions (counts given on the bottom line of each cell) of individuals who showed reliable improvement or deterioration, or improvement/deterioration below the reliable change threshold for that measure (or no change) for individuals receiving CT-PTSD, EMDR and across the whole sample
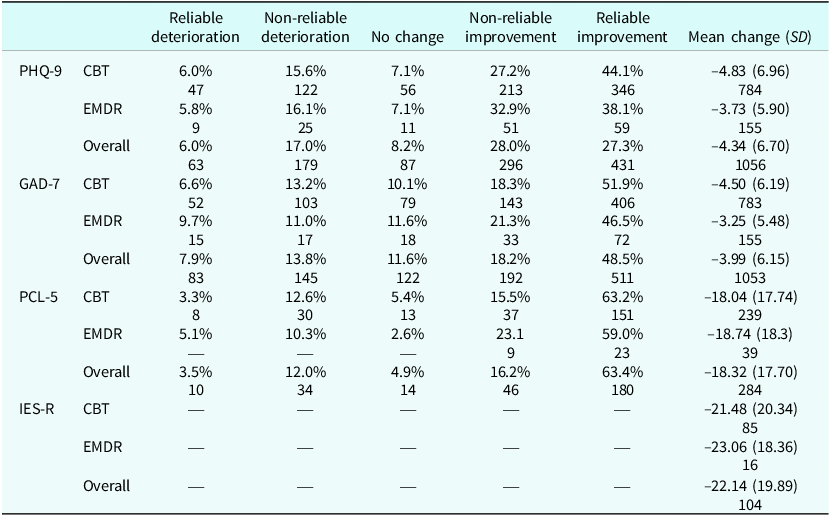
NB. Reliable change thresholds were ±6 for the PHQ-9, ±4 for the GAD-7 and ±10 for the PCL-5. Mean change gives the difference between first and last score for each measure (for individuals in the sample with both of these scores), with negative scores indicating a reduction in symptoms. Specific cell counts are not reported for counts <6, to prevent identifiability of participants.
A set of mixed ANOVAs were run to examine any differences in symptoms at baseline and treatment outcome between service users receiving CBT versus EMDR. Four ANOVAs were conducted – one for each treatment outcome measure (PHQ-9, GAD-7, PCL-5, IES-R). Each ANOVA included time (first score/pre-treatment; last score/post-treatment) as a 2-level within-subjects factor and treatment type (CBT, EMDR) as a 2-level between-subjects factor.
Tab le 5 shows that all four symptom measures improved significantly over time (i.e. from pre- to post-treatment). There was no main effect of treatment type or treatment×time interaction for either the IES-R or PCL-5 measures of PTSD symptoms. There were main effects of treatment for both GAD-7 and PHQ-9 measures, as well as a significant time×treatment interaction for GAD-7 and a trend level time×treatment interaction for PHQ-9 scores in the same direction (see Table 1 for means and SDs). These effects indicate larger changes in anxious and depressive symptoms for individuals who received CBT (compared with EMDR) – but this is confounded by the fact that PHQ-9 and GAD-7 scores were significantly higher in the CBT group pre-treatment.
Table 5. ANOVA output comparing outcome scores across time (pre-/post-treatment) and treatment (CBT, EMDR)
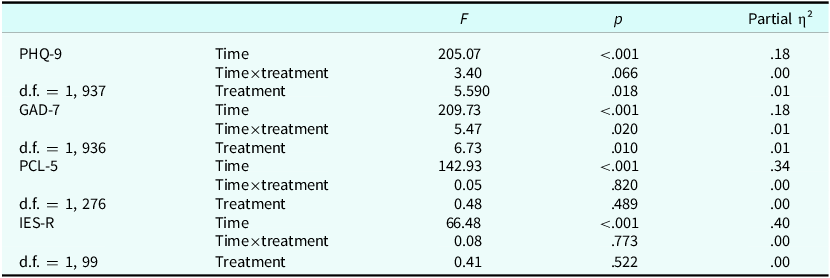
All ANOVAs were repeated as ANCOVAs, including age and gender (coded as a binary variable: woman/not-woman) as covariates. Including these covariates did not change any effects reported above, or lead to any new interaction, with the exception of a time×gender interaction for IES-R scores exclusively, such that men and non-binary people showed smaller reductions in IES-R scores than women: F(1,97)=5.94, p=.017, partial η²=0.06; MeanWomenT1=57.16 (SD=15.59), MeanNonWomenT1=59.03 (SD=16.69), MeanWomenT2=30.29 (SD=20.23), MeanNonWomenT2=39.51 (SD=23.77).
Age and gender both showed main effects in ANCOVAs for PHQ-9 scores F Gender(1,934)=23.06, p<.001, partial η²=0.02, F Age(1,934)=5.68, p=.017, partial η²=0.01; and for GAD-7 scores F Gender(1,933)=15.75, p<.001, partial η²=0.02, F Age(1,933)=6.42, p=.011, partial η²=0.01. The direction of these effects suggested that older age and male or non-binary genders are associated with higher PHQ-9 and GAD-7 scores at all time points.
Discussion
Comparing CT-PTSD and EMDR
When looking at recovery as a binary measure (i.e. recovered/non-recovered) there was no difference between CBT (namely, CT-PTSD) and EMDR. ANOVAs found no difference between CBT and EMDR in the extent to which either changed PTSD-specific symptom scores (indexed by the PCL-5 and IES-R), despite the CBT group having higher levels of anxiety and depression than the EMDR group at the start of treatment. CBT led to larger changes in anxious and depressive symptoms than EMDR; however, this is confounded by these higher anxiety and depression scores at start of treatment for the CBT group. A significant time×treatment interaction provides some indication that CBT (relative to EMDR) led to greater reductions in anxious symptoms, but this difference is less clear for depressive symptoms as that interaction was a non-significant trend – and both interactions had very small effect sizes. A follow-up analysis of this service evaluation comparing individuals who received EMDR with a sub-sample of service users who received CBT matched on initial anxiety and depression scores might stand to better inform any conclusions about the degree of change here.
The fact that individuals receiving EMDR in the service initially presented with lower anxiety and depression scores than individuals who went onto receive CBT is a finding worth highlighting in itself, especially as the two groups did not show any differences in PTSD symptoms at start of treatment. Given that allocation to CBT or EMDR in the service is made on the basis of personal preference (NICE, 2018), one possibility is that individuals in the EMDR group had spent more time researching treatments or have a different mindset in approaching therapy that is associated with lower subjective difficulties in mood or anxiety. In any event, the difference in anxious and depressive symptoms between these treatment groups at start of treatment is worth taking into account with service planning. For example, if clinicians know that there is likely to be variation in anxious and depressive symptoms at start of treatment that is not directly predicted by severity of PTSD symptoms, this may better inform decisions around initial stages of treatment (e.g. the duration or need for stabilisation or life-reclaiming work), particularly for clients receiving tfCBT such as CT-PTSD.
It is also worth noting that EMDR training may be longer than CBT practitioners’ baseline training in tfCBT – typically 3–6 days, compared with 2 days for most of the therapists. As such, EMDR-trained practitioners in the service may have a better understanding of treating PTSD and trauma. Some practitioners in the service have received the NHS TT top-up training for tfCBT, but this only began in 2020 while data collection started in 2012. More significantly perhaps, EMDR practitioners received specialist supervision for their EMDR practice, while those offering CBT had the supervision of their PTSD cases within generic supervision.
Overall recovery
Recovery rates across all measures at first glance appeared to increase from 2012 to 2018, before decreasing and then levelling out (Table 2). Taking into account the lower referral numbers (and moreover, the very low completion rate of PTSD-specific symptom questionnaires) prior to 2020, the most likely interpretation is that the last few years of recovery data are more reliable due to greater and more representative numbers of clients completing symptom questionnaires.
Encouragingly, the largest symptoms changes (and highest proportions of reliable improvement) following both CBT and EMDR are shown for PTSD-specific symptom measures (Table 4). This aligns with the foci of both CBT and EMDR for PTSD upon re-experiencing symptoms of traumatic events and the distress this causes, rather than broader emotional symptoms (Ehlers and Clark, Reference Ehlers and Clark2000; Shapiro, Reference Shapiro2001). Having said this, both CBT and EMDR did lead to substantive improvements in anxious and depressive symptoms. Recovery from PTSD was comparable to national recovery rates for PTSD in NHS TT (formerly IAPT) services (Health and Social Care Information Centre, 2020; Murray, Reference Murray2017).
However, there is still a great deal of room for improvement compared with recovery rates previously found using CT-PTSD in specialist services (Ehlers et al., Reference Ehlers, Clark, Hackmann, McManus, Fennell, Herbert and Mayou2003; Ehlers et al., Reference Ehlers, Hackmann, Grey, Wild, Liness, Albert, Deale, Stott and Clark2014), suggesting that there may be wider issues in how PTSD is treated in NHS TT services, or the appropriateness of referrals to these services. Recent research has sought to better understand the processes of effective treatment for PTSD – CT-PTSD in particular (Wiedemann et al., Reference Wiedemann, Janecka, Wild, Warnock-Parkes, Stott, Grey, Clark and Ehlers2023). Improved understanding of the processes of change in effective treatment in NHS TT services may stand to better inform future training of clinicians and service planning in the current setting. It is also the case that more training days on PTSD in core CBT training, specialist tfCBT supervision for PTSD cases, and greater treatment length will enhance recovery rates for tfCBT in NHS TT services.
Thirty-seven per cent of individuals referred or triaged for PTSD over the past 11 years did not receive treatment in the service. Of those who did not receive treatment, 41% were formally referred to another service – i.e. over half of the people presenting to the service with PTSD or similar problems who were not deemed appropriate to be seen in the current service were not referred onwards. This could be an issue of service provision within the trust (e.g. an absence of commissioned services for individuals with needs more complex than NHS TT criteria allow), lack of clinicians’ knowledge regarding appropriate services to refer onto, or a combination of these issues as well as other factors. As such, it may be helpful for the service to conduct a complementary audit on processes of onward referral for individuals who are not seen by the service, and/or do not meet criteria for the service.
The present data also give some indication of individual differences that may be worth considering in service planning. In the current sample, older age and non-female (male or non-binary) gender were both associated with higher anxiety and depression scores. These higher anxiety and depression scores were seen at referral, so this effect could be explained as older individuals, men and non-binary people taking longer to be referred for treatment, or only doing so when they have reached a higher level of subjective distress (Boneham et al., Reference Boneham, Williams, Copeland, McKibbin, Wilson, Scott and Saunders1997; Galdas et al., Reference Galdas, Cheater and Marshall2005; Mackenzie et al., Reference Mackenzie, Gekoski and Knox2006; Pettit et al., Reference Pettit, Qureshi, Lee, Stirzaker, Gibson, Henley and Byng2017). Older adults in particular are recognised to be under-represented in NHS TT services (Clark, Reference Clark2018; Saunders et al., Reference Saunders, Buckman, Stott, Leibowitz, Aguirre, John, Lewis, Cape and Pilling2021). If there is such a delay in accessing care for these groups, then it may be warranted to conduct targeted outreach to older adults, men and non-binary individuals who may be experiencing trauma-related problems – especially as research suggests that older adults actually have better outcomes from mental health treatment when they do access care (Saunders et al., Reference Saunders, Buckman, Stott, Leibowitz, Aguirre, John, Lewis, Cape and Pilling2021). However, it would be prudent to conduct follow-up audits of these smaller groups within the wider dataset before making changes to outreach, clinical policy or service provision based on findings from normative statistical analyses of a client dataset that is predominantly female and relatively young.
Given the relatively small numbers of older adults, men and non-binary people in the service, it would be feasible to conduct a case series looking at these putative effects in greater detail. With age in particular, it could be that non-linear effects may be present – for example if younger people do particularly well in treatment due to early intervention effects (cf. McGorry and Mei, Reference McGorry and Mei2018) then this could additionally give rise to the observed effects. In terms of gender, men and non-binary people show smaller reductions in IES-R scores (not any other measure) following any kind of treatment when compared with women. This may indicate relatively smaller treatment effects for this group, but the fact that this effect is not seen in more recent PCL-5 data is encouraging insofar as it could suggest that this is no longer an issue in the service, or that this IES-R specific effect was an artefact of the previously used symptom questionnaire, or another kind of false positive.
Of 1696 service users initially screened as having PTSD in the service over the past 10 years, 116 (6.8%) received treatment for a problem other than PTSD within that same treatment episode. This suggests that while the vast majority of individuals initially screened as having PTSD were screened accurately, there was a small but substantial minority who may have been screened incorrectly. This could be worth bearing in mind by the service with respect to screening and triage, and how therapists are trained to provide these. There are a wide variety of mental health problems that can be experienced by individuals who have experienced trauma or adverse experiences, and not all individuals exposed to trauma necessarily develop PTSD (Kessler et al., Reference Kessler, Aguilar-Gaxiola, Alonso, Benjet, Bromet, Cardoso, Degenhardt, de Girolamo, Dinolova and Ferry2017; Kilpatrick et al., Reference Kilpatrick, Resnick, Milanak, Miller, Keyes and Friedman2013). So even if there is clear evidence of trauma at screening or triage it may still be the case that another focus or form of treatment may end up being better suited to a given individual’s needs at that time.
Strengths and limitations
The current study used a large, comprehensive dataset of real-world interventions in an NHS setting, meaning that the results and conclusions have excellent ecological validity. From the point of view of the service evaluation, the sample used is the entire population, meaning that no statistical generalisation is needed.
That being said, current findings should not be generalised further than the service from which data were collected. Of particular relevance, all individuals who received EMDR in the sample had chosen this treatment. As such, the current findings do not and cannot allow the direct comparison of treatment modalities that is possible with a randomised controlled trial and necessary for any broader inferences about clinical efficacy.
Given this is a real-world evaluation study, it is not possible to know how closely therapists adhered to each treatment or whether there were any significant differences in the quality of the treatments delivered, or how trauma-focused each was. It is assumed that all individuals designated as receiving ‘CBT’ received CT-PTSD specifically, but without this kind of data about model adherence, this cannot be stated definitively. Future research examining the impact of how trauma-focused the treatments provided were may help clarify this question.
A key shortcoming of the current study is that it does not include details regarding race or ethnicity, as this information was not available when the routinely collected data were downloaded for the current service evaluation. This is a particular shortcoming owing to the fact that individuals from minoritised ethnic backgrounds are often under-represented in NHS TT services, despite having higher rates of PTSD than White British populations (Clark, Reference Clark2018). Similar patterns are seen in non-UK samples (Hall-Clark et al., Reference Hall-Clark, Sawyer, Golik and Asnaani2016; Roberts et al., Reference Roberts, Gilman, Breslau, Breslau and Koenen2011). Furthermore, the fact that there is limited current research available regarding the relative efficacy of EMDR or CT-PTSD, together with evidence that ethnicity affects PTSD outcomes (Asnaani and Hall-Clark, Reference Asnaani and Hall-Clark2017; Spoont et al., Reference Spoont, Nelson, Kehle-Forbes, Meis, Murdoch, Rosen and Sayer2021) makes this an especially pressing topic for future research to consider.
Allocation of individuals to treatment for PTSD was made on the basis of the NHS TT triage/assessment process; however, there was no formal assessment of the validity of these diagnoses. Accurate assessment or diagnosis of PTSD is complicated by its wide range of co-morbidities and differential diagnoses (Megnin-Viggars et al., Reference Megnin-Viggars, Mavranezouli, Greenberg, Hajioff and Leach2019), making this difficult even in specialist services (Atkinson et al., Reference Atkinson, Kristinsdottir, Lee and Freestone2024). As both CT-PTSD and EMDR are treatments specifically tailored to PTSD, any inaccuracies at the stage of assessment may influence or obscure the efficacy of these treatments as reported.
Other limitations of the study are mentioned above, namely the baseline differences in anxious and depressive symptoms between CBT and EMDR groups, and the limits to potential conclusions to be drawn about age and gender effects from normative analysis of the sample as a whole. Recommendations for follow-up analyses to address these limitations are given above and summarised below.
Analyses used in this evaluation treat all treatment episodes in the dataset as independent observations. However, there are instances where observations were non-independent – most pertinently, different PTSD treatment episodes for individuals who had more than one episode of treatment for PTSD in the service. Analyses could therefore have been improved by nesting treatment episodes within each individual in the dataset. This would be worth doing for any further analyses that wished to look more closely at multiple treatment instances. Such nested analyses might then be able to inform specific questions regarding treatment order – e.g. does an additional tfCBT or EMDR treatment episode improve outcomes for an individual who has already received one or more instances of treatment with tfCBT or EMDR, etc.
Finally, completion rates for the IES-R and PCL-5 (particularly the former) were notably lower across the sample than for the PHQ-9 and GAD-7, as the PTSD-specific measures are not mandated for completion by clinical note software in the same way as the PHQ-9 and GAD-7. This comparison can be seen in regard to overall questionnaire completion rates in Table 1. Completion rates for these questionnaires have improved in the service over time, but these still remain far lower than PHQ-9 and GAD-7 rates.
Key practice points
-
(1) In light of no difference in recovery rates between and EMDR (and the far smaller number of EMDR-trained clinicians in the service), continue using service user preference as a basis for offering CBT or EMDR for PTSD.
-
(2) PCL-5 questionnaires should be collected alongside PHQ-9 and GAD-7 for individuals being treated for PTSD in the service to allow for the best comparison of relevant treatment outcomes and the most evidence-based conclusions for future clinical data (as mandated in the NHS TT manual).
-
(3) The service may wish to consider offering training for clinicians around presenting problems and triages for individuals who have experienced trauma but may not necessarily have PTSD, or may benefit from treatment of a non-PTSD issue in the first instance.
-
(4) Clinicians in the service should be mindful of anxious and depressive symptoms (how these may present at start of treatment and change over time) when working on PTSD with individuals in the service, particularly individuals receiving tfCBT.
-
(5) Service planning may benefit from additional audits, service evaluations or other considerations of:
-
Older adults, men and non-binary individuals being seen for PTSD in the service (including case series of existing data) – potentially to inform outreach activities to these groups.
-
Matched-group comparisons of CT-PTSD and EMDR treatment outcomes to further control for baseline differences in anxious and depressive symptoms between these groups.
-
Onward referral processes for individuals with PTSD who may not meet the service’s criteria (NHS England, 2024).
-
Data availability statement
The data that support the findings of this study are available from West London NHS Trust. Restrictions apply to the availability of these data, which were used for the purposes of service evaluation and publication in a non-identifiable format, as the study uses routinely collected clinical data where participants gave permission for data to be used for these purposes, but not to be shared more widely for research purposes. Individuals or organisations with permission to access NHS Talking Therapies (formerly IAPT) data from the service at which this service evaluation was conducted may access this data through the IAPTUS interface. Others may be able to access this data for certain purposes with the permission of West London NHS Trust.
Acknowledgements
None.
Author contributions
Stefano Belli: Conceptualization (equal), Data curation (lead), Formal analysis (lead), Investigation (lead), Methodology (lead), Project administration (equal), Writing - original draft (lead); Mark Howell: Conceptualization (supporting), Data curation (supporting), Methodology (supporting), Project administration (equal), Resources (equal), Supervision (supporting), Writing - review & editing (equal); Nick Grey: Methodology (supporting), Writing - review & editing (equal); Silvia Tiraboschi: Methodology (supporting), Writing - review & editing (equal); Alexander Sim: Conceptualization (lead), Data curation (supporting), Formal analysis (supporting), Project administration (equal), Supervision (lead), Writing - review & editing (equal).
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
Nick Grey is an Associate Editor of the Cognitive Behaviour Therapist. They were not involved in the review or editorial process for this paper, on which they are listed as authors. The other authors have no declarations.
Ethical standards
In conducting, analysing and preparing this study for publication, authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS.








Comments
No Comments have been published for this article.