Schizophrenia progresses according to different phases. Reference Lamberti1 Wiersma et al Reference Wiersma, Nienhuis, Slooff and Giel2 reported that the first psychotic episode lasts, on average, 20 months. Only 10-15% of individuals do not experience further psychotic episodes. Reference Wiersma, Nienhuis, Slooff and Giel2,Reference McGlashan3 After recovery from the first acute episode, most individuals have periods of partial or complete remission interspersed with relapses of varying length and severity. 4
Schizophrenia relapse: costs and risk
Relapse in schizophrenia is a major clinical event and commonly affects the personal and social functioning of the person. Moreover, relapses are associated with a high economic burden. A study conducted in the UK showed that the 6-month direct cost of healthcare services for individuals who experience a relapse is four times higher than for those who do not (£8212 v. £1899), most of the difference being explained by in-patient costs. Reference Almond, Knapp, Francois, Toumi and Brugha5
The risk of relapse for a person with schizophrenia has been estimated at 3.5% per month Reference Csernansky and Schuchart6 and approximately 40% experience a relapse within the year following hospital admission. Reference Hogarty and Ulrich7 Risk factors include poor adherence, severe residual psychopathology, poor insight, substance misuse and poor interpersonal relationships. Reference Csernansky and Schuchart6 It is estimated that 40% of relapses are caused by poor treatment adherence, Reference Weiden, Mott, Curcio, Shriqui and Nasrallah8 a major problem in many service users. Reference Weiden and Zygmunt9 As relapse in schizophrenia is associated with a heavy human and financial burden, its prevention has become an important goal.
In 2002, the National Institute for Health and Clinical Excellence (NICE) issued guidance on the use of atypical antipsychotic drugs for the treatment of schizophrenia. 10 It recommended that individuals experiencing adverse effects or unsatisfactory response to typical medications be switched to atypical antipsychotics. In addition, the prescription of clozapine was advocated in those with treatment-resistant schizophrenia. Implementation of this guidance was expected to improve treatment adherence and shift individuals from in-patient care. 10 In an updated guideline, 11 NICE emphasises the importance of relapse prevention and treatment adherence: ‘For people with established schizophrenia, the chance of relapse while receiving continuous antipsychotic medication appears to be about a third of that on placebo’ (p. 98).
Although the cost of schizophrenia in the UK is relatively well documented, data related to the characteristics of individuals who experience relapse and its cost are scarce since the implementation of the 2002 NICE guidance. The only publication on this topic we identified is the study conducted by Almond et al, Reference Almond, Knapp, Francois, Toumi and Brugha5 which compared patients’ characteristics and 6-month treatment costs according to relapse status. However, as the relapse may last longer than 6 months, this estimate may not capture the total cost.
Study aims
We aimed to assess the cost of a schizophrenia relapse admission in South London and Maudsley NHS Foundation Trust (SLAM trust). The first objective was to describe the characteristics of individuals admitted to hospital for relapse. Second, the study aimed to describe the pharmacological treatment of the relapse. The final objective was to determine the length and cost of the relapse admission.
Method
The study was approved by the local ethics committee and research and development unit. The study was conducted between 2004 and 2005. The SLAM trust provides mental health and substance misuse services to a catchment population of more than 1 million. 12
The study team (research nurse or psychiatrist) identified in-patients aged 18 or older, with a diagnosis of schizophrenia or schizoaffective disorder. Diagnosis was determined using the ICD-10 codes entered as standard practice by the psychiatrist (responsible medical officer) on admission. A relapse admission was defined as readmission with a diagnosis of schizophrenia or schizoaffective disorder, thus excluding individuals experiencing their first in-patient episode. The circumstances precipitating hospital admission assessed in the study were reviewed and individuals admitted for reasons other than a schizophrenia relapse were excluded. Patients provided written consent to participate. Once the person was discharged from hospital, a retrospective analysis of medical notes was undertaken.
Information was obtained from the patients and the trust database. The sociodemographic characteristics documented were: age, gender, ethnic origin, marital status, employment status and accommodation. Medical history was recorded: age at diagnosis of schizophrenia, substance misuse, prior prescription of clozapine and number of in-patient stays for schizophrenia over the 5 years preceding the current admission. Last, the details of in-patient stay were recorded: diagnosis on admission (ICD-10), treatment at the time of admission and whether or not the person was detained under the Mental Health Act. Details of prescribed psychotropic medications were recorded from admission to discharge. For each treatment the drug name, dose, route, start date and stop date were recorded. The case notes were reviewed to identify whether non-adherence to treatment was documented to be a cause of the relapse and were classified as: ‘Not known’; ‘No’; ‘Yes suspected’; ‘Yes definite’; and ‘Yes, as one of a number of factors’. No further information regarding other causes of relapse was documented.
Cost per in-patient day was estimated using the Personal Social Services Research Unit 2006 estimate. Reference Curtis and Netten13 Daily cost of National Health Service mental health hospital services is specific to the type of stay: acute stay (£201), long stay (£181) and psychiatric intensive care (£528). To avoid overestimating the cost of relapse, the daily cost of long stay was applied to the whole length of stay in hospital. This includes: capital costs (£25.30); salary, supplies and service costs (£99); agency overheads (£54); and disability living allowance, as calculated by the Department for Work and Pensions (£2.30). The cost of prescribed medications was estimated using unit costs from the British National Formulary and treatment duration. 14 Total cost of hospital treatment was the cost of in-patient stay plus the cost of prescribed in-patient medications.
Data analysis was undertaken using SAS version 9.1 for Windows. Descriptive statistics were generated on patients’ characteristics, medical history, Mental Health Act status and prescribed psychotropic medications. Analyses were undertaken to evaluate the relationship between cost of relapse and patients’ characteristics, medical history and Mental Health Act status on admission. As healthcare costs are generally positively skewed, this variable was log-transformed. Analysis of variance (ANOVA) was used to assess the effect of categorical variables and linear regression was used to test the influence of continuous variables on the total cost of relapse.
Results
A total of 112 in-patients met the eligibility criteria, of whom 71 consented to participate.
Patient characteristics
Two-thirds of patients were men (n = 47; 66%) and mean age on admission was 40.3 years (Table 1). More than half of the cohort was Black and minority ethnic (n = 37; 52%) and a quarter was White (n = 18; 25%). The majority of patients were single (n = 61; 86%) and only one patient was employed.
Table 1 Patient characteristics on admission (n = 71)
| Gender, n (%) | |
| Male | 47 (66) |
| Female | 24 (34) |
| Age, years | |
| Mean | 40.3 |
| Range (s.d.) | 20–69 (11.7) |
| Ethnicity, n (%) | |
| White | 18 (25) |
| Mixed | 9 (13) |
| Black Caribbean | 23 (32) |
| Black African | 6 (8) |
| Black Other | 8 (11) |
| Other | 7 (9) |
| Marital status, n (%) | |
| Married | 5 (7) |
| Cohabiting | 3 (4) |
| Single | 61 (86) |
| Observations missing | 2 (3) |
| Accommodation status, n (%) | |
| Own home | 6 (8) |
| Living with parents/siblings | 6 (8) |
| Rented accommodation | 34 (48) |
| Supported accommodation | 17 (24) |
| No fixed abode | 8 (11) |
Medical history
The mean age at diagnosis of schizophrenia/schizoaffective disorder was 25.2 years (s.d. = 7.2; range 16-50). Psychiatric comorbidities were identified in 14% of individuals (n = 10) on admission. Substance misuse was reported in 27 in-patients (38%): 21 reported using one substance only (30%); two-thirds of these were using cannabis (n = 14; 20% of the total) and fewer were using alcohol (n = 6; 8% of the total) or crack cocaine (n = 1; 1% of the total). Four patients (6% of the total) were using multiple substances.
Almost a third of patients (n = 23; 32%) had received clozapine before the study admission (including those receiving clozapine on admission). All had been admitted at least once within the 5 years preceding the relapse admission; merely 11% (n = 8) had been admitted only once, whereas a third had been admitted at least four times (n = 24; 34%).
Admission for relapse
On admission, 87% of individuals were diagnosed with schizophrenia and 13% with schizoaffective disorder. For a substantial proportion of individuals (n = 50; 70%) the admission was compulsory. Non-adherence to treatment was at least suspected as having precipitated admission in three-quarters of individuals (n = 54): for more than a half (n = 38) it was recognised as a definite cause of relapse, in 14% it was a suspected factor (n = 10) and in 8% it was considered one of a number of factors (n = 6).
Psychotropic medications
On admission
At the time of admission, only a third of individuals (n = 24; 34%) were receiving psychotropic medications, which always included at least one antipsychotic (Fig. 1). Oral preparations were prescribed in 31% of individuals (n = 20) and 10% were receiving depot medications (n = 7), including three in-patients on both depot and oral medications.

Fig 1 Antipsychotic treatments on admission and at discharge.
Olanzapine was prescribed most frequently (10%; n = 7) and sodium valproate, clozapine, quetiapine, oral risperidone and risperidone depot injection were each used in 4% (n = 3) of individuals on admission.
On discharge
The majority of individuals (93%; n = 66) were discharged with at least one psychotropic medication, which always included at least one antipsychotic. The most common type of antipsychotic was an oral atypical used as a single agent in 21 in-patients (30%), followed by typical depot injections as a single agent (n = 18; 25%). A combination of antipsychotics was prescribed in 13 in-patients (18%) (Fig. 1).
The most often prescribed drugs on discharge were sodium valproate (21%); clozapine (17%); oral olanzapine (14%); flupentixol decanoate depot (13%); risperidone long-acting injection (10%); pipotiazine palmitate (10%); and oral risperidone (8%).
Among the 12 individuals who were prescribed atypical oral antipsychotics on admission, 6 were discharged on the same treatment they were admitted on (50%), 4 switched to or added depot medication (33%) and 2 stopped antipsychotic treatment (17%). The two individuals on a single depot antipsychotic remained on the same treatment and the two receiving clozapine on admission were added an oral atypical antipsychotic. Other switches occurred in single cases only.
In-patient length of stay and cost
For one in-patient, information on length of stay was not available. Generally, the duration of stay varied markedly and ranged from 1 week to 1.8 years (658 days); median was 15 weeks (105 days) (Fig. 2). Mean length of stay was 138.9 days (s.d. = 133.6). In only 24% of in-patients (n = 17) length of stay was 5 weeks or less and in 24% it was longer than 6 months (n = 17).
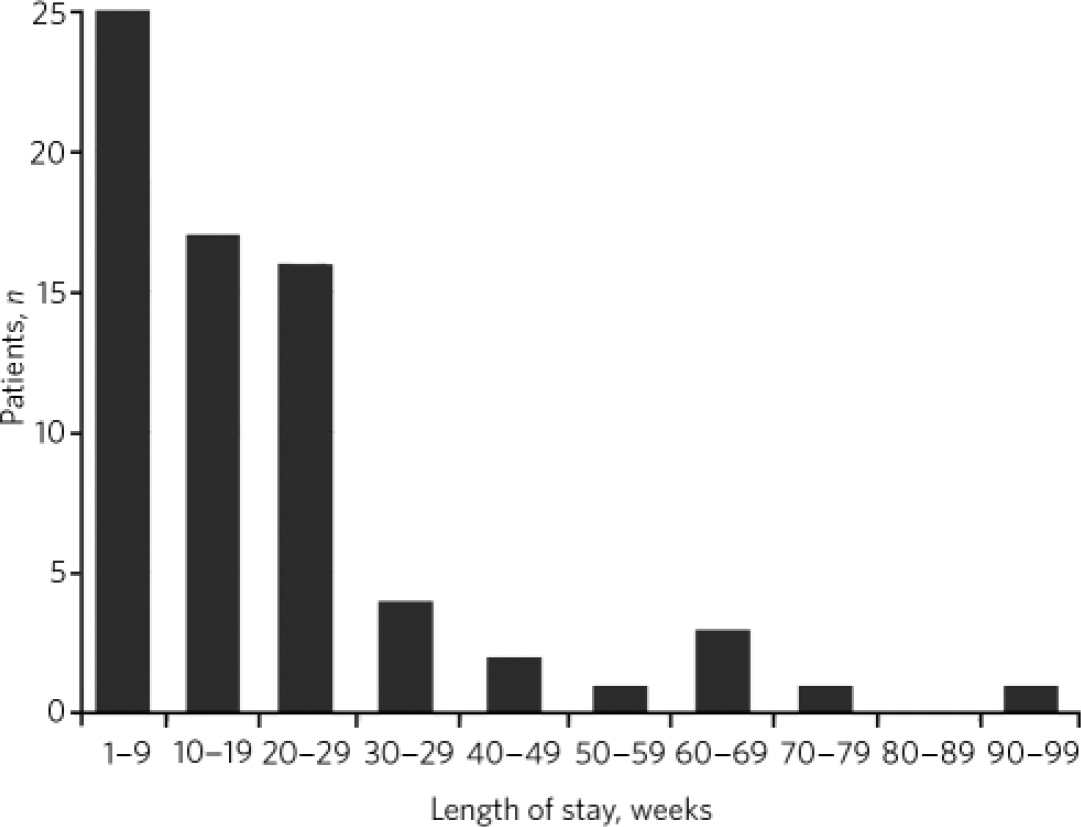
Fig 2 Hospital length of stay in weeks (mean 19.8; median 15, range 1-94).
The analysis of costs used log-transformed costs; the log-transformation resulted in a normal distribution of the regression residuals.
The mean in-patient cost of relapse was £25 852 and varied from £ 1270 to almost £120 000 (Table 2). More than 97% of the costs were attributable to hospital care costs and less than 3% related to pharmacological treatment. The hospital costs alone for the 24% of in-patients (n = 17) that were admitted for 6 months or more ranged from £32 942 to £119 098 and accounted for 57% of the hospital costs incurred by the whole cohort.
Table 2 Cost of relapse admission (n=70)
| Total cost | In-patient cost | |
|---|---|---|
| £ | ||
| Mean (s.d.) | 25 852 (24 777) | 25 141 (24 186) |
| Median | 19 482 | 19 005 |
| Range | 1270–119 933 | 1267–119 098 |
Factors significantly affecting the cost of relapse were analysed via univariate analyses: individuals admitted under the Mental Health Act incurred significantly higher costs compared with those admitted voluntarily, with an observed mean incremental cost of £12 650 per relapse. The cost of relapse was negatively correlated with age on admission and 8% of the variation in the log-transformed costs was explained by age. Diagnosis, history of clozapine, ethnicity, gender, age at diagnosis, and 5-year history of admission and drug misuse were not significantly correlated with the cost of relapse in this cohort. As length of stay is the primary driver of cost, the relationships between in-patient characteristics and length of stay were not further explored.
Discussion
Main findings
This study demonstrates the considerable economic costs of hospital admissions precipitated by a relapse in individuals with schizophrenia. It provides further insight into the extent and consequences of non-adherence to treatment, which was at least suspected to have precipitated the relapse admission in three-quarters of the cohort. Only a third of individuals were receiving antipsychotic treatment at the time of admission and of those, only a third received an antipsychotic depot preparation. Use of depot antipsychotics was markedly more frequent on discharge, when 43% of in-patients received depot. Although the duration of admission varied markedly between in-patients, the mean length of stay was 4.6 months, leading to a mean cost of hospital admission exceeding £25 000 per person. The mean cost of medication was £711, corresponding to 3% of the hospital care budget.
Study cohort
The majority of in-patients in the study were Black and minority ethnic (52%). The Office for National Statistics 2001 census 15 indicates that people of Black African and Black Caribbean ethnicity are in the top three ethnic groups for each borough in the SLAM trust catchment area. Moreover, the proportion of ethnic minorities in this geographical area is much higher than at the national level (34% v. 8%). It is worth noting that the prevalence of functional psychosis has been reported to be three times higher in Black than in White people in the UK. Reference Singleton, Bumpstead, O'Brien, Lee and Meltzer16
Only one individual recruited in this study had part-time employment (1.5% of the cohort under 65 years of age). The survey conducted by Singleton et al Reference Singleton, Bumpstead, O'Brien, Lee and Meltzer16 reports that 28% of individuals with probable psychotic disorder are employed compared with 67% of individuals without such a disorder. The lower employment rate in our study may partly be explained by the local demographics and partly by the severity of illness in the enrolled population.
In the 2002 guidelines, 10 NICE reported that a third of individuals with schizophrenia were unresponsive or intolerant to conventional antipsychotic drugs and should be considered for treatment with clozapine, which is consistent with the fact that 32% of the sample in our study had previously been prescribed clozapine or were on clozapine at admission. The high proportion of individuals admitted under the Mental Health Act (70%) and the frequent in-patient episodes before the study admission suggest that individuals enrolled in this study experienced severe schizophrenia.
Non-adherence to treatment
Adherence to treatment has been identified as a main challenge in the management of schizophrenia. Weiden & Zygmunt Reference Weiden and Zygmunt9 estimated that the rate of out-patient non-adherence to maintenance antipsychotic treatment was 50% within 1 year of discharge and 75% within 2 years. Furthermore, approximately 40% of relapses are because of non-adherence. Robinson et al Reference Robinson, Woerner, Alvir, Bilder, Goldman and Geisler17 reported that individuals who discontinue antipsychotic therapy after a first episode of schizophrenia multiplied their risk of relapse by almost five.
Our study confirms and reinforces these findings, as non-adherence was identified as a definite cause of relapse in the majority of the sample and was at least suspected in 75%. These proportions are consistent with the study conducted by Kamali et al, Reference Kamali, Kelly, Gervin, Browne, Larkin and O'Callaghan18 who reported non-adherence in two-thirds of patients re-admitted for schizophrenia or schizoaffective disorder.
Treatment adherence is influenced by multiple factors. Person-related factors are often a consequence of the illness itself, such as impaired insight into the need for medication or cognitive impairment of memory or understanding. The person's relationship with the physician and factors relating to the medication itself, such as tolerability, efficacy and dosing schedules, also influence adherence. Although only the overall contribution of non-adherence to the relapse admission could be determined from the case notes for this study, further research assessing the importance of the various risk factors may guide targeted interventions to minimise non-adherence.
Strategies for improving treatment adherence may reduce the rate of relapse. Reference Kamali, Kelly, Gervin, Browne, Larkin and O'Callaghan18,Reference Fenton, Blyler and Heinssen19 As reported in the NICE guidelines: 11 ‘There is also some evidence to suggest a better global outcome with depot as compared with oral antipsychotics Reference Adams, Fenton, Quraishi and David20 with a reduced risk of rehospitalisation.’ Reference Schooler21
Treatment pathway
On admission, only a third of individuals received any psychotropic medication. The most commonly prescribed were oral atypical antipsychotics. On discharge, almost all in-patients (94%) received antipsychotic treatment and the number receiving atypical oral antipsychotics had more than doubled.
Sodium valproate was among the most often prescribed medications at discharge (21%). Although this treatment is usually used as a mood stabiliser in individuals with schizoaffective disorder, more than two-thirds of the in-patients who received sodium valproate at discharge did not have a diagnosis of schizoaffective disorder at admission. This finding reflects the diagnostic continuum of schizophrenia and schizoaffective disorder and shows that a person's diagnosis, and hence treatment, may alter over time.
Last, the number of individuals receiving antipsychotic depot medication more than quadrupled between admission and discharge, from 10 to 44%, which suggests that physicians recognise the potential of depot formulations to improve outcome, possibly through better adherence.
Cost of relapse
Individuals re-admitted for a relapse of schizophrenia incurred a mean admission cost exceeding £25 000, of which only 3% was attributed to medications. This study did not capture any costs associated with care after discharge, such as community mental health visits or supported accommodation, and it may therefore underestimate the total cost of a relapse involving hospital admission. The high cost of in-patient care has been documented by other authors. Reference Almond, Knapp, Francois, Toumi and Brugha5,Reference Knapp, King, Pugner and Lapuerta22 Almond et al Reference Almond, Knapp, Francois, Toumi and Brugha5 reported that individuals who experienced relapse incurred 6-month treatment costs more than four times higher than those who did not (£8212 v. £ 1899). The definition of relapse used in their study was based on re-emergence or aggravation of psychotic symptoms and included episodes that did not require hospital treatment. The Almond study population had less severe schizophrenia than our own study cohort, as confirmed by the lower rate of admission under the Mental Health Act (20% as compared with 70% in our study). In addition, our study captures the full in-patient treatment costs, as retrospective data capture was conducted after individuals were discharged, regardless of length of stay, whereas Almond et al report cost at a 6-month cut-off. Truncating the in-patient costs at 6 months in our study resulted in a cost of approximately £18 900 per patient.
Based on data from a 1994 survey report on adults living in institutions that accommodate people with mental illness, Knapp et al Reference Knapp, King, Pugner and Lapuerta22 estimated the mean in-patient cost of schizophrenia at £7487 per annum. Jones et al Reference Jones, Barnes, Davies, Dunn, Lloyd and Hayhurst23 analysed healthcare resource use (including hospital in-patient and out-patient services, primary and community care services, and prescribed medications) and estimated the direct cost of schizophrenia at approximately £ 20 000 per annum.
The mean length of stay observed for the study cohort (138.9 days) was similar to the national mean; hospital episodes statistics 24 report a mean length of stay of 130.2 days for 2004-2005 in individuals with schizophrenia. However, the national median (41 days) is much lower than the median observed in our study (105 days). This indicates that although hospital length of stay, and hence cost, varies widely between patients from this cohort (a quarter of patients accounting for 57% of the in-patient costs), the distribution at the national level is even more scattered, with few patients concentrating a large proportion of the costs. This reflects the NICE guideline update: 11
Hospitalisation costs have been shown to drive healthcare costs incurred by people with schizophrenia, both in published evidence and in the economic analysis carried out for this guideline. It might be reasonable to argue that antipsychotic drugs that reduce the rate and length of hospital admissions (for example, drugs that reduce the rate of future relapses and/or the length of acute episodes) are cost-saving options in the long term, despite potentially high acquisition costs. This hypothesis is supported by published evidence, which shows that increased adherence to antipsychotic treatment is associated with a significant decrease in healthcare costs incurred by people with schizophrenia through a reduction in the risk of relapse and subsequent need for hospitalisation.
This study was undertaken in the period between the publication of the two NICE schizophrenia care guidelines (2002 and 2009). Subsequent research could, therefore, focus on the treatment patterns following the publication of the 2009 guideline.
Study limitations
In this study the definition of a relapse admission was re-admission of a person with a diagnosis of schizophrenia/schizoaffective disorder. Although admissions were screened for precipitating events other than relapse (e.g. social crises), no prospective assessments of symptom severity were available to confirm a deterioration of symptoms and a relapse of schizophrenia. However, the high level of compulsory admissions and the pressure on beds within the trust suggest that these in-patients had significant symptomatology and were not admitted for ‘social’ reasons. The study was based on a retrospective analysis of case notes, which inherently leads to a number of limitations. For example, the duration of historical data on prior relapse may differ between individuals. Moreover, some of the information, such as medication adherence and the reasons for any non-adherence, may not be systematically recorded during medical visits. For these parameters, the level of information and definition used may also differ between physicians. This study was conducted in the SLAM trust, whose catchment area may not be representative of all areas of the UK, as indicated by the longer median length of stay in this cohort than nationally. Therefore, the results from this cohort may not be directly representative and transferrable to other trusts in the UK, but they provide an indicative cost of an in-patient relapse. Last, the results of the study are 4 years old. However, it is important to note that this type of detailed review of schizophrenia relapse admissions in the UK setting has not been published before; the timing of the study in the context of the two NICE guideline documents is also of interest. Future research should focus on a broader capture of costs beyond the in-patient treatment and should assess these costs in several diverse catchment areas.
Funding
The study was funded by Janssen-Cilag. A.G. was funded by Janssen-Cilag for study analyses and preparation of study data.
Acknowledgements
We wish to acknowledge the support and encouragement of the late Professor Robert Kerwin, who was the principle investigator for this study. The study data analyses and write up were undertaken following his untimely death in 2007. We thank Jayantha Ratnayake from Quanticate for undertaking the statistical analysis and the clinical directorates and patients of the SLAM trust who participated in the study.







eLetters
No eLetters have been published for this article.