Discordant fetal growth is one of the causes of increased morbidity and mortality in multiple pregnancies, as well as the cause of divergent, asymmetrical fetal growth. Literature presents several definitions of discordant twin growth. The most widely used definition is intertwine birth weight difference, which is expressed as a percentage (%) of the birth weight of the larger twin. It ranges from 15% to 40% depending on the authors (Divon & Weiner, Reference Divon and Weiner1995). The incidence of fetal growth abnormalities in multiple pregnancies increases significantly compared to singleton pregnancies. The main factors determining fetal growth are genetic potential and the function of the placenta.
Placental failure may induce redistribution in the fetal circulatory system by reducing vascular resistance at the level of the brain and an increased resistance in peripheral vessels. It is the most important mechanism that protects the perfusion of the most vital organs such as the brain, heart, and adrenal glands. Fetuses with features of increased resistance in the placental circulation may have a little possibility to compensate the reduced placental perfusion. Therefore, fetuses with high vascular resistance in the umbilical artery (UA) often demonstrate distress symptoms. Lack of the end-diastolic flow in the UA in multiple pregnancies is definitely associated with worse outcome, increased prenatal mortality, greater risk of growth restriction and developmental delay, oligohydramnios, fetal distress symptoms, as well as some chromosomal abnormalities. If observed during the second and third trimester, most placentas show signs of chronic insufficiency. Absent end-diastolic flow is a sign of severe deterioration, an extreme form of abnormal vascular resistance in the placental circulation.
Cerebral circulation is regulated by several metabolic, neurogenic, and chemical factors. Brain vasculature has the ability of autoregulation. In case of fetal distress, the fetus compensates by centralization of the circulation and distributes blood flow to the major organs, i.e., brain, heart, and adrenal glands. Circulatory centralization can be transient in nature. It may not be observed in fetuses with severe intrauterine hypoxia, in cases of brain edema and cardiac failure. Significant damage to the fetus, during time prior to intrauterine death, may lead to loss of adaptation mechanisms and reconstriction of the vascular bed, which is associated with both the change in vascular sensitivity to hypoxia and the reduction of cardiac output. The resistance to flow in the middle cerebral artery (MCA) can return to normal values even with coexistent increase in vascular resistance in the feto-placental circulation, as a result of depletion of autoregulatory mechanisms.
Aim
The aim of this study was to determine the usefulness of Doppler ultrasonography in the diagnosis of twin pregnancies complicated by discordant fetal growth.
Materials and Methods
The study included 214 patients in twin dichorionic pregnancies, admitted to the Department of Perinatology and Gynecology, University of Medical Sciences in Poznan. Maternal age ranged between 17 and 42 years. The study group included 53 twin pairs with discordant fetal growth. Growth discrepancy was defined as the intertwine birth weight difference expressed as a percentage (%) of the birth weight of the larger twin of 15% or more.
Doppler examination was performed once or repeatedly, and the last one took place not later than seven days before delivery. The last result before the delivery was included into the analysis. The gestational age was determined on the basis of the first day of the last menstrual period and confirmed by the first trimester ultrasound as well as the date of the first fetal movements. All patients gave their informed consent. Doppler blood flow studies were performed using VOULSON 730 EXPERT, equipped with a transducer 3.5 and 5.0 MHz, with the option of pulse wave and color Doppler. During the examination, the patients were lying in the left lateral recumbent position to avoid hemodynamic changes associated with the compression of the inferior vena cava. Time of the examination did not exceed 15–30 min. The test was performed in the absence of fetal movements and breathing activity.
Doppler examination of the blood flow in the UA and MCA was performed in 106 twins. Pulsatility index (PI) values in the umbilical artery (UA PI) above the 95th percentile for given gestational week and the intertwine UA PI difference of ≥0.5 were considered abnormal (14). Similarly, blood flow in the MCA was also studied. The PI values below the 5th percentile for given gestational week were considered abnormal. Fetal blood flow centralization, known also as the brain sparing effect, was defined on the basis of the cerebro-umbilical ratio (C/U), which is MCA PI/UA PI quotient. The value of <1.08 was considered abnormal.
Sequentially, Doppler results were compared with selected parameters that characterize the course of pregnancy and fetal outcome. The analyzed parameters included: maternal age, obstetric history, gestational age at delivery, degree of growth discordance, Apgar score at 1 and 5 min of life, the value of pH and base excess (BE) in the UA, the percentage of abnormal fetal outcome, mean birth weight, the percentage of small for gestational age (SGA) newborns, as well as those with birth weight below 1,000 g and 1,500 g. Finally, the predictive value of abnormal Doppler blood flow parameters was evaluated.
Fetal outcome was analyzed on the basis of the acid-base equilibrium parameters and Apgar score. Fetal outcome was considered abnormal when:
• 5-min Apgar score is < 7, or
• pH is < 7.20, or
• BE is ≤ 12 mEq/L.
Then, selected parameters, characterizing pregnancy course, and fetal outcome, were compared with abnormal Doppler studies. The prognostic value of abnormal parameters characterizing blood flow in relation to selected parameters determining the pregnancy course and fetal outcome were also assessed.
Parameters expressed on an interval scale, such as gestational age, birth weight, pH, or BE were described as the arithmetic mean and standard deviation. The compliance of those parameters with normal distribution with the Shapiro-Wilk test was analyzed. For parameters consistent with the normal distribution, to compare between the two groups, Student's t-test for independent variables was used when the variances in the samples were homogeneous, otherwise the Welch test was used. When compliance with the normal distribution was confirmed, non-parametric Mann-Whitney test was used. Apgar score at 1 and 5 min expressed on an ordinal scale described median, minimum, and maximum values and the Mann-Whitney non-parametric test was used to compare two independent groups. Parameters expressed in nominal scale were depicted as the number of newborns in each category and the corresponding percentage. Contingency tables were determined as a composite of two parameters at nominal scale. Chi-square test with Yates’ correction or Fisher exact test was used to investigate the relationship between these parameters in the tables 2×2. The evaluation was performed for the following levels of significance: p < 0.05, < 0.01, < 0.001. The normal and abnormal values of Doppler indices were coded. These categories accounted for the test. The comparison with the parameters of the newborn assessment and the number of true positive, true negative, false positive, and false negative cases were determined. Then, sensitivity, specificity, positive predictive values (PPV), and negative predictive values (NPV) were defined. Calculations were performed using the statistical package STATISTICA, a 2007 data analysis software system by StatSoft, Inc., version 8.0, your package GraphPad Instat Software, and Analyse-it for Microsoft Excel v. 2.2.
Results
In the study group of 106 twins with discordant fetal growth, 71.7% presented the normal value of UA PI and 28.3% had abnormal results. Tables 1–3 present pregnancy course and fetal outcome with regard to the UA blood flow, UA PI intertwine differences, and signs of the brain sparing effect.
TABLE 1 Pregnancy Course and Fetal Outcome in the Group With Normal and Abnormal UA PI Values
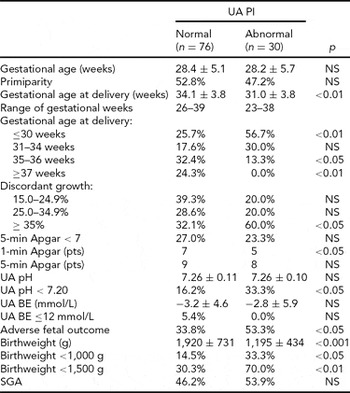
UA PI = umbilical artery pulsatility index; UA pH = pH value in the umbilical artery; UA BE = base excess in the umbilical artery; SGA = small for gestational age.
TABLE 2 Pregnancy Course and Fetal Outcome With Regards to Intertwine UA PI Values’ Difference

UA PI = umbilical artery pulsatility index; BE = base excess; SGA = small for gestational age.
TABLE 3 Evaluation of Parameters Characterizing the Course of Pregnancy Depending on the Cerebro-Umbilical Ratio
BE = base excess; SGA = small for gestational age.
Abnormal UA PI correlated significantly with lower gestational age at delivery, intertwine growth discordance of 35% or more, lower birth weight, and abnormal fetal outcome. Similarly, the intertwine PI difference of 0.5 and more was significantly associated with an increased risk of premature labor, significantly lower birth weight, increased risk of SGA, and abnormal fetal outcome. Statistically significant differences were also found in the group with abnormal C/U ratio. The abnormal C/U ratio correlated with lower birth weight, abnormal fetal outcome, and an increased risk of premature delivery.
In the study group, 81.1% fetuses presented normal PI values and 18.9% with abnormal PI results in the MCA. There were no statistically significant differences in the majority of parameters that characterize the neonatal outcome between the groups with normal and abnormal MCA PI (data not included in tables). In the group with abnormal MCA PI values, significantly lower mean birth weight and higher percentage of birth weight less than 1,500 g were observed. Those fetuses were delivered prematurely, but this parameter did not achieve any statistical significance.
Table 4 illustrates the predictive value of analyzed Doppler indices. The intertwine UA PI difference of ≥0.5 had the highest predictive value in the assessment of adverse fetal outcome and risk for SGA. This parameter demonstrated the highest sensitivity. Relatively poor sensitivity was noted with regard to the abnormal values of UA PI and C/U ratio. The worse correlation was found in case of MCA PI. The highest value of odds ratios was observed with regard to the intertwine UA PI difference of ≥0.5.
TABLE 4 The Predictive Value of Abnormal Doppler Indices With Regards to Fetal Outcome
PPV = positive predictive value; NPV = negative predictive value; LR = likelihood ratio; OR = odds ratio; UA PI = umbilical artery pulsatility index; SGA = small for gestational age; C/U ratio = cerebro-umbilical ratio; MCA PI = middle cerebral artery pulsatility index.
Discussion
Discordant fetal growth is considered to be a potential indicator of impaired growth. The aim of this study was to evaluate the applicability of Doppler ultrasonography in predicting the course of pregnancy and fetal outcome in twin pregnancies complicated by growth discordance.
In twins with growth discordance of 15% and more with abnormal Doppler results in the MCA and UA significantly lower, gestational age at birth, lower mean birth weight, a higher percentage of SGA, and abnormal fetal outcome were observed. However, in the literature different data may be found. Frezza et al. (Reference Frezza, Gallini, Puopolo, De Carolis, D'Andrea, Guidone, Luciano, Zuppa and Romagnoli2011) evaluated whether growth discordance is an independent risk factor in the neonatal outcome of the smaller twin. No significant differences between the four groups of different discordance were found with regard to obstetric complications and neonatal diseases. Occurrence of birth weight below the 10th percentile and rate of admission to the neonatal intensive care unit significantly increased as intra-pair birth weight difference increased (p = 0.03). The >40% discordant group had a significantly lower gestational age (p = 0.03), lower birthweight (p = 0.007), and a significantly higher mortality rate (4/10 vs. 3/39; p = 0.04) in comparison with the other discordant groups. Gestational age was the most reliable predictor for major neonatal complications. However, neonatal outcome in discordant twins appeared to be related to gestational age and birthweight rather than to the degree of discordance. Miller et al. (Reference Miller, Chauhan and Abuhamad2012) analyzed twin gestations with growth discordance of at least 20%. They found that discordant growth alone is not an indication for preterm birth. Although there are multiple publications on an increased morbidity and mortality rates with discordant growth, there is a paucity of reports on how to manage them optimally and deliver them in a timely manner. Morin and Lim reviewed the literature with respect to the use of diagnostic ultrasound in the management of twin pregnancies (Morin & Lim, Reference Morin and Lim2011). They suggested that growth discordance might be defined using either a difference (20 mm) in absolute measurement in abdominal circumference or a difference of 20% in the ultrasound-derived estimated fetal weight. Moreover, UA Doppler was found to be useful in the surveillance of twin gestations when there were complications involving placental circulation or fetal hemodynamic physiology. Increased fetal surveillance should be considered when there is either growth restriction diagnosed in one twin or significant growth discordance. Fox et al. (Reference Fox, Saltzman, Schwartz, Roman, Klauser and Rebarber2011) discovered that patients with second-trimester discordance of 15% or greater were significantly more likely to deliver a twin with a birth weight below the 10th percentile for gestational age (67.7% vs. 44.1%; p = 0.012) and below the 5th percentile for gestational age (41.9% vs. 22.8%; p = 0.019). It has been stated that second-trimester estimated fetal weight below the 10th percentile and discordance of 15% or greater are associated with fetal growth restriction. In contrary, Gezer et al. (Reference Gezer, Rashidova, Güralp and Oçer2012) did not find any relation between perinatal mortality and morbidity and the intrauterine growth restriction and intertwine growth discordance in twin pregnancies. However, opposite results were found by Breathnach et al. (Reference Breathnach, McAuliffe, Geary, Daly, Higgins, Dornan, Morrison, Burke, Higgins, Dicker, Manning, Mahony, Malone and Consortium2011). They examined a group of unselected twin pairs. Adjusting for gestation at delivery, twin order, gender, and growth restriction, perinatal mortality, individual morbidity, and composite perinatal morbidity were all seen to increase with birth weight discordance exceeding 18% for dichorionic pairs (hazard ratio 2.2, 95% confidence interval (CI) 1.6–2.9, p < 0.001) and 18% for monochorionic twins without twin-twin transfusion syndrome (hazard ratio 2.6, 95% CI 1.6–4.3, p < 0.001). A minimum two-fold increase in risk of perinatal morbidity persisted even when both twin birth weights were appropriate for gestational age. Alam Machado et al. (Reference Alam Machado, Brizot, Liao, Krebs and Zugaib2009) compared twin pregnancies with weight discordance of 20% or more with pregnancies concordant for fetal weight. No differences between monochorionic and dichorionic subgroups were observed in discordant twins. Pregnancies in which at least one baby was born with a birthweight below the 10th percentile showed that discordant pregnancies had a lower gestational age at delivery (35.2 vs. 36.8 weeks) and a longer period of hospital stay (nine vs. four weeks) compared to concordant cases. Neonatal mortality was similar in discordant (3.7%) and concordant (4.5%) twins. The authors concluded that early perinatal morbidity is increased in twin pregnancies with birthweight discordance ≥20% only when associated with fetal growth restriction and low birthweight.
Studies of monochorionic twins revealed differences in prognosis for discordant twins. Lewi (Reference Lewi2010) studied monochorionic diamniotic twin pregnancy outcome. He postulated that unequally shared placentas have a more elaborate blood exchange, which reduces the birthweight discordance. In these cases, the anastomoses fulfill a beneficial role by increasing the availability of oxygen and nutrients to the twin on the smaller placental share. Pairs with early onset discordant growth have a higher mortality and a more unequally shared placenta than pairs with late onset discordant growth. Unequal placental sharing therefore appears to be the cause of early onset discordant growth, whereas a late intertwine transfusion imbalance may be involved in some cases with late onset discordant growth. Gratacós et al. (Reference Gratacós, Lewi, Muñoz, Acosta-Rojas, Hernandez-Andrade, Martinez, Carreras and Deprest2007) concluded that selective intrauterine growth restriction (sIUGR) in monochorionic twins might be classified on the basis of UA Doppler into three types that correlate with different clinical behavior and different patterns of placental anastomoses. This classification may be of help in clinical decision-making and when comparing clinical studies. Similarly, Valsky et al. (Reference Valsky, Eixarch, Martinez and Gratacós2010) assessed abnormal twin growth in monochorionic twins. They have proposed a classification of sIUGR into three types according to UA Doppler findings (Type 1: normal; Type 2: absent/reverse end-diastolic flow; and Type 3: intermittent absent/reverse end-diastolic flow), which correlates with distinct clinical behavior and placental features and may assist in counseling and management. In terms of prognosis, sIUGR was roughly divided in two groups: Type 1 cases, with a fairly good outcome, and Types 2 and 3, with a substantial risk for a poor outcome.
Many researchers have drawn attention to the usefulness of Doppler examinations in monitoring the development and growth in multiple pregnancies. Degani et al. (Reference Degani, Paltiely, Lewinsky, Shapiro and Sharf1988) have proposed adding the measurement of vascular resistance in the internal carotid artery to the analysis of blood flow in UA in order to improve prediction of twin pairs at risk of growth disorders and delivery of a child with low birth weight. Measurement of the PI values in the internal carotid artery contributed to increased sensitivity of the test. Presented by Degani and coworkers, sensitivity of blood flow in the UA in predicting the SGA newborn was 47%, while in the UA and internal carotid artery 58%. The highest sensitivity was obtained by combining biometric parameters (AC) with Doppler examinations (84%).
The results of the present study confirm the work reported by other authors. Joern et al. (Reference Joern, Schroeder, Sassen and Rath1997) assessed the predictive value of a combined analysis of blood flow in the aorta, UA, and MCA in predicting the birth of a SGA infant. A combined analysis of blood flow in these vessels had 76% sensitivity and 58% specificity. Analysis of blood flow in the UA was characterized by 47% sensitivity and 71% specificity, while in the MCA it was 33% and 86%, respectively. In the present study, the analysis of blood flow was characterized by low sensitivity and PPV. The fact is that the predictive value of the studied diagnostic methods depends greatly on the adopted criteria that identify adverse fetal outcome. Hence, from a methodological point of view, comparison of the obtained results is difficult and sometimes even impossible. Most of the publications concerning the application of blood flow studies in monitoring of multiple pregnancy, underline the usefulness of Doppler examinations (Divon & Weiner, Reference Divon and Weiner1995; Saldana et al., Reference Saldana, Eads and Schaefer1987).
Many authors emphasized the importance of the presence of extremely abnormal blood flow results in UA in the form of the phenomenon known as arterial absent or reversed-end-diastolic flow (ARED). Hastie et al. (Reference Hastie, Danskin, Neilson and Whittle1989) found that the absence of end-diastolic flow in UA was associated with poor prognosis in a group of 89 unselected twin pregnancies. Increased morbidity and mortality in the absence of end-diastolic flow was also observed in triplet pregnancies. Ezra et al. (Reference Ezra, Jones and Farine1999) found that the presence of ARED was associated with increased prenatal mortality of up to 50%. Rafla (Reference Rafla1989) also found an increase in prenatal mortality in case of triplet pregnancies complicated by ARED. Giles (Reference Giles1998) observed two cases of in utero fetal deaths among 17 fetuses with ARED in 20 pairs of triplet pregnancies. There are few publications evaluating the role of Doppler examinations in the supervision of triplet and higher-order pregnancies. Prompeler et al. (Reference Prompeler, Madjar, Klosa, du Bois, Peukert, Wilhelm and Breckwoldt1993) observed 16 triplet and two quadruplet pregnancies. They showed that a precise diagnosis of restriction or discordant fetal growth was easier by adding of blood flow analysis to biometric assessment.
There are also reports on the significance of the brain-sparing effect phenomenon in twins. Many authors highlight the role of this phenomenon in determining the risk to the fetus (Arias, Reference Arias1994; Bahado-Singh et al., Reference Bahado-Singh, Kovanci, Jeffres, Oz, Deren, Copel and Mari1999; Breathnach et al., Reference Breathnach, McAuliffe, Geary, Daly, Higgins, Dornan, Morrison, Burke, Higgins, Dicker, Manning, Mahony, Malone and Consortium2011). However, the exact clinical significance remains to be investigated. Confirmation of potential significance of this phenomenon is the work of Bahado-Singh et al. (Reference Bahado-Singh, Kovanci, Jeffres, Oz, Deren, Copel and Mari1999), who showed a higher prognostic value of this phenomenon in comparison to blood flow assessment in the UA in predicting an unfavorable prognosis for the fetus in the group with growth restriction. Similarly, Arias (Reference Arias1994) found that the occurrence of centralization of fetal circulation in a single pregnancy is associated with high risk of growth restriction and neonatal morbidity. In the present study, the brain-sparing phenomenon was observed in 27.4% of twins with discordant growth. Those twins were at risk of premature delivery, mean weight was significantly lower (1,460 g vs.1,980 g), and there was higher percentage of SGA infants (53.9% vs. 46.2%) and adverse fetal outcome compared to the group without the brain-sparing effect. Gaziano et al. (Reference Gaziano, Gaziano, Terrell and Hoekstra2001) presented similar results. It has been found that the brain-sparing effect had the highest predictive value in relation to fetal growth disturbance (SGA), abnormal fetal outcome, and the length of hospitalization compared to blood flow monitoring in only one vessel. However, it should be noted that in the present study the analysis of this phenomenon was based on the PI values. It seems that the incidence of this phenomenon may have different meanings depending on the twin's chorionicity. In dichorionic pregnancy, the increase in the placental–fetal circulation reflects mainly placental failure, often preceding the occurrence of fetal heart rate abnormalities in the form of decelerations recorded by cardiotocograph (Rizzo et al., Reference Rizzo, Arduini and Romanini1994). Reports of Gaziano et al. (Reference Gaziano, De Lia and Kuhlmann2000, Reference Gaziano, Gaziano, Terrell and Hoekstra2001) suggest the significance of the beginning and magnitude of changes in the UA in comparison to the magnitude and beginning of disturbances in MCA in predicting fetal abnormalities. In addition, they observed a higher incidence of this phenomenon in a population of monochorionic twins, which may indicate a potentially higher risk group. This phenomenon was observed even more frequently in monochorionic twins with growth restriction. However, no relationship between brain-sparing effect and fetal prognosis was found (Gaziano et al., Reference Gaziano, Gaziano and Brandt1998).
In summary, it seems safe to conclude that the results obtained in this study, in regard to predicting the SGA infants and abnormal fetal outcome, confirmed the reports of other researchers. It should be noted, however, that the results presented in the literature differ considerably. Undoubtedly, the diversity of the criteria adopted by the researchers (e.g., in relation to the mass disproportion (>300 g, ≥15%, ≥25%, etc.), the SGA infant (<3, 5, or 10 percentile, for singleton or multiple pregnancy), and prognosis for the fetus) is significant. This lack of uniform criteria is an essential obstacle in comparing the results obtained by other researchers. Undoubtedly, abnormal UA Doppler results correlate with low birth weight infant (SGA) in multiple pregnancies. These results may be also useful in predicting life-threatening conditions for the fetus. It seems that the differences in the PI values in the UA and MCA in pairs of twins may suggest growth restriction secondary to placental insufficiency of the smaller twin. The difference in the UA PI values has the highest value in the prediction of abnormal neonatal status and low birth weight. Just as in singleton pregnancy, serial measurements of many parameters seem to be better than a single measurement. Adding Doppler examinations to biometric measurements may increase the probability of detecting abnormalities of fetal growth in multiple pregnancies. Considering much greater number of complications occurring in multiple pregnancies, we can say that despite the relatively low sensitivity of Doppler examinations its application in the monitoring of twins is justified.
Acknowledgment
The study was funded by a KBN grant 2PO5E 030 27.






