Genetic and genomic testing is rapidly becoming widespread across healthcare, leading to genetic diagnoses in many people who would previously have remained undiagnosed. When these diagnoses point to conditions that are inherited, blood relatives may have the opportunity to undergo carrier testing to identify whether they also carry the familial variant. For this testing to be conducted in an appropriate and supportive way, ethical and psychosocial aspects need to be considered.
This Position Statement from the Human Genetics Society of Australasia (HGSA) presents the major practical, psychosocial and ethical considerations associated with carrier testing in the following groups: adults who have the capacity to make a decision; adults living with reduced or fluctuating cognitive capacity; children and young people who lack capacity; and young people under the age of majority who have capacity.
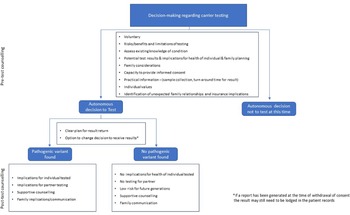
There are a number of different ways in which carrier status can be identified (see Figure 1). Additionally, Table 1 provides relevant definitions.

Fig. 1. Ways in which carrier status can be identified.
Note: Blue denotes settings where carrier status identification is the goal of the test. Grey denotes tests where a carrier result may be unexpected and are thus beyond the scope of this position statement. ^Affected — individual with a genetic diagnosis of a condition that can be inherited. *Carrier — individual with a pathogenic variant for an autosomal recessive or X-linked recessive condition or carrying a balanced chromosomal rearrangement. #Also known as online DNA testing.
Table 1. Definition of terms
This Position Statement is relevant to healthcare settings where genetic testing is requested to determine carrier status. This testing can be offered when there is a known pathogenic variant(s) in the family and the test will definitively determine whether or not someone is a carrier of a particular familial variant. This Position Statement does not provide guidance in relation to: (1) reproductive or population-based genetic carrier screening (see Box 1); (2) carrier results ascertained as an incidental finding through a research project; (3) carrier results reported by a clinical laboratory as an incidental finding in the context of diagnostic genetic testing; or (4) carrier results identified by direct-to-consumer testing where an individual may seek genetic counseling to understand the result. This Position Statement also does not provide guidance in relation to conducting predictive or pre-symptomatic testing for autosomal dominant conditions as this is addressed in a separate HGSA Position Statement, Predictive and Pre-symptomatic Genetic Testing in Adults and Children (2020PS01).
Box 1. Reproductive Genetic Carrier Screening
Reproductive genetic carrier screening (RGCS; also referred to as expanded carrier screening or universal carrier screening) is available to individuals and couples to provide information about the chance they will have a child with certain recessive or X-linked genetic conditions. RGCS can be undertaken prior to conception or early in pregnancy. At the time of writing, RGCS is largely available in Australia via private providers, for a fee. In 2019, the Medical Services Advisory Committee recommended that the federal Minister for Health approve funding for reproductive carrier screening for three conditions: spinal muscular atrophy, cystic fibrosis and Fragile-X. No funding has yet been committed. A research project, Mackenzie’s Mission, is running from 2018–2022 to screen up to 8,500 Australian couples for ∼1,300 genes to detect ∼750 recessive and X-linked conditions. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG, 2019) recommends that all pregnant persons are provided with information about carrier screening. RGCS is not testing for a particular variant, but simultaneously tests for many different potential variants at once. RGCS can identify carriers; however, RGCS is not able to rule out carrier status, which is why it is considered screening.
General Considerations in Carrier Testing
Carrier testing may be requested for many reasons but is usually prompted by the presence of a family history of a genetic condition. Once a person is diagnosed with a pathogenic variant causing an inherited genetic condition or identified as a carrier for that condition, carrier testing can be offered to the individual’s blood relatives. Carrier testing of this nature is sometimes referred to as cascade testing.
Understanding the inheritance pattern of the condition identified in the family helps inform which blood relatives should be offered carrier testing. In some cases, carrier status may have health implications for the individual’s own health or development. Carrier status may inform reproductive choices.
Requests or referrals for carrier testing may occur in different contexts:
-
An individual from a family with a known autosomal recessive condition may seek carrier testing.
-
An individual’s partner may request carrier screening for a condition to inform their joint reproductive choices.
-
A genetically female individual (e.g., XX) from a family with a known X-linked condition may seek carrier testing to ascertain whether they have inherited the X-linked pathogenic variant identified in other blood relatives. The result may have implications for their own health/development (be diagnostic in nature) and/or may inform reproductive choices.
-
An individual from a family with an unbalanced chromosomal translocation/rearrangement may seek testing to determine if they carry a balanced chromosomal translocation/rearrangement. This is because balanced chromosomal translocations/rearrangements can have implications for family members and influence reproductive decision making.
-
Carrier testing may also be requested by an individual whose blood relative has been identified as a carrier through reproductive carrier screening or as an incidental finding through testing for other purposes.
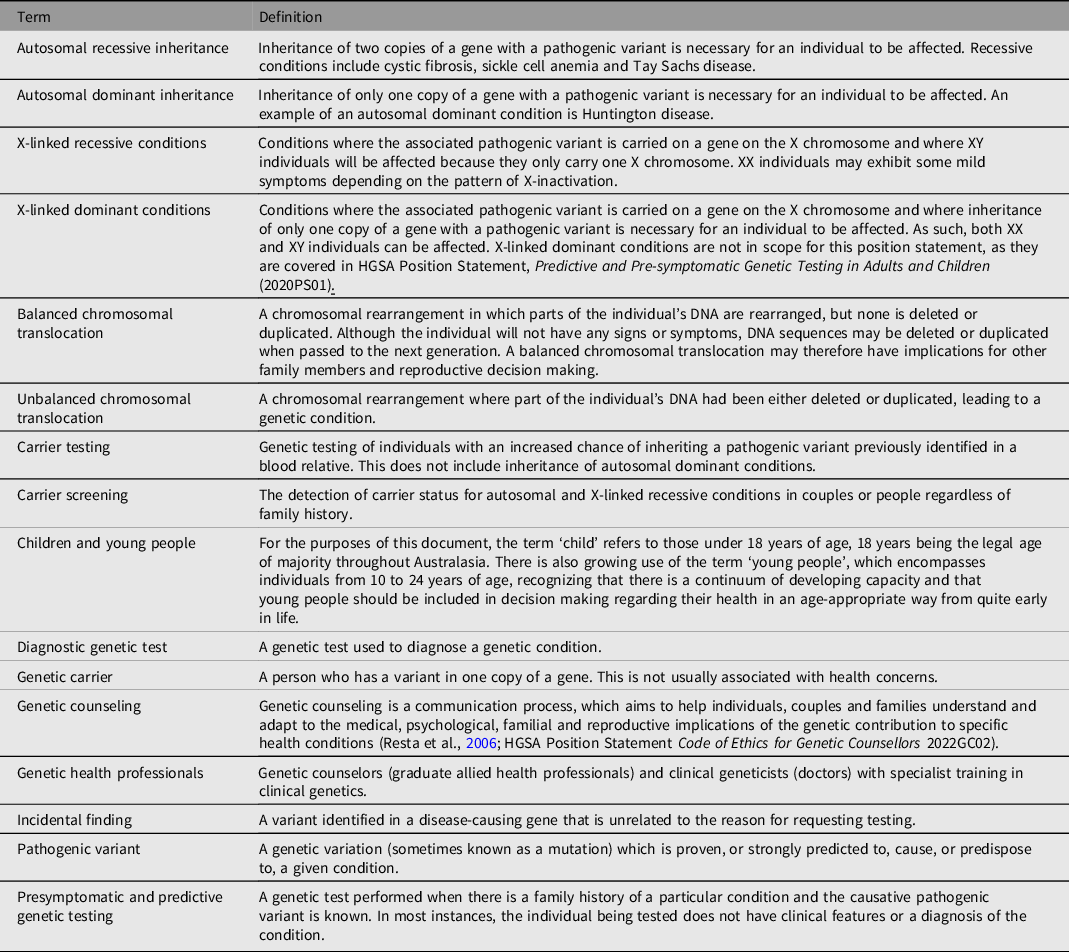
Figure 2 outlines the decision-making pathway and counseling considerations for carrier testing.

Fig. 2. Flow chart of the decision-making pathway and counseling considerations for carrier testing.
Counseling Considerations in Carrier Testing
Carrier testing should only be performed with an individual’s knowledge and consent. Counseling considerations for carrier testing depend on:
-
The mode of inheritance (i.e., autosomal recessive, X-linked, chromosomal translocation/rearrangement).
-
Personal experience with the genetic condition.
-
The severity of the clinical presentation.
-
The frequency of the variant in the population.
-
The healthcare setting in which the test is being performed.
Individuals undergoing carrier testing for autosomal recessive conditions may experience some degree of anxiety while waiting for results and immediately after learning carrier status, but this typically dissipates shortly thereafter (Bekker et al., Reference Bekker, Denniss, Modell, Bobrow and Marteau1994; Callanan et al., Reference Callanan, Cheuvront and Sorenson1999; Honnor et al., Reference Honnor, Zubrick, Walpole, Bower and Goldblatt2000). In contrast, carrier testing for X-linked conditions is associated with a risk of psychological distress prior to testing, while awaiting results, and after receiving the test result. Similarly, carrier testing for a chromosomal translocation/rearrangement can be associated with psychological distress, especially when there is a high chance of fetal anomaly and/or pregnancy loss.
Being identified as a carrier may also negatively affect relationships with the individual’s partner and family more broadly. Within the family, this can be exacerbated by the fact that a pathogenic variant identified in one family member automatically changes the chance of being a carrier for relatives; for example, siblings have a 50% chance of being a carrier. Carrier parents also articulate the fear and guilt of passing on conditions to their children.
Of note, genetic conditions have been particularly well studied in individuals of European ancestry and, to a lesser extent, individuals from Asia and Africa (Henneman et al., Reference Henneman, Borry, Chokoshvili, Cornel, van El, Forzano, Hall, Howard, Janssens, Kayserili, Lakeman, Lucassen, Metcalfe, Vidmar, de Wert, Dondorp and Peterlin2016). Consequently, testing is often focused on those groups. However, it is important to be inclusive of minority populations who have been less studied to date — particularly Aboriginal and Torres Strait Islander peoples and Māori — to ensure these populations are not further disadvantaged. Testing should always be offered in a culturally safe, respectful manner.
Guidance for the Provision of Carrier Testing
Carrier testing for most conditions should be offered by a genetic counselor or a clinical geneticist.
Carrier testing for some conditions can be offered by non-genetic health professionals as a routine test. For example, carrier testing for hemochromatosis is appropriately offered by general practitioners while hemophilia testing is appropriately offered by a hematologist.
All health professionals offering genetic carrier testing must be knowledgeable about the genetic condition being tested for and confident that they can discuss results accurately.
Testing should be done in an accredited laboratory by staff appropriately trained using a validated test.
-
The voluntary nature of the testing and the opportunity to withdraw from the testing process at any point.
-
Testing risks and benefits, including the potential psychological impact on the individual, their partner and other family members. This is particularly important for X-linked conditions.
-
Exploration of the person’s level of knowledge about the condition. If the individual or couple are not familiar with the condition(s) for which they are being tested, the clinical features and impacts of these conditions should be discussed.
-
The mode of inheritance for the condition(s) being tested and, if positive, the implications for other family members.
-
Potential test results and the possible implications of these outcomes for the individual or couple.
-
Whether there is a possibility for incidental findings (i.e., when using chromosome microarray technology to determine carrier status).
-
The reproductive options available for individuals or couples, depending on the results.
-
Logistics such as sample collection, test costs, test limitations and turn-around-time for results.
-
The possibility of revealing unexpected family relationships (if relevant).
-
Reassurance that, in general, being identified as a healthy carrier of a recessive genetic condition should not negatively impact an individual’s ability to obtain risk-rated insurance policies (e.g., life or income protection insurance). See HGSA position statement Genetic Testing and Personal Insurance Products in Australia (2018 PS01).
-
The plan for disclosure of results, whether this will vary depending on the result and the option of declining to receive results.
Information covered in the post-test discussions should include:
-
Clear, sensitive, objective, and noncoercive communication of results. It is important to ensure individuals understand their carrier status and the significance of the result for themselves, their children, other blood relatives, and future pregnancies. Individuals identified as carriers may find it beneficial to review the diagnosis, prognosis, and management of the associated condition.
-
Discussion about the plan for sharing an individual’s carrier status with other family members. Testing is typically offered to all relevant relatives. This has confidentiality implications (see below). To facilitate family communication, the health professional may offer to provide a letter with information about what it means to be a carrier, information about the condition itself, as well as how to access further information, support and/or testing. This letter is typically non-identifying and can be provided to relatives to complement family communication.
-
The degree of certainty associated with a noncarrier result, and whether there is any possibility that a variant was present but not detected.
-
Reproductive options for the individual/couple.
-
Referral to another health professional (e.g., fetal medicine specialist, pediatrician) or support organisation may be appropriate for some individuals following the result.
-
Offer of a follow-up appointment or phone call, depending on individual needs, the nature of the result, the implications of testing, and the policy of the clinical service.
Circumstances in Which Individuals Should See a Genetic Health Professional
Although carrier testing is increasingly integrated into standard clinical care, there are some circumstances in which an individual may benefit from seeing a genetic health professional:
-
When an individual is being tested for a condition which affects a close relative as this ensures both accuracy in testing and appropriate counseling in the event of test-related anxiety.
-
When an individual has a high chance of being a carrier of an X-linked condition or a chromosomal translocation/rearrangement.
-
When both members of a couple have an increased chance of carrying a pathogenic variant for an autosomal recessive condition.
-
When carrier testing is being requested in children, young people, and/or individuals with limited capacity to consent.
Confidentiality
Maintaining confidentiality of genetic test results is important, as is the case for all health information. This accords with both ethical norms (such as trust in health professionals, respect for privacy and patient autonomy) and legal obligations. At the time of testing, the individual being tested (or their parent/guardian) should be informed about how their personal information, including their test result, will be stored and accessed.
Further, as touched upon above, the shared nature of genetic information means that a genetic test result in one individual can also have implications for family members. The communication of this information within the family is not always faithfully transmitted nor welcomed. This dilemma gives rise to numerous issues, including whether genetic information should be said to belong to individuals or families, who should take responsibility for disclosure, and what ethical and legal obligations are generated when so-called non-disclosure occurs. In the post-test counseling session, the implications for relatives should be explored and individuals encouraged to disseminate information to potentially impacted family members. Health professionals should also seek consent to share relevant information (minimizing identifying details wherever possible) with other relevant family members.
These issues have been discussed in more detail in the HGSA Position Statement Use of Human Genetic and Genomic Information in Healthcare Settings (2021PS01).
Capacity to Give Informed Consent
Adults with reduced capacity
Health professionals need to take extra care and allow additional time to support people with reduced cognitive capacity, such as adults with intellectual disability, through the process of carrier testing. It is important to be mindful that such appointments can be traumatic and people with intellectual disability may have a tendency to pretend they understand information. Information should be provided in a clear, sensitive, comprehensible and individualized way to all individuals according to their cognitive ability. Where possible, accessible resources such as easy-to-read information should be provided. For individuals who lack the capacity to consent, a support person, such as the carer, legal guardian, relative, or designated decision-maker who will be providing consent, should be present during consent conversations. However, it is important that health professionals still actively include the individual being offered testing in the genetic counseling process.
Assessing a young person’s capacity to make medical/health decisions
Most states and territories recognize 18 years as the age at which young people attain the capacity to make decisions for themselves regarding their medical care, provided they have sufficient understanding of the medical intervention under consideration and adequate cognitive ability to meet capacity requirements Footnote 1 . Young people may be able to provide consent before the age of 18 if they are found to possess the cognitive ability and psychological maturity to understand the consequences of their decisions and therefore make an informed choice about their medical care, known as a ‘mature minor’. The capacity of young people to consent to genetic carrier testing needs to be assessed in accordance with the law applicable to the relevant jurisdiction. This assessment will include several aspects, including their cognitive and psychosocial maturity, their ability to understand genetic concepts, and also whether they are able to appreciate the potential long-term repercussions of their decision. Such repercussions could include impacts on their mental health, social situation and relationships, employment, and ability to obtain certain types of insurance. Young people should always be included in the decision-making process regarding genetic testing at a level that is appropriate for their age, cognitive ability, and level of maturity, even if they are not legally capable of making the decision alone.
Considerations in Deciding Whether to Facilitate Carrier Testing in Children and Young People
Requests for carrier testing in children may occur in several situations:
-
Parents may request carrier testing for their unaffected children following the diagnosis of a sibling with an autosomal recessive or X-linked condition.
-
If a child is diagnosed with a chromosomal translocation/rearrangement, parents may wish to know if their unaffected children have inherited a balanced translocation.
-
Parents may request carrier testing in unaffected siblings in response to routine newborn screening, both when a sibling is diagnosed with a condition or identified incidentally to be a carrier (e.g., newborn screening for cystic fibrosis).
-
Young people may also request carrier testing for themselves as they get older if they have an affected sibling or blood relative.
-
Testing may be requested if a young person is pregnant or may become pregnant.
Guidelines on Carrier Testing in Children and Young People
International guidelines generally recommend against carrier testing in childhood, particularly where identifying carrier status does not have the potential for medical benefit (American Society of Human Genetics Board of Directors and American College of Medical Genetics Board of Directors, 1995; Committee on Bioethics et al., 2013; Human Genetics Society of Australasia, 2008; Italian National Bioethics Committee, 1999; Ross et al., Reference Ross, Saal, David and Anderson2013). These guidelines and position statements raise several concerns:
-
The potential for negative psychosocial impacts for the child.
-
Failing to protect the future autonomy of the child by removing both their right to decide for themselves once they are able to, and their right not to know their carrier status.
-
The potential for harm created by parental guilt, anxiety, misunderstandings about their child’s health, failure to disclose the result to the child, or social impacts, such as discrimination or stigmatization.
Evidence regarding whether these concerns are warranted is limited due to a paucity in empirical studies assessing the outcomes from performing carrier testing in children. Despite this, reviews of the existing literature, the majority of which relates to families with X-linked conditions, have suggested that overall, there is no evidence of psychosocial harm from carrier testing in childhood (Wade et al., Reference Wade, Wilfond and McBride2010; Vears & Metcalfe, Reference Vears and Metcalfe2015).
Some guidelines suggest there may be circumstances where testing young people might be appropriate.
-
When a young person is an independent minor (i.e., pregnant or living independently) (American Society of Human Genetics Board of Directors and American College of Medical Genetics Board of Directors, 1995; Ross et al., Reference Ross, Saal, David and Anderson2013).
-
When a young person self-requests testing and clearly understands the implications of the information they will receive (i.e., they meet the criteria to be classified as a mature minor, e.g., Gillick competence) (Canadian College of Medical Geneticists, 2000).
-
When a positive carrier status could be associated with health implications (e.g., X-linked conditions such as hemophilia where XX carriers can have clotting issues; American Society of Human Genetics Board of Directors and American College of Medical Genetics Board of Directors; Italian National Bioethics Committee, 1999).
-
When declining to provide testing is causing significant parental anxiety and distress, which is inhibiting family functioning. (British Medical Association, 1998; Dalby, Reference Dalby1995)
It is recognized that parents are usually best placed to make decisions for their children and should therefore be allowed to determine whether they want carrier testing performed for them, provided there is minimal likelihood of harm and they have undergone genetic counseling (British Medical Association Ethics Department, 2012). This is also based on the fact that it is more common for carriers to be identified in childhood than it was in the past and genetic literacy has also increased (British Medical Association Ethics Department, 2012).
Advantages and disadvantages to performing carrier testing in children
Research suggests there may be benefit from performing carrier testing in childhood in some situations (Vears & Metcalfe, Reference Vears and Metcalfe2015). Studies show that parents want to know their child’s carrier status so that they can communicate the information to them during childhood, avoiding the shock of the child finding out when they are older and preparing them with knowledge of their reproductive options (Barnes, Reference Barnes and Clarke1998; Thomas et al., Reference Thomas, Herbert, Street, Barnes, Boal and Komesaroff2007; Vears et al., Reference Vears, Delany, Massie and Gillam2016). Testing in childhood may also allow children to integrate the knowledge of their carrier status into their concept of self, which may, in turn, reduce the perceived threat to the child’s future parental role, reducing associated psychological distress (McConkie-Rosell & DeVellis, Reference McConkie-Rosell and DeVellis2000).
The counter argument to this is that testing is not always required to achieve these outcomes; parents can still communicate to the young person that there is a condition in the family and explain that they can request carrier testing when they are older. However, in some situations, living with the uncertainty of whether they are a carrier or not can create anxiety for the young person and their family. Further research to examine both the short- and long-term outcomes of carrier testing in childhood and young people is needed, particularly with regards to whether and how disclosure of carrier status to children occurs (when testing is performed) and whether and how a condition is discussed in a family (when testing is not undertaken).
Genetic Counseling of Children and Young People Requesting Carrier Testing
Genetic counseling is critical in all cases where the family or young person is requesting carrier testing for someone under the age of majority. Such testing should only be ordered by a genetic health professional.
Importantly, rather than refusing a request for carrier testing in a child or young person, it is critical to engage parents and/or the young person themselves in a dialogue about why they wish to know their child’s carrier status. This may be an opportunity to correct any misunderstandings the parents (or young person) may have about the health of their child (or themselves) and help them think through whether testing at that point in time is in the best interests of the child or young person, as well as the family as a whole. As carrier results generally will not change health management, the decision about whether testing takes place is not time-critical and can be revisited in the future, allowing more time to consider the decision. If situations arise where there is disagreement about carrier testing between a young person and their parents, the health professional’s role should be to advocate for the young person, whilst recognizing family dynamics. Counseling should be provided to both the young person and the family, separately and together.
Acknowledgments
We thank the working group for this position statement: Danya Vears, Jackie Boyle, Chris Jacobs, Aideen McInerney-Leo and Ainsley Newson. We also acknowledge the additional members of the Education, Ethics, and Social Issues Committee of the Human Genetics Society of Australasia: Amy Nisselle, Julia Mansour, Bronwyn Terrill, Sam Ayers, Heather Renton, Dylan Mourdant, Michael Gabbett, Rebekah McWhirter, Fiona Lynch and Jacqueline Savard. This statement was reviewed and approved by the HGSA Council in July 2022.
Financial support
During this project A.M.L. held an NHMRC Early Career Fellowship (APP1158111) and is currently supported by a University of Queensland Faculty of Medicine Fellowship.
Conflict of interest
None.
Ethical standards
Not applicable.