Introduction
When parents develop health limitations adult children often take on support tasks in response (Silverstein et al., Reference Silverstein, Gans and Yang2006; Blomgren et al., Reference Blomgren, Breeze, Koskinen and Martikainen2012). The extent to which adult children feel compelled to do this and the impact that care-giving has on their lives may depend on the long-term care (LTC) context. In many European countries, and in particular in those that were traditionally characterised by generous state provision of LTC services, responsibilities for the care of older persons with health limitations have increasingly been shifted from the state to informal networks, most notably the family (Pavolini and Ranci, Reference Pavolini and Ranci2008; Ranci and Pavolini, Reference Ranci and Pavolini2015). Given that providing informal care is associated with a wide range of economic and non-economic costs (Fast et al., Reference Fast, Williamson and Keating1999), it has been argued that shifting care responsibilities from the state to the family would better be framed as cost redistribution than as cost-containment, and that policy makers should take into account the implications of informal care-giving for the lives of those engaged in it (Kotsadam, Reference Kotsadam2011; Van den Broek, Reference Van den Broek2013). The aim of the current study is to shed light on how the coverage of home-based LTC services may shape changes in quality of life that may occur when people become care providers for their ageing parents.
When care is more highly de-familialised, that is, when affordable state-supported care services are more widely available, there is arguably less pressure on family members to take on care tasks (Saraceno, Reference Saraceno2010), and care-giving may thus be more a matter of choice. This may mean that any negative impacts of care-giving on wellbeing are less pronounced (Verbakel, Reference Verbakel2014). Testing whether this is the case is a challenging affair, however. A common approach to estimate how the organisation of LTC shapes the impact of informal care-giving is to compare whether this impact varies between countries that have different LTC coverage, but this approach leaves considerable room for omitted variable bias. The country differences in LTC coverage often coincide with various other cultural, economic, demographic and policy differences between countries that may also influence the implications of informal care provision for people's lives. Consequently, it remains unclear what factors effectively drive country differences in the impact of informal care-giving.
As considered in further detail later, our approach differs from earlier work on the potential moderating impact of LTC coverage on the implications of informal care-giving. We use individual fixed-effects regression analyses to reduce omitted variable bias in the estimates of the effects of informal care-giving on care-givers’ quality of life,Footnote 1 and combine this with a difference-in-difference approach to reduce omitted variable bias in the estimated impact of LTC coverage on these effects. We draw on longitudinal data for Sweden and Denmark from the Survey of Health, Ageing and Retirement in Europe (SHARE) collected between 2004 and 2015. Both countries have traditionally tended to be presented as countries where the coverage of LTC services is markedly more generous than elsewhere in Europe (e.g. Anttonen and Sipilä, Reference Anttonen and Sipilä1996). However, substantial cutbacks in LTC services were implemented at the end of the 20th century in Sweden and more recently in Denmark. We use this country difference in the timing of the LTC cutbacks to shed light on possible effects of the availability of state-supported LTC services on the impact of care-giving on quality of life.
Care for older people in Sweden and Denmark
Sweden and Denmark were among the first countries in Europe to recognise the need for LTC as a social risk requiring welfare state intervention (Österle and Rothgang, Reference Österle, Rothgang, Castles, Leibfried, Lewis, Obinger, Pierson, Österle and Rothgang2010). In the middle of the 20th century, both countries adopted a universalistic LTC system centred on the wide availability of affordable, state-supported services for all residents in need of care (Österle and Rothgang, Reference Österle, Rothgang, Castles, Leibfried, Lewis, Obinger, Pierson, Österle and Rothgang2010; Colombo, Reference Colombo, Costa-Font and Courbage2012). Early care regime typologies, most of which drew on data from the 1980s and 1990s, usually clustered Sweden and Denmark together and presented them as being among the countries where the coverage of care services was the most generous in Europe (Anttonen and Sipilä, Reference Anttonen and Sipilä1996; Leitner, Reference Leitner2003; Bettio and Plantenga, Reference Bettio and Plantenga2004). Anttonen and Sipilä (Reference Anttonen and Sipilä1996) speak of a Scandinavian model of public services.
Rauch (Reference Rauch2007), however, questioned whether such a categorisation was still appropriate for Sweden by the early 21st century. With the 1992 Ädel reform, the responsibility of Swedish municipalities for the provision of LTC was expanded. Municipalities had to take over the responsibility for patients treated in hospital within three days after they had been assessed as being well enough to be discharged, with non-compliant municipalities having to pay high hospital fees as a penalty (Lofgren, Reference Lofgren2002). The Ädel reform meant that increasing numbers of older people with high care needs turned to Swedish municipalities whose budgets were already strained (Meagher and Szebehely, Reference Meagher, Szebehely, Ranci and Pavolini2013). Given that rules about entitlement to care services were weaker in Sweden than in Denmark, Swedish municipalities could be increasingly restrictive with regard to the provision of care services, whereas Danish municipalities were prevented from doing this (Rauch, Reference Rauch2008). In Sweden, care services were increasingly targeted at those in the most severe need and co-payments from persons with less-severe care needs were increased (Sundström and Johansson, Reference Sundström and Johansson2005; Pavolini and Ranci, Reference Pavolini and Ranci2008; Johansson et al., Reference Johansson, Long and Parker2011). Consequently, older Swedes became less likely to receive state-supported home care services between the late 1990s and the early 2000s, and this could not be accounted for by improved health status of the later cohorts of older people (Larsson, Reference Larsson2006; cf. Meagher and Szebehely, Reference Meagher, Szebehely, Ranci and Pavolini2013). In Denmark, in contrast, coverage levels and eligibility criteria for home-based LTC services remained largely unchanged (Rauch, Reference Rauch2008; Burau and Dahl, Reference Burau, Dahl, Ranci and Pavolini2013).
More recently, LTC provision in Denmark and Sweden has become more similar again, albeit in a markedly different way than in the 1980s. Following Sweden, Denmark also started to move away from the ideal-type of the Scandinavian model of public services as described by Anttonen and Sipilä (Reference Anttonen and Sipilä1996). Recent changes in LTC coverage have been more pronounced in Denmark than in Sweden. Szebehely and Meagher (Reference Szebehely and Meagher2018: 4) noted that Danish municipalities ‘started to interpret the (unchanged) legislation in a more restrictive way’. They were further encouraged to do so by a 2011 court ruling confirming that under specific circumstances municipalities had the right to stop providing home care services to older persons who previously received home care, but no longer met tightened eligibility criteria (Szebehely and Meagher, Reference Szebehely and Meagher2018: 4). In contrast, Sweden has recently seen a slight increase in home care coverage, although this is likely related to continuing de-institutionalisation, i.e. an increased emphasis on home-based care services rather than on care provided in institutions, which resulted in strong declines in the availability of beds in residential care settings in Sweden (Ulmanen and Szebehely, Reference Ulmanen and Szebehely2015; Szebehely and Meagher, Reference Szebehely and Meagher2018). Similar declines in the availability of residential care took place in Denmark and other Nordic countries (Szebehely and Meagher, Reference Szebehely and Meagher2018).
The impact of the changes in home care coverage is evident in the proportions of older people receiving home-based LTC services. As shown in Figure 1, Organisation for Economic Co-operation and Development data indicate that utilisation of formal home care services (either publicly or privately financed) among the population aged 65 and older was around 3 percentage points higher in Denmark than in Sweden around the year 2000. Twelve years later, however, the country difference had disappeared.Footnote 2
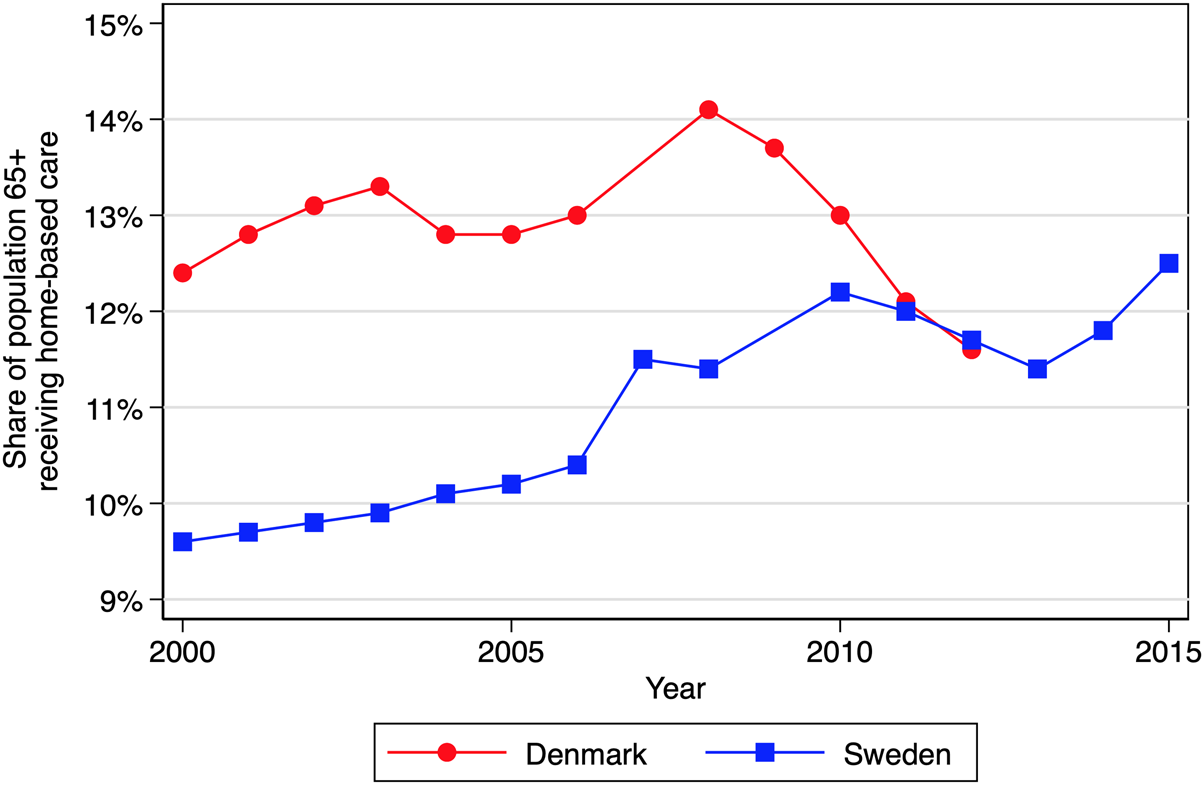
Figure 1. Home care services utilisation.
Theoretical background and hypotheses
Although providing care to ageing parents can be rewarding (Cohen et al., Reference Cohen, Colantonio and Vernich2002), it is also potentially stressful. Care-giving stress may stem directly from the care recipients’ health limitations and the extent and type of care needed, as well as indirectly through intra-psychic strains caused by changes in the care-giver's self-perception or through conflicts that may arise between care-giving and, for instance, other family or work responsibilities (Pearlin et al., Reference Pearlin, Mullan, Semple and Skaff1990). Given that stress is known to be detrimental for quality of life (Litzelman et al., Reference Litzelman, Skinner, Gangnon, Nieto, Malecki and Witt2014), we expect that becoming a care-giver for ageing parents is negatively associated with quality of life (Hypothesis 1).
Research suggests that informal care-giving is particularly detrimental for wellbeing when care-givers perceive a lack of choice in taking on the care-giving role (Schulz et al., Reference Schulz, Beach, Cook, Martire, Tomlinson and Monin2012). Pearlin et al. (Reference Pearlin, Mullan, Semple and Skaff1990) argued that so-called role captivity, i.e. the feeling of being compelled to engage in care-giving against one's will, is an important source of care-giver stress. Consistent with this reasoning, previous research has shown that care-givers report relatively high levels of anxiety and depressive symptoms when they resent having to care for a frail older relative (Aggar et al., Reference Aggar, Ronaldson and Cameron2011).
The extent to which the decision to take on care tasks is a matter of choice is arguably partly dependent on how LTC is organised. Leitner's (Reference Leitner2003) typology of care systems is useful here. She distinguished countries by the extent to which they provide services that relieve families of the need to provide care to relatives and by the extent to which they support care-giving family members. Care-giving is assumed to be least burdensome in countries in the so-called optional familialism cluster and most burdensome in countries in the so-called implicit familialism cluster. In the former cluster, people are not strongly pressed to provide care to relatives in need, because state-supported LTC services are widely available, and those who choose to take on the care-giver role are supported, for instance through the availability of care leave arrangements, pension rights and/or cash benefits. In the latter cluster the situation for family members of older persons with care needs is the exact opposite. Here, LTC services coverage is low, effectively leaving the family few options but to take on caring responsibilities. Moreover, policies supporting family members engaged in the provision of care are lacking.
Drawing on data from the 1990s, Leitner (Reference Leitner2003) placed both Denmark and Sweden in the optional familialism cluster. However, as described earlier, already by the early 2000s Sweden had moved away from the optional familialism way of organising LTC, given the country's cutbacks in LTC services in the 1990s (Rauch, Reference Rauch2007; Rostgaard and Szebehely, Reference Rostgaard and Szebehely2012). In the early 2000s, coverage of state-supported home care services was more extensive in Denmark than in Sweden (Rauch, Reference Rauch2007; Saraceno, Reference Saraceno2010; Rostgaard and Szebehely, Reference Rostgaard and Szebehely2012). This may have made care-giving more a matter of choice and consequently potentially less stressful in the former country than in the latter. Also, care-giving adult children may provide care less frequently (Schmid et al., Reference Schmid, Brandt and Haberkern2012) or take on less onerous care tasks (Brandt et al., Reference Brandt, Haberkern and Szydlik2009) when care-giving responsibilities can be shared with formal care-givers. We therefore expect any negative association between becoming a care-giver for ageing parents and quality of life to be stronger in Sweden than in Denmark (Hypothesis 2).
As described earlier, Szebehely and Meagher (Reference Szebehely and Meagher2018) showed that the move away from the optional familialism ideal type as formulated by Leitner (Reference Leitner2003) in Sweden mainly took place in the 1990s and stagnated around the turn of the century. In Denmark, in contrast, cutbacks in care services, and thus a move away from optional familialism, were only implemented more recently. This suggests that differences between Denmark and Sweden in the extent to which care-giving can be perceived as a matter of choice may have shrunk, which, in turn, leads us to hypothesise that the difference between both countries in the impact of the transition to the care-giver role on quality of life has become smaller over the course of the 21st century (Hypothesis 3).
Data
Sample
This study draws on data from Waves 1, 2, 4, 5 and 6 of SHARE (Börsch-Supan et al., Reference Börsch-Supan, Brandt, Hunkler, Kneip, Korbmacher, Malter, Schaan, Stuck and Zuber2013). SHARE is a longitudinal, cross-national data-set on the health, socio-economic status and social relations of older Europeans. Data collection for the waves used in the current study took place in 2004–2005 (Wave 1), 2006–2007 (Wave 2), 2011 (Wave 4), 2013 (Wave 5) and 2015 (Wave 6). We limited our sample to Swedish and Danish men and women aged 50–75 who had at least one living parent in both Waves 1 and 2 or in both Waves 4 and 5 or in both Waves 5 and 6. For each respondent in our sample we thus have two observations. These selection criteria resulted in a sample of 5,450 observations nested in 2,725 women and men. Supplied calibrated longitudinal weights were used to adjust for bias arising from non-response and attrition.Footnote 3 There were 454 respondents present in multiple sub-samples (Waves 1–2; Waves 4–5; Waves 5–6). We treated them as different persons and estimated all models with robust standard errors.Footnote 4
Measures
Quality of life, i.e. ‘the degree to which human needs are satisfied’ (Hyde et al., Reference Hyde, Wiggins, Higgs and Blane2003: 187), was measured with the CASP-12 instrument. CASP-12 is a shortened version of the validated CASP-19 measure of quality of life developed by Hyde et al. (Reference Hyde, Wiggins, Higgs and Blane2003) and captures four sub-dimensions of quality of life: control (C), autonomy (A), self-realisation (S) and pleasure (P). Each item of the CASP-12 consists of a statement about respondents’ current lives or feelings, and respondents were asked to answer how often, if at all, the statement applied to them on a four-point scale ranging from ‘never’ to ‘often’.Footnote 5 A summed scale ranging from 12 to 48 was generated, with higher scores indicating better quality of life. In line with what has been reported in earlier work using the CASP-12 measure (Von dem Knesebeck et al., Reference Von dem Knesebeck, Wahrendorf, Hyde and Siegrist2007), a reliability test indicated that the internal consistency of the shortened version of CASP was high in our sample (Cronbach's α = 0.79).
Care provision to parents was measured with a dichotomous variable capturing whether or not the respondent reported having provided personal care or practical household help to a father and/or mother in less than good health during the last 12 months. Parental fair or poor health was included as a condition to acknowledge what Walker et al. (Reference Walker, Pratt and Eddy1995) call the criterion of dependence, i.e. the notion that assistance can only be labelled care as opposed to aid when the recipient is unable to perform autonomously the everyday task for which support is received. This implies that older parents can only receive informal care when they have functional limitations. Unfortunately, information on whether or not respondents’ parents had functional limitations was not available in our data, so we had to use the child's report that the parent's health was ‘poor’ or ‘fair’ as opposed to ‘good’, ‘very good’ or ‘excellent’ as a proxy for parental functional limitations. When respondents provided care at the first observation, but not at the second observation, they were coded as ex-care-givers, rather than as non-care-givers at the second observation. In selected analyses, we distinguished between sporadic and frequent care provision. Care to ageing parents was coded as frequent when respondents reported that they provided it ‘about daily’ or ‘about every week’ and as sporadic when care was provided less often.
In all models we included a range of time-varying control variables (age, partnership status and employment status) known to be associated with the likelihood of becoming a care-giver (Haberkern and Szydlik, Reference Haberkern and Szydlik2010; Leopold et al., Reference Leopold, Raab and Engelhardt2014; Van den Broek and Dykstra, Reference Van den Broek and Dykstra2017; Van den Broek et al., Reference Van den Broek, Dykstra and Van der Veen2019), as well as with quality of life and mental wellbeing (Zaninotto et al., Reference Zaninotto, Falaschetti and Sacker2009; Jivraj et al., Reference Jivraj, Nazroo, Vanhoutte and Chandola2014; Gibney et al., Reference Gibney, Delaney, Codd and Fahey2017; Grundy et al., Reference Grundy, Van den Broek and Keenan2017). We distinguished five age groups: (a) 50–54 years old, (b) 55–59 years old, (c) 60–64 years old, (d) 65–69 years old and (e) 70–75 years old. Partnership status was measured with a dummy variable that distinguished between respondents who lived with a partner and their counterparts who did not. Employment status was measured with a dummy variable distinguishing respondents who reported that their current situation was best described as ‘employed or self-employed (including working for family business)’, rather than ‘retired’, ‘unemployed’, ‘permanently sick or disabled’, ‘homemaker’ or ‘other’.
We also included a dichotomous variable distinguishing adult children with both parents still alive from those who had only one living parent. We did so, because when both parents are still alive and together, the other partner is typically first in line to take on care tasks (Shanas, Reference Shanas1979; Messeri et al., Reference Messeri, Silverstein and Litwak1993; Jacobs et al., Reference Jacobs, Broese van Groenou, Aartsen and Deeg2018), and parental loss is associated with declines in the mental wellbeing of adult children (Scharlach and Fredriksen, Reference Scharlach and Fredriksen1993; Leopold and Lechner, Reference Leopold and Lechner2015).
Our definition of care-giving requires that the parent to which the child provides assistance is in less than good health, and several studies have shown that parental health limitations are associated with poorer mental wellbeing of their children, regardless of whether or not care is provided to the parent (Amirkhanyan and Wolf, Reference Amirkhanyan and Wolf2006; Wolf et al., Reference Wolf, Raissian and Grundy2015; Van den Broek and Grundy, Reference Van den Broek and Grundy2018). We therefore included a dummy variable indicating that at least one living parent reportedly had ‘fair’ or ‘poor’ health, as opposed to ‘excellent’, ‘very good’ or ‘good’ health.
Two observations were available for every respondent in our sample. We included a dichotomous variable to distinguish between first observations and second observations.
Missing values
In our sample, 1,231 observations (22.6%) had missing values on at least one variable of interest: CASP-12 (N = 281), care-giver status (N = 806), parental health limitations (N = 151) or employment status (N = 23). Values on our quality of life measure, CASP-12, were particularly likely to be missing in Wave 1 (N = 212), when the items were collected as part of the individual paper questionnaire, rather than as part of the computer-assisted personal interviews. Wave 4 (N = 189) and Wave 5 (N = 613) had large numbers of missing values on care-giver status. This was because in these waves questions about informal care-giving were only asked of so-called family respondents.
To deal with this missing information, we used multiple imputation with chained equations under the missing at random assumption (Young and Johnson, Reference Young and Johnson2015). This means that we assume that any differences between the distributions of missing values and the distributions of observed values can be explained by variables included in the imputation model (Bhaskaran and Smeeth, Reference Bhaskaran and Smeeth2014). Imputations were conducted in wide data format (cf. Young and Johnson, Reference Young and Johnson2015). Separate imputation models were estimated by country and period. Time-invariant ancillary variables included in the imputation models were gender, number of siblings, number of children and educational attainment measured at baseline. Education was measured with a categorical variable, whereby we distinguished low (International Standard Classification of Education (ISCED) 0–2; pre-primary to lower secondary education), medium (ISCED 3–4; upper secondary to post-secondary non-tertiary education) and high (ISCED 5–6; tertiary education) levels of educational attainment. The findings from the substantive analyses on 20 imputed data-sets were combined into a single set of results following Rubin's rules (Little and Rubin, Reference Little and Rubin1989), which take the variability in results between the imputed data-sets into account.
Method
We estimated fixed-effects linear regression models to study intra-individual change in mid-life persons’ quality of life. We started by estimating a straightforward model, such as depicted in Equation (1):
 $${\ddot y}_{it} = \beta_{1} {\ddot S}_{it} + \beta_{2} {\ddot X}_{it} + {\ddot e}_{it}$$
$${\ddot y}_{it} = \beta_{1} {\ddot S}_{it} + \beta_{2} {\ddot X}_{it} + {\ddot e}_{it}$$Where
 $${\ddot y}_{it} = y_{it} - \bar y_i$$
$${\ddot y}_{it} = y_{it} - \bar y_i$$ $${\ddot S}_{it} = S_{it} - \bar S_i$$
$${\ddot S}_{it} = S_{it} - \bar S_i$$ $${\ddot X} _{it} = X_{it} - \bar X_i$$
$${\ddot X} _{it} = X_{it} - \bar X_i$$ $${\ddot e}_{it} = e_{it} - \bar e_i$$
$${\ddot e}_{it} = e_{it} - \bar e_i$$Equations (2)–(5) indicate that for the outcome variable y (quality of life), main explanatory variable S (care-giver status), time-varying covariates X and the error term e, we deducted the mean score for individual i over both time-points from the score for individual i on time-point t. This procedure implies that we regressed temporal variation in quality of life within individuals on within-individual change in care-giver status and the control variables. Consequently, all time-invariant characteristics, including those not observed, were accounted for (Allison, Reference Allison2009). This makes our estimates of the effects of providing care to ageing parents on quality of life not prone to bias due to omitted variables that are constant over time (Taylor et al., Reference Taylor, Ford and Dunbar1995; Kaschowitz and Brandt, Reference Kaschowitz and Brandt2017; Van den Broek and Grundy, Reference Van den Broek and Grundy2018).
To test whether the association between providing care to ageing parents and quality of life was more strongly negative in Sweden than in Denmark, we estimated a model in which we allowed the effect of the transition to the role of care provider to vary by country C (Denmark versus Sweden), which is time invariant.
 $${\ddot y}_{it} = \beta _1 {\ddot S}_{it} + \beta _2{\ddot X}_{it} + \beta _3C_i {\ddot S}_{it} + {\ddot e} _{it}$$
$${\ddot y}_{it} = \beta _1 {\ddot S}_{it} + \beta _2{\ddot X}_{it} + \beta _3C_i {\ddot S}_{it} + {\ddot e} _{it}$$In the final model, we combined the fixed-effects approach with a difference-in-difference strategy. The effect of change in care-giver status on change in quality of life was allowed to vary not only as a function of country C, but also as a function of period P (2011–2015 versus 2004–2007, also time invariant) and as a function of the interaction between the two:
 $${\ddot y}_{it} = \beta _1 {\ddot S}{it} + \beta _{2} {\ddot X}_{it} + \beta _3C_i {\ddot S}_{it} + \beta _4P_i {\ddot S}_{it} + \beta _5C_iP_i {\ddot S}_{it} + {\ddot e}_{it}$$
$${\ddot y}_{it} = \beta _1 {\ddot S}{it} + \beta _{2} {\ddot X}_{it} + \beta _3C_i {\ddot S}_{it} + \beta _4P_i {\ddot S}_{it} + \beta _5C_iP_i {\ddot S}_{it} + {\ddot e}_{it}$$where β 5 denotes the estimates in which we are most interested. It captures the estimated change over the two considered time periods in the difference between the two considered countries in the effect of change in care-giver status on change in quality of life. This approach leaves less room for bias in the estimates of the moderating effects of contextual factors due to the presence of omitted higher-level confounding factors than is the case in country comparisons at a single point in time (or multiple, pooled time-points), commonly used in previous studies. In traditional country comparisons, any omitted variable associated with the country-level moderator variable of interest – in our case LTC coverage – may be a confounder of the estimated moderating effect. In our approach, country characteristics omitted from the model as moderator variables can only lead to biased estimates if they develop differently in Sweden and Denmark over the considered time-frame (cf. Angrist and Pischke, Reference Angrist and Pischke2009; Lechner, Reference Lechner2011). Omitted country characteristics that are constant over time or that vary similarly over time in both countries may influence the estimated stable country differences in the impact of change in care-giver status on change in quality of life (β 3 ), but not our main coefficients of interest (β 5). All models were estimated with robust standard errors (White, Reference White1980).
Results
Descriptive results are presented in Table 1. Quality of life was higher among members of the Danish than the Swedish sample (F(1, 5448) = 85.4, p < 0.001). Although coverage of state-supported home care services was more extensive in Denmark than in Sweden for most of the period studied, the proportion of adult children providing care to ageing parents did not differ substantially between countries (cf. Verbakel et al., Reference Verbakel, Tamlagsrønning, Winstone, Fjær and Eikemo2017). Also, the share of respondents that made a transition from non-care-giver to care-giver or from care-giver to ex-care-giver did not vary substantially across the two countries (see Appendix A in the online supplementary material).
Table 1. Sample characteristics

Notes: Multiple imputation using chained equations was used to deal with missing values. Data are weighted.
Source: Survey of Health, Ageing and Retirement in Europe (SHARE), Waves 1, 2, 4, 5 and 6.
Results of our fixed-effects regression analyses of quality of life are presented in Table 2. Consistent with our first hypothesis, the first model shows that starting to provide care to ageing parents was associated with a reduction in quality of life. Possibly because it may take time to recover from the hardships associated with care-giving, transition from care-giver to ex-care-giver was not associated with a significant increase in quality of life (Δb = 0.46, p = 0.30).Footnote 6 Being in the 60–64 or the 65–69 age group, as opposed to the 50–54 age group, was associated with better quality of life. No significant effects were found for any of the other explanatory variables included in the model.
Table 2. Results of fixed-effects regression analyses of quality of life (CASP-12)

Notes: N = 5,450. Multiple imputation using chained equations was used to deal with missing values. Data are weighed. SE: robust standard errors. Ref.: reference category.
Source: Survey of Health, Ageing and Retirement in Europe (SHARE), Waves 1, 2, 4, 5 and 6.
Significance levels: * p < 0.05, ** p < 0.01.
In the second model, we allowed the effects of care-giver status transitions to differ between Denmark and Sweden by adding an interaction term. The model shows a marked negative effect of care provision on quality of life in Sweden. The significant interaction term (current care-giver × Denmark) indicates support for our second hypothesis: the negative effect of becoming a care-giver was markedly weaker in Denmark than in Sweden. The effect of care provision was in fact not statistically significant in Denmark (b = 0.30, p = 0.84).
In an additional model (not shown in Table 2; see Appendix B in the online supplementary material), we included two three-way interaction terms (current care-giver × country × period; ex-care-giver × country × period) to test whether the country differences in the effects of care provision have become smaller over time. Figure 2 shows the size of the estimated effect of a transition to care-giving on quality of life by country and period based on the three-way interaction model. The figure shows convergence over time between Sweden and Denmark in the impact of becoming a care-giver. The estimated effect of becoming a care-giver was more strongly negative in Sweden than in Denmark (b = −2.59, p < 0.01) in the 2004–2007 period. In the 2011–2015 period (Waves 4–6), the country difference in the estimated effect was smaller and no longer statistically significant (Δb = −0.70, p = 0.13). The difference-in-difference estimate, i.e. the change between Period 1 (2004–2007) and Period 2 (2011–2015) in the country difference in the estimated effect of becoming a care-giver on quality of life, was statistically significant (ΔΔb = 1.89, p < 0.05). This is consistent with our third hypothesis that the difference between Sweden and Denmark in the effect of providing care to ageing parents on quality of life was smaller in the 2011–2015 period than in the 2004–2007 period, and suggests that LTC coverage shapes the impact of informal care-giving on quality of life.

Figure 2. Estimated impact of care provision to ageing parents on quality of life.
Given that the frequent provision of care might be more burdensome and so more detrimental for quality of life than sporadic provision of care (cf. Pinquart and Sörensen, Reference Pinquart and Sörensen2003; Verbakel et al., Reference Verbakel, Tamlagsrønning, Winstone, Fjær and Eikemo2017), we distinguished between at least weekly care provision and less frequent provision of care in Model 3 (see Table 2). However, the differences between frequent and sporadic care provision in the estimated impact on quality of life were negligible and not statistically significant in either Sweden (Δb = −0.18, p = 0.70) or Denmark (Δb = −0.16, p = 0.71).
In the models presented here, we did not adjust for respondents’ own health, because this arguably could be considered a so-called ‘bad control’. Research suggests that providing informal care can be detrimental for adult children's own health (Coe and Van Houtven, Reference Coe and Van Houtven2009), and this may, in turn, result in declines in quality of life. Adjusting for respondents’ own health may thus lead to under-estimation of the full effect of informal care provision. However, own poor health may also be a reason for not taking on care tasks. As a robustness check, we therefore re-estimated Models 1–3, additionally adjusting for respondents’ own health measured with a dichotomous variable for ‘fair’ or ‘poor’ versus ‘excellent’, ‘very good’ or ‘good’ self-reported overall health. These models (full results available on request) show that a transition from good to less than good self-rated health was associated with a marked decline in quality of life. The estimates of effects of becoming a care-giver did not change substantially, however, after the addition to the models of respondents’ own self-rated health. This suggests that mechanisms other than care-giving-induced declines in adult children's own self-rated health underlie the detrimental effect of becoming a care-giver on quality of life.
In the models presented in Table 2, the effects of care-giving on quality of life were constrained to be similar for men and women. We re-estimated these models, allowing the effects of care-giving and, in Models 2 and 3, the country differences in these effects to vary by gender (not shown in Table 2; full results available on request), to test whether it was problematic to assume the absence of gender differences in the impact of care-giving on quality of life. These additional analyses did not provide evidence that this was the case, as Wald tests indicated that neither the addition of a gender interaction (care-giver status × gender) to Model 1, nor the addition of three-way interaction terms to Model 2 or Model 3, was statistically significant.
Discussion
When affordable state-supported care services are more widely available, there is arguably less pressure on family members to provide care to ageing relatives with health limitations, which may mean that care-giving has less of an impact on care-givers’ wellbeing. In the current study, we investigated the impact of providing care to ageing parents on adult children's quality of life in Sweden and Denmark. Both countries were traditionally characterised by generous LTC coverage, but in the 1990s in Sweden and more recently in Denmark there has been substantial retrenchment of provision.
Our approach differs from earlier studies on the ways in which LTC coverage might shape the implications of informal care-giving. Often, the effects of formal LTC arrangements on the impact of care-giving on wellbeing and quality of life are analysed using country comparisons at a single point in time, or at multiple, pooled time-points. In such an approach it is assumed that in the absence of the difference in the way LTC is organised, the effects of care-giving on wellbeing and quality of life would be identical across countries. This is a rather bold assumption, given that country differences in LTC policy arrangements often coincide with various cultural, economic, demographic and policy differences between countries that may also influence the implications of informal care provision for people's lives. Verbakel (Reference Verbakel2014: 426), who showed that the difference in happiness between people who provided informal care and people who did not was smaller in countries with more generous formal LTC resources, acknowledged that she could ‘not be conclusive regarding whether it is truly the national policy measure that reduces negative well-being consequences of informal caregiving’. We used individual fixed-effects regression analyses to reduce omitted variable bias in the estimates of the effects of informal care-giving, and combine this with a difference-in-difference approach to reduce omitted variable bias in the estimated impact of LTC coverage on these effects. Consequently, our assumptions when estimating the impact of LTC coverage on the implications of care-giving are relatively weak: we assume that in the absence of country differences in the change in LTC coverage, the difference between Sweden and Denmark in the effect of change in care-giver status on quality of life would be constant across periods.
As hypothesised, our analyses show that care-giving was more detrimental for quality of life in Sweden than in Denmark. In fact, no significant impact of care-giving on quality of life was found in Denmark. Moreover, we showed that the country difference in the effect of care-giving on quality of life weakened significantly when LTC coverage was reduced in Denmark, but not in Sweden. Given the relatively weak assumptions underlying our analyses, this result provides evidence that LTC coverage shapes the impact of care-giving on quality of life.
It should be noted that we had to use a somewhat crude measure of care provision. In selected analyses, we distinguished between care provided at least weekly and care provided less often. We could not, however, take into account the time spent on care-giving, because this information was not collected in Waves 4–6 of SHARE. This is unfortunate, because research has shown that care-giving is considered more burdensome when more hours per week are spent on care-giving (Pinquart and Sörensen, Reference Pinquart and Sörensen2003). Also, we could not distinguish between household chores, such as cleaning the house and grocery shopping, and personal care tasks, such as help with bathing or dressing. This is because in Waves 4 and 5 of SHARE the question about the types of assistance was omitted. Given that the latter tasks are more intensive and less routine than the former (Walker et al., Reference Walker, Pratt and Eddy1995), they may also be more detrimental for quality of life. Furthermore, our difference-in-difference approach was based on aggregate trends of LTC coverage in Sweden and Denmark, with substantial cutbacks occurring in the 1990s in the former country and more recently in the latter country. Given the autonomy of municipalities, particularly in Sweden, local deviations from these aggregate trends are likely. However, reliable time-series data at the municipality level is, to our best knowledge, not available (cf. Schön and Johansson, Reference Schön and Johansson2016).
The current study may also be relevant for researchers interested in topics other than LTC, informal care-giving or intergenerational support exchanges. The fact that the small number of countries available in most cross-national data-sets limits the number of cross-level interaction terms that can be included in statistical models is a problem with which scholars interested in a wide range of different topics have been grappling. For some of these scholars, our approach of combining fixed-effects analyses with a difference-in-difference approach may provide a useful blueprint of how the impact of a country characteristic on the implications of a transition from one state to another at the individual level could be modelled in a way that limits room for omitted variable bias.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0144686X18001708.
Data
This paper uses data from SHARE Waves 1, 2, 4, 5 and 6 (DOIs: 10.6103/SHARE.w1.600, 10.6103/SHARE.w2.600, 10.6103/SHARE.w5.600, 10.6103/SHARE.w6.600), see Börsch-Supan et al. (Reference Börsch-Supan, Brandt, Hunkler, Kneip, Korbmacher, Malter, Schaan, Stuck and Zuber2013) for methodological details. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: No. 211909, SHARE-LEAP: No. 227822, SHARE M4: No. 261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the US National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Financial support
The research leading to these results has received funding from the European Research Council under the European Union's Seventh Framework Programme (FP7/2007-2013)/ERC Grant Agreement No. 324055 (FAMHEALTH).
Ethical standards
Not applicable.






