Introduction
A growing body of evidence suggests that lung ultrasound can be a useful procedure for assessing patients with respiratory complaints. The most well-known study of this is the “BLUE Protocol,” reported by Lichtenstein in 2008. This study found that lung ultrasound in the intensive care unit was highly accurate in differentiating causes of respiratory failure, including congestive heart failure, pneumothorax, acute respiratory distress syndrome, and pneumonia.Reference Lichtenstein and Meziere 1 Subsequent to this report, numerous studies have shown that emergency physicians can accurately apply lung ultrasound in the emergency department (ED). Zanobetti et al. found that in 404 ED patients presenting with acute dyspnea, point-of-care ultrasound (PoCUS) was on average 95 minutes faster than a chest x-ray, and had a higher agreement rate with chest CT findings than did chest x-ray.Reference Zanobetti, Poggioni and Pini 2 PoCUS for pneumonia is also well studied. In a recent systematic review comparing ultrasound with chest CT, lung ultrasound in adults was found to have a sensitivity of 94% and a specificity of 96% for pneumonia.Reference Chavez, Shams and Ellington 3 For patients arriving with undifferentiated shortness of breath and sepsis, PoCUS may be a valuable tool to help to rapidly diagnose the presence of important lung and pleural pathology.
Case Report
A 61-year-old woman was transported to the ED, by paramedics, with confusion and a decreased level of consciousness. Her family indicated she had a two-week history of worsening minimally productive cough without hemoptysis, fatigue, weakness, and mild dyspnea on exertion in the prior 24 hours. Her past medical history included rheumatoid arthritis and Sjogren syndrome, for which she was on no medical therapy. She had no prior history of congestive heart failure or restrictive lung disease and no recent history of travel or unusual exposures. She was a non-smoker, did not consume alcohol, and was normally high-functioning. The decline in her functional status in the past several days had been precipitous.
Her initial triage vitals were: heart rate of 140 beats per minute, blood pressure of 91/61 mm Hg, respiratory rate 25 breaths per minute, temperature of 39°C (102.2°F), room air oxygen saturation of 86%. Physical examination revealed the patient was drowsy but easily roused. Head and neck examination was normal. Cardiac examination was unremarkable, with no murmurs, rubs, or thrills. Respiratory examination revealed decreased air entry to the right base. A portable chest x-ray was performed (Figure 1). This demonstrated an extensive heterogenous and poorly defined right-middle lobe consolidation. Intravenous antibiotics were commenced and the patient was referred to internal medicine for further management for a presumed right-middle lobe pneumonia.

Figure 1 Chest X-ray, demonstrating a right infiltrate.
Due to the lung consolidation visible on chest x-ray, and subsequent to the decision to commence IV antbiotics and admit the patient, we performed a point-of-care ultrasound (PoCUS) of the patient’s thorax. In the right posterolateral region, we identified a complex loculated pleural fluid collection suggesting the presence of an empyema (Figures 2 and 3). The findings were reported to internal medicine and a thoracic CT was ordered for further characterization of the collection. The CT confirmed a complex loculated fluid collection consistent with an empyema (Figure 4).

Figure 2 PoCUS of the right chest, demonstrating a complex, cystic, structure. Findings in keeping with an empyema.

Figure 3 CT Chest, demonstrating the complex empyema seen on PoCUS.
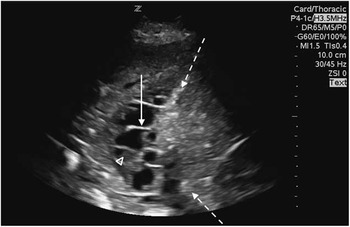
Figure 4 Dashed arrow: Representing the hyper echoic diaphragm. Solid arrow: Septation present within the cystic structure. Arrow head: Echogenic debris within the cystic structure, suggesting possible empyema.
The patient underwent immediate chest tube drainage of the empyema. Her blood cultures and empyema fluid cultures were both positive for Streptococcus pneumoniae and she was admitted to hospital for approximately two weeks. She was then transferred to another institution with thoracic surgery capabilities, as her subsequent chest CTs demonstrated incomplete drainage of the empyema collection; however, no surgery was ultimately required. The patient was discharged home from hospital with a complete recovery.
Discussion
Although 40% of pneumonias may be complicated with parapneumonic effusion, only 5%-10% go on to formation of an empyema.Reference Desai and Agrawal 4 , Reference Light, Girard and Jenkinson 5 A study of 3,675 patients found that empyemas occurred in only 1.3% of community-acquired pneumonia cases.Reference Ahmed, Marrie and Huang 6 A national Canadian database found non-surgical empyema rates have increased by an incidence rate ratio of 1.30 over an nine-year period ending in 2003.Reference Finley, Clifton and Fitzgerald 7 Patients who were younger and with a history of intravenous drug use were found to be at higher risk for empyema. Common organisms implicated are Streptococcus pneumoniae, Staphylococcus aureus, and Streptococcus milleri. Anaerobic bacteria are also identified in between 36% and 76% of cultures.Reference Brook and Frazier 8
Empyema carries a mortality rate of between 4% and 7%. Chalmers and colleagues prospectively identified six risk factors associated with patients admitted with community-acquired pneumonia developing a complicated parapneumonic effusion or empyema. These factors were: albumin <30 g/L, sodium <130 mmol/L, platelet count >400×109, C-reactive protein (CRP) >100 mg/L, and a history of alcohol or intravenous drug use. Elevated CRP and hypoalbuminemia conferred the highest adjusted odds ratios, at 15.7 and 4.6, respectively.Reference Chalmers, Singanayagam and Murray 9 Beyond situations involving the aforementioned risk factors, the diagnosis of empyema should be considered in pneumonia patients with prolonged symptoms, failure of antibiotic treatment, or failure of infiltrate resolution on radiography.Reference Ahmed, Marrie and Huang 6 , Reference Chalmers, Singanayagam and Murray 9 , Reference Sahn 10
Point-of-care ultrasound is increasingly used for the assessment of lung and pleural pathology in the ED. Recent studies have found that PoCUS has a high sensitivity and specificity for the detection of pneumonia, and may in fact be more sensitive than chest radiography.Reference Brook and Frazier 8 , Reference Chalmers, Singanayagam and Murray 9 Ultrasound findings suggesting pneumonia include a consolidated lung that takes on the appearance of a solid organ (termed “hepatization”), dynamic air bronchograms (air and fluid moving in and out of the consolidated lung), and a surrounding interstitial pattern (identified by bright lines with irregular margins spreading deep to the consolidation).Reference Bourcier, Paquet and Seinger 11
In addition to its potential utility in diagnosing pneumonia, PoCUS may be helpful in determining whether there are associated complications such as pleural effusions or empyema. In an ICU study of 42 patients, ultrasound has been found to be superior to chest radiography for the detection of pleural fluid, with a sensitivity and specificity of 100%, compared to a sensitivity and specificity of 65% and 81%, respectively, for chest x-ray.Reference Xirouchaki, Magkanas and Vaporidi 12 In addition, ultrasound has been reported to be more accurate than chest x-ray for determining the size of the pleural effusion.Reference Eibenberger, Dock and Ammann 13 Ultrasound findings suggestive of an empyema include a complex fluid collection in the pleural space with echogenic debris or septations.Reference Yang, Luh and Chang 14 The British Thoracic Society Guideline on management of pleural infection in adults states that ultrasound can be used for the initial assessment of the presence of pleural effusions and empyemas.Reference Davies, Davies and Davies 15 We were unable to identify any studies evaluating the sensitivity or specificity of PoCUS for the diagnosis of empyema.
In the case we present, a thoracic ultrasound was performed as a routine educational scan by trainees in the process of learning how to identify lung and pleural pathology. Trainees had received a didactic lecture on the background of lung ultrasound, and were on a training shift to learn the technical aspects of lung ultrasound examination. The lung ultrasound assessment was performed according to commonly used scanning protocols.Reference Lichtenstein and Meziere 1 , Reference Gargani and Volpicelli 16 The fact that the PoCUS identified an important unexpected finding in our case may suggest that emergency physicians should have a lower threshold to pursue thoracic ultrasound in patients with respiratory complaints, or when there is a consolidation identified on chest x-ray in the setting of risk factors for empyema. In the case we present, the patient’s main risk factor for formation of an empyema was the prolonged duration of her symptoms.Reference Davies, Davies and Davies 15 In addition to this, her ED blood work revealed thrombocytosis (platelet count 500) and hypoalbuminemia (albumin 21 g/L), both of which are predictive for possible empyema, though extremely non-specific.Reference Light, Girard and Jenkinson 5
Conclusion
We present a case where a point-of-care thoracic ultrasound done for educational purposes identified an unsuspected empyema in a patient being treated for community-acquired pneumonia. Emergency physicians should be aware of the limitations of chest radiography for the identification of pleural effusions and empyemas, and may need to have a lower threshold for consideration of thoracic ultrasound in patients with significant respiratory complaints. In particular, pneumonia patients with prolonged symptoms, patients who fail antibiotic therapy, intravenous drug users, and patients who are immunosuppressed should be considered for point-of-care ultrasound examination of the lungs. Further studies are needed to determine the test characteristics of PoCUS for the diagnosis of empyema.
Competing Interests: None to declare.






