The increased prevalence of childhood obesity and the associated co-morbidities is a major public health concern. Approximately one-third of obese and overweight children continue to follow a higher BMI trajectory throughout the life course(Reference Hruby and Hu1). It is also well established that adults, who were obese as children, have an increased risk of morbidity and mortality, independent of their current body weight(Reference Reilly and Kelly2,Reference Llewellyn, Simmonds and Owen3) .
Behaviours which lead to a positive energy balance and consequently to a gradual increase in body weight are established early in life. Consequently, preschool age is a key period for the implementation of behavioural change intervention. Energy balance-related behaviours (EBRB) in preschool years, such as limited engagement into physical activities and increased engagement into sedentary activities (i.e. TV viewing, playing video games etc.), have been associated with obesity in preschool children(Reference Reilly4,Reference te Velde, Van Nassau and Uijtdewilligen5) . In preschool children, the evidence on relevant associations between obesity and dietary behaviour is also strong but mixed in terms of different dietary behaviours reported to be significantly associated with obesity by different studies(Reference te Velde, Van Nassau and Uijtdewilligen5). However, despite the existing evidence on significant associations between EBRB and childhood obesity in preschool years, the effect of behavioural change interventions that attempt to positively modify EBRB in this young age group is still not adequately explored.
Preschool children do not entirely regulate their own EBRB, as they considerably rely on their parents/guardians. In this context, parental perception of their child’s body weight seems to play a significant role on their children’s EBRB and weight trajectory. More than half of overweight/obese children have their weight status underestimated by their parents(Reference Lundahl, Kidwell and Nelson6). Parents’ underestimation of their child’s increased body weight could be a significant barrier to the modification of ERBR(Reference Duncan, Hansen and Wang7), since parents who do not recognise their children’s overweight status will probably not take any corrective actions. In addition, parental characteristics can have a significant effect on parental modelling, which can subsequently influence children’s EBRB(Reference Campbell, Crawford and Ball8). In this regard, parental overweight and obesity produces and sustains an obesogenic environment at home that has been associated with obesity in preschool children in several countries worldwide(Reference Manios, Costarelli and Kolotourou9–Reference Semmler, Ashcroft and van Jaarsveld11) as well as with rapid increases in BMI percentile during preschool years(Reference Griffiths, Hawkins and Cole12).
Further to the effect of social environmental factors on EBRB and weight status of preschool children, a plethora of evidence also highlights the significant effect of factors occurring during early life stages on the subsequent development and growth of children(Reference Rinaudo and Lamb13,Reference Woo Baidal, Locks and Cheng14) . There is much to support the linkage of perinatal factors with overweight and obesity in preschool children. As such, maternal pre-pregnancy weight has been associated with a significant risk of childhood overweight and obesity at ages 3, 4 and 5 years(Reference Dubois and Girard15–Reference Whitaker20). A systematic review and meta-analysis considering both preschool and elementary age children also reported that pre-pregnancy overweight was associated with two- and threefold increased likelihood of childhood overweight/obesity, respectively(Reference Yu, Han and Zhu21). Furthermore, gestational weight gain above the recommended threshold has been independently associated with risks of overweight/obesity in early childhood(Reference Tie, Xia and Zeng22,Reference Voerman, Santos and Golab23) , although the effect relative to that of maternal pre-pregnancy overweight has been reported to be smaller(Reference Voerman, Santos and Golab23). In addition, maternal smoking during pregnancy has been associated with a higher BMI in preschool-aged children(Reference Dürmuş, Kruithof and Gillman24,Reference Oken, Levitan and Gillman25) , with a systematic review and meta-analysis suggesting an increased risk of overweight in childhood of 50 %(Reference Oken, Levitan and Gillman25). Maternal parity has also been associated with a lower risk of childhood overweight(Reference Gaillard, Rurangirwa and Williams26), although this maybe dependent on breast-feeding(Reference Kitsantas and Gaffney27). Exclusive breast-feeding and later age of introduction of non-breast milk have shown protective effects on preschool overweight/obesity in some(Reference Baran, Weres and Czenczek-Lewandowska28–Reference Nascimento, da Silva and Ferreira30) but not all studies. Despite the well-established relationship between perinatal and early life factors with overweight and obesity at preschool years, their effect on BMI changes in this age group remains to be thoroughly investigated.
The ToyBox-study designed, implemented and evaluated a kindergarten-based, family-involved intervention to 3·5–5·5-year-old children from six European countries, who were followed-up for 1 year. The ToyBox-intervention focused on four different EBRB (water consumption, healthy snacking, sedentary behaviour and physical activity) and has successfully demonstrated decreases in prepacked fruit juice consumption(Reference Pinket, Van Lippevelde and De Bourdeaudhuij31) and computer/video games use(Reference Latomme, Cardon and De Bourdeaudhuij32).
This study aimed to investigate whether the modification of EBRB attributed to the Toybox intervention could potentially have a positive effect on the changes observed on children’s age- and sex-specific BMI percentile. By also recording a wide range of other potentially determining factors, the secondary aim of the present study was to assess the effect of perinatal factors and parental perceptions, socio-demographic and anthropometric characteristics on children’s BMI percentile change.
Methods
ToyBox-study
The ToyBox-intervention study was a multicomponent, kindergarten-based, family-involved intervention with a cluster-randomised design. The intervention focused on modifying EBRB (see online supplementary material, Supplementary Table 1). A detailed description of the design of the ToyBox-study is provided elsewhere(Reference Manios, Androutsos and Katsarou33).
In brief, a standardised, multistage sampling approach was applied on preschool children aged 3·5–5·5 years old and their families, who were recruited from randomly selected municipalities within the provinces of Oost-Flanders and West-Flanders (Belgium), Varna (Bulgaria), Bavaria (Germany), Attica (Greece), Mazowieckie (Poland) and Zaragoza (Spain) (see online supplementary material, Supplementary Table 2). Randomisation of the recruited municipalities to intervention and control groups was conducted centrally by the coordinating centre, after the completion of baseline measurements. The municipalities were assigned to the intervention or control group in a 2:1 ratio within each of the three socio-economic status groups. Since the randomisation was conducted at a municipality level, the 309 kindergartens within each municipality were automatically allocated to the intervention or control group. Kindergartens were randomly selected within each municipality.
Intervention mapping protocol was used to plan and develop the standardised ToyBox and provides a systematic, stepwise framework for planning, implementing and evaluating an intervention based on existing scientific literature, theories and research data. Seven hundred kindergarten teachers were trained and delivered the programme in the kindergartens. For evaluation purposes, data were obtained both at baseline and follow-up from more than 5500 parents, indicating significant improvements on the targeted obesogenic behaviours among children and parents, as well as relevant parental practices. The intervention ran for 24 weeks and consisted of four modules on water consumption, healthy snacking, sedentary behaviour and physical activity delivered by the kindergarten teacher. Each model had a four-week ‘first focus’ and a two-week ‘repetition’ phase(Reference Manios, Androutsos and Katsarou33).
Data collection
Data were collected from 7541 preschool children and their parents/caregivers from May to June 2012 and 2013. Children’s anthropometrics were measured at baseline and 1-year post intervention, while parents/caregivers self-reported sociodemographic, lifestyle and perinatal information in questionnaires, administered at baseline and the 1-year follow-up.
Energy balance-related behaviour measurement
Both in the baseline and follow-up measurements, parents/caregivers were asked to describe the child’s usual food and beverage habits over the last 12 months in a FFQ for young children. Items regarding beverage consumption included plain water, soft drinks, light soft drinks, home-made and freshly squeezed fruit juice, pre-packed/bottled fruit juice, tea, smoothies (all kinds), plain milk and sugared or chocolate milk.
Snacking behaviours were also measured using the FFQ completed by the child’s guardian, with snacks defined as a small portion of food eaten in between regular meals. Intakes of yogurt (i.e. plain yogurt), sugared or aromatised yogurt, cheese, fresh fruit, raw vegetables, milk-based desserts (e.g. chocolate mousse, ice cream, custard), chocolate and candy bars (e.g. plain chocolate bars, chocolate candy bars), sugar-based desserts (e.g. hard candies, jelly beans, lollipops), cakes, biscuits and salty snacks (e.g. potato chips) were each assessed.
Questions regarding sedentary behaviour were answered by parents/guardians as part of the Primary Caregivers’ Questionnaire. The amount of time that children spent on TV/DVD/video viewing, computer/video games use and quiet play on weekdays and weekend days was assessed in three questions of the Primary Caregivers’ Questionnaire (one for each SB subcomponent, i.e. TV viewing, computer/video games use and quiet play). For example, ‘How much time does your child spend on TV-viewing (a) on weekdays, and (b) on weekend days?’. Possible answer options varied on a nine-point Likert-type scale, ranging from ‘never’ to ‘more than 8 hours/day’.
Physical activity was measured objectively by step counts. Before the start of the intervention, baseline measurements were performed on weekdays from May to June 2012. On those days, researchers visited intervention and control kindergartens and fitted those preschool children with an accelerometer (Belgium) or a pedometer (other countries). One year later, from May to June 2013, follow-up measurements were performed.
Anthropometric measures
Researchers in all participating centres were rigorously trained to conduct anthropometric measurements following a standardised procedure(Reference De Miguel-Etayo, Mesana and Cardon34,Reference Mouratidou, Miguel and Androutsos35) . More specifically, researchers conducted two consecutive measurements of children’s body weight to the nearest 100 g and of children’s height, to the nearest 1 mm, using the same types of electronic scales (SECA 861 and SECA 813; Seca) and height using portable stadiometers (types SECA 225 and SECA 214; Seca), respectively. If the difference between first and second measurement was ≥1 kg in the case of weight, and ≥2 cm in the case of height, a third measurement was required and the two closest measurements were averaged.
Baseline and follow-up BMI percentile and z-scores were calculated for each child using the WHO ANTHRO software for those less than or equal to 60 months, and the WHO ANTHRO-PLUS software for those over 60 months. Children were categorised as: ‘underweight’, ‘normal weight’, ‘overweight’ or ‘obese’, based on the appropriate z-score. BMI percentile change in 1 year was defined as the difference of age- and sex-specific BMI percentile from baseline to 1-year post intervention (BMI percentile post intervention minus baseline BMI percentile) and was considered as the primary response variable in this analysis.
Parental perception on children’s body weight
Parents/caregivers of children were also surveyed concerning their opinion about their child’s weight. Cross tabulation between BMI at baseline (per cut-off) and perception of child’s weight (‘What do you think about your child’s weight?’; response on a five-point scale) was used to evaluate the guardian’s ability to correctly identify their child’s body weight status at baseline. Correct perception was considered for: a child grouped as overweight/obese with parents’/caregivers’ response as ‘high’ or ‘very high’ child’s weight OR a child grouped as normal weight/underweight with response as ‘very low’ or ‘low’ or ‘normal’ child’s weight. Misperception was considered for: a child grouped as overweight/obese with response as very low/low/normal child’s weight.
Parental socio-demographic and anthropometric characteristics
Children were categorised as ‘native’ if both biological parents were born in the country where the questionnaires were administered, whereas all other children as ‘non-native’ (i.e. having at least one parent born abroad). Parental body weight and height were self-reported by the parents/caregivers, and their BMI was calculated according to the Quetelet’s equation (weight (kg)/height2 (m2)). Parents/caregivers were categorised according to their BMI as ‘normal weight’ (≤24·9 kg/m2), ‘overweight’ (≥25 and ≤29·9 kg/m2) or ‘obese’ (≥30 kg/m2). Last, parents/caregivers were asked to report the level of their education.
Perinatal and early life factors
Mothers were also asked to recall smoking habits during pregnancy (yes/no), pre-pregnancy weight, weight gained during pregnancy based on the classification recommended by the Institute of Medicine(36), multiparous gestation, parity, birth weight and gestational age for the classification into ‘small for gestational age’ (<10th percentile), ‘appropriate for gestational age’ (10th–89th percentile) and ‘large for gestational age’ (⩾90th percentile), child’s feeding patterns from birth to 6 months of age (exclusive breast-feeding, exclusive formula or mixed), and child’s weight and length. Parents/guardians were asked to consult their child’s recorded infant’s growth chart/medical record and report the weight and length of their child at birth and at the 6th, 7th, 11th and 12th months of their child’s life. Using this information, change in weight-for-length Z-score from birth to 6 months of age was calculated and then classified into ‘poor’ (<−1 Z-score), ‘average’ (−1 to +1 Z-score) and ‘rapid’ (>+1 Z-score) weight gain during infancy.
Statistical analysis
Differences between the control and intervention groups in descriptive variables were calculated by the χ 2 test. To account for the nested and hierarchical nature of the sampling linear mixed effect models were used to assess associations between BMI percentile change in 1 year and (i) intervention and (ii) perinatal factors, parental socio-demographic and anthropometric characteristics. Random intercepts were used for country, socio-economic status and kindergarten, with fixed mean for each country and the intercept varying among socio-economic status and kindergarten within socio-economic status.
A multivariate model was produced, containing the intervention effect and all factors found in univariate analysis to be significantly (P < 0·05) associated with change in BMI percentile, which were then eliminated from the multivariate model if not significant. Factors with potential collinearity issues were assessed separately and the strongest variable retain in the final model. We also tested for an interaction between the intervention and those factors that were found to be significantly (P < 0·05) associated with BMI percentile changes, in order to assess whether these factors could influence the effect of the intervention.
Regression coefficients are presented as beta with 95 % CI. Statistical analysis was performed in R statistical programme (version 3.5.3 (2019-03-11)). The level of significance was set as P < 0·05.
Results
Table 1 presents the descriptive characteristics of the study sample. In total, 6268 children (51·9 % boys, mean age at baseline 4·74 ± 0·44 years) provided valid height and body weight data at baseline and follow-up. Previous attrition analyses(Reference Latomme, Cardon and De Bourdeaudhuij32) showed no significant differences in age, sex and group of preschoolers who were lost to follow-up and those who were included (95 % CIage = 0·93, 1·16; 95 % CIsex = 0·92, 1·14; 95 % CIgroup = 0·91, 1·52). At baseline, the majority of children were under/normal weight (89·4 %), with 7·8 % overweight and 2·8 % obese. The mean change in BMI percentile was –1·48 (sd 13·49), with 907 children (14·5 %) increasing their BMI percentile by more than 10 %. The weight status of overweight/obese children was underestimated by 70·6 % of their parents or primary guardians (470/666 overweight/obese children; 7·5 % of total sample), and parents/guardians were more likely to underestimate the body weight of male children (P < 0·001). Conversely, only 2·3 % of parents/guardians overestimated the weight of their child. Just below 70 % of families had at least one parent/guardian who was overweight/obese.
Table 1 Socio-demographic, parental characteristics and perinatal factors in preschool children from six European countries (n 6268)

* P-value derived from χ 2 test between control and intervention.
** Gestational weight gain recommendations provided by the Institute of Medicine (IOM).
Table 2 summarises the findings derived from the univariate models testing the effect of the intervention, perinatal factors, parental socio-demographic and anthropometric characteristics on the changes observed in children’s BMI percentile. The intervention had no significant effect on the change in BMI percentile. Regarding the effect of parental characteristics, parents’/guardians’ underestimation of children’s weight status at baseline was associated with an increase in children’s BMI percentile (1·41, 95 % CI 0·10, 2·72). Furthermore, children with only one or both parents being overweight/obese had a 2·47 (95 % CI 1·66, 3·29) and a 4·00 (95 % CI 2·94, 5·06) increase in BMI percentile, respectively, compared with those children whose parents were under/normal weight. As far as the effect of perinatal factors was concerned, overweight/obesity in mothers before pregnancy was associated with an increase (2·32, 95 % CI 1·41, 3·23) in children’s BMI percentile, while mother’s age at pregnancy was associated with a decrease (–0·10, 95 % CI –0·20, –0·01) in BMI percentile, but only in girls. In addition, children whose mothers exceeded the recommended weight gain during pregnancy and had a higher gestational age significantly increased their BMI percentiles by 1·15 (95 % CI 0·43, 1·86) and 0·25 (95 % CI 0·07, 0·43), respectively. Mixed feeding during infancy was also found to be significantly associated with an increase in BMI percentile (1·86, 95 % CI 0·33, 3·40) compared with formula feeding, but this was observed only in boys. Girls whose mothers smoked during pregnancy significantly increased their BMI percentiles by 1·42 (95 % CI 0·28, 2·56), compared with girls whose mothers did not smoke at pregnancy. Decreases in BMI percentile of –1·26 (95 % CI –2·63, –0·11) and –1·48 (95 % CI –2·59, –0·38) were also observed for those children who were born first and small for gestational age, compared with those born at a rank other than first and appropriate for gestational age, respectively.
Table 2 Effect of parental characteristics and perinatal factors on the change in the age- and sex-specific BMI percentile over the 1-year period of the ToyBox intervention – univariate modelling *

IOM recommendations = recommendations by the Institute of Medicine (IOM) 2009 report; AGA, normal for gestational age; LGA, large for gestational age; SGA, small for gestational age.
* Estimates from linear mixed effect models with random intercept for country, socio-economic status and school, and fixed effect adjustment for BMI pre-intervention.
The findings derived from the multivariate model that examined the intervention effect and all factors found in the univariate analyses to be significantly associated with the change in BMI percentile are displayed in Table 3. The non-significant effect of the intervention observed at the univariate analysis was also observed at the multivariate model. However, parents’/caregivers’ underestimation of children’s weight status at baseline remained significantly associated with increase in BMI percentile (1·72, 95 % CI 0·22, 3·21). Similarly, children with one (2·34, 95 % CI 1·50, 3·18) or both parents (2·87, 95 % CI 1·61, 4·13) being overweight/obese, as well as children whose mother was overweight/obese before pregnancy (2·03, 95 % CI 0·89, 3·17), were also found to significantly increase their BMI percentile, compared with children with under/normal-weight parents. Girls born small for gestational age showed a decrease in their BMI percentile (–2·75; 95 % CI –4·49, –1·02) compared with their appropriate for gestational age and large for gestational age counterparts. There were no significant interaction effects seen between the intervention and any other factors.
Table 3 Effect of parental characteristics and perinatal factors on the change in the age- and sex-specific BMI percentile over the 1-year period of the ToyBox intervention – multivariate modelling*
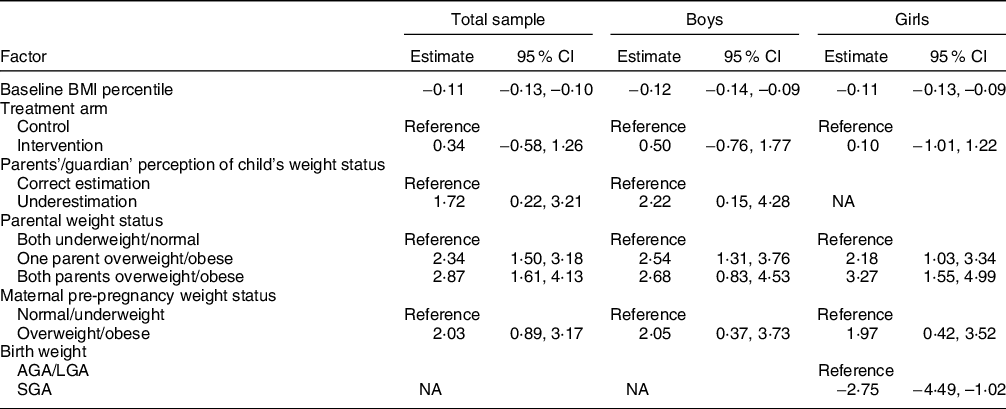
AGA, normal for gestational age; LGA, large for gestational age; SGA, small for gestational age.
* Estimates from linear mixed effect models with random intercept for country, socio-economic status and school.
Discussion
The primary aim of the present study was to investigate whether the ToyBox-intervention affected the change in BMI percentile of preschool children from six European countries, over the course of 1 year. However, the intervention was not found to have any significant effect on the change observed in children’s BMI percentile. Although some of the targeted EBRB, such as prepacked fruit juice consumption(Reference Pinket, Van Lippevelde and De Bourdeaudhuij31) and computer/video games use(Reference Latomme, Cardon and De Bourdeaudhuij32), decreased, this favourable impact of the intervention was not followed by a relevant favourable effect on children’s BMI percentile values. The non-significant findings observed in the present study regarding the effect of the intervention on children’s weight trajectory could partly be attributed to the fact that the intervention could not modify all targeted EBRB, such as children’s physical activity levels(Reference De Craemer, Verloigne and De Bourdeaudhuij37) and TV viewing(Reference Latomme, Cardon and De Bourdeaudhuij32). Parental lack of concern may play a part, as <10 % of children were overweight/obese at baseline and parents of younger children may believe that excessive adipose tissue is typical during development and that overweight/obese children will outgrow their excess body weight(Reference Chang, Mendelsohn and Fierman38).
The accuracy of parental perceptions of their child’s weight status could be an important determinant that might have influenced children’s BMI percentile, since parental misperception of their child’s body weight can affect relevant EBRB(Reference Duncan, Hansen and Wang7). The percentage of parents who underestimated the weight status of their overweight/obese children was found to be quite high in the present study (70·6 %) and is comparable to relevant percentages reported by a meta-analysis(Reference Lundahl, Kidwell and Nelson6) of seventy-eight studies (i.e. 67·5 %; 95 % CI 62·9, 71·7 %, unadjusted). The majority of studies that examine parental misperception of their child’s weight status(Reference Lundahl, Kidwell and Nelson6,Reference Duncan, Hansen and Wang7) and factors associated with misperceptions(Reference Maynard, Galuska and Blanck39) have been cross-sectional, while the evidence coming from prospective studies is limited. Regarding the role of parental misperceptions on childhood obesity, it has been hypothesised that correct perception of child’s weight status would help parents realise that they need to promote and model healthier behaviours, as a means to improve the child’s weight trajectory(Reference Lundahl, Kidwell and Nelson6). However, this is not confirmed by the results from other studies. An Australian longitudinal study(Reference Robinson and Sutin40) in 3557 children and their parents, reported that children whose parents perceived their 4–5-year-old children as ‘overweight’, gained more weight across the 8-year follow-up than those perceived as ‘normal weight’, while a similar, though non-significant, result was also reported by another study(Reference Kroke, Strathmann and Günther41). A Dutch study(Reference Gerards, Gubbels and Dagnelie42) looked at accurate parental perception of child’s body weight at the age of 5 years and subsequent changes in the child’s BMI z-score over time. While 85 % of the parents underestimated their overweight child’s weight status, accurate weight status perception was associated with a greater increase in children’s BMI from 5 until 9 years of age, compared with the underestimation of the child’s weight status. In this regard, and despite the fact that the present study showed that underestimation of weight status is associated with an increase of children’s BMI percentile over this important preschool year, previous evidence suggests that parental awareness of the child’s overweight status is not necessarily protective against subsequent increases in body weight. On the contrary, a recent systematic literature review suggested that interventions aiming to correct parental misperceptions of children’s weight status, especially in younger age groups, will most likely not be effective(Reference Blanchet, Kengneson and Bodnaruc43).
Although the findings regarding the role of parental perceptions on their child’s weight trajectory are inconsistent, the evidence on the role of parental weight status has been reported to be much stronger. Both paternal and maternal overweight and obesity have been shown to increase the risk of preschool obesity in several countries worldwide, including Greece(Reference Manios, Costarelli and Kolotourou9), the UK(Reference Semmler, Ashcroft and van Jaarsveld11) and Iran(Reference Koomanaee, Tabrizi and Naderi10). Parental overweight and obesity is also an important risk factor for an unfavourable growth trajectory during childhood. In this context, a large study conducted in the UK(Reference Griffiths, Hawkins and Cole12) showed that the increase in the BMI of preschool children between the age of 3 and 5 years was strongly associated with overweight status of either parents. Besides inheritance of genes that confer susceptibility to obesity, parental overweight is also a proxy for shaping the postnatal eating and physical activity environment of children. In most cases, overweight parents create and sustain an ‘obesogenic’ environment (i.e. high-energetic diets and physical inactivity) for themselves and their children(Reference Whitaker20).
Extensive research that has been conducted during the last decades in the field of the early origins of chronic disease has produced a wide range of evidence and relevant theoretical models that highlight the predisposing role of several perinatal factors on the later manifestation of childhood obesity. These theoretical models suggest that the effect of certain environmental factors during specific, critical periods of early development can lead to permanent physiological and metabolic adaptations that although serve the purpose of improving the chances of fetal and postnatal survival, may become detrimental in the long term and may be expressed at different life stages in the presence of certain environmental influences(Reference Godfrey and Barker44). In this regard, the present study reported mother’s pre-pregnancy overweight/obesity status to be one of the strongest perinatal factors that remained positively associated with children’s BMI percentile change at the multivariate model. Mother’s pre-pregnancy BMI is a well-established risk factor which has been associated with accelerated growth trajectory(Reference Giles, Whitrow and Davies45), abdominal adiposity(Reference Jacota, Forhan and Saldanha-Gomes17) and obesity at preschool years(Reference Whitaker20). Although gestational weight gain has also been associated with obesity in preschool children(Reference Oken, Taveras and Kleinman46), the univariate association observed in the present between gestational weight gain above IOM recommendations and increases in boy’s BMI percentile became non-significant after including mother’s pre-pregnancy BMI into the model. This suggests that mother’s pre-pregnancy weight status is a stronger perinatal determinant of children’s weight trajectory at preschool years, a finding that is also supported by a recent meta-analysis which combines a wide range of data from various countries worldwide(Reference Voerman, Santos and Golab23).
The results of the present study derived from the multivariate model also revealed a significant association between size at birth and BMI change at preschool years in girls. More specifically, girls born small for gestational age decreased their BMI percentile compared with girls who were born large for gestational age or appropriate for gestational age. The associations observed between size at birth and adiposity at later life are complex, with the majority of studies however reporting a ‘J’-shaped positive association between birth weight and children’s weight status(Reference Woo Baidal, Locks and Cheng14). Regardless of the exact associations, as size at birth is the product of the nutritional and hormonal milieu in which the fetus develops(Reference Godfrey and Barker44), better control of the trajectory of intrauterine growth via the optimisation of maternal nutrition and health status during pregnancy is fundamental.
The present study should be interpreted under the light of its limitations and strengths. The main limitation was that the ToyBox-sample is not fully representative of the source population of preschool children in Europe, due to the sampling of study participants from specific regions in each country. Further limitations include the possibility of recall bias in the assessment of perinatal factors and the reliance on self-reported parental height and body weight data, although this is mitigated by the use of questionnaires with moderate-to-excellent reliability. Regarding strengths, the main study outcome, that is, the change in the child’s BMI percentile, was based on reliable measurements conducted by rigorously trained researchers who achieved excellent intra- and inter-observer reliability(Reference De Miguel-Etayo, Mesana and Cardon47). Strengths also include the large sample of preschooler children and the cluster-randomised pre- and post-test design including an intervention and control group, as well as the simultaneously consideration of several factors that were previously identified as potential correlates of preschool children’s BMI.
Conclusion
The present study showed that parental overweight status and parental underestimation of their child’s body weight constitute unfavourable conditions for the BMI trajectory in preschool years. While the ToyBox intervention did not affect BMI percentile change in preschool children, the significant favourable findings observed by ToyBox-intervention implementation, as well as its low resource requirements and use of available personnel and infrastructure, indicate its scalability potential. It is currently expanding in more regions and countries globally, that is, in Argentina, Belgium, Boston, Bulgaria, Ecuador, Estonia, Germany, Greece, Italy, Malaysia, Malta, New Zealand, Nicaragua, Poland, South Africa, Scotland, Spain and UK(Reference Malden, Reilly and Hughes48,Reference Reeves, Poh and Cheah49) . Although not fully supported by the available literature, increasing parental awareness on the health risks associated with overweight might help increase readiness for change, thus positively modifying EBRB that can support a healthier weight status for the entire family. Furthermore, considering the significant positive associations observed between mother’s pre-pregnancy weight status and children’s BMI percentile change at preschool age, any initiatives that can support women to enter pregnancy with a normal body weight but also adopt and maintain a healthy lifestyle for them and their children after birth, could be proved to be effective early preventive measures in tackling childhood obesity.
Acknowledgements
Acknowledgements: ToyBox-study group: Coordinator: Yannis Manios; Project Manager: Odysseas Androutsos, Steering Committee: Yannis Manios, Berthold Koletzko, Ilse De Bourdeaudhuij, Mai Chin A Paw, Luis Moreno, Carolyn Summerbell, Tim Lobstein, Lieven Annemans, Goof Buijs; External Advisors: John Reilly, Boyd Swinburn, Dianne Ward; Harokopio University (Greece): Yannis Manios, Odysseas Androutsos, Eva Grammatikaki, Christina Katsarou, Eftychia Apostolidou, Anastasia Livaniou, Katerina Lymperopoulou, Eirini Efstathopoulou, Christina-Paulina Lambrinou, Angeliki Giannopoulou, Evita Siatitsa, Efstathoula Argiri, Konstantina Maragkopoulou, Athanasios Douligeris; Ludwig Maximilians Universitaet Muenchen (Germany): Berthold Koletzko, Kristin Duvinage, Sabine Ibrügger, Angelika Strauß, Birgit Herbert, Julia Birnbaum, Annette Payr, Christine Geyer; Ghent University (Belgium): Department of Movement and Sports Sciences: Ilse De Bourdeaudhuij, Greet Cardon, Marieke De Craemer, Ellen De Decker, Department of Public Health: Lieven Annemans, Stefaan De Henauw, Lea Maes, Carine Vereecken, Jo Van Assche, Lore Pil; VU University Medical Center EMGO Institute for Health and Care Research (the Netherlands): EMGO Institute for Health and Care Research: Mai Chin A Paw, Saskia te Velde; University of Zaragoza (Spain): Luis Moreno, Theodora Mouratidou, Juan Fernandez, Maribel Mesana, Pilar De Miguel-Etayo, Esther M. González-Gil, Luis Gracia-Marco, Beatriz Oves; Oslo and Akershus University College of Applied Sciences (Norway): Agneta Yngve, Susanna Kugelberg, Christel Lynch, Annhild Mosdøl, Bente B Nilsen; University of Durham (UK): Carolyn Summerbell, Helen Moore, Wayne Douthwaite, Catherine Nixon; State Institute of Early Childhood Research (Germany): Susanne Kreichauf, Andreas Wildgruber; Children’s Memorial Health Institute (Poland): Piotr Socha, Zbigniew Kulaga, Kamila Zych, Magdalena Góźdź, Beata Gurzkowska, Katarzyna Szott; Medical University of Varna (Bulgaria): Violeta Iotova, Mina Lateva, Natalya Usheva, Sonya Galcheva, Vanya Marinova, Zhaneta Radkova, Nevyana Feschieva; International Association for the Study of Obesity (UK): Tim Lobstein, Andrea Aikenhead; CBO B.V. (the Netherlands): Goof Buijs, Annemiek Dorgelo, Aviva Nethe, Jan Jansen; AOK- Verlag (Germany): Otto Gmeiner, Jutta Retterath, Julia Wildeis, Axel Günthersberger; Roehampton University (UK): Leigh Gibson; University of Luxembourg (Luxembourg): Claus Voegele. Financial support: The ToyBox-study was funded by the Seventh Framework Programme (CORDIS FP7) of the European Commission under grant agreement n° 245200. The content of this article reflects only the authors’ views, and the European Community is not liable for any use that may be made of the information contained therein. Conflicts of interest: The authors declare no conflicts of interest. Authorship: Y.M., E.K., C.M., L.A.M., V.I., A.Ś.L., B.K., G.C. and O.A. designed, obtained funding and conducted the ToyBox Study. K.A.L. and G.M. led the analysis of data. All authors contributed to interpreting of the data, drafting the manuscript, to the intellectual content and revising of the final draft of the manuscript. The final version of the manuscript was approved by all the authors. Ethics of human subject participation: The ToyBox-study (www.toybox-study.eu) adhered to the Declaration of Helsinki and the conventions of the Council of Europe on human rights and biomedicine. Approval for the study was obtained by the following entities: in Belgium by the Medical Ethics Committee of the Ghent University Hospital (20·March·2012, number 2012/110); in Bulgaria by the Ethics Committee of the Medical University of Varna (21·July·2011, number 15); in Germany by the Ethics Committee of the Ludwig Maximilian University of Munich (11·April·2012/Project number: 400-11); in Greece by the Bioethics Committee of Harokopio University (28·February·12 -2010) and the Greek Ministry of Education (21·December·2011, 135559/Γ7); in Poland by the Bioethics Committee of the Children’s Memorial Health Institute and the Department of Information and Publicity of the Polish Ministry of Education (number 1/KBE/2012); and in Spain by the Clinical Research Ethics Committee and the Department of Consumers’ Health of the Government of Aragón (31·August·2011, number 12/2011). All headmasters/teachers and parents/caregivers provided a signed consent form before being enrolled in the study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001518






