Introduction
The coronavirus disease (COVID-19) pandemic has had profound consequences on physical, mental, and social well-being (Shah, Mohammad, Qureshi, Abbas, & Aleem, Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021; Varma, Junge, Meaklim, & Jackson, Reference Varma, Junge, Meaklim and Jackson2021). International research examining mental health during the pandemic indicates that 30–77% of the general population is experiencing elevated stress, anxiety, and depression (Luo, Guo, Yu, Jiang, & Wang, Reference Luo, Guo, Yu, Jiang and Wang2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021), compared to an estimated 15–33% pre-pandemic (American Psychological Association, 2019; Ettman et al., Reference Ettman, Abdalla, Cohen, Sampson, Vivier and Galea2020; Terlizzi & Villarroel, Reference Terlizzi and Villarroel2020). Canadian research indicates increased distress, loneliness, anxiety and depression, suicidal ideation, substance use, and a decline in overall mental health since the pandemic onset, particularly among ethnic, sexual and gender minorities, and those with pre-existing mental health conditions, physical disabilities, and lower incomes (Best, Law, Roach, & Wilbiks, Reference Best, Law, Roach and Wilbiks2020; Dozois, Reference Dozois2020; Jenkins et al., Reference Jenkins, McAuliffe, Hirani, Richardson, Thomson and McGuinness2021).
Age has also emerged as a predictor of differential mental health during the pandemic (Best et al., Reference Best, Law, Roach and Wilbiks2020; El-Gabalawy & Sommer, Reference El-Gabalawy and Sommer2021; Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). Younger adults have been more negatively impacted, with adults ages 25 and younger experiencing the highest rates of anxiety, stress, and depression (e.g., Best et al., Reference Best, Law, Roach and Wilbiks2020; Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). As older adults face more serious physical consequences of COVID-19 and may be experiencing more social isolation due to public health restrictions, compounded by less familiarity with technologies that facilitate social contact (e.g., video conferencing), researchers speculate that they may be experiencing higher pandemic-related stress (e.g., Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020). However, older adults are reporting greater satisfaction with life, social cohesion, and resilience, as well as lower depression, anxiety, and emotional distress than are younger adults (Best et al., Reference Best, Law, Roach and Wilbiks2020; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). While older adults appear to be faring better overall, they are nonetheless reporting increased loneliness and depression since the onset of the pandemic (April/May 2020) (Krendl & Perry, Reference Krendl and Perry2021). A better understanding of mental health impacts of the pandemic in Canadian adults is needed to guide resource development and allocation to those with the most urgent needs.
Extant pandemic-related research suggests that, in young adults, loneliness and financial stress are associated with elevated symptoms of depression and anxiety, respectively (Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). Younger and middle-aged adults are more likely to have faced adjustments to online academic or work environments (e.g., remote work; family–work conflict) and perceived greater threats to long-term academic/occupational, social, and economic prospects (Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021), which may further contribute to poorer mental health. In contrast, weekly exercise (Varma et al., Reference Varma, Junge, Meaklim and Jackson2021) and prior management of adverse life events (Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021) have been identified as resilience factors among older adults that may protect against adverse mental health effects. Still, those older adults with fewer resilience factors are experiencing poorer mental health (e.g., those living alone, minorities, unpaid caregivers; Vahia, Jeste, & Reynolds, Reference Vahia, Jeste and Reynolds2020), suggesting vulnerability to mental health impacts varies according to personal, social, and financial circumstances.
Given significant impacts of pandemic-related public health orders on access to social networks, social support and loneliness may be key mental health determinants and may relate to observed differential age effects. Both perceived social support (i.e., the evaluation of quality of one’s social relationships; Zimet, Dahlem, Zimet, & Farley, Reference Zimet, Dahlem, Zimet and Farley1988) and loneliness (i.e., the perceived inadequacy of social connections in relation to one’s needs; Hawkley & Cacioppo, Reference Hawkley and Cacioppo2010) are robust risk factors for mental health outcomes including depression, anxiety, stress, and suicidal ideation (Beutel et al., Reference Beutel, Klein, Brähler, Reiner, Jünger and Michal2017; Erzen & Çikrikci, Reference Erzen and Çikrikci2018; Richardson, Elliott, & Roberts, Reference Richardson, Elliott and Roberts2017). Younger adults typically report larger social circles and higher support (Vaux, Reference Vaux1985), whereas social spheres (including availability and frequency of social contact) tend to get smaller with age (Antonucci, Reference Antonucci, Birren and Schaie2001). Many older adults may be experiencing less discrepancy between pre-pandemic and current social spheres (Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021) and, thus, may perceive pandemic-related reduced social contact as less disruptive and distressing (Best et al., Reference Best, Law, Roach and Wilbiks2020; Dozois, Reference Dozois2020; Wu, Reference Wu2020). Moreover, frequency of social contact is important among younger adults (Williams & Galliher, Reference Williams and Galliher2006), whereas quality of support is a stronger predictor of health and well-being than is frequency of contact among older adults (Ashida & Heaney, Reference Ashida and Heaney2008; Krendl & Perry, Reference Krendl and Perry2021; Werner-Seidler, Afzali, Chapman, Sunderland, & Slade, Reference Werner-Seidler, Afzali, Chapman, Sunderland and Slade2017). Given the robust role of social connectedness in mental health functioning, further examination of perceived social support and frequency of contact across age groups during the pandemic is critical.
Loneliness is another important factor in mental health functioning across age groups (Beutel et al., Reference Beutel, Klein, Brähler, Reiner, Jünger and Michal2017; Erzen & Çikrikci, Reference Erzen and Çikrikci2018; Richardson et al., Reference Richardson, Elliott and Roberts2017); however, findings relating to the role of loneliness for older adults during the pandemic are mixed. Qualitative research examining experiences of those ages 60 and over indicates the most common sources of comfort throughout the pandemic have included interpersonal relationships, virtual social contact, and engagement in hobbies, whereas common sources of stress have included confinement, restrictions, isolation, and loneliness (Whitehead & Torossian, Reference Whitehead and Torossian2021). Loneliness has been associated with higher rates of anxiety and depression during the pandemic; however, those ages 55 and over have reported less loneliness relative to middle-aged (36–54) and young adults (18–35), and loneliness has been found only to predict anxiety for young (but not middle-aged or older) adults in the pandemic context (Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). On the other hand, older adults are more likely to live alone, and those who have not adjusted to isolation, or who are recently bereaved, may be at a disproportionate risk for negative pandemic-related mental health impacts (Vahia et al., Reference Vahia, Jeste and Reynolds2020). However, researchers have shown that many older adults living alone have connected with friends and family virtually and, in some cases, report increased communication with loved ones, which may contribute to observed resilience against loneliness (Hamm et al., Reference Hamm, Brown, Karp, Lenard, Cameron and Dawdani2020). Preliminary evidence suggests that loneliness may be a less salient predictor of mental health among older age groups during the pandemic (Varma et al., Reference Varma, Junge, Meaklim and Jackson2021) and that technology-assisted communication may serve as a source of comfort (Hamm et al., Reference Hamm, Brown, Karp, Lenard, Cameron and Dawdani2020).
Given that social support is a protective factor against negative mental health outcomes and may circumvent feelings of loneliness, examining how social support and loneliness interact within the pandemic context is critical. Among older adults, perceived closeness in social relationships (but not social isolation or frequency of communication) has been shown to moderate the association between loneliness and depression such that the association was no longer significant when high perceived closeness was reported (Krendl & Perry, Reference Krendl and Perry2021). However, in those who are socially isolated, virtual communication may buffer against loneliness (i.e., Hamm et al., Reference Hamm, Brown, Karp, Lenard, Cameron and Dawdani2020). These results highlight the importance of examining interactions between key resilience constructs related to mental health during the pandemic.
The Current Study
More research is needed to better understand differential age effects of the pandemic on Canadian adults’ mental health (e.g., Best et al., Reference Best, Law, Roach and Wilbiks2020; Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020). The aims of the current study were to: 1) describe impacts of the pandemic on key mental health and social connectedness variables (i.e., perceived social support, loneliness, frequency of technology-assisted communication) across adult age groups; 2) examine associations between social connectedness variables and mental health outcomes (i.e., depression, anxiety, psychological stress) both within and between adult age groups, to determine for which age groups these predictors are most salient; and 3) examine potential interactions between loneliness and perceived social support, and between loneliness and frequency of communication, in predicting mental health outcomes in a large sample of Canadian adults.
Given recent research suggesting that mental health in the context of the pandemic improves as age increases (i.e., Best et al., Reference Best, Law, Roach and Wilbiks2020; Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020; Shah et al., Reference Shah, Mohammad, Qureshi, Abbas and Aleem2021; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021), we hypothesized that 1) the oldest age groups (i.e., 65–69 and 70 and over) would report better mental health (i.e., lower depression, anxiety, trauma-related stress), more perceived social support, and less loneliness compared to younger age groups (i.e., 17–64). Given robust literature demonstrating protective effects of social connectedness (e.g., Nitschke et al., Reference Nitschke, Forbes, Ali, Cutler, Apps and Lockwood2021), neutral effects of frequency of social communication among older adults (e.g., Werner-Seidler et al., Reference Werner-Seidler, Afzali, Chapman, Sunderland and Slade2017), and detrimental effects of loneliness (e.g., Beutel et al., Reference Beutel, Klein, Brähler, Reiner, Jünger and Michal2017;), we also hypothesized that 2) higher perceived social support would be associated with better mental health across age groups; 3) frequency of communication would predict better mental health in younger (i.e., 17–34 years old), but not middle-aged and older (i.e., over 35), age groups; and 4) loneliness would be positively associated with negative mental health across age groups; but that 5) this association would be stronger in younger (i.e., 17–24, 25–34 years old) versus older (i.e., 65 and over) age groups. Finally, we hypothesized that 6) there would be significant moderation effects of perceived social support and frequency of communication in older adults, with the association between loneliness and poorer mental health stronger at low levels of social support, while for younger groups, this association would be stronger for those not engaged in at least daily (technology-assisted) communication.
Methods
Participants
A nationwide, online survey was administered to a convenience sample of Canadians (with recruitment quotas for age and sex, and by province; n = 8,646, 59.0% female) between August 18 and October 1, 2020, in the context of a larger international study assessing the impacts of the COVID-19 pandemic on mental health functioning (Rathod et al., Reference Rathod, Pallikadavath, Young, Graves, Rahman and Brooks2020). For the Canadian survey, participants were required to be 1) living in Canada, 2) ages 17 years and older, and 3) able to complete the online survey. Participants were recruited via social media advertising (i.e., Facebook and Instagram using unpaid, non-targeted posts; n = 629) and through a sample and data services company (MARU/Blue; n = 8,017) to participate in an online survey investigating the impacts of the COVID-19 pandemic and lockdown on Canadians’ mental health and well-being. The survey was open for any eligible participant to complete. For participants recruited through MARU/Blue, we set quotas by age, sex, and province to match population proportions from the 2019 Canadian census. According to MARU/Blue’s internal metrics, 10,558 individuals viewed or initiated the survey, and 4,745 individuals completed the survey (metric data were unavailable for individuals recruited by MARU/Blue through partner sources and via social media).
Procedure
The following procedures are reported in accordance with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES; Eysenbach, Reference Eysenbach2004). The survey was independently piloted by research assistants for item clarity, survey length, and skip logic. Our social media advertisements contained an open link to the online survey, hosted on the Qualtrics Survey platform, while additional participants were recruited by MARU/Blue using their internal participant database. The link directed participants to the consent form, which detailed the purpose, scope and length of the study, data storage and privacy, compensation, study withdrawal, and how to contact the researchers for additional questions. Participants recruited via social media were offered an entry into a draw for various gift cards as compensation for their participation (identifying information was saved separately from anonymous survey responses), and participants recruited via MARU/Blue were awarded points for completing the survey in accordance with MARU/Blue’s compensation structure. Participants checked a box to indicate their consent to participate. Consenting participants were then automatically directed to the eligibility screening questions (i.e., ages 17 years and older, residing in Canada), and eligible participants were directed to begin the survey. The survey took approximately 15–20 minutes to complete and contained predominantly closed-ended, non-randomized items pertaining to demographics; mental-health functioning; and emotional, social, living, and working circumstances. Skip logic adaptive functioning was programmed to ensure that participants were only shown questions that were relevant to them (e.g., if participants reported they were retired, they did not see questions pertaining to work environment). Participants could navigate back between pages to change survey responses and could close the survey at any time if they wished to withdraw (survey responses were saved after the final page of responses was submitted, provided that the survey was completed within 1 week of the survey closure; otherwise, partial data were collected). De-identified survey data were stored in an encrypted cloud server that only members of the research team had access to. All aspects of the study for the Canadian cohort were approved by the Human Research Ethics Board at the University of Victoria.
Measures
Age
Participants were asked to indicate their age group using a single item (i.e., “Under 21,” “21-24,” “25-34,” “45-44,” “45-54,” “55-64,” and “65 and over”). Alternative 10-year age bands (e.g., “18-29,” “30-39,” … “60-69,” and “70 and over”) were used for stratification of the MARU/Blue sample, allowing us to further divide the 65-and-over age group into “65-69” and “70 and over” age groups. Due to small sample sizes, the under 21 and 21-24 age groups were combined into a single age group (i.e., 17-24) for analyses. The final age groups used in these analyses are as follows: 17-24, 25-34, 45-44, 45-54, 55-64, 65-69, and 70 and over.
Depression
Depressive symptoms were assessed using the Patient Health Questionnaire (PHQ-9; Kroenke & Spitzer, Reference Kroenke and Spitzer2002). The PHQ-9 comprises nine items querying depressive symptoms (e.g., “Feeling down, depressed, or hopeless”; “Little interest or pleasure in doing things”; “Feeling tired or having little energy”) over the past 2 weeks. Responses on the PHQ-9 are rated on a 4-point Likert scale (i.e., “Not at all” to “Nearly every day”) such that higher scores reflect more severe symptoms. A score of 10 or more on this measure indicates at least moderate depression. The PHQ-9 has demonstrated good validity and reliability in general population samples (Kroenke & Spitzer, Reference Kroenke and Spitzer2002) and had excellent internal consistency in our sample (Cronbach’s α = 0.93).
Anxiety
Symptoms of anxiety were assessed using a slightly modified version of the Generalized Anxiety Disorder 7 (GAD-7; Spitzer, Kroenke, Williams, & Löwe, Reference Spitzer, Kroenke, Williams and Löwe2006). This measure comprises seven items querying symptoms associated with generalized anxiety over the past 2 weeks (e.g., “Feeling nervous, anxious or on edge”; “Trouble relaxing”; “Not being able to stop or control worrying”). The GAD-7 was modified to specifically query anxiety symptoms in relation to the pandemic; participants were instructed to consider whether they experienced “the following problems specifically in relation to coronavirus.” Responses are rated on a 4-point Likert scale (i.e., “Not at all” to “Nearly every day”) such that higher scores reflect more severe anxiety. A score of 10 or more indicates at least moderate anxiety. The unmodified GAD-7 shows good reliability and validity in general primary care patient samples (Spitzer et al., Reference Spitzer, Kroenke, Williams and Löwe2006), and this modified version had excellent internal consistency in our sample (Cronbach’s α = 0.94).
Trauma-related stress
Psychological trauma-related stress symptoms due to the COVID-19 pandemic were examined using a slightly modified version of the Impact of Events Scale-Revised (IES-R; Weiss & Marmar, Reference Weiss, Marmar, Wilson and Keane1997). The IES-R is a 22-item scale that captures distressing symptoms related to traumatic events or stressors over the past 7 days (e.g., reminders, avoidance, irritability). The IES-R was modified to query symptoms of trauma-related stress associated with the pandemic; participants were asked to consider, “… how distressing each difficulty has been for you … with respect to the current coronavirus outbreak?” Responses on the IES-R are rated on a 5-point Likert scale (i.e., “Not at all” to “Extremely”) such that higher scores reflect more severe symptoms, with scores of 24 or more indicating posttraumatic stress disorder (PTSD) may be a clinical concern. The unmodified IES-R shows good reliability and validity in patient and general population samples experiencing grief or loss (Weiss & Marmar, Reference Weiss, Marmar, Wilson and Keane1997), whereas the modified version had excellent internal consistency in our sample (Cronbach’s α = 0.97).
Perceived social support
Perceived social support was assessed using a slightly modified version of the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1988). The MSPSS is a 12-item scale that assesses subjective social support (e.g., “I can count on my friends/family for support”). The modified version asked, "How do you feel about the following statements in light of the coronavirus outbreak?” Responses are rated on a 7-point Likert scale (i.e., “Very strongly disagree” to “Very strongly agree”) with higher scores reflecting more perceived social support. The MSPSS shows good reliability and moderate to good validity in university undergraduates (Zimet et al., Reference Zimet, Dahlem, Zimet and Farley1988) and older adults with and without psychiatric conditions (Stanley, Beck, & Zebb, Reference Stanley, Beck and Zebb1998), and it had excellent internal consistency in our sample (Cronbach’s α = 0.94).
Loneliness
Feelings of loneliness and social isolation were assessed using the UCLA 3-item Loneliness Scale (Hughes, Waite, Hawkley, & Cacioppo, Reference Hughes, Waite, Hawkley and Cacioppo2004). Responses are on a 3-point Likert scale (i.e., “Hardly ever,” “Some of the time,” and “Often”) with higher scores reflecting more loneliness. The 3-item UCLA Loneliness Scale has been shown to have good reliability and validity (Hughes et al., Reference Hughes, Waite, Hawkley and Cacioppo2004) and had good internal consistency in our sample (Cronbach’s α = 0.89).
Mental health diagnoses and changes in functioning
Participants were asked, “Do you have any pre-existing, diagnosed mental health conditions?” Participants who indicated that they had a mental health condition were also asked to rate how their mental health had changed since the start of the COVID-19 pandemic (i.e., “My mental health has improved,” “My mental health has got worse,” “No change,” or “Not sure”).
Substance use
Participants who indicated that they drank alcohol (i.e., “How often do you have a drink containing alcohol?”) on a previous item were then asked to indicate how their drinking had changed since the start of the COVID-19 pandemic (i.e., “Increased,” “Decreased,” “Stayed the same,” “Not sure”). Participants who indicated that they consumed recreational drugs (i.e., “Do you use drugs other than those required for medical reasons?”) were asked the same question regarding changes since the start of the pandemic, with the same response options.
Technology-assisted social communication
Participants were asked how often they communicate with family/friends using the following four technology-assisted methods: messaging services (e.g., WhatsApp, text messages), telephone calls, video calls, and social media (i.e., “Several times a day,” “Daily,” “Every few days,” “Not at all”). The highest endorsed frequency across all four technology-assisted social communication methods was assigned as a given participant’s communication frequency score. For example, if a participant responded “Daily” to messaging services use and “Every few days” to telephone call use, their frequency of technology-assisted social communication was assigned as “Daily.” Frequency of technology-assisted communication was then coded into a dichotomous variable for all analyses; “Not at all” and “Every few days” were coded together, whereas “Daily” and “Several times a day” were coded together to distinguish between participants engaging and not engaging in at least daily technology-assisted social communication.
Data Cleaning
The data (n = 8,646) was screened for multiple responses from the same IP address (for those completing via social media recruitment; those completing via MARU/Blue were unable to do so more than once due to MARU’s participant ID system). Participants who displayed fast responding, failed catch questions, and/or had incomplete responding were also flagged as failing screening criteria (n = 2,017) and removed from the data set, resulting in a sample of 6,629.Footnote 1 Participants who failed to complete one or more measures of interest were also removed (n = 1,256), to ensure uniform sample size across study analyses. Participants who did not complete the additional age item that allowed further stratification of our 65-and-over age group into “65–69” and “70-and-over” groups were also removed (n = 53). A total of 1,309 participants were excluded due to missing data, and the final sample size for all analyses was 5,320.
Data Analyses
All analyses for the current study were conducted using IBM SPSS, version 26.
Aim 1
Demographics. The χ2 analyses were conducted to examine differences across age groups on several categorical demographic variables (i.e., sex, ethnicity, geographic region, education level, employment status, living situation, self-isolation, and social distancing compliance).
Mental health and social connectedness. The χ2 analyses were also used to examine differences across age groups on categorical mental health and social connectedness variables, including changes in mental health functioning, and alcohol and drug use since the start of the COVID-19 pandemic, previous mental health diagnosis status, and at least daily technology-assisted social communication. For these analyses, pairwise post-hoc comparisons were performed using Bonferroni-corrected pairwise z-tests. Next, a series of one-way analysis of variance (ANOVA) were conducted to examine age group differences on continuous mental health and social connectedness outcomes, including depression, anxiety, trauma-related stress, loneliness, and social support (Table 1). For ANOVA and χ2 analyses, we report p-values and effect sizes. For pairwise post-hoc comparisons, Tukey’s “honest significant difference” test was used when F was interpreted, and Games-Howell test was used when Welch’s F was interpreted.
Table 1. Participant characteristics

Notes. All values represent proportions (%). Superscripts denote post-hoc test results, whereby matching superscripts denote no significant difference.
† Self-isolating due to own symptoms or due to symptoms of other co-dweller(s).
Aims 2 and 3
Associations. Preliminary analyses were conducted to examine associations between demographic (e.g., sex), mental health status (e.g., pre-existing condition, changes in mental health functioning), mental health outcomes (e.g., depression, anxiety, and trauma-related stress), and social connectedness variables (e.g., loneliness, social support, and daily technology-assisted communication). To confirm that mental health differences across age groups were not due to differences in pre-existing diagnosis alone, a preliminary analysis of covariance (ANCOVA) was used to examine age group differences in mental health measures when controlling for pre-existing mental health diagnosis, ethnicity, and sex.
Predictors and moderators of mental well-being. A series of hierarchical multiple regression analyses were conducted in each age group to examine whether loneliness, social support, and frequency of technology-assisted social communication were associated with variance in symptoms of depression, anxiety, and trauma-related stress within a given age group. Firstly, pre-existing mental health diagnoses, sex, and ethnicity were entered into the model (block 1) as control variables. Secondly, continuous independent variables (i.e., loneliness and social support) were mean-centred to reduce collinearity and entered into the model, along with frequency of technology-assisted social communication (block 2). Finally, two interaction terms, loneliness by social support and loneliness by frequency of technology-assisted social communication, were calculated using mean-centred variables and entered into the model (block 3). The variance inflation factors remained below 10 for all variables in all models. The final model included all control and independent variables and any significant interaction terms. To compare the importance, or weight, of our predictors in determining mental health outcomes across age groups, regression coefficients from each age group model were compared to one another (only regression coefficients that were significant in a particular model were compared to significant coefficients in other models). Specifically, we used z score estimates to quantify the difference between model coefficients (for equation, see Paternoster, Brame, Mazerolle, & Piquero, Reference Paternoster, Brame, Mazerolle and Piquero1998). Model coefficients were determined to be significantly different from one another if the z score estimate exceeded the two-tailed critical value.
Results
Sample Characteristics
The χ2 analyses were conducted to determine whether there were significant differences between participants excluded due to missing data (n = 1,309) versus those included (n = 6,629). There were no significant differences between the excluded and included sample in sex, ethnicity (i.e., White vs. other), education, living alone, or self-isolating. A higher proportion of those excluded resided in British Columbia, whereas a higher proportion of those included resided in Ontario (χ2(12) = 41.7, p < 0.001). Significant differences were seen for employment (i.e., full-time employment and unemployment higher in included sample; more retired participants in excluded sample; χ2(10) = 30.89, p = 0.001). A higher proportion of the excluded sample also reported not following social distancing guidelines (χ2(1) = 6.77, p = 0.009).
Aim 1
Demographics. Participant characteristics for the study sample (n = 5,320) are summarized in Table 1. Notably, there were more females than males in younger age groups (71.7-73.5% female) compared to older age groups (45.5-61.3% female; p < 0.001, Cramer’s V = 0.19), diverging from the Canadian census, which reflects a relatively even sex distribution across age groups under age 65 (Statistics Canada, 2019). Additionally, diversity of the sample significantly decreased with increasing age; 55.8% of the 17-24 age group self-identified as White compared to 96.1% of the 70-and-over age group (p < 0.001, Cramer’s V = 0.14), which somewhat resembles the distribution of visible minorities across the lifespan in Canada (Statistics Canada, 2018). There were expected differences across age groups in education (p < 0.001, Cramer’s V = 0.10) such that a greater proportion of older and middle-aged adults had completed at least some post-secondary education relative to younger adults. In terms of employment status, most young- and middle-aged adults (25-34 through 45-54 age groups) were employed full-time, whereas most older adults (65-69 and 70 and over) were retired (p < 0.001, Cramer’s V = 0.39). A smaller proportion of adults ages 17-24 reported living alone (11.7%) compared to other, older age groups (18.8-30.1%; p < 0.001, Cramer’s V = 0.11). While the majority of individuals in all age groups reported compliance with social distancing public health guidelines, compliance was highest in the oldest adults (70 and over; 72.9%; p < 0.001, Cramer’s V = 0.08). The proportion of individuals reporting that they had to self-isolate at some point due to COVID-19 symptoms (own symptoms or symptoms of co-dwellers) was greater for younger age groups (12.7% in the 17-24 group vs. 1.7-2.7% in age groups 55 and up; p < 0.001, Cramer’s V = 0.14).
Mental health and social connectedness. The χ2 post-hoc analyses revealed significant differences across most age groups on prevalence of pre-existing mental health diagnosis (p < 0.001, Cramer’s V = 0.22) such that the proportion of adults with a pre-existing diagnosis generally declined across increasing age groups (post-hoc p’s < 0.05; Table 2). Among those who endorsed a pre-existing mental health diagnosis, there were significant age-related differences in changes in mental health since the start of the COVID-19 pandemic, such that a smaller proportion of older adults (65-69 and 70 and over) reported worsened mental health since the start of the pandemic, relative to most other age groups (p < 0.001, Cramer’s V = 0.15, post-hoc p’s < 0.05). Likewise, smaller proportions of older adults reported increased alcohol use (p < 0.001, Cramer’s V = 0.14, post-hoc p’s < 0.05). Finally, smaller proportions of older adults (70 and over) reported increased drug use relative to adults ages 17-24 (p < 0.001, Cramer’s V = 0.16, post-hoc p’s < 0.05).
Table 2. Group comparisons

Notes. In all ANOVA, the homogeneity of variances assumption was violated and therefore the reported effect size is omega squared (ω2) instead of partial eta squared (ηp2). Values for the PHQ-9, GAD-7, IES-R, perceived social support, and loneliness are displayed as the mean (standard deviation). All other values are displayed as proportions (%). Superscripts denote post-hoc test results whereby matching superscripts denote no significant difference.
† Only participants who reported a mental health diagnosis, alcohol use, or drug use were asked to respond to these items.
Results from one-way ANOVA revealed significant differences (p’s < 0.001) between age groups on depression scores (ω2 = 0.14), anxiety (ω2 = 0.12), and trauma-related stress (ω2 = 0.08) such that scores steadily decreased as age increased, with those ages 17-24 generally reporting the most depression, anxiety, and trauma-related stress (see Table 2; Figure 1). For depression, there were significant differences in scores between most age groups (post-hoc p’s < 0.001) except for between 35-44 and 45-54, 55-64 and 65-69, and 65-69 and 70-and-over age groups. For anxiety, there were significant differences in scores between most age groups (post-hoc p’s < 0.001) except for between the 17-24 and 25-34 age groups, and 65-69 and 70-and-over age groups. For trauma-related stress, there were significant differences in scores between most age groups (post-hoc p’s < 0.001) except for between 17-24 and 25-34, 55-64 and 65-69, and 65-69 and 70-and-over age groups.

Figure 1. Results of depression, anxiety, and trauma-related stress scores by age group. Error bars represent Standard Error.
With respect to social connectedness, there were significant differences (p’s < 0.001) between age groups for perceived social support (ω2 = 0.002), loneliness (ω2 = 0.07), and daily technology-assisted social communication (Cramer’s V = 0.25). For perceived social support, there were significant differences in scores such that older adults (70 and over) reported higher perceived social support than the 17-24 age group (post-hoc p’s < 0.001). For loneliness, there were significant differences in scores between most age groups, except between 65-69 and 70-and-over age groups, such that scores decreased as age increased (post-hoc p’s < 0.001). For engagement in at least daily technology-assisted social communication, there were significant differences between age groups (post-hoc p’s < 0.001) such that smaller proportions of older adults (70 and over) endorsed at least daily technology-assisted communications relative to most other age groups. While there were no significant differences between age groups in using telephone calls for daily communication, higher proportions of younger adults (17-24) endorsed using social media and video calls for daily communication relative to all other age groups (post-hoc p’s < 0.001).
Aims 2 and 3
Preliminary correlations between mental health and social connectedness variables. Each social connectedness variable was correlated with each mental health scale in the expected directions (p’s < 0.01), justifying their inclusion in regression models. Significant correlations were also found between our control variables (sex, ethnicity, and mental health diagnosis) and mental health measures (p’s < 0.01; Table 3). Additionally, after controlling for mental health diagnosis, ethnicity, and sex, there were still differences between age groups on scores on depression (ηp2 = 0.28), anxiety (ηp2 = 0.23), and trauma-related stress (ηp2 = 0.17).
Table 3. Association matrix

Notes. For sex: 0 = male, 1 = female; for mental health diagnosis: 0 = no diagnosis, 1 = at least one diagnosis. Associations between continuous variables were computed as Pearson correlations. Associations between dichotomous categorical variables and continuous variables were computed as Point Biserial correlations. Associations between dichotomous categorical variables were computed as Phi coefficients.
* p < 0.05, **p < 0.01
Social connectedness predictors and interactions of mental well-being. After controlling for pre-existing mental health diagnosis, sex, and ethnicity, loneliness was the strongest predictor of symptoms of depression, anxiety, and trauma-related stress across all age groups, such that increased loneliness was associated with higher scores on depression, anxiety, and trauma-related stress scales. Other age-group-specific results from final regression models are outlined below. Results from regression analyses can also be found in Tables 4 and S1 (depression), Tables 5 and S2 (anxiety), and Tables 6 and S3 (trauma-related stress). Tables 4-6 contain only final models (only significant interaction terms retained), and Tables S1-S3 contain full hierarchical regression analyses (all models).
Table 4. Depression final regression models

Notes. Bolded values are significant at p < 0.05.
MH Dx = mental health diagnosis; PSS = perceived social support; Freq. Comm.= minimum daily technology-assisted communication; Lone = loneliness; and SE = standard error.
Table 5. Anxiety final regression models

Notes. Bolded values are significant at p < 0.05.
MH Dx = mental health diagnosis; PSS = perceived social support; Freq. Comm.= minimum daily technology-assisted communication; Lone = loneliness; and SE = standard error.
Table 6. Trauma-related stress final regression models
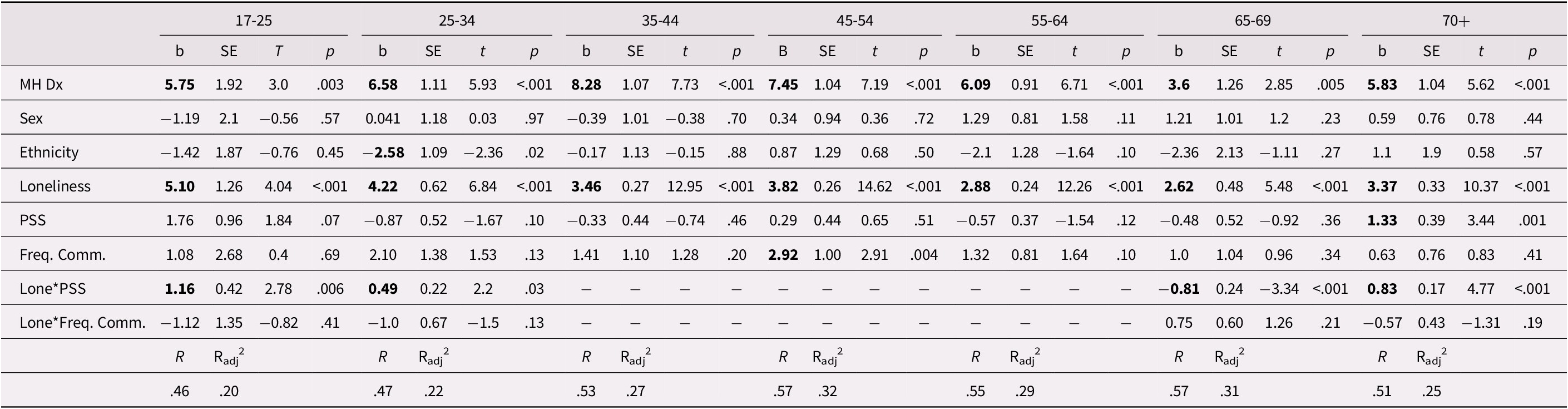
Notes. Bolded values are significant at p < 0.05.
MH Dx = mental health diagnosis; PSS = perceived social support; Freq. Comm. = minimum daily technology-assisted communication; Lone = loneliness; and SE = standard error.
17-24 Group ( n = 403). For trauma-related stress symptoms, there was a significant interaction between loneliness and social support such that higher social support was associated with increased trauma-related stress symptoms only at high levels of loneliness.
25-34 Group ( n = 1,048). For depression symptoms, there were additional significant main effects of social support and frequency of technology-assisted social communication such that lower social support and having no daily technology-assisted social communication were associated with increased depression symptoms. For trauma-related stress symptoms, there was also a significant interaction between loneliness and social support such that higher social support was associated with a decrease in trauma-related stress symptoms only at low and average levels of loneliness.
35-44 Group ( n = 987). Aside from loneliness, there were no other significant main effects or interactions.
45-54 Group ( n = 895). For trauma-related stress symptoms, there was a main effect of frequency of technology-assisted social communication such that engaging in at least daily technology-assisted communication was associated with increased trauma-related stress symptoms.
55-64 Group ( n = 851). For depression and anxiety symptoms, there were also significant main effects of social support such that higher social support was associated with decreased symptoms of depression and anxiety. Additionally, there was a significant main effect of frequency of technology-assisted social communication for anxiety, such that engaging in at least daily technology-assisted communication was associated with increased anxiety symptoms.
65-69 Group ( n = 439). For all three mental health outcomes, there was a significant interaction between loneliness and social support such that higher social support was associated with decreased depression, anxiety, and trauma-related stress symptoms only at high and average levels (depression) and high levels (anxiety and trauma-related stress) of loneliness.
70-and-Over Group ( n = 697). For anxiety and trauma-related stress symptoms, there was a significant main effect of perceived social support such that higher social support was associated with increased anxiety and trauma-related stress symptoms only at average and high levels of loneliness.
Comparison of regression coefficients. The effect of loneliness on symptoms of depression was significantly less salient in 70 and over and 55-64 age groups compared to 17-24 (z = 3.24, p < 0.05; z = 2.23, p < 0.05), 25-34 (z = 4.05, p < 0.05; z = 2.48, p < 0.05), 35-44 (z = 2.68, p < 0.05; not significantly different from the 55-64 group), and 45-54 (z = 4.86, p < 0.05; z = 3.25, p < 0.05) age groups. As well, the effect of loneliness on symptoms of depression was significantly less salient in 35-44 and 65-69 age groups compared to the 45-54 age group (z = 2.12, p < 0.05; z = 2.09, p < 0.05). The effect of loneliness on anxiety symptoms was significantly less salient in 55-64 and 65-69 age groups compared to 25-34 (z = 2.63, p < 0.05; z = 2.13, p < 0.05) and 45-54 (z = 2.68, p < 0.05; z = 2.13, p < 0.05) age groups. The effect of loneliness on anxiety symptoms was also significantly less salient in the 70-and-over age group compared to the 55-64 age group (z = 2.33, p < 0.05). The effect of loneliness on trauma-related stress symptoms was significantly less salient in 55-64 and 65-69 age groups compared to 25-34 (z = 2.02, p < 0.05; z = 2.04, p < 0.05) and 45-54 (z = 2.67, p < 0.05; z = 2.19, p < 0.05) age groups. There were no significant differences between age groups in the strength of regression coefficients for perceived social support or at least daily technology-assisted communication.
Discussion
Consistent with previous research examining age-based differences in mental health functioning during the COVID-19 pandemic (e.g., García-Portilla et al., Reference García-Portilla, de la Fuente Tomás, Bobes-Bascarán, Jiménez Treviño, Zurrón Madera and Suárez Álvarez2020; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021) and in support of our hypothesis, results demonstrated that mental health is generally better in older age groups. Specifically, older adults reported fewer symptoms of anxiety, depression, trauma-related stress and less loneliness (but not social support), and smaller proportions of older adults reported worsened mental health and increased alcohol and drug use since the start of the COVID-19 pandemic, suggesting that older adults are faring better on several key indicators of mental health functioning. In partial support of our hypotheses, higher perceived social support was associated with better mental health for some (25-34, 55-64, and 65-69) but not all age groups, and having at least daily technology-assisted social communication was associated with better mental health for some younger adults (i.e., those ages 25-34, but not those ages 17-24). In support of our hypotheses, loneliness emerged as a robust predictor of negative mental health outcomes across all age groups, though the effects of loneliness on mental health were less salient for older adults (i.e., 55-64, 65-69, and 70 and over) compared to all other age groups. Contrary to our hypothesis, neither social support nor frequency of technology-assisted social communication moderated associations between loneliness and mental health; however, loneliness was seen to moderate associations between social support and mental health outcomes in some age groups. Overall, our findings suggest that 1) older Canadian adults are more resilient in their mental health functioning relative to younger adults, and 2) indicators of quality and quantity of social interactions and loneliness are differentially important in predicting mental health across age groups. These findings suggest that mental health intervention in younger adults should be geared towards increasing resilience, while, among some older adults, particularly lonely older adults, interventions focused on increasing social support may be of more benefit.
Loneliness has emerged as an important determinant of mental health functioning during the pandemic (García-Portilla et al., Reference García-Portilla, de la Fuente Tomás, Bobes-Bascarán, Jiménez Treviño, Zurrón Madera and Suárez Álvarez2020; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). In our sample, the oldest age group (70 and over) had the highest proportion of individuals living alone and the lowest prevalence of engaging in at least daily technology-assisted social interaction compared to all other, younger age groups, despite also reporting the lowest scores of loneliness. This finding illuminates the important distinction between objective social isolation (i.e., physical isolation, frequency of communication) and subjective feelings of social isolation (i.e., feelings of loneliness; de Jong Gierveld, Van Tilburg, & Dykstra, Reference de Jong Gierveld, Van Tilburg and Dykstra2006). Consistent with past research, our results support a robust association between loneliness and mental health outcomes (e.g., Beutel et al., Reference Beutel, Klein, Brähler, Reiner, Jünger and Michal2017) and indicate that loneliness exerts a less salient effect on mental health in older adults (ages 55 and over; Varma et al., Reference Varma, Junge, Meaklim and Jackson2021). This age-related difference may be driven by older adults’ greater use of adaptive coping, which has been shown to be more effective in reducing negative affect and stress in older, compared to younger, adults (Charles & Carstensen, Reference Charles and Carstensen2008; Pearman, Hughes, Smith, & Neupert, Reference Pearman, Hughes, Smith and Neupert2021) and is negatively associated with loneliness among older adults (Raut et al., Reference Raut, Singh, Subramanyam, Pinto, Kamath and Shanker2014). Disparities in efficiency of active coping across the lifespan (e.g., Blanchard-Fields, Reference Blanchard-Fields2007; Kraaij, Pruymboom, & Garnefski, Reference Kraaij, Pruymboom and Garnefski2002; Phillips, Henry, Hosie, & Milne, Reference Phillips, Henry, Hosie and Milne2008) may help explain why older adults are experiencing less loneliness and resultant negative mental health consequences relative to younger adults. Bolstering adaptive coping skills may be an intervention target for decreasing loneliness and, in turn, boosting resiliency during periods of public health restrictions. Future research should directly test the role of adaptive coping in mental health functioning in the pandemic context.
Differing expectations and needs for social communication and support across the adult age-span may also help explain observed age-related differences in loneliness and mental health functioning. Given that older adults may have already adjusted to a smaller social sphere prior to the pandemic (Antonucci, Reference Antonucci, Birren and Schaie2001), they may be experiencing less resultant loneliness and psychological stress due to self-isolation and social distancing (Best et al., Reference Best, Law, Roach and Wilbiks2020; Dozois, Reference Dozois2020). Indeed, our findings demonstrate that, although a greater proportion of younger Canadians are attempting to stay connected through technology-assisted communication, these efforts do not appear sufficient in fulfilling young adults’ emotional needs for social connectedness, as they report being lonelier. One explanation for this age disparity in loneliness may be that younger adults are using social media as their preferred platform communication, which is known to negatively impact mental health (Gao et al., Reference Gao, Zheng, Jia, Chen, Mao and Chen2020; Hong et al., Reference Hong, Liu, Ding, Fu, Zhen and Sheng2020). Indeed, a greater proportion of those ages 17-24 reported using social media as their platform for technology-assisted communication, indicating that using social media to communicate with others may counteract the positive effects of social communication and support. Additionally, the oldest adults (70 and over) reported the highest perceived social support, on average, despite engaging in less frequent technology-assisted communication. This dichotomy may reflect decreased social needs among older adults relative to younger adults (Krendl & Perry, Reference Krendl and Perry2021). Together, these differences may help explain age-related variability in loneliness across age groups and suggest that method, rather than frequency, of engagement in technology-assisted communication is important in garnering positive effects of social connectedness and support, and buffering against loneliness. Younger adults may benefit from spending more time connecting through other virtual means such as phone or video calls.
Regarding the role of social support, there was an expected negative association with mental health difficulties for only the 25-34, 55-64, and 65-69 age groups, and a positive association between mental health difficulties and social support for the 17-24 and 70-and-over age groups. This is surprising given that social support is robustly associated with better health functioning across the lifespan (Harandi, Taghinasab, & Nayeri, Reference Harandi, Taghinasab and Nayeri2017; Siedlecki, Salthouse, Oishi, & Jeswani, Reference Siedlecki, Salthouse, Oishi and Jeswani2014; Wang, Wu, & Liu, Reference Wang, Wu and Liu2003). As previously mentioned, the 17-24 age group reported the most frequent use of social media for technology-assisted communication with others. Past research suggests a positive association between social media use and perceived social support (Lu & Hampton, Reference Lu and Hampton2017). As such, the perceived social support reported by individuals in the 17-24 age group may largely stem from connections forged and strengthened through social media use, instead of connections forged through other means (e.g., phone or video calls). Because social media use can negatively impact mental health, particularly during the COVID-19 pandemic where there may be increased exposure to stressful information on social media (Gao et al., Reference Gao, Zheng, Jia, Chen, Mao and Chen2020), it may be that social support garnered via social media use is having negative impacts on mental health. This explanation is unlikely to apply to the positive association between social support and mental health in the 70-and-over age group since a very low proportion of this group reported using social media to communicate on at least a daily basis. Given the causal direction of this association is unknown, it is possible oldest adults experiencing greater mental health concerns are currently more reliant on their social networks for support, and therefore report higher perceived social support. It might also reflect the fact that when oldest adults reach out for support, they perceive their needs as having been met, whereas this may not be the case for younger adults, who may be less skilled at identifying their needs and making maximal use of their social networks.
Similarly, given past research suggesting that frequency and availability of social contact are important to younger adults (Williams & Galliher, Reference Williams and Galliher2006), but less important to older adults (Krendl & Perry, Reference Krendl and Perry2021; Werner-Seidler et al., Reference Werner-Seidler, Afzali, Chapman, Sunderland and Slade2017), it is surprising that not engaging in at least daily communication was associated with worse mental health outcomes for those ages 25-34, but was not for those ages 17-24. Although a large proportion of both age groups were engaging in at least daily communication, the 17-24 group reported using more social media and video calls for their daily communication relative to the 25-34 group. Again, given the negative associations between social media use and mental health (Gao et al., Reference Gao, Zheng, Jia, Chen, Mao and Chen2020; Hong et al., Reference Hong, Liu, Ding, Fu, Zhen and Sheng2020), increased social media use may be obscuring the association between engaging in daily technology-assisted communication and better mental health in the 17-24 age group. Furthermore, engaging in at least daily technology-assisted communication was associated with poorer mental health among those ages 45-64; however, given the causal directionality of the association is unknown, this may reflect the fact that those with poorer mental health are reaching out more often (using technology) for support, and thus may represent a positive coping mechanism (Wills, Reference Wills1987). Future research should examine the age-dependent role of technology-assisted communication as both a positive coping mechanism and as potentially harmful to mental health.
Our moderation analyses also revealed a negative association between social support and mental health in adults ages 65-69, only at average and high levels of loneliness. This finding corroborates past research suggesting that social support is a protective factor against poor mental health outcomes (e.g., Newman & Zainal, Reference Newman and Zainal2020; Saeri, Cruwys, Barlow, Stronge, & Sibley, Reference Saeri, Cruwys, Barlow, Stronge and Sibley2018; Schwartz & Litwin, Reference Schwartz and Litwin2019) and further explains this association by highlighting the importance of social support for older adults specifically experiencing average to high levels of loneliness. However, our moderation analyses also revealed that there was a positive association between social support and mental health outcomes in adults ages 70 and over, at average and high levels of loneliness. There are several possibilities as to why an opposite moderation effect was found for the 65-69 and 70-and-over age groups. Firstly, the 70-and-over age group represents a large age-span compared to the 65-69 age group. As such, it is possible that these moderation effects may be artificially driven by those in the 70-and-over group, especially since loneliness has been shown to share a U-shaped association with age, increasing after age 80 (Beam & Kim, Reference Beam and Kim2020). Secondly, there was less variance accounted for by the final model for both anxiety and trauma-related stress in the 70-and-over age group compared to the 65-69 age group, suggesting that other factors not accounted for may better explain mental health in the 70-and-over group, for example, life experiences that become more common with older age, such as caring for a spouse or family member or having a serious chronic illness (Vahia et al., Reference Vahia, Jeste and Reynolds2020). Finally, depression symptoms were notably not correlated with sex in any of the final models, and even in initial models (prior to entering predictor variables of interest), sex was only correlated with depression symptoms in 25-34 and 55-64 age groups. This is surprising given that depression has been shown to disproportionally affect women (Salk, Hyde, & Abramson, Reference Salk, Hyde and Abramson2017). A likely explanation is that previous mental health diagnosis was also included in the initial model, which likely over-powered the effect of sex and, moreover, is conflated with sex as mental health diagnosis rates typically vary by gender/sex. Future research should further explore the role of sex in mental health in the context of the COVID-19 pandemic, as the circumstances of the pandemic may also play a role in the lack of association between sex and depression.
Limitations and Future Directions
While our study offers several strengths, including its large sample with age, sex, and province quotas, and examination of key mental health outcomes, there are several limitations. Older adults are a heterogeneous population, and therefore the lack of granularity in our oldest age category (i.e., 70 and over) may mask some differences that exist across the oldest age-span. Longitudinal studies suggest loneliness is relatively stable from ages 60 to 80 years and then increases (Beam & Kim, Reference Beam and Kim2020), and that progressive changes in cognitive, functional, and mental health status are seen between ages 70 and 85 (Jacobs et al., Reference Jacobs, Maaravi, Cohen, Bursztyn, Ein-Mor and Stessman2012). Older age is also associated with increased likelihood of stressful life events (e.g., bereavement, caretaking, physical illness or disability; Fiske, Wetherell, & Gatz, Reference Fiske, Wetherell and Gatz2009), which present a risk factor for negative mental health outcomes. Research focused specifically on these oldest age bands is necessary to better elucidate mental health and social needs specific to these oldest age groups during the pandemic.
The prevalence of having a pre-existing mental health diagnosis was much higher in our sample (in most age groups, see Table 2) compared to what would be expected in the general population (approximately 20%; Mental Health Commission of Canada, 2013). It is unclear whether this reflects self-reporting bias (e.g., participants endorsing subjective mental health concerns in addition to formal diagnoses) or self-selection bias in sampling (e.g., consent materials described the study focus as mental health). However, we controlled for pre-existing mental health diagnosis/concerns in relevant analyses, and therefore our results are likely still generalizable to individuals without specific mental health diagnoses or concerns. Of note, on average, most age groups reported fewer symptoms of anxiety, depression, and psychological stress relative to another Canadian study conducted at the onset of the pandemic (Nwachukwu et al., Reference Nwachukwu, Nkire, Shalaby, Hrabok, Vuong and Gusnowski2020), and, as such, our sample does not appear to disproportionally represent those with higher current mental health concerns.
In terms of study design, our study employed a cross-sectional research design and, as such, cannot speak to directionality of observed associations and mental health trajectories throughout the pandemic. Moreover, our study was administered online. As a result, we were unable to collect data from marginalized groups lacking resources or knowledge to access an online survey (e.g., individuals experiencing homelessness). Evidence suggests that these marginalized groups are at a disproportionally higher risk of experiencing negative health (including mental health) during the pandemic (Vahia et al., Reference Vahia, Jeste and Reynolds2020). Future research should attempt to administer surveys that are accessible to these groups as they may have unique mental health and social needs as the pandemic continues.
These data were collected at a single time point approximately 5-6 months after the World Health Organization declared a global pandemic (August-October, 2020), and thus results may not be generalizable as public health restrictions and COVID-19 virus infection rates change. Longitudinal investigations to examine the evolution of mental health concerns as the pandemic continues and as vaccination rates increase would be beneficial.
Finally, although we recruited participants to fulfill quotas of age, sex, and geographic region in accordance with the Canadian census, we were unable to provide an entirely balanced demographic representation within age groups (e.g., 95.3% of participants in the combined 65-69 and 70-and-over age groups were White compared to 87.4% according to the latest census; Statistics Canada, 2018). Therefore, our findings may not be directly generalizable to visible minority Canadians. Future work with more racially balanced samples is warranted to ensure that findings are generalizable, particularly to older adults of diverse backgrounds. Further investigation into age-related differences in active coping mechanisms and the role of housing situation (e.g., long-term care facility, retirement community, independent living) during the pandemic (see Ayalon & Avidor, Reference Ayalon and Avidor2021) may also help further clarify differences in the salience of loneliness as a predictor of mental health across age groups.
Conclusion
This national survey study examined mental health impacts of the first 6 months of the COVID-19 pandemic and resultant public health restrictions on Canadians across the adult lifespan. This study had several strengths, including its large sample, recruitment across multiple platforms, and timely completion. Despite having a higher vulnerability to contract severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), older adults (ages 70 and over) demonstrated better mental health (i.e., less anxiety, depression, psychological trauma-related stress), lower impacts on substance use, and more social connectedness (i.e., loneliness, but not social support). Older Canadian adults are faring better during the COVID-19 pandemic, possibly due to their more developed active coping skills and less disparity between pre-pandemic and current size of their social spheres, relative to younger adults. Although loneliness emerged as a consistent and robust predictor of negative mental health across all age groups, it was a stronger predictor of mental health in younger age groups relative to the 55-64, 65-69, and 70-and-over age groups. Social support was also an important predictor among Canadians ages 25-34, 55-64, and 65-69, suggesting that addressing loneliness and quality of social connections should be key intervention targets during the COVID-19 pandemic across certain age groups. Moreover, social support was an important protective factor against poor mental health for adults ages 65-69, but only at average or high levels of loneliness, elucidating the differential protective pathways of social support on mental health across age groups. Future studies should further investigate mechanisms that may explain the differential impacts of the COVID-19 pandemic on mental health functioning across the lifespan, and further explore the relationships between levels of adaptive coping skills and resiliency, especially among more finely stratified older age cohorts. Longitudinal research will also be beneficial to illuminate mental health trajectories throughout the pandemic.
Acknowledgements
The authors would like to thank the rest of our research team for their assistance, including Reina Stewart, Brooke Lagore, and Jennifer Reeves. The authors would also like to thank Julie Prud’homme for her help with French language translations.
Supplementary Materials
To view supplementary material for this article, please visit http://dx.doi.org/10.1017/S0714980821000477.
Funding
This work was supported by the Canadian Institutes of Health Research (with partner funding from the Michael Smith Foundation for Health Research) and by the British Columbia Ministry of Health. MAG is funded by the Canadian Institutes of Health Research. NKL is funded by the Social Sciences and Humanities Research Council of Canada. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the Federal or Provincial Governments. None of the aforementioned funding agencies had any role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.










