Introduction
Multiple epidemics and pandemics during the 21st century have challenged health systems to effectively communicate health concerns to populations. Reference Swire-Thompson and Lazer1 In addition to the SARS-COV2 pandemic, outbreaks of preventable diseases continue worldwide, even though scientific evidence regarding efficacious containment, control strategies, and/ or treatments exist. Reference Larson2 Vaccine-preventable diseases continue to propagate in many countries regardless of resources, capacities, and available guidelines. Reference Dror, Eisenbach and Taiber3 Health communication is an essential part of healthcare provision and effective information delivery is critical for related agencies and health professionals to prevent the spread of diseases. In the era of rapidly disseminating information, it is crucial that scientists and healthcare providers can seamlessly communicate accurate health messages. Reference Swire-Thompson and Lazer1 At the individual level, communication is vital to establishing a trustful relationship between patients and providers. Reference Ferreira-Padilla, Ferrandez-Anton, Baleriola-Julvez, Bras and Dordevic4 Studies have shown that inadequate medical care communication is a leading cause of preventable death and is responsible for a significant amount of mortality. Reference Taran5 However, despite numerous communication and strategic evaluation methods, the accuracy or veracity of presented health information is increasingly being challenged in healthcare fields. Reference Ferreira-Padilla, Ferrandez-Anton, Baleriola-Julvez, Bras and Dordevic4 Information from health professionals is undermined by other sources despite established evidence for epidemic and pandemic control across resource-diverse countries. Reference Larson2
Health communication faces unprecedented challenges and the efficacy of previously utilized tools and methods has been decreasing in the current era. Reference Anwar, Malik and Raees6 Disinformation, misinformation, and the strategies by which these ideas propagate to the public threaten effective information delivery and its acceptance by the public. Reference Sylvia Chou, Gaysynsky and Cappella7 While misinformation is spread without intent, disinformation is part of a concentrated effort to spread false information, and both contribute to the concept of an infodemic, that needs be addressed. Reference Sentell, Vamos and Okan8 Communication strategies have been developed during the recent epidemics to overcome this phenomenon (vaccine campaigns, awareness and poster campaigns, and content labels), but an evaluation of these strategies is equally important to determine the most effective approaches in health communication. Reference Finset, Bosworth and Butow9 For the purposes of this paper, effective communication is defined as the dissemination of factual information that is readily accepted in a timely manner by the intended audience. Understanding the barriers to effective communication is crucial to controlling and mitigating current, and future, epidemics, and pandemics. Reference Henrich and Holmes10 This study aims to assess the gaps and barriers to effective health communication and evaluate the strategies to address them in both public health and medical care domains during epidemics and pandemics.
Methods
The communication methods and strategies included those that provided health information to the public or individuals through any communication venues including public (i.e., posters, billboards, radio, and television), social media, and individual encounters with health professionals inside or outside health facilities. It also included the global population who faced the threat or risk of any infectious diseases with the propensity to reach epidemic and pandemic levels. 2 overarching and complementary areas of health communication strategies, public health and healthcare delivery, were included for a better understanding of overall barriers to health communication at the group and individual levels.
Data sources and searches
A literature search was conducted in multiple databases including PubMed, SCOPUS, Cochrane Library, Google Scholar, and grey literature pertaining to study aims. This review included randomized, observational, case studies and case series, case reports, meta-analyses, and prior reviews published from January 2000 to December 2020. This time period included the advent of broadly used social networking and the internet as a primary method of communication. The interventions of interest were those that addressed health communication targeting the public or patients and individuals during epidemics or pandemics of infectious diseases. A list of search terms was developed in consultation with expert librarians and through initial literature reviews. An exhaustive search of relevant MeSH terms was developed in PubMed and subsequently translated to other databases for a complete list of potential search terms (Table 1). Keywords were broad to assure a comprehensive search. Complete search strategies and database codes are presented in Appendix A.
Table 1. Keywords for literature review on communication strategies during epidemics and pandemics

Study selection
The inclusion criteria included all primary data articles that (a) referenced health information communication during epidemics and pandemics, (b) described communication strategies to the public at the individual or group level, (c) included strategies within health systems, (d) described the outcomes, efficacy, and effectiveness of communication strategies in controlling epidemics and pandemics, and (e) included all clinical, public health, basic and social science studies published from 2000 - 2020. Exclusion criteria were non-human, non-English, behavioral concept studies, and panel of expert opinions.
Data extraction, quality assessment, data synthesis, and analysis
A 4-stage screening strategy was developed. First, selected databases were searched with keywords or MeSH terms in their titles or abstracts. Second, the titles and abstracts were reviewed, and the exclusion and inclusion criteria were applied by 2 independent reviewers. A tiebreaker resolved any conflicts prior to a full-text screening of the articles. Third, full article texts were reviewed to determine if they fully met the inclusion and exclusion criteria. Fourth, resultant articles were examined qualitatively and a data extraction tool was developed to assess characteristics of the study design including sample size, intervention, outcome measures, efficacy and effectiveness of strategies, barriers and challenges, and the overall internal validity and external validity. Appendices B and C present extensive information regarding components of the data extraction tool. They also contain details on the characteristics of resultant articles. A quality assessment was also conducted using the metrics outlined in the Cochrane Risk of Bias tool. Reference Higgins, Altman and Gøtzsche11 2 reviewers reviewed all articles for the bias assessment.
Institutional review board
This study did not include any human subjects and did not require an institutional review board approval.
Results
Figure 1 presents data from the screening phases. 55 articles were included for full-text assessment.
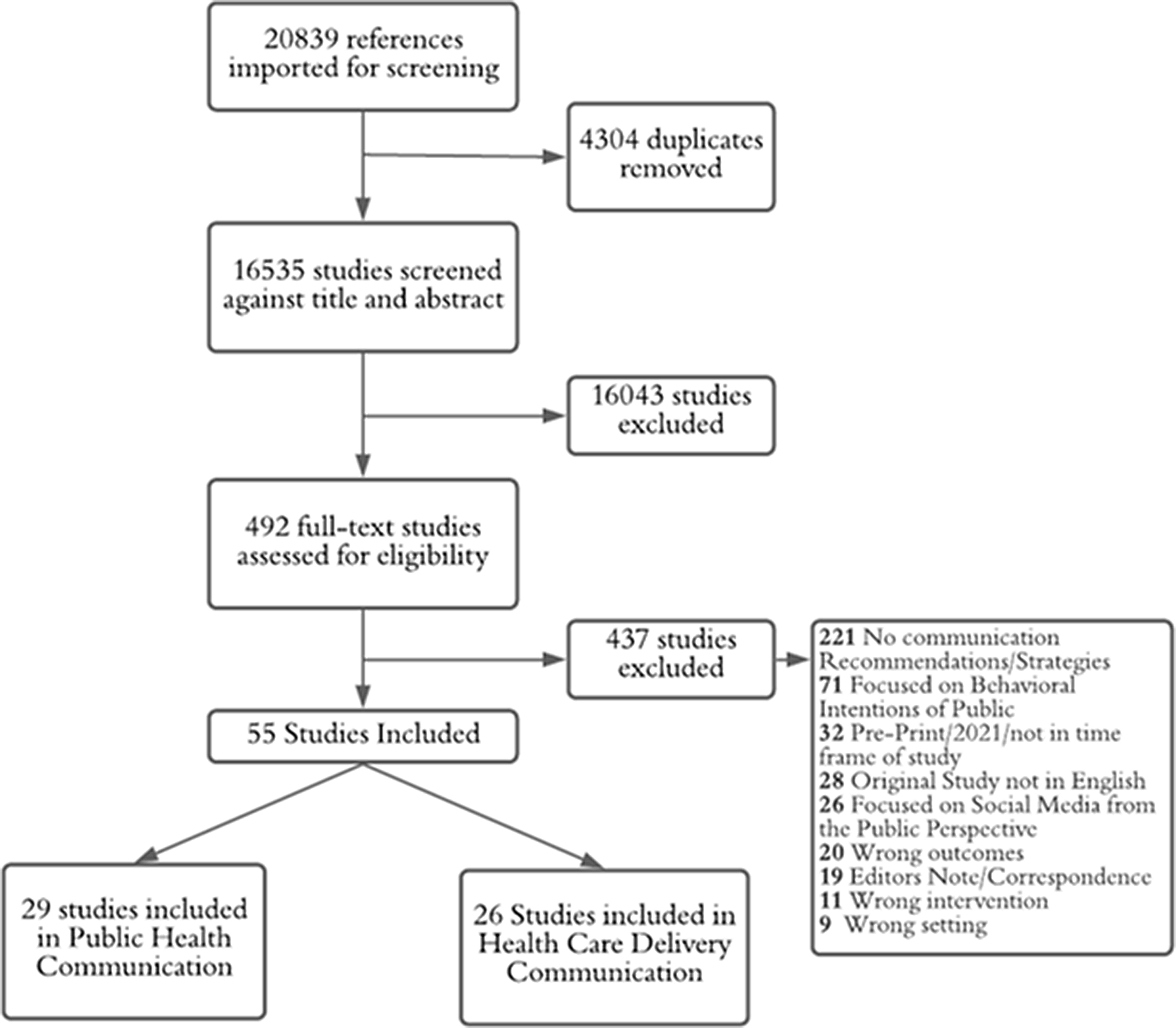
Figure 1. Screening process and data.
Studies included communication methods from 18 countries with 34.5% from the United States. There were 21 case reports, 10 qualitative randomized studies, 7 cross-sectional surveys, and 17 with other study designs.
Public health communication during epidemics and pandemics
Communication strategies and methods utilized by the public health system included articles from 12 countries or regions and referenced 7 epidemics. These were primarily qualitative analyses involving the evaluation of public communication methods from agencies and governments, which described specific communication tools to address vulnerable populations.
Most articles described key barriers to the timely and effective dissemination of information to the public during a dynamic process of communication, and noted that information can be easily distorted even if well intentioned. Political controversies and influences by governments were reported as barriers to dissemination and access to information. Misinformation and disinformation were the most frequently cited barriers. Inconsistencies in media approaches or messaging, unregulated social media, inadequate targeting of age groups, cultures, and languages, distrust to government agencies, inconsistencies in messages and their implementation, and perceived safety of vaccines or treatments were among broader barriers to effective communications. Notably, developed communication plans were not implemented as they were intended to mitigate pandemics. Table 2 presents further data on key gaps.
Table 2. Key gaps and recommendations in effective communication in public health sector during epidemics and pandemics Reference Anwar, Malik and Raees6,Reference Finset, Bosworth and Butow9,Reference King and Lazard12–Reference Vraga and Jacobsen35

Communication from public health agencies and governments
During epidemics, public health agencies are important sources of effective and clear information to the public. While most governments have frameworks for communication, there were important gaps and recommendations. Improving the use of targeted messaging, transparency, acknowledging and reasoning for changes in messaging during threats of novel pathogens, and consistency of health messaging especially early in the course of an epidemic, were recommended. Early and timely communication requires the preparation of planned materials ahead of time, which should include centralized messaging with localized risk communication strategies. Other recommendations included the incorporating perspectives from community stakeholders, 2-way communication channels, and the use of clear and simple language when designing communication materials for the public.
Role of the media in public health communication
Mass media of all forms is commonly used for health communication during epidemics and pandemics. A primary limitation of the media was a failure to disseminate information directly from public health officials to the public, and that media sources do not solely present unbiased information from credible members of the scientific community or emphasize trust in the scientific process even when applying a critical lens. Another important gap was the limited use of infographics that can be easily translated into other languages and cultural contexts. Content analyses, modeling, and controlled experiments were used to evaluate social media for the acceptance of presented information. Other gaps included unclear information sources, limited monitoring and evaluation regarding information accuracy and efficacy, and limited mitigation strategies against misinformation and disinformation.
Sociodemographic and sociocultural factors
During public health crises, including epidemics and pandemics, sociodemographic and socio-cultural inequalities are often more pronounced. Health communicators do not often address the presence and impact of socioeconomic and sociodemographic inequalities such as not targeting subgroups, and treating all minorities as a monolithic community. Additionally, health communicators often failed to provide contextually appropriate communication with the appropriate use of cultural identities, taboos, or differences to positively drive changes in healthy behaviors. Community stakeholders were often underutilized when attempting to introduce new concepts and information. Despite acknowledging the importance and impact of sociocultural factors, the implementation of related strategies by public health agencies and officials was often inadequate.
Healthcare delivery communication during epidemics and pandemics
Communication strategies and methods utilized by the medical care system included articles from 12 different countries and regions, and 2 pandemics. They covered social media messaging, national disasters and risk communication plans, and clinician first-hand accounts and surveys.
Major barriers were identified in how providers communicate with each other and their patients, and in how providers receive information from government and other health entities. Other major barriers to effective communication in the healthcare delivery sector included limited face-to-face contact with patients or audience during Covid-19, lack of collaboration in communication planning between health care entities, misinformation about the pandemic in media sources, and limited scientific knowledge of pathogens. General recommendations to address these barriers included collaborative approaches between stakeholders to plan effective communication during outbreaks. Methods of communication between clinicians, clinicians and patients, and clinicians and other stakeholders were analyzed including social media, national, state, and organizational communication frameworks, and digital response communication. A wide range of key gaps in communication in the healthcare delivery sector were identified and some recommendations were made to improve communication efforts and effective messaging (Table 3).
Table 3. Key gaps and recommendations in health communication in healthcare delivery sector during epidemics and pandemics Reference Zamberg, Manzano and Posfay-Barbe36–Reference Sharov57

Attitudes and perceptions of frontline providers
Frontline providers, including physicians, nurses, hospitalists, and other healthcare personnel, are major players in disease control and provide patients with information to address epidemics and pandemics, as well as related misinformation. For effective care, they require evidence-based information in a timely manner. Many clinicians reported feelings of lack of support from the media and institutions, inadequate collaborations with stakeholders and media, and doubts or lack of trust in governments and in national policies for risk communication during emergencies. Feeling overwhelmed with information overload and message volume from institutional and government messages about the pandemic was also a common theme.
Characteristics of social media messages
Social media played an important role in health messaging during H1N1 influenza and COVID-19 pandemics. From the perspective of medical professionals and the public, positive outcomes of social media messaging by clinicians included increased morale among healthcare workers, positive attitudes, and gaining trust of the public. Insufficient number of clinicians on social media to accurately inform the public was reported. Personal recommendations shared by clinicians on Twitter translated into a wider range of actions from the public, which government officials should take into consideration to improve public compliance and understanding of health messages during outbreaks. Clinicians, however, experienced stress and anxiety associated with the urgency of relaying accurate information before non-evidence-based narratives are posted. Mixed messaging between local, state, and global information sources was an important gap in effective health communication during both H1N1 and COVID-19 pandemics.
Prompt communication using electronic and digital sources
Continuous electronic communication involved instant messaging between providers to synthesize clinical learning and information dissemination in real-time. However, providers received a high influx of emails and information from multiple organizations and entities, which was perceived cumbersome and non-productive. Providers preferred single source of sending relevant information when contents or strategies were changed or new information emerged compared to multiple messages throughout the day. During the Covid-19 pandemic, in hospitals and emergency rooms, the use of electronic messaging was useful when face-to-face encounters were not possible or quick dissemination of information to staff was needed. With the influx of streaming information about COVID-19, hospital workers could quickly send electronic messages (phone apps, messaging apps, hospital servers) to colleagues on priority information. Clinicians suggested increased training on infodemic management for healthcare managers for prompt and effective digital communication.
Characteristics of information sources
While national and state policies provide clinicians with guidelines and communication tools for control of outbreaks, limited collaboration between clinicians in communication responses has been an important gap. Members of the public are more likely to get health recommendations and information from sources on social media platforms such as Twitter, YouTube, and Facebook, and they trust recommendations coming from clinicians on these platforms more when compared to government authorities or agencies. Therefore, clinical providers who communicate on social media platforms can expand their sphere of influence and reach a larger audience. Internal communication networks and platforms were also sources to access and share relevant information for providers. Hospital bulletins were also effectively utilized for printed forms of health communication.
Discussion
To improve the delivery of timely and accurate information and address current barriers in health communication during epidemics and pandemics, there are at least 3 broad areas to consider. These include devising of and investment in accurate, concise, and reliable public health communication frameworks; the improved and advanced use of media, and addressing misinformation by tailoring messaging to highlight facts that directly counter misinformation. Communication strategies need to be further updated to reflect nuances and requirements in the current digital era, and should be implemented more effectively during epidemics and pandemics. Reference Nazir, Hussain and Tian13 A renewed investment in timely communication methods on the part of public health agencies is warranted. Addressing mistrust toward the governments and healthcare industry requires a transparent and clear information exchange with the acknowledgment of limitations without resorting to fear tactics during epidemics or pandemics. Reference Han, Zikmund-Fisher and Duarte14 The status and needs of vulnerable populations should be evaluated and prioritized during epidemics and pandemics as soon as possible. Reference Vraga and Jacobsen35 Tested and evidence-based guidelines on health crisis communication should be implemented with a commitment to address public mistrust. Reference Reynolds and Quinn Crouse21,Reference Barrelet, Bourrier, Burton-Jeangros and Schindler22,Reference Gesser-Edelsburg, Mordini, James, Greco and Green25 During recent epidemics and pandemics, while broad aspects of the public health communication frameworks have been followed, political agendas and influences took precedence and diminished the impact of the intended health messages. Reference Kim and Kreps32 Interagency cooperation needs to be re-emphasized when developing and releasing prompt press statements to improve the implementation of evidence-based frameworks and guidelines, maintain consistent messaging, and ensure that all aspects of the communication plans are followed. Reference Barrelet, Bourrier, Burton-Jeangros and Schindler22,Reference Kim and Kreps32 Regional, and local governments should be regularly included in communication planning and strategizing approaches so that all stakeholders have shared goals and ownership of their implementation during epidemics and pandemics. Reference Barrelet, Bourrier, Burton-Jeangros and Schindler22
Public health communication could more effectively use clear and plain language when interacting with the public. Reference Barrelet, Bourrier, Burton-Jeangros and Schindler22 The use or overuse of technical language will increase the risk of misinterpretation and decrease the likelihood of positive changes in preventative behaviors. Reference Peinado, Treiman, Uhrig, Taylor and Stryker23 Public health agencies should constantly improve and update their approaches in utilizing both mass media and social media channels. While it is neither feasible nor advisable for governments and health agencies to exert complete control over what general media publishes, it is important to prioritize inputs and insights from independent scientists and experts as these direct health communicators could help improve the acceptance of the messages less affiliated with governmental instutitions. Reference Finset, Bosworth and Butow9,Reference Lee and Basnyat17,Reference Leask, Hooker and King18 The relationship between healthcare delivery and public health communicators, and for all types of media sources, is vital in the dissemination of accurate and effective information to the public. Health messages that are collaboratively framed will promote knowledge and improve efficacy while avoiding media sensationalism when the facts are daunting or unclear. Reference Bekalu, Bigman, McCloud, Lin and Viswanath16–Reference Leask, Hooker and King18,Reference Walker and Adukwu26 In times of information uncertainty, public health and healthcare organizations could emphasize and communicate simple evidence-based solutions that were successful in comparable situations or conditions and justify their application to the present situation while remaining truthful that more information on the specific condition may change the approach or recommendations as they become available. Moreover, promoting positive or preventative behaviors and community safety should be prioritized over fear-based approaches to engage the public. Reference Han, Zikmund-Fisher and Duarte14,Reference Peinado, Treiman, Uhrig, Taylor and Stryker23,Reference Walker and Adukwu26 By providing accurate and narrative-type stories to news agencies, public health and healthcare agencies may be able to provide support for positive communication and improve the delivery of accurate information through the media.
Public health agencies often do not tailor or adapt their messages to social media networking format, but instead replicate other materials produced elsewhere, Reference Sutton, Renshaw and Butts34 which will likely be less effective. Social media platforms can be effective tools. However, they require careful implementation in the right context, strategically utilized for the right audiences, and with information originating from the official public health or healthcare delivery sources. Reference Anwar, Malik and Raees6,Reference Nazir, Hussain and Tian13,Reference Walker and Adukwu26 As social media continues to be 1 of the most preferred public source of information, health messages should appeal to the related audience to improve uptake and effectiveness. Reference Sylvia Chou, Gaysynsky and Cappella7 The interactive nature of social media, as an accessible platform to promote 2-way dialogue with public health professionals, could be effectively utilized in health messaging. Reference Anwar, Malik and Raees6,Reference Henrich24 Merely posting repeated information without addressing questions or the gaps in knowledge will not be effective use of social media and is unlikely to translate into significant behavior changes. Reference Sutton, Renshaw and Butts34 Public health agencies may need to better invest in employing experts in social media utilization and adapt their communication frameworks for the high-speed nature of such platforms as the most powerful tools to directly target misinformation.
Misinformation has become a dangerous concurrent epidemic, and the scientific community, public health, and healthcare delivery agencies have so far struggled to manage this important challenge. Actors and stakeholders in the health communication field need to collaboratively develop strategic solutions to mitigate a continuum that includes the spread of passive misinformation to developed disinformation campaigns. Reference Gesser-Edelsburg, Diamant, Hijazi and Mesch58 The primary approaches should include transparency, addressing emotions, fears, and uncertainty, and providing clear information. Reference Finset, Bosworth and Butow9,Reference Han, Zikmund-Fisher and Duarte14,Reference Gesser-Edelsburg, Diamant, Hijazi and Mesch58 However, even with these strategies, public health has struggled to improve behaviors among those susceptible to misinformation. 1 of the most prominent examples is the problem of vaccine hesitancy. Vaccination is 1 of the oldest and best tools to mitigate infectious diseases and has decades of scientific research to promote its safety, feasibility, and accessibility. Reference Dror, Eisenbach and Taiber3 Nevertheless, large segments of the population are still wary of vaccines and their potential side effects, largely due to decades of counter-information messaging and campaigns. Reference Nowak, Sheedy, Bursey, Smith and Basket20 Due to the extent of anti-vaccination culture, strategies to increase vaccinations are an important area to test and improve health communication methods. Reference Nowak, Sheedy, Bursey, Smith and Basket20,Reference Henrich24,Reference Gesser-Edelsburg, Diamant, Hijazi and Mesch58 Many of the same principles discovered in the vaccine hesitancy domain could also be applied to the misinformation regarding epidemics and pandemics. Solely highlighting the specific inaccuracies that are believed by individuals can be counterproductive, but carefully developing targeted messages that provide the concrete facts presented within the frame of open communication could help minimize the effects of misinformation. Reference Gillespie, Obregon and El Asawi19,Reference Reynolds and Quinn Crouse21,Reference Henrich24,Reference Vraga and Jacobsen35,Reference Godinho, Yardley and Marcu59 Many of these population subgroups are inherently distrustful of governments and their communications, but the inclusion of trusted stakeholders, especially local healthcare providers and faith-based community leaders has been shown to improve credibility and increase the acceptance of the public health recommendations. Reference Gillespie, Obregon and El Asawi19,Reference Nowak, Sheedy, Bursey, Smith and Basket20
Once a channel of communication has been established, the focus should be on clear behavior risk-reduction messaging while refraining from blaming individuals for their beliefs. Reference Nowak, Sheedy, Bursey, Smith and Basket20,Reference Godinho, Yardley and Marcu59 Additionally, communication messages should emphasize the evidence of efficacy of recommended strategies in health messages from comparable epidemics or situations to improve acceptance and build further trust compared to misinformation sources. Potential psychosocial distress, as well as reasonable questions and concerns, should be addressed rather than dismissed as anti-vaccination sentiments. Reference Finset, Bosworth and Butow9,Reference Nowak, Sheedy, Bursey, Smith and Basket20,Reference Reynolds and Quinn Crouse21 Public health officials and healthcare providers must emphasize the safety and efficacy of vaccines and other preventative behaviors with evidence while concurrently addressing the fears among the target audience, all while evaluating and addressing the underlying factors. The vilification of individuals with inaccurate beliefs is often polarizing and may hinder their willingness to accept accurate information. By acknowledging the differences in baseline knowledge and communicating from a place of genuine desire to help and protect, there can be an increased uptake of protective and preventive behaviors. Reference Gillespie, Obregon and El Asawi19
Addressing specific barriers to effective health communication at healthcare delivery level would require multidisciplinary approaches to devise and tailor consistent communication frameworks based on population needs, which include collaborations among all sectors of governments, public health authorities, healthcare organizations, clinicians, and frontline providers. 2-way communication between health entities during health emergencies to develop data systems and communication strategies has been recommended by many researchers. Reference Glatman-Freedman, Bromberg and Ram38,Reference Bowden, Burnham and Keniston49,Reference van Dijk, Hooiveld and Jentink53,Reference Staes, Wuthrich and Gesteland56 When medical providers provide recommendations based on experience and data from actual encounters with patients, the government and health officials should take these insights and input into consideration in creating health communication frameworks and messages. Reference Wahbeh, Nasralah, Al-Ramahi and El-Gayar41 Studies have recommended using tiered systems for communicating management of disease epidemics including capacity building, containment, collaboration, and conscientious use of resources. Reference Bowden, Burnham and Keniston49 Health communication at healthcare delivery level cannot follow a 1-size-fits-all approach. The target population demographics and specific needs should be considered when creating health communication messaging and related frameworks. Tailoring of messages should be based on humility and taking into account the insight, perspectives, and knowledge of the target population. Reference Goldstein, Murray, Beard, Schnoes and Wang37
To improve direct and indirect patient care, health facilities should consider differences in types and methods of health communication and counseling when providing relevant information to frontline providers. Reference Klein, Cohen and Baseluos46 Medical providers can help tailor plans and information if they are provided with accurate, clear, timely information, and the needed support to deliver them. Reference Bagdasarian, Cross and Fisher39,Reference Locatelli, LaVela, Hogan, Kerr and Weaver47 The input, support, and ownership from researchers, journal or magazine editors, publishers, and mass media may be needed to have consistent messaging and avoid having the medical community be an inadvertent source of misinformation. Reference Bagdasarian, Cross and Fisher39 Unexpected needs or unforeseen situations will likely and frequently arise in healthcare settings during epidemics and pandemics, therefore a preparedness plan that involves a collaborative team approach can translate into better and more effective health communication that addresses uncertainties. Reference Bowden, Burnham and Keniston49 Medical staff should also be trained to tailor and better disseminate accurate and consistent messages among the medical community. Reference Tham, Lu and Teo50,Reference Janssen, Tardif, Landry and Warner55,Reference Scott and Van Scoy60 Additionally, in order to promote behavior changes during epidemics and pandemics, policies and infrastructure that support behaviors such as quarantining, isolating, and social distancing will also be needed in healthcare delivery settings. Communicating their importance is an important step but there also needs to be policies and structural support to promote their implementation and utilization.
Limitations
Most studies explicitly provided health communication recommendations developed for specific diseases such as COVID-19 and H1N1 pandemics, which may not represent other important epidemics or pandemics. A wide variety of and non-specificity of communication platforms makes it difficult to compare the efficiency across methods. There is minimal evidence-based data regarding physician-to-physician communication and current published data are likely compounded by selection bias. Additionally, a majority of the current available data is qualitative, depending on the sampling and perception, and interpretation, of the subjects. However, the broad nature of this review and resultant data from both public health and healthcare delivery sectors helped identify important contextual factors to address barriers and gaps in effective health communication strategies across outbreaks.
Conclusions
Pandemics and epidemics present unique barriers to accurate and effective information exchange with the individuals and the public at large. A lack of accurate information or research is not the primary barrier to proper health communication, but the failure of health agencies, scientists, and practitioners to convincingly convey the facts and accurate information. There are political mistrust and divisions, especially in regard to agencies with authorities that are prone to political influence. Communication frameworks should have input from all stakeholders including trusted members of the communities and frontline providers in all relevant domains. Public health and healthcare delivery sectors should be equipped with effective and available tools and have the needed support to present and convey proven evidence to prevent and address misinformation, disinformation, and important concerns from the public during epidemics and pandemics. The vilification of individuals with inaccurate beliefs is counter-productive and polarizing and will likely lead to more misinformation. Acknowledging differences in baseline knowledge, complemented by a genuine desire to protect, could improve acceptance of accurate messages.
Health messaging should be clear, timely, consistent, and adaptable to all information outlets and sources. Social media could be used with a greater intention and developed as a critical part of health communication frameworks to assure a wide-reaching audience. Involving clinicians and frontline providers who are in direct contact with individuals and communities, and have already built trustful relationships due to the nature of their work, is crucial when creating health communication strategies to bridge the information gap left by the distrust of larger organizations. Health communications need to be specific and tailored to fit the needs of at risk populations and the most vulnerable groups in times of a health emergency. Undoubtedly, urgency and ambiguity, as well as uncertainty during epidemics and pandemics, will significantly challenge the health sector with the difficult task of informing and protecting the public. However, to gain trust and acceptance, the health sector may have to provide a burden of proof far beyond that of the opposing side that produces and disseminates misinformation and disinformation.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/dmp.2023.61
Authors’ contribution
LB: conceptualization, data curation, formal analysis, and investigation, as well as project administration, resources, validation, and visualization. Also contributed in writing - original draft, writing – review, and editing; KG: conceptualization, data curation, formal analysis, and investigation, as well as project administration, resources, validation, and visualization. Also contributed in writing - original draft, writing – review, and editing; RA: conceptualization, data curation, formal analysis, and investigation, as well as methodology, project administration, resources, and supervision. Also contributed in validation, visualization, writing - original draft/ review, and editing.
Funding information
There is no funding resource to report for this study.
Competing interest
There is no conflict of interest to report for this study.






