Introduction
The pace of population ageing worldwide is increasing and by 2050 it is expected to reach 2 billion, up from 15 million in 2015 (World Health Organisation (WHO), 2017). By 2021 and beyond, the number of people 60 years and older will outnumber children younger than five years. With this demographic shift comes the challenges to ensure health and social systems can provide environments to support extra years of life by living independently and in relatively good health (WHO, 2017). The concept of healthy ageing supports the ‘ageing in place’ policy, where older people can continue to live at home or within their communities despite significant declines in capacity. This shift in focus centres new models of care firmly within primary health care principles and interdisciplinary community services that can promote dignity, autonomy, functioning and continued personal growth (AIHW, 2016; 2020).
Healthy ageing is defined by the WHO as ‘the process of developing and maintaining the functional ability that enables well-being in older age’ (WHO, 2017:12). Healthy ageing takes into account that even when chronic diseases do emerge, their consequences can be limited through high-quality and integrated primary health care to strengthen and maintain capacity or reverse decline (Smith et al., Reference Smith, Wallace, O’Dowd and Fortin2016; Kluge et al., Reference Kluge, Kelley, Theodorikas, Barkley and Valderas2018). In countries with more developed primary health care systems, strategies have been initiated to promote multi-sectoral action supporting integrated frameworks to achieve person-centred, long-term care in community settings (Metzelthin et al., Reference Metzelthin, Rostgaard, Parsons and Burton2020). Similarly in Australia, state and commonwealth funded integrated care services are developing that cross the boundaries between primary, community, acute health, and social care settings to support screening and assessment pathways for conditions such as dementia (Alzheimer’s Australia, 2015). However, to date, similar evidence-informed models of practice that include staff training and interdisciplinary client assessment pathways to support capacity and overall wellness in the community for older people continue to be sparse (Australian Association of Gerontology, 2020).
One response to the need for a more inclusive framework is the concept of reablement, which has emerged during the last two decades both within Australia and globally, and has recently been defined through a Delphi study comprising of reablement experts from 11 countries (Metzelthin et al., Reference Metzelthin, Rostgaard, Parsons and Burton2020:11). There has been some debate internationally about the differences between reablement, rehabilitation, and restorative programmes based on definitions by the World Health Organisation (WHO) and the Department of Health in the UK (Legg et al., Reference Legg, Gladman, Drummond and Davidson2016). The current consensus definition below addresses this debate by clearly describing reablement as a programme focused on home-based rather than institutionalised or hospital care.
The key concepts as captured by the current consensus definition of reablement are as follows:
Reablement is a person-centred, holistic approach that aims to enhance an individual’s physical and/ or other functioning …. Reablement … is delivered by a trained and coordinated interdisciplinary team. Reablement supports an individual to achieve their goals, if applicable, through participation in daily activities, home modifications and assistive devices as well as involvement of their social network. Reablement is an inclusive approach irrespective of age, capacity, diagnosis or setting. (Metzelthin et al., Reference Metzelthin, Rostgaard, Parsons and Burton2020:11)
The concept of reablement was first adopted in Australia in the early 2000s in the state of Western Australia. Since this time, the practice of ‘wellness and reablement’ as it is termed in Australia, has grown nationwide but is still a relatively new model for providing services in primary health care settings, with very little evidence of workforce development (Australian Association of Gerontology, 2020). Systematic reviews to date, mainly from the United Kingdom and Scandinavian countries, have focussed on the outcomes of using reablement in community and other social care environments, with limited focus on staff training, such as for support workers, assistant workers, and allied health professionals (Moran et al., Reference Moran, Nancarrow and Enderby2015). Some studies have identified that future research should focus on evaluating the implementation of agreed reablement components to inform practice, education, and policy (Laragy and Allen, Reference Laragy and Allen2015; WA Home and Community Services, 2019).
Reablement interventions and activities are designed collaboratively with clients to focus generally on activities of daily living with the aim of allowing people to ‘age in place’ in their own residence and participate socially as they wish. Programmes are delivered predominantly by community service providers who focus on personalised health and support to enable people to continue living in their homes safely and independently.
There is some evidence that embedding reablement as an organisational framework, or model of care in practice, can be problematic as opportunities for staff education and training are not yet well established in Australia (Maxwell et al., Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021). One innovative training programme adopted recently by a community service provider demonstrated the importance staff placed on client-centred care and working in partnership with clients to achieve goals following the training (Maxwell et al., Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021). Reablement principles were applied and embedded in the creation and development of the learning and teaching materials, the teaching programme as well as the evaluation of the impact of reablement across the organisation (Maxwell et al., Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021). However, the outcomes from this and other programmes have been limited in developing robust models of training and client assessment that could be embedded in practice across disciplines in primary health care.
Research aim
The aims of this scoping review are
-
1. To explore the evidence by which a reablement framework has been integrated by community service providers into existing models of training and client assessment; and
-
2. To explore the methods for evaluation of reablement training programmes in practice.
Methods
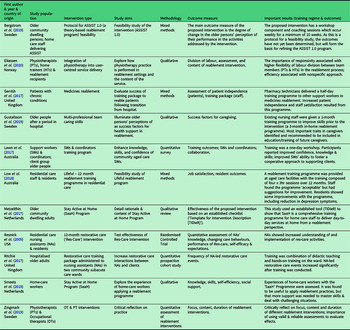
This scoping review was designed with the intention of exploring to what extent there is evidence that a reablement framework has been integrated by service providers into existing models of training and assessment. To achieve this aim, a literature review method was adopted, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) approach (Moher et al., Reference Moher, Liberati, Tetzlaff and Altman2009; Peters et al., Reference Peters, Godfrey, Khalil, McInerney, Parker and Soares2015; Tricco et al., Reference Tricco, Lillie, Zarin, O’Brien, Colquhoun and Levac2018), (see Table 1). For the purposes of the scoping review, papers including training programmes were limited to those that by definition focused on reablement and to client assessment that focused on positive outcomes. In accordance with PRISMA-ScR stages 12 and 13, individual papers were then critically assessed using these definitions of training and client assessment, then synthesised and summarised (see Table 2).
Table 1. Search concepts and key search terms
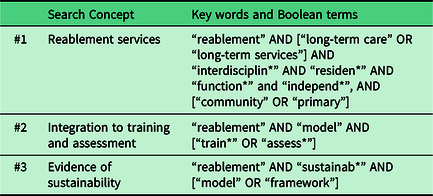
Table 2. Characteristics and findings of included studies of reablement training and client assessment
In a scoping review, it is important to establish inclusion criteria to determine which studies are eligible for inclusion in the review (Peters et al., Reference Peters, Godfrey, Khalil, McInerney, Parker and Soares2015). In this case, the context of included studies was those related to community care, primary care, long-term care, and residential care. The populations of interest included service providers, interdisciplinary staff, trainers, patients/clients, and assessors. Studies were restricted to English language with a date range of 2009–2020. Peer-reviewed literature, as well as grey literature and dissertations, was eligible for inclusion in the study.
Search strategy
The search strategy (Figure 1) used a combination of terms based on three concepts using electronic databases JBI, Scopus, CINAHL, PsycInfo, Web of Science, Medline & Embase via OVID, Psychology & Behavioural Sciences collection, and Google Scholar. A Boolean search was conducted using key terms developed from the search concepts (Table 1).
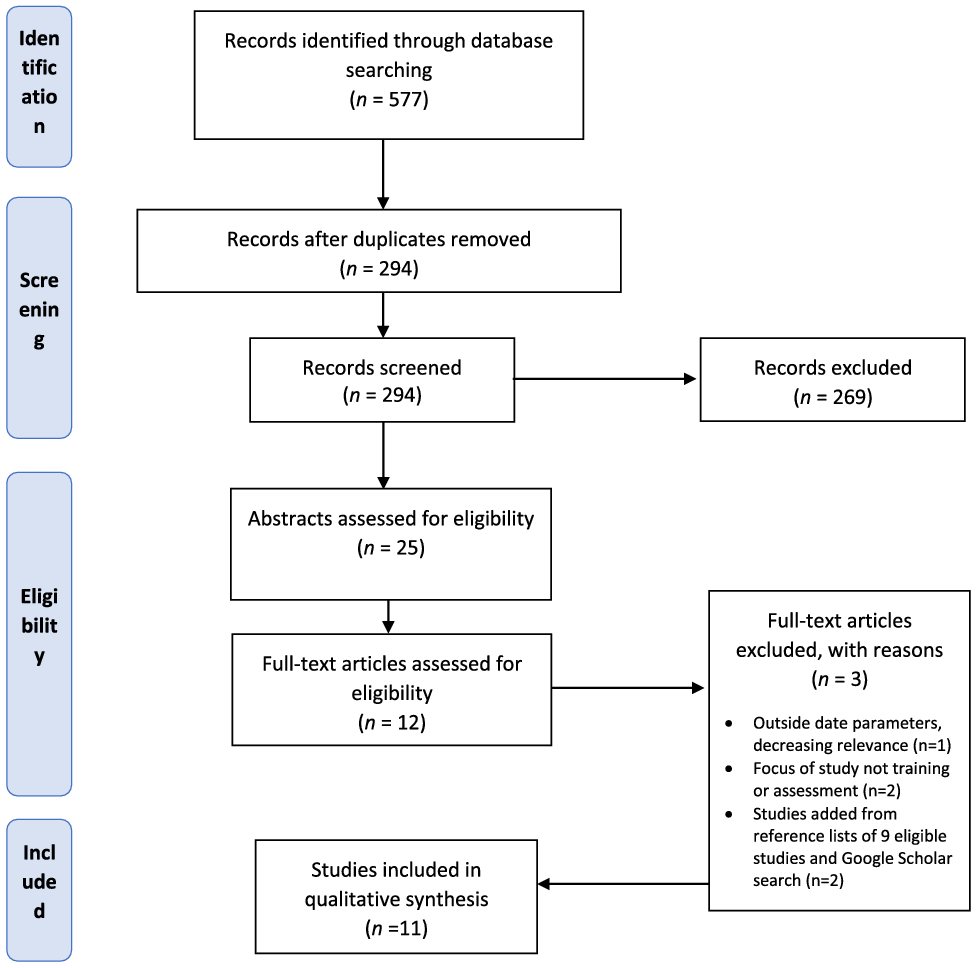
Figure 1. PRISMA flow diagram for the scoping review process
From the seven databases, 577 results were retrieved and exported to EndNote®. After automatic and manual removal of duplicates, 294 records remained. The titles and abstracts of these records were assessed against the inclusion criteria listed above. Of the 294 records assessed, 25 were retained for abstract review. An online software platform, Covidence®, was used to facilitate this review process. All abstracts and metadata were imported into Covidence® to facilitate the implementation of the PRISMA-ScR screening approach (see Figure 1). Of the 12 articles remaining after abstract screening, three were excluded after full-text review. Two further studies were added after reviewing the reference lists of the nine eligible articles and conducting a Google Scholar search for completeness, for a total of 11 articles included in this review. A single author (SY) screening process was used for the title/abstract screening, and three authors (SY, SP, MB) participated in the full-text review process. The validity of the papers included in the full-text review was assessed against the eligibility criteria:
-
i. The paper relating to reablement in the context of community service provision; and
-
ii. The paper making specific reference to reablement as a component of training or assessment.
If there was an affirmative answer to both questions, the paper was retained. One article (Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017) was retained despite its hospital setting because of the potential the hospital-based reablement interventions described could impact patient engagement with reablement care post-discharge in the community. Consequently, the utility of the insights provided by the study in terms of future reablement programme design was deemed valuable. Papers were assessed for quality as part of the review process. All nine included papers were appraised to ensure methodological rigor during the full-text review stage (by three authors – SY, SP, MB).
Data extraction and charting
For each article, the author, year, study population, country of origin, intervention type, study aims, methodology, outcome measure(s), and important results were abstracted from the article, as per guidance for scoping review procedures (Arksey & O’Malley, Reference Arksey and O’Malley2005; Peters et al., Reference Peters, Godfrey, Khalil, McInerney, Parker and Soares2015). A summary of these findings is shown in Table 2. The findings will be discussed in narrative format in combination with discussion of these results in the following sections.
Results
Three qualitative papers, four quantitative, and four mixed-method studies were identified (Table 2). Eight of the 11Footnote 1 studies included in this review provided discussion of staff training regimes for reablement care in a community setting, with the exception of one study that was conducted in a hospital setting (Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017). Four of the reablement training programmes comprised an educational, theoretical component in combination with a more hands-on or practical component (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018; Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019). Four other studies included an educational component with a role-play or simulation element added (Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Lawn et al. Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019). A ‘student-centred’ approach with consideration of adult learning styles, inclusion of interactive components and open discussion with reduced focus on ‘lecturing’, was described in two of the training programmes (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017). Case studies were used as teaching tools in two studies, and these same two studies provided course manuals for their enrollees (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017).
Study population
In terms of staff reablement training programme delivery, a variety of different disciplines delivered the training across the eight studies, including an occupational therapist (Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019), members of the research team conducting the study (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018), nurses with varying levels of education and capability (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009), physiotherapists (Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017), or a combination of nurses and research team members (Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019). In all cases, the programmes were being delivered to staff responsible for client care including rehabilitation assistants and support workers (Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017); community support workers and their supervisors (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017); nursing assistants (Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017); home care staff (Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018; Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019); nurses and domestic support workers (Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019); and nurses, nursing assistants, and other interested care staff (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009).
Theoretical frameworks
With regard to the design of the reablement training programmes, many of the programmes described an explicit theoretical underpinning, such as Bandura’s theory of self-efficacy and behaviour change (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019), or a combination of Bandura’s social learning theory and Kotter’s eight-step model for change (Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018). The role of behaviour change and motivation in reablement care, without specific reference to Bandura’s theories, was also referred to by one programme (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017). Most programmes also mentioned adopting a person-centred approach to care (Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018; Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019), or the importance of person-centred care (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017).
In reference to the detailed content of the reablement training programmes, the more educational and theoretical elements of the programmes had a variety of foci. Common topics for teaching included: an introduction to or setting the context for reablement and reablement theory (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018; Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019); strategies for practical care activities or interventions (e.g., exercise, bathing, transfers, and medication administration) (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018); encouraging and motivating older adults (Resnick et al. Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019); and incorporating reablement activities into existing care regimes (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009).
Practical components
The practical components included in three of the training programmes (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017; Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019) were quite varied. In the Bergstrom et al. (Reference Bergstrom, Borell, Meijer and Guidetti2019) study, the practical elements were focused on the priorities of the older person involved in the study. The occupational therapist (OT) providing the training worked together with the staff and older person to facilitate reablement for a particular task identified by the client as important to them (e.g., independent grocery shopping), and reablement for this task, including site visits if needed, became the focus (Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019). In the Resnick et al. (Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009) study, the practical component was focused on the work of a ‘champion’ for the reablement programme, a role filled by a ‘Res-Care’ Nurse Coordinator (RCN) from the research team. The RCN helped the staff engage with the residents in reablement-focused activities and provided on-going practical learning opportunities for the staff participating in the training programme (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009). Lastly, in the Ritchie et al. (Reference Ritchie, Wood, Martin and Jones2017) study, the physiotherapist worked with each staff member in the training programme in ward-based practice sessions to reinforce reablement principles and to help identify reablement opportunities.
Four studies (Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Lawn et al. Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Metzelthin et al., Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019) included ‘role play’ or ‘simulation’ activities as a form of practical component in their training programmes. In the Gerrish et al. (Reference Gerrish, Laker, Wright and Stainrod2017) study, the competencies of the staff being trained in medicines reablement were assessed by the physiotherapists training them through simulation and role-play activities. In the Lawn et al. (Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017) study, video clips were used to demonstrate skills in reablement practice, after which role-play was used to put these ideas into action. In the ‘Stay Active at Home’ program described by both Metzelthin et al. (Reference Metzelthin, Ziljstra, van Rossum, de Man-van Ginkel, Resnick, Lewin, Parsons and Kempen2017) and Smeets et al. (Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019), practical assignments/tasks were given between didactic training sessions to simulate the application of skills in practice.
Staff training evaluation
In the studies where reablement training programmes were administered as part of the research, in some cases evaluation of the training programmes was conducted (Table 1). In four cases (Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019), this training programme evaluation was explicitly undertaken and reported, and in two other cases the evaluation was implicit in the reporting of the findings (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017).
In the Lawn et al. (Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017) study, 102 of the 140 trainees completed the programme evaluation survey, and the ‘majority’ (56.4%–76.6%) agreed that the training programme had improved their ‘confidence, knowledge, and skills’, and they better understood the principles of how to support clients in reablement-orientated behaviour change (p. 461). In the Low et al. (Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018) study, 104 staff members provided an evaluation of the training programme. The majority (99.3%) of staff found the training material easy to understand, that it improved their understanding of the concepts presented, and ‘helped them build better relationships with residents’ (p. 5). In the Ritchie et al. (Reference Ritchie, Wood, Martin and Jones2017) study, evaluation of the reablement training programme was undertaken using observational measurements of the frequency of reablement care events pre- and post-intervention. A statistically significant proportional increase (74% to 92%) in these events was documented over the course of the study (Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017). Smeets et al. (Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019) found the trainees in their study perceived the ‘Stay Active at Home’ reablement training programme as useful for the application of reablement, and found the programme helpful in reminding them to apply reablement principles in their care practice.
While the Resnick et al. (Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009) study did not explicitly conduct an evaluation of their reablement training programme, the outcome measures could be considered an evaluation in terms of programme effectiveness. The nursing assistants (NAs) who completed the programme described having increased knowledge of and beliefs about the benefits of reablement care after 12 months in the programme than the NAs in the control group (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009). However, it was noted that the frequency of reablement care events did not increase over the 12 months. In the Gerrish et al. (Reference Gerrish, Laker, Wright and Stainrod2017) study, the trainees found the reablement training ‘informative’ and ‘highly relevant’, and that they had gained the skills necessary to support patients in medicines reablement (p. 308).
While the reablement training was evaluated as the only outcome measure in four studies (Resnick et al., Reference Resnick, Gruber-Baldini, Galik, Pretzer-Aboff, Russ, Hebel and Zimmerman2009; Lawn et al., Reference Lawn, Westwood, Jordans, Zabeen and O’Connor2017; Ritchie et al., Reference Ritchie, Wood, Martin and Jones2017; Smeets et al., Reference Smeets, Kempen, Zijlstra, van Rossum, de Man-van Ginkel, Hanssen and Metzelthin2019), in two studies (Gerrish et al., Reference Gerrish, Laker, Wright and Stainrod2017; Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018), the outcome measures included both the reablement training evaluation and a measure of the reablement outcomes, for example assessment of clients. One study (Bergstrom et al., Reference Bergstrom, Borell, Meijer and Guidetti2019) included client capabilities as the only outcome measure.
Client assessment
The reablement programme evaluation outcomes were presented in the preceding section. The assessment of client capabilities, while not directly measured in all studies, are important outcome measures to be considered in reablement training or evaluation. In terms of assessing the efficacy of reablement programmes, and therefore informing the design of future programmes, client assessment outcomes will be presented in this capacity. In the Gerrish et al. (Reference Gerrish, Laker, Wright and Stainrod2017) study, all eight client participants were able to achieve successful medicines reablement by the end of their participation in the programme. In the Low et al. (Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018) study, staff members who conducted the reablement programme noticed ‘positive changes in the units they worked in’, and described clients as more ‘settled’. 8). The data collected directly from the clients showed promising improvements in the clients’ mental health symptoms, functionality, and social-care related quality of life (Low et al., Reference Low, Venkatesh, Clemson, Merom, Casey and Brodaty2018). The Bergstrom et al. (Reference Bergstrom, Borell, Meijer and Guidetti2019) study based its outcome measures primarily on the Swedish version of the Canadian Occupational Performance Measure (COPM). The COPM measures the ‘self-assessed performance and satisfaction of valued activities in everyday life within the areas of self-care, productivity, and leisure’ (p. 6). Because this study was a feasibility study, no actual outcome measures were reported.
Studies with no programme/assessment focus but useful to inform future reablement training programme development
Three of the studies included in this review (Gustafsson et al., Reference Gustafsson, Ostlund, Zander, Elfstrom and Anbacken2019; Zingmark et al., Reference Zingmark, Evertsson and Haak2019; Eliassen et al., Reference Eliassen, Henriksen and Moe2020) are not focused on reablement training programmes or the evaluation of these programmes, but present information that could be useful to inform future reablement training programme design and development. The study by Eliassen et al. (Reference Eliassen, Henriksen and Moe2020) focused on how physiotherapy is performed in reablement settings and the content and delivery mode of this service. This study showed that reablement teams with flexible roles and division of labour were able to better meet the needs of clients than teams where roles were distinct and predefined (Eliassen et al., Reference Eliassen, Henriksen and Moe2020). Gustafsson et al.’s (Reference Gustafsson, Ostlund, Zander, Elfstrom and Anbacken2019) study examined older adults’ perceptions of the components of successful short-term reablement care. The older adults found that a motivating caregiver who created a positive atmosphere, and who treated them with dignity and went ‘beyond the expected’ in terms of care delivered (Gustafsson et al., Reference Gustafsson, Ostlund, Zander, Elfstrom and Anbacken2019:501) were the most important elements of successful reablement care. Zingmark et al.’s (Reference Zingmark, Evertsson and Haak2019) study documented the reablement practices of occupational (OT) and physical therapists (PTs) and found both key differences (e.g., duration of interventions) and important similarities (e.g., focus on mobility) in the way reablement activities are administered by these two sets of professionals. These findings illustrated the importance of critical reflection on the design of reablement intervention components and how OTs and PTs can best work together to promote a successful and positive reablement experience for clients (Zingmark et al., Reference Zingmark, Evertsson and Haak2019).
Discussion
This scoping review has demonstrated variation in the population, intervention type, theoretical framework, and outcome measures of included studies. These studies represent the range of settings where community service and health care organisations can deliver reablement programmes. Each training programme included in this review is initiated by an allied health professional or nurse and tailored to frontline staff with the aim for them to: better understood and apply the principles of reablement; support clients in reablement-orientated behaviour change (Stay Active at Home, ASSIST); build better relationships with clients; and increase knowledge and skills in reablement practices. Frameworks such as the ASSIST (OT) program assess changes in self-efficacy, perceived health, and well-being of the clients. The COPM is more focused on measures of self-assessed staff performance and client satisfaction with valued activities. Nursing frameworks include assessment of clients’ mental health symptoms, functionality, and social-care related quality of life. Qualitative measures of assessment focused on how staff can promote a positive and successful experience for clients. Consistent with the consensus definition of reablement (Metzelthin et al., Reference Metzelthin, Rostgaard, Parsons and Burton2020), these measures have been shown to contribute to improving and/or maintaining independence in individuals in a community setting through direct and collective assessments and interventions.
As a complex intervention, reablement has at its core a commitment to a person-centred, holistic approach with clients and the requirement for trained, interdisciplinary staff who are capable of conducting initial and ongoing assessment of clients. The studies in this review support this approach and highlight the importance of individual client assessment to support positive outcomes. The training programmes focused on reablement in this review also mostly draw from the model of person-centred care in different contexts, which inherently relies on individual client input and a collaborative approach to developing and assessment of activities included in individual plans. Theoretical underpinnings most commonly applied in the studies to the establishment of reablement principles were Bandura’s social learning theory of self-efficacy and behaviour change and Kotter’s eight-step model for change to facilitate a culture of assessment (Gorran Farkas, Reference Gorran Farkas2013; Montcalm, Reference Montcalm1999).
In the studies reviewed, the application of these theories to practice provides the catalyst for ensuring the right environmental and cognitive factors are recognised as being important for human learning and behaviour and to bring about lasting change. As such they are pragmatic and philosophically aligned with reablement. Further exploration of these two approaches would have merit and advantage particularly where the researchers and training team work with the organisation to develop appropriately targeted learning and teaching resources, reflecting suitable reablement practices of working with clients to achieve goals (Maxwell et al., Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021).
Maxwell and colleagues (Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021) found that post implementation of reablement practices there was evidence of improved motivation of staff which appeared to enhance morale and confidence. Important advantages of adopting a reablement ethos were also observed in other international studies (Rostgaard, Reference Rostgaard2018). Research from Denmark shows that staff working intensively with reablement experience a number of benefits (Rostgaard, Reference Rostgaard2018). Evidence indicates the importance of the relationship between care coordinators within organisations and direct care workers and that into the future this could be improved and developed to further enhance and deliver client care and reablement education within organisations (Maxwell et al., Reference Maxwell, Bramble, Prior, Heath, Reeves, Marlow, Campbell and Doherty2021). Improvements from the staff perspective included opportunities for regular meetings, seeking advice and discussing workforce-related and client-related issues. This is consistent with previous research (Rabiee & Glendinning Reference Rabiee and Glendinning2011) that illustrates the features, content, and delivery of reablement services (such as a limited potential for staff to be independent, a lack of continuity of support and time pressures) may detract from its effectiveness in an organisation.
Furthermore, it has been suggested that the use of a pre-employment questionnaire to determine how commencing or potential employees might interact with clients and their families physically and emotionally may provide further evidence of supporting reablement in practice (Prior et al., Reference Prior, Heath, Reeves, Campbell, Maxwell, Bramble and Doherty2020). A workforce aligned with the values of reablement in a community-based support field would promote the national aim of allowing people to age in place, improving client-centred care overall and will contribute to lessening the burden on residential aged care facilities (Prior et al., Reference Prior, Heath, Reeves, Campbell, Maxwell, Bramble and Doherty2020).
Limitations
The limitations in this study mainly relate to scope. Due to its exploratory nature, the study and the authors’ main interest were to establish the evidence associated with reablement practices in community settings. Other relevant studies conducted in hospital or rehabilitation settings therefor may have been excluded. There may have been a limitation from excluding studies before 2009; however, this is unlikely given that the framework of reablement has been introduced after that time.
Conclusions
This review has identified that currently reablement programmes are not yet embedded as a framework for standard practice by community service providers in primary health care settings. Different programmes of training and client assessment are being designed based on single disciplinary approaches and the context in which they are delivered. Further developmental work is required to integrate the components of individual training programmes within interdisciplinary frameworks. This will achieve not only an integrated framework for delivery across settings but also develop an interdisciplinary workforce aligned with the values of reablement, promote ageing in place and ultimately lessen the burden on residential aged care facilities.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1463423621000918
Funding information
Family Based Care Association North West Inc.