The prevalence of obesity has dramatically increased in recent years, becoming a major public health concern(Reference Gortmaker, Swinburn and Levy1). The number of obese people has more than doubled since 1980 in most countries, and among behavioural, environmental, occupational and metabolic risk factors, obesity has become one of the largest risks for mortality(2,Reference Stanaway, Afshin and Gakidou3) . The aetiology of obesity is multifaceted and encompasses a broad range of genetic and environmental factors(Reference Qasim, Turcotte and De4). Among environmental factors, the influence of dietary habits on obesity has received much interest over the last few decades(Reference Gómez-Donoso, Martínez-González and Martínez5). Interestingly, although the influence of organic food consumption on several aspects of human health has been assessed, its influence on obesity has been little studied(Reference Hurtado-Barroso, Tresserra-Rimbau and Vallverdú-Queralt6). Here, we present the results of the first study to assess whether the consumption of organic food is related to obesity throughout life.
A generalised definition of organic agriculture proposed by the Codex Alimentarius stated that ‘organic agriculture is a holistic production management system which promotes and enhances agro-ecosystem health, including biodiversity, biological cycles, and soil biological activity. It emphasises the use of management practices in preference to the use of off-farm inputs, taking into account that regional conditions require locally adapted systems. This is accomplished by using, where possible, agronomic, biological, and mechanical methods, as opposed to using synthetic materials, to fulfil any specific function within the system’(7). Several plausible mechanisms have been proposed to explain how organic food may affect obesity. For example, organic foods are known to have lower concentrations of pesticide residues(Reference Smith-Spangler, Brandeau and Hunter8,Reference Baranski, Srednicka-Tober and Volakakis9) . Of note, pesticide consumption has been associated with obesity in humans(Reference Thayer, Heindel and Bucher10–Reference Twum and Wei13). Moreover, several studies have shown that organic meat and dairy products have a higher concentration of PUFA than the corresponding non-organic products (in particular n-3 fatty acids)(Reference Średnicka-Tober, Barański and Seal14,Reference Średnicka-Tober, Barański and Seal15) and that organic plant-based foods have higher levels of antioxidants (in particular phenolic compounds)(Reference Baranski, Srednicka-Tober and Volakakis9). These variations in nutrient intake in an organic-rich diet could be beneficial for reducing obesity risk(Reference Simopoulos16–Reference Abdali, Samson and Grover18).
Only two experimental studies have assessed the relationship between organic food consumption and BMI. In the first study, all participants followed a conventional Mediterranean diet (MD) for 15 d and then an organic MD for 15 d in a trial conducted among both healthy participants and patients with chronic kidney disease. This study revealed a decrease in BMI during the organic MD phase solely for the patient group(Reference De Lorenzo, Noce and Bigioni19). However, the design employed precludes causal conclusions on the role of organic food consumption on BMI. In the second study, a cluster randomised controlled trial conducted among children incidentally showed that an organic food diet could reduce BMI v. a conventional diet(Reference Makris, Konstantinou and Andrianou20). However, because the primary aim of this trial was to observe the consequences of organic food consumption on pesticide exposure, the authors did not control for nutrient and energy intake between the groups. Participants in the organic food group had lower energy intake and higher vegetable and fruit consumption than the conventional group, making it impossible to infer any causality between organic food consumption and a lower BMI.
In addition to these trials, four epidemiological studies reported that consumers of organic food have a lower BMI or a lower obesity rate than non-consumers(Reference Eisinger-Watzl, Wittig and Heuer21–Reference Torjusen, Brantsæter and Haugen24). However, these epidemiological studies had several limitations. Only two controlled for potential confounding factors when assessing the relationship between organic food and BMI. Of note, the two studies that controlled for potential confounding factors were conducted among convenient non-representative samples (e.g. 78 and 100 % of the two samples were women) and measured BMI using self-reported weight and height(Reference Kesse-Guyot, Baudry and Assmann22,Reference Torjusen, Brantsæter and Haugen24) (in one study, the results were replicated when objectively measuring BMI in a subsample)(Reference Baudry, Lelong and Adriouch25). Last, all four epidemiological studies were restricted to an adult population.
Additional observational evidence is required before setting up well-designed clinical trials to investigate whether the consumption of organic food could be used to prevent obesity. The present cross-sectional study aimed to investigate whether the consumption of organic food is related to obesity in childhood and adulthood. Due to the observational design, we assessed this relationship while considering numerous potential confounding variables. In particular, previous studies have highlighted that organic food consumers tend to have a higher socio-economic status, a better-quality diet (e.g. higher consumption of fruits and vegetables or a greater adherence to national dietary guidelines) and a higher level of physical activity(Reference Kesse-Guyot, Baudry and Assmann22,Reference Torjusen, Brantsæter and Haugen24) . As these three factors are known to be strongly related to obesity, we controlled for their potential confounding effect.
Methods
Study
The Third French Individual and National Food Consumption (INCA3) Survey 2014–2015 was a cross-sectional study carried out between February 2014 and September 2015 among a representative sample of individuals living in mainland France. The objectives, design and methodology have been described before(Reference Dubuisson, Dufour and Carrillo26). This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving human subjects/patients were approved by the (CCTIRS, no. 13.055). Verbal informed consent was obtained from all participants. Verbal consent was witnessed and formally recorded.
Participants
A representative French sample of 5855 individuals, selected according to three-stage stratified cluster sampling, participated in the study(27) (2698 0- to 17-year-old children and 3157 18- to 79-year-old adults; see details in online Supplementary Text S1). Among them, 1993 children (74 % of the initial sample) and 2121 adults (67 % of the initial sample) completed both a food propensity questionnaire and a 24-h dietary recall or records (24HR). Sampling weights were specifically generated for these two subsamples to maintain their representativeness. Finally, 218 children were excluded because they were 3 years old or younger (all statistical analyses performed in the children group accounted for this exclusion, as detailed in the Statistical analysis section).
The final working samples thus included 1775 4- to 17-year-old children and 2121 18- to 79-year-old adults. Among them, values of at least one of the thirteen variables included in the regression models were missing for 317 children and 442 adults. Therefore, analyses based on multiple imputation included 1775 children and 2121 adults, whereas the analyses based upon complete cases included 1458 children and 1679 adults.
Materials and procedure
Participants underwent anthropometric measurements and completed several questionnaires concerning demographic information, lifestyle and dietary habits – including a food propensity questionnaire and at least two 24HR (see full description in online Supplementary Text S2). For participants under 10 years of age, a legal representative completed the questionnaires in the presence of their child. For participants between 11 and 17 years of age, participants completed the questionnaires themselves but were assisted by their representative. Participants older than 18 years of age completed the questionnaires on their own.
Organic food consumption
Participants were asked to report their frequency of consumption of organic food by food groups during the last 12 months (‘always’, ‘often’, ‘rarely’, ‘never’, ‘did not eat’ or ‘do not know’). Organic consumption of twelve food groups was investigated (milk and dairy products, eggs, poultry, other meats, fish, fruits, vegetables, legumes, potatoes, bread and/or wheat, other cereals and any other product). For each food group, consumption was scored ‘always’ = 3 points, ‘often’ = 2 points, ‘rarely’ = 1 point, ‘never’, ‘did not eat’ = 0 point and as a missing value otherwise. The sum of the scores for these twelve food groups constituted our index of organic food consumption. If a participant had answered at least one of the twelve items about organic food consumption, missing values for one or more of the other items were given no points. On the contrary, if a participant had missing values for all items, the data concerning organic food consumption were considered to be missing (note that the same procedure was applied to all composite variables of this study).
We assessed the pertinence of this index of organic food consumption by assessing its convergent validity with data of the 24HR. For each brand-named aliment consumed and reported in the 24HR, the brand was used to determine whether the aliment was necessarily produced by organic or conventional agriculture or whether this information could not be determined from the brand name (water was excluded from this list given that it cannot be produced by organic agriculture). Then, we determined the percentage of aliment consumed that was explicitly produced by organic agriculture (total number of aliments produced by organic agriculture/total number of aliments for which the brand was reported) for each participant. Spearman correlations (performed without taking the survey design into account since Spearman’s rho is not currently implemented in the syvset feature of Stata or the ‘survey’ package in R) revealed moderate to strong associations between the percentage of organic aliments reported in the 24HR and our index of organic food consumption, suggesting the appropriateness of this index (Spearman’s rho = 0·52 in children and adults).
Anthropometric measures
The weight and height of individuals were measured during a home visit. Weight was measured using a digital scale (accuracy = 100 g). Participants were weighed in light clothes with no shoes. Following the WHO recommendations, height was measured using a measuring tape and an angle stop. Less than 9 % of participants were not measured (height, weight or both) and instead declared their weight and/or height. Restricting analyses to participants with a measured height and weight did not affect our results. BMI was computed as the ratio of the weight and the squared height for all participants (kg/m2). The BMI-z could not be computed in children because the exact age of the participants was not publicly released due to ethical reasons (exact age, in combination with other variables, may lead to the identification of a participant). Therefore, although organic food consumption was not related to age in the children group, we reproduced our analyses with the tri-ponderal mass index as a dependent variable. The tri-ponderal mass index is an alternative to the BMI known to be less affected by developmental age(Reference Peterson, Su and Thomas28). Results of the children group remained unchanged with this alternative dependent variable. The obesity status was estimated following international guidelines (children and adolescents: International Obesity Task Force(Reference Cole and Lobstein29); adults: WHO(30)).
Confounding variables
Demographics
The two demographic variables used as covariates were sex and age group. Children and adolescents were grouped within four ordered categories, early childhood (4–6 years old), late childhood (7–10 years old), early adolescence (11–14 years old) and late adolescence (15–17 years old), and adults within three, early adulthood (18–44 years old), middle adulthood (45–64 years old) and elderly (65–79 years old).
Education level and family income
The education level (or parental education for minor participants) and income per household unit were recorded as proxies of socio-economic status. Education level was divided into seven ordered categories based upon highest diploma achieved (from elementary school to doctorate), and family income was divided into four ordered categories (<€900 per month, between €900 and €1339 per month, between €1340 and €1850 per month, and more than €1850 per month).
Energy intake
Overall gross energy intake was obtained by converting data recorded in the 24HR using a standard nutrient composition table(31).
Mediterranean diet
To assess consistent adherence to the MD throughout life, we used a modified version of two standard MD indices (one designed for children and adolescents, KIDMED(Reference Serra-Majem, Ribas and García32); one designed for adults(Reference Trichopoulou, Costacou and Bamia33)). For each participant, the consumption of various food groups was compared with that of participants of the same sex and similar age. Data from the food propensity questionnaire were preferred over those of the 24HR for long-term food consumption tendencies (data from the 24HR were used only for computing the monounsaturated:saturated fat ratio). Participants were given one point if they had a higher intake of vegetables, legumes, fruits and tree nuts, cereals, fish and a higher monounsaturated:saturated fat ratio relative to the median of their age- and sex-matched group. They also obtained one point if they had a lower intake of meat and sugar-added dairy products and a lower frequency of eating fast food. Participants obtained a score ranging from 0 to 9, in which higher scores represent a higher adherence to the MD.
Dietary supplements
Participants reported their dietary complement use and were then categorised as users or non-users of dietary complements. The French legal definition of dietary complements was used (Article 2, Décret no. 2006-352).
Regimen
Following a specific regimen – for example, due to personal conviction (e.g. veganism), for a specific condition (e.g. food allergy) or for weight loss – was recorded and included as a dichotomous covariate (following v. not following a regimen).
Food processing
Information on the method of production was collected for all mixed dishes and for the majority of processed foods, that is, composed of several ingredients (e.g. savoury pies, cakes, etc.). Then, this information was dichotomised depending on whether the food was prepared/processed at home or not. Other preparation/processing options were: industrially processed, prepared by an artisan, prepared at a school cafeteria, prepared in a classic restaurant, prepared in a fast-food restaurant, prepared in an automatic distributor (e.g. tea, coffee and soup), not prepared at home or did not know. An index of food processing was then computed by calculating the proportion of foods prepared or processed at home for each participant.
Physical activity and sedentary lifestyle
For all participants, previously validated questionnaires were used to assess physical activity and sedentary lifestyle (children: Santé publique France questionnaire(27); adolescents: questionnaire used in the Youth Risk Behavior Survey(Reference Troped, Wiecha and Fragala34); adults: adapted version of the Recent Physical Activity Questionnaire(Reference Golubic, May and Borch35)). Questionnaires focused on the past 7 d for children and adolescents and the past month for adults. Physical activity and sedentary lifestyle were categorised into three ordered categories (low, moderate and high). The levels of physical activity were adapted from those given by the WHO (see details in online Supplementary Text S3 (36)). The levels of sedentary lifestyle were adapted from previous studies (being sedentary for an amount of time strictly inferior to 3 h/d was categorised as low, between 3 and 7 h/d as moderate, and strictly above 7 h/d as high(Reference Chau, Grunseit and Chey37,Reference Rezende, Sá and Mielke38) ).
Statistical analysis
Our analyses were performed using Stata (version 16) and R. Because the data were collected using a complex survey design and to ensure representativeness of our sample, we used the syvset function of Stata or the ‘survey’ package in R(Reference Lumley39). These analyses make it possible to adjust standard statistical analyses (e.g. linear regressions) by considering multiple elements of the design (such as sampling units, weights, number of sampling stages and finite population correction). Moreover, all analyses performed on subpopulations (e.g. the exclusion of infants and toddlers of the children age group) were performed using the subpop command in Stata or the subset function of the ‘survey’ package in R. Because the sample of children and adolescents v. adults was not drawn from the same population, we could not merge these two groups within the same model. Therefore, models were estimated on children and adolescents on the one hand and adults on the other.
The independent variable in all regression models was organic food consumption, the dependent variable was either the BMI or obesity status (obese v. non-obese) and the covariates were the age group, sex, family income, education level, energy intake, MD adherence, dietary supplements, regimen, processing of food, physical activity and sedentary lifestyle level. All these potential confounding variables were selected a priori and were retained in the present analyses, regardless of their association with the outcome or exposure. Although it has sometimes been recommended to adopt a data-driven method to select covariates (e.g. Dunkler et al. (Reference Dunkler, Plischke and Leffondre40)), this would have potentially led us to include a different set of covariates depending on the outcome (BMI or obesity status) and/or age group (youths or adults). Therefore, we included all a priori covariates in the adjusted models to facilitate comparison of the various regression models used in this study. However, it could be argued that the significance of the main analyses presented in this study could have been driven by a suppression effect. We have thus reproduced all our regression analyses but selecting the covariates using a backward elimination procedure with a retention criterion of 0·20. The results were similar to those reported in the manuscript for the two age groups.
We performed linear regressions when BMI was the dependent variable and logistic regression when obesity status was the dependent variable. Our organic index was treated as a continuous variable in all regression models. In linear regressions, we report the unstandardised regression coefficient along with the partial correlation coefficient and the R 2 statistics. The R 2 was obtained by performing the ratio of the dispersion parameter:the population variance subtracted from 1. In logistic regressions, we report OR (crude or adjusted depending on the presence of covariates) and the pseudo R 2 (using the Nagelkerke method)(Reference Lumley39).
It should be noted that several participants had missing data. Although no variable had more than 13 % missing values, recent guidelines recommend addressing this issue by performing multiple imputation rather than complete case analysis (e.g. Madley-Dowd et al. (Reference Madley-Dowd, Hughes and Tilling41)). Therefore, we performed both multiple imputation and complete case analysis. Multiple imputation was performed using chained equations (with twenty imputations) and with all our predictors with no missing values, the organic food consumption obtained via the 24HR, and various nutritional status indicators as auxiliary variables. No small sample adjustments were made. The ratio of variables to cases with complete data was lower or equal to 1 %, which is well below the recommended 33 % cut-off(Reference Hardt, Herke and Leonhart42). The largest fraction of missing information was systematically lower than 0·27. For the complete case analysis, participants with a missing value for the outcome, predictor or any of the covariates were excluded from models.
Finally, to the best of our knowledge, statistical procedures to diagnose regression models combining multiple imputation and a complex survey design have not yet been implemented in standard statistical software. Therefore, we did not report any regression diagnostic for our models using multiple imputation. However, interested readers may find a complete description of regression diagnostics for the subsample of models for which regression diagnostics were feasible in Supplemental Analysis S4: linear regressions with complete case analysis(Reference Li and Valliant43–Reference Lee and Valliant45). The ‘svydiags’ package in R was used for these analyses(Reference Valliant46).
Results
Overall, obesity was present in 4 % of children and adolescents and 17 % of adults. As shown in Fig. 1, a substantial proportion of both the children and adults samples did not report consuming any organic food over the last year. However, more than 25 % of the participants in the two age groups have nonetheless an index of organic food consumption superior or equal to 10. The characteristics of the participants according to their organic food consumption are presented in Table 1. Because multiple imputation is intrinsically designed for inference purpose, the means and proportions presented are based on non-imputed values of participants with no missing data on all our variables (i.e. participants included in the complete case analysis). As predicted, participants significantly differed for several of the targeted variables. In both the children and adults groups, organic food consumption tended to be associated with a higher education level, family income, MD adherence, dietary supplement use, home-made food processing and lower levels of sedentary lifestyle (all P values < 0·05). Organic food consumption was also associated with a higher level of physical activity but specifically in adults. In contrast, organic food consumption tended to be related to a higher adherence to a regimen and a lower energy intake in children (both P values were marginally significant) but not in adults. Last, consumption of organic food was not related to age and sex in both groups.
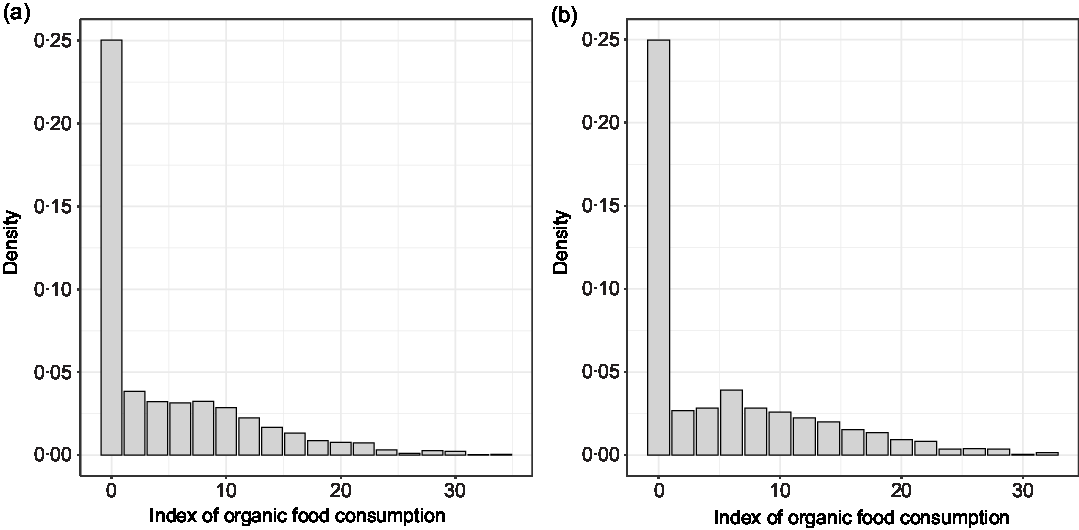
Fig. 1. Distribution of the index of organic food consumption in children (a) and adults (b).
Table 1. Characteristics of the sample according to organic food consumption*
(Percentages; mean values with their standard errors)
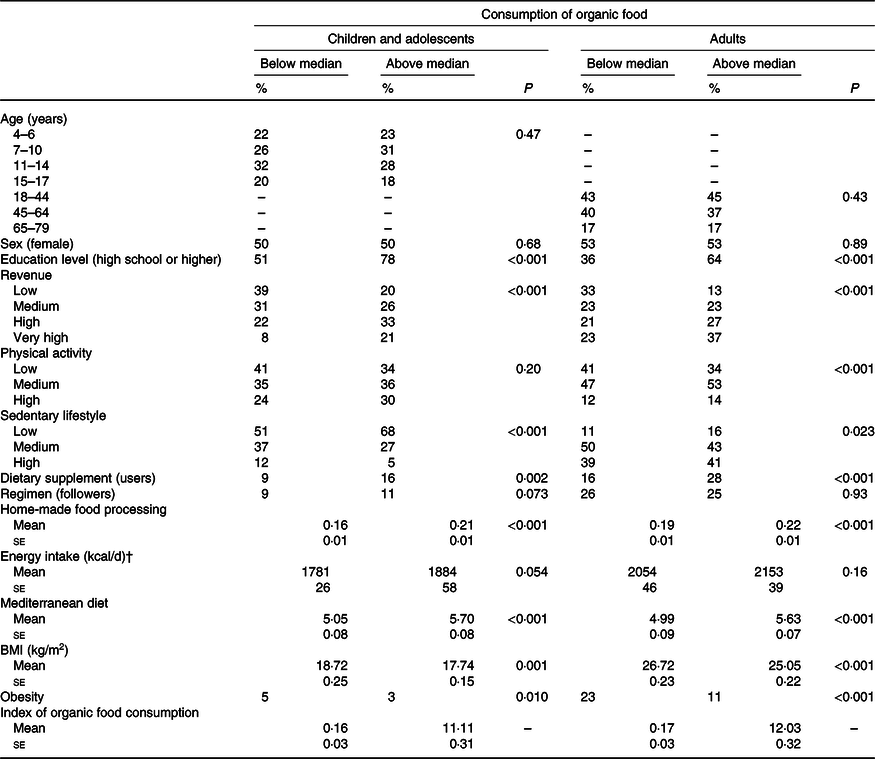
* Organic food consumption was the independent variable of univariate regressions including each of the variables presented here as dependent variable. Dichotomisation of the organic food consumption (below median v. above median) and education level was made for presentation purposes.
† To convert kcal to kJ, multiply by 4·184.
Concerning the relationship between organic food consumption and BMI or obesity status, unadjusted models systematically revealed a negative relationship (all P values < 0·01). Greater consumption of organic food was associated with a lower BMI in the two age groups. Similarly, greater consumption of organic food was also associated with a lower obesity rate (see Fig. 2). These associations remained statistically significant in adjusted models controlling for all a priori confounding variables (excepted for complete case analysis, in which the adjusted association between organic food consumption and obesity was marginally significant in children; see Table 2). Critically, effect sizes were systematically low in both the unadjusted and adjusted models.
Table 2. Coefficients for the multiple regression models using either multiple imputation (MI) or complete case analysis (CCA) and in which BMI and obesity status are alternatively used as the dependent variables*
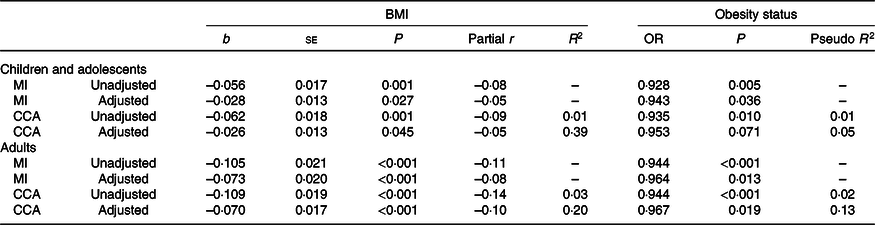
* Unadjusted models were run with no covariate. Adjusted models were run with all a priori covariates: demographics (age and sex), socio-economic status (family income and education level), nutritional covariates (Mediterranean diet adherence, food processing, regimen, dietary supplements and energy intake) and physical activity (physical activity and sedentary lifestyle). BMI was treated as a continuous variable (linear regression) and obesity status as a categorical variable (logistic regression).
Interested readers may find a complete description of the diagnostics of linear regression models using complete case analysis and including BMI as the dependent variable in online Supplementary Analysis S4. Essentially, these diagnostics revealed that the adjusted association of organic food consumption with BMI remained statistically significant (or marginally statistically significant) when excluding influential observations. Effect sizes remained of similar magnitude.
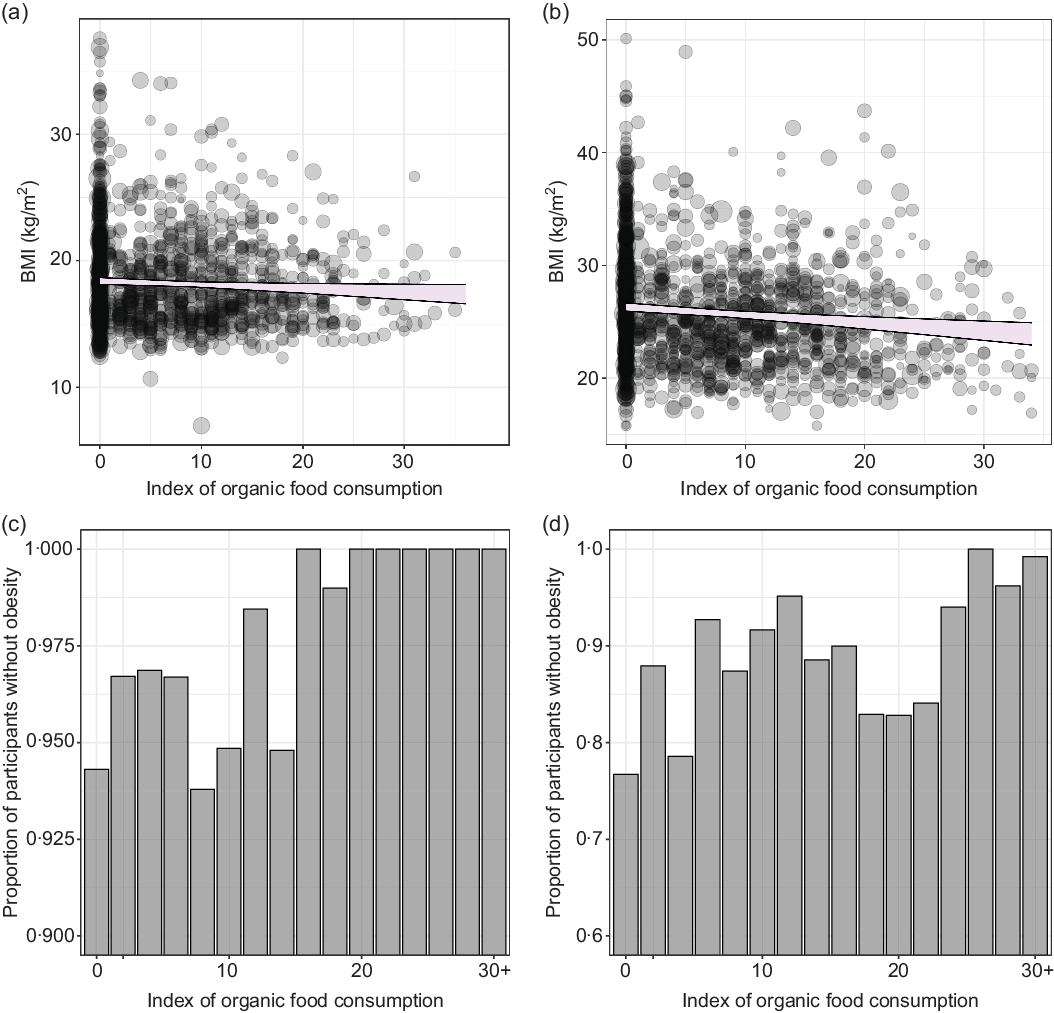
Fig. 2. Scatterplots of the association of organic food consumption with BMI in children (a) and adults (b). The size of the dots reflects their sampling weight. The lines represent the 95 % confidence intervals around the slope of the regression line adjusted for covariates. Proportion of participants without obesity depending on the organic food consumption in children (c) and adults (d).
Discussion
Based on the data of the INCA3 study, we assessed the relationship between organic food consumption and obesity in a nationally representative sample comprising children, adolescents and adults. In both childhood and adulthood, unadjusted associations revealed that organic food consumption is negatively associated with BMI and obesity. Of interest, although the consumption of organic food was associated with a wide range of socio-economic status and lifestyle factors, the association of organic food consumption with both BMI and obesity persisted after accounting for these potentially confounding variables. Notably, the strength of these associations could be classified as small.
Our data not only confirmed the negative association of organic food consumption with BMI and obesity previously found by previous epidemiological studies, but they also extend these studies in several ways. First, the present study is the first epidemiological study to show that the association of organic food consumption with BMI and obesity is not restricted to the adult population. Second, this is also the first study to assess the convergent validity of the index of organic food consumption. Our index showed a moderate to strong association with objective data collected in the 24HR. Although a stronger association could have been expected, it is worth noting that the index of organic food consumption targets a relatively long period (the previous year), whereas the 24HR targets a very short period (2 or 3 d). In addition, the strength of the convergent validity was similar in both age groups, indicating the relative appropriateness of this index throughout life. Future studies should investigate the psychometric properties of the organic food consumption index to develop more reliable methods to assess it. Finally, this study is also the first to combine a complex survey design, resulting in a nationally representative sample, and an adjustment for confounding variables. These two methodological precautions, associated with various sensitivity analyses, confirmed the robustness of the association between organic food consumption and obesity during childhood and adulthood. Of note, the sampling of the present study – and the non-availability of each participant exact age – did not allow assessing the development of the association between organic food consumption and either BMI or obesity rate throughout life. This remains to be evaluated in future work.
This study addressed two of the main biases of observational studies: information bias, by assessing the convergent validity of the organic food index and objectively measuring height and weight, and selection bias, by using a complex survey design ensuring the representativeness of our sample. Concerning confounding bias, even if we controlled for the main confounding factors related to obesity (such as energy intake and energy expense), residual confounding factors may explain our results. In particular, no study investigating the association of organic food consumption with BMI and obesity (including ours) has considered psychological factors, although it is well known that they are intimately related to obesity (e.g. Yang et al. (Reference Yang, Shields and Guo47)). For example, numerous observational studies have shown a bidirectional association between obesity and depression(Reference Rajan and Menon48). Moreover, another potential residual confounding factor is drug use. Numerous studies have shown that drug use is associated with weight gain (e.g. Apovian et al. (Reference Apovian, Aronne and Bessesen49)); to the best of our knowledge, no study has yet examined whether the prevalence of drug use differs depending on organic food consumption. Therefore, it is possible to argue that the relationship between organic food and obesity consistently found in epidemiological studies is artificially produced by the shared influence of psychological factors and/or drug use on both the likelihood to consume organic food and the obesity rate. Future studies should address this issue.
Finally, an important limitation of our results regards the length of the period assessed in the questionnaire of organic food consumption. Although the present index targets a relatively lengthy period for a questionnaire (1 year), it is very important to note that BMI and obesity status are the result of a nutritional history that exceeds the previous year. Future very long-term longitudinal studies should therefore provide important insights into our understanding of the association between organic food consumption and obesity.
In conclusion, our data confirm the association of organic food consumption with both BMI and obesity during childhood and adulthood. Although this association remained statistically significant after controlling for several potential confounding variables, the corresponding effect sizes were small. Future randomised controlled trials are required to investigate causality between organic food consumption and lower BMI or obesity rate.
Acknowledgements
The present study received no specific funding.
C. J. G. and A. G. designed the research; C. J. G., M. E. and R. V. analysed the data; C. J. G., A. G., M. E. and R. V. interpreted the data and wrote the paper. C. J. G. had primary responsibility for the final content. All authors read and approved the final manuscript.
The authors have no conflicts of interest to declare.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114520003189







