Introduction
Globally, there are an estimated 300,000 maternal deaths each year, and approximately 20% of these occur in Nigeria (WHO, 2015). In 2015, it was estimated that Nigeria’s maternal mortality ratio (MMR) was 800 deaths per 100,000 live births, which totals approximately 58,000 deaths (WHO, 2015). It is likely that the MMR is much higher in north-western Nigeria where maternal health outcomes are typically worse than national averages (Government of Nigeria and DHS Program, 2019). Given the burden of maternal mortality in Nigeria, improving maternal health in the country is both a national priority and a cornerstone for achieving the United Nations Sustainable Development Goals (United Nations, 2015; Government of Nigeria & DHS Program, 2019; Souza, Reference Souza2019).
Antenatal care (ANC) visits and facility-based deliveries are critical contact points with the formal health system that present opportunities to reach mothers and newborns with effective interventions to improve their chances of survival and well-being (WHO, 2016). The World Health Organization (WHO) has recommended at least four ANC visits (ANC4+) during pregnancy, and more recently eight routine check-ups, in order to provide a range of interventions for a positive pregnancy experience (WHO, 2016). The WHO also promotes giving birth in a health facility with skilled personnel, since most deaths are due to direct obstetric causes that occur around the time of delivery and are difficult to predict in advance (Sageer et al., Reference Sageer, Kongnyuy, Adebimpe, Omosehin, Ogunsola and Sanni2019). Nigerian national guidelines for pregnancy and childbirth are closely aligned with these global recommendations (Government of Nigeria, 2017a).
Despite the importance of these essential maternal health services, there remains low utilization of ANC and facility-based delivery in north-western Nigeria (Pedersen & Liu, Reference Pedersen and Liu2012). According to the 2018 Nigeria Demographic and Health Survey (DHS), only half (53%) of women aged 15-49 years in north-western Nigeria attended ANC at least one time with a skilled provider during her last pregnancy, and only 16% gave birth in a facility (DHS, 2019). Previous qualitative and quantitative research conducted in north-western Nigeria suggests that barriers to uptake of these services may include distance to the health facility, health care costs, spousal disapproval, religious beliefs, maternal education, lack of perceived need, as well as broader gender norms and socio-cultural dynamics (Adamu & Salihu, Reference Adamu and Salihu2002; Fetohy, Reference Fetohy2004; Doctor et al., Reference Doctor, Findley, Ager, Cometto, Afenyadu, Adamu and Green2012; Fagbamigbe & Idemudia, Reference Fagbamigbe and Idemudia2015; Ishola et al., Reference Ishola, Fayehun, Isiugo-Abanihe, Segun, Yusuf and Orji2017; Meh et al., Reference Meh, Thind, Ryan and Terry2019).
Psychosocial factors are also posited by theories as important intermediate determinants of a person’s actions, and are often targeted by Social and Behavioural Change (SBC) programmes to spur action. In the Ideation Model of Strategic Communication and Behaviour Change, psychosocial factors are theorized to consist of three ideational domains – cognitive, emotional and social – and each domain consists of specific behavioural influences, including: knowledge, attitudes, beliefs, perceived risk, subjective norms and self-image (cognitive); emotional response, empathy and self-efficacy (emotional); and social support, social influence, interpersonal communication and personal advocacy (social) (Kincaid et al., Reference Kincaid, Delate, Storey and Figeroa2013).
Despite the theorized importance of psychosocial influences on behavioural outcomes, there there has only been limited quantitative research examining their relationship with pregnancy and childbirth behaviours in low- and middle-income countries (LMICs), including Nigeria. The aim of this paper was to develop a set of pregnancy-related ideational metrics relevant to the north-western Nigerian context, and to subsequently examine their associations with the use of essential maternal health services, including attending ANC4+ times and giving birth in a facility.
Methods
Study setting
Data for this study were from a survey conducted in September 2019 in Kebbi, Sokoto and Zamfara states in north-western Nigeria within wards targeted for a SBC programme to help improve the health and well-being of women and children. The study analysed baseline survey data collected prior to initiation of the SBC programme (Johansson et al., Reference Johansson, Hutchinson, Omoluabi, Akinyemi, Smith and Welty2020).
The three study states share a border with Niger Republic, while Kebbi also borders Benin Republic to the west. The estimated populations of the states were 4.9 million (Sokoto), 4.3 million (Kebbi) and 4.4 million (Zamfara) in 2015 (Govenrment of Nigeria 2017b). Hausa is the dominant ethnicity and Islam is the main religion in the three states. The study area also has some of the highest poverty rates within Nigeria, and among the worst maternal and child mortality outcomes. According to the 2018 Nigeria Demographic and Health Survey (DHS, 2019) the under-five mortality rate was highest in the north-west region at 187 deaths per 1000 live births. Maternal mortality is relatively high in this region compared with national estimates (800 deaths per 100,000 live births in 2015). The region also has the highest total fertility rate in Nigeria, with 6.6 births per woman, and, on average, 8.3 children were born to a woman aged 40–49 years in 2018. In addition, only half of women attended ANC at least once during her last pregnancy, and only 16% delivered in a health facility according to the 2018 survey (DHS, 2019).
This same survey also showed that women’s empowerment measures in the north-western region were among the lowest nationally, including women who completed primary school (9%), were unemployed in the past 12 months (45%) and owned a mobile phone (35%), and married women who participated in their own health care decisions (20%). Early child marriage is common in this area, with mean age of first marriage at 15.4 years for women, and 18 years was the median age of first birth for a woman in 2018 (DHS, 2019). Early child marriage is linked to poverty and lack of educational and economic opportunities for women, reinforces the dominant role of men in the household and societal decision-making more broadly, and places young women at greater risk of pregnancy complications and other adverse health outcomes (Efevbera & Bhabha, Reference Efevbera and Bhabha2020; Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020). Qualitative research further highlights the importance of gender and cultural norms in health care utilization and broader social and economic opportunities for women (Adamu & Salihu, Reference Adamu and Salihu2002; Oguntunde et al., Reference Oguntunde, Nyenwa, Yusuf, Dauda, Salihu and Sinai2019; Yaya et al., Reference Yaya, Okonofua, Ntoimo, Udenigwe and Bishwajit2019).
The health system context itself also shapes women’s perceptions and their utilization of maternal health services. Health care provision is the responsibility of federal, state and local governments in Nigeria, and also commonly includes private health care provision (Government of Nigeria 2016). The federal government sets health policies, standards and regulations, and is also responsible for tertiary level care at federal medical centres and teaching hospitals. The State Ministries of Health provide secondary level care at comprehensive medical centres and general hospitals, while Local Government Areas (LGAs) focus on primary health care, which is overseen by the National and State Primary Health Care Development Agencies. In terms of maternal health services, the primary level is responsible for providing antenatal, delivery and postnatal care in addition to basic emergency obstetric care. Each LGA typically consists of 10–15 wards that have their own structures for Primary Health Care (PHC) delivery, including PHC centres, dispensaries, health posts and Community Health Extension Workers (CHEWs), which are also supported by Ward Development Committees (WDCs). Private provision of health care is also common in this area, including Proprietary and Patent Medicine Vendors (PPMVs) (Beyeler et al., Reference Beyeler, Liu and Sieverding2015).
Nevertheless, the availability and quality of maternal and reproductive health services varies across LGAs and wards in the north-west region (FMOH, 2016). Previous studies have highlighted important health system challenges in this area, including human resource constraints, limited service availability and inadequate equipment and supplies with common medicine stock-outs (Galadanci et al., Reference Galadanci, Ejembi, Iliyasu, Alagh and Umar2007; Fagbamigbe & Idemudia, Reference Fagbamigbe and Idemudia2015, Reference Fagbamigbe and Idemudia2017; FMOH, 2016). Such health system constraints influence community perceptions and practices with respect to local health services, as shown in this previous research and further investigated in the current study. Importantly, the SBC programme that will be implemented in the study area will be complemented by health system strengthening work which, taken together, aim to improve both supply- and demand-side problems in health system utilization in these states. The findings reported in this paper were derived from a baseline survey of the SBC programme evaluation to gauge women’s perceptions of local maternal health services.
Study design
A two-stage cluster-sample cross-sectional survey was conducted targeting women with a child under 2 years living in Kebbi, Sokoto and Zamfara states within wards targeted for SBC programming. The survey sample size was determined based on the SBC programme evaluation design, with three comparison groups. Sample size estimation allowed for a 10% non-response rate, a power criterion of 0.80, an alpha coefficient of 0.05 and varying intra-cluster correlations and minimal detectable differences for priority outcomes of the evaluation. Based on this estimation, a sample size of approximately 3000 women with a child under 2 years was estimated for survey inclusion. At the first sampling stage, a total of 108 enumeration areas (EAs) was selected from programme wards within the three states (36 EAs per state) using digital maps and a grid sampling methodology. At the second sampling stage, all households within each sampled EA were enumerated to randomly select households with a resident woman aged 15–49 years who had a child under 2 years.
Data collection
Fieldwork was conducted in September–October 2019 over a 4-week period by female interviewers recruited from the local communities. Interviewer training occurred during the 1-week period prior to data collection. This training reviewed the study objectives, protocol and instruments, fieldwork procedures and ethical considerations. All interviewers participated in a pilot exercise that tested skip patterns, checked questionnaire translation (Hausa) and assessed question appropriateness and sequence. There were two questionnaires administered to survey participants. The household questionnaire collected information on household members, characteristics and assets. The female questionnaire collected information on respondent demographics, reproductive history and gender norms. For women with a child under 2 years, respondents were specifically asked about behaviours during their last pregnancy in a standardized format to the Nigeria Demographic and Health Survey (DHS, 2019). These behaviours included ANC attendance, timing, location, provider type, content and number of check-ups during her last pregnancy. Women were also asked where she gave birth to her youngest child and who assisted with the delivery. Women who did not attend ANC or who gave birth outside a facility were asked about reasons for service non-use. In addition, all respondents were asked ideational questions related to various health behaviours, including pregnancy and childbirth.
Explanatory variables
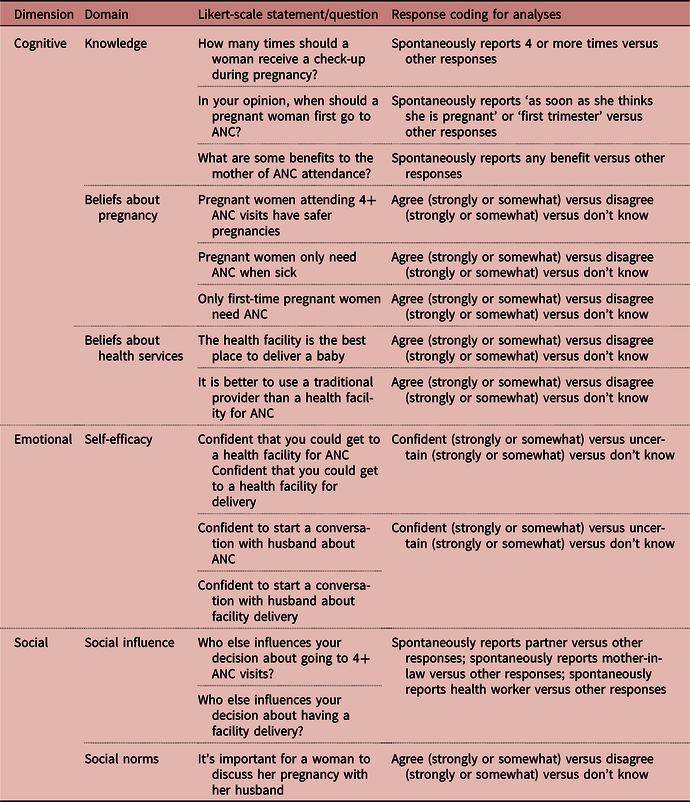
Table 1 presents the definitions of pregnancy-related ideations that were the main explanatory variables in the analysis. Ideational questions were developed using Kincaid’s Model of Strategic Communication and Behaviour Change with the aim to measure at least one psychosocial factor within each cognitive, emotional and social domain (Kincaid et al., Reference Kincaid, Delate, Storey and Figeroa2013). Survey questions were also adapted from ideational research in other health areas as appropriate (Kincaid et al., Reference Kincaid, Delate, Storey and Figeroa2013; Babalola et al., Reference Babalola, John, Ajao and Speizer2015; Larson et al., Reference Larson, Jarrett, Schulz, Chaudhuri, Zhou and Dube2015; Storey et al., Reference Storey, Babalola, Ricotta, Fox, Toso, Lewicky and Koenker2018). Socio-demographic variables were included in the analysis based on empirical evidence of their relationship with use of maternal health services in Nigeria and elsewhere (Amoakoh-Coleman et al., 2015; Fagbamigbe & Idemudia, Reference Fagbamigbe and Idemudia2015; Aliyu & Dahiru, Reference Aliyu and Dahiru2017; Okedo-Alex et al., Reference Okedo-Alex, Akamike, Ezeanosike and Uneke2019; Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020). These variables included maternal age (15–24, 25–34 or 35–49 years), maternal education (any formal education, none or informal education), spousal education (any formal education, none or informal education), maternal employment (works outside home or student, or does not work outside home), spousal employment (works outside home or student, or does not work outside home) and household wealth (lowest, second, third, fourth or highest wealth quintile). Wealth was measured using an asset-based measure constructed from ownership of key consumer durables and then compiled into an index using principal components analysis (Filmer & Pritchett, Reference Filmer and Pritchett1998). Households were then categorized into quintiles from lowest to highest wealth asset ranking.
Table 1. Pregnancy-related ideational metrics
Outcome definitions
There were two main outcomes. The first outcome was ANC4+, defined as reported attendance at ANC at least four times by the respondent during her last pregnancy within the past 2 years, and where the first visit was with a skilled provider (doctor, nurse or midwife). Specifically, during the survey interview, the woman was asked if she saw anyone for ANC during her last pregnancy, and if so, whom she saw for the first visit. She was then asked how many ANC check-ups she had during this pregnancy. The second outcome was facility-based delivery, defined as giving birth in a health facility during her last pregnancy within the past 2 years. During the survey interview, the woman was asked where she gave birth during this pregnancy; a facility-based delivery included: government hospital, PHC centre, health post, community health outreach post, nursing/maternity home, private hospital or private clinic.
Data analysis
Mixed-effects logistic regression models were used to estimate average marginal effects, or the change in the probability of an outcome when a predictor variable increased by one unit. For binary predictor variables, marginal effects represent the additional likelihood of using ANC or delivering in a facility for a person who possesses that characteristic (e.g. husband influences decisions about delivering in a facility) relative to a person who does not. All ideational and socio-demographic variables were included in the models as categorical fixed effects nested within cluster identifiers. Testing for multicollinearity among variables was conducted using variance inflation factors. The level of statistical significance was set to p<0.05. Point estimates were tabulated using weights to account for unequal probabilities of selection. Standard error estimation accounted for data clustering in the complex survey design. All analyses were conducted in Stata version 16.
Results
A total of 3039 women responded to questions about the antenatal and delivery care received during her last completed pregnancy in the past 2 years. Among these respondents, 23.6% (95% CI: 18.0–30.3) attended ANC4+ times during her last pregnancy, and 15.5% (95% CI: 11.8–20.1) gave birth in a health facility (Table 2). The mean age of respondents was 26.0 years, while the average age of their spouse was 38.7 years. Only 26.1% and 31.0% of respondents and their spouses had any formal schooling, while 50.3% and 91.9% worked outside the home, respectively. There was a mean of 2.2 wives per husband in the study sample.
Table 2. Socio-demographic characteristics of study sample
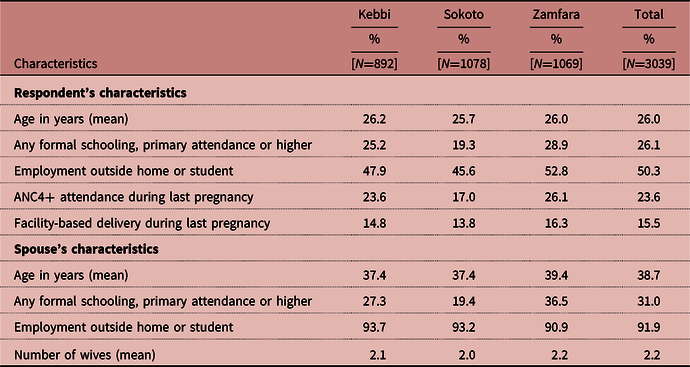
Point estimates were derived using weights to account for unequal probabilities of selection in the survey sample.
Bivariate results of ANC4+ and facility-based delivery by ideational variables
Among respondents attending ANC4+ times during her last pregnancy, a greater percentage had positive cognitive, emotional or social ideations than negative or disagreeable ones. For example, 48.1% (95% CI: 39.2%–57.2%) knew that women should receive four or more check-ups during pregnancy and only 4.9% (95% CI: 3.2%–7.5%) were unaware of this (knowledge) (Table 3). Similarly, 11.7% (95% CI: 23.3%–40.6%) believed pregnant women only need ANC when sick compared with 34.9% (95% CI: 26.4%–44.4%) who did not hold this belief (beliefs). At the same time, 34.0% (95% CI: 26.6%–42.3%) of these respondents were confident they could get to a health facility for ANC compared with 1.3% (95% CI: 0.6%–3.1%) who were uncertain (self-efficacy). Among respondents attending ANC4+ times during their last pregnancy, health workers (37.9%, 95% CI: 20.1%–59.6%) and spouses/partners (28.9%, 95% CI: 21.5%–37.5%) were most commonly cited as influencing the woman’s decision.
Table 3. Facility-based delivery and ANC4+ attendance reported by women aged 15–49 years with a live birth in the past 2 years by socio-demographic and ideational variables
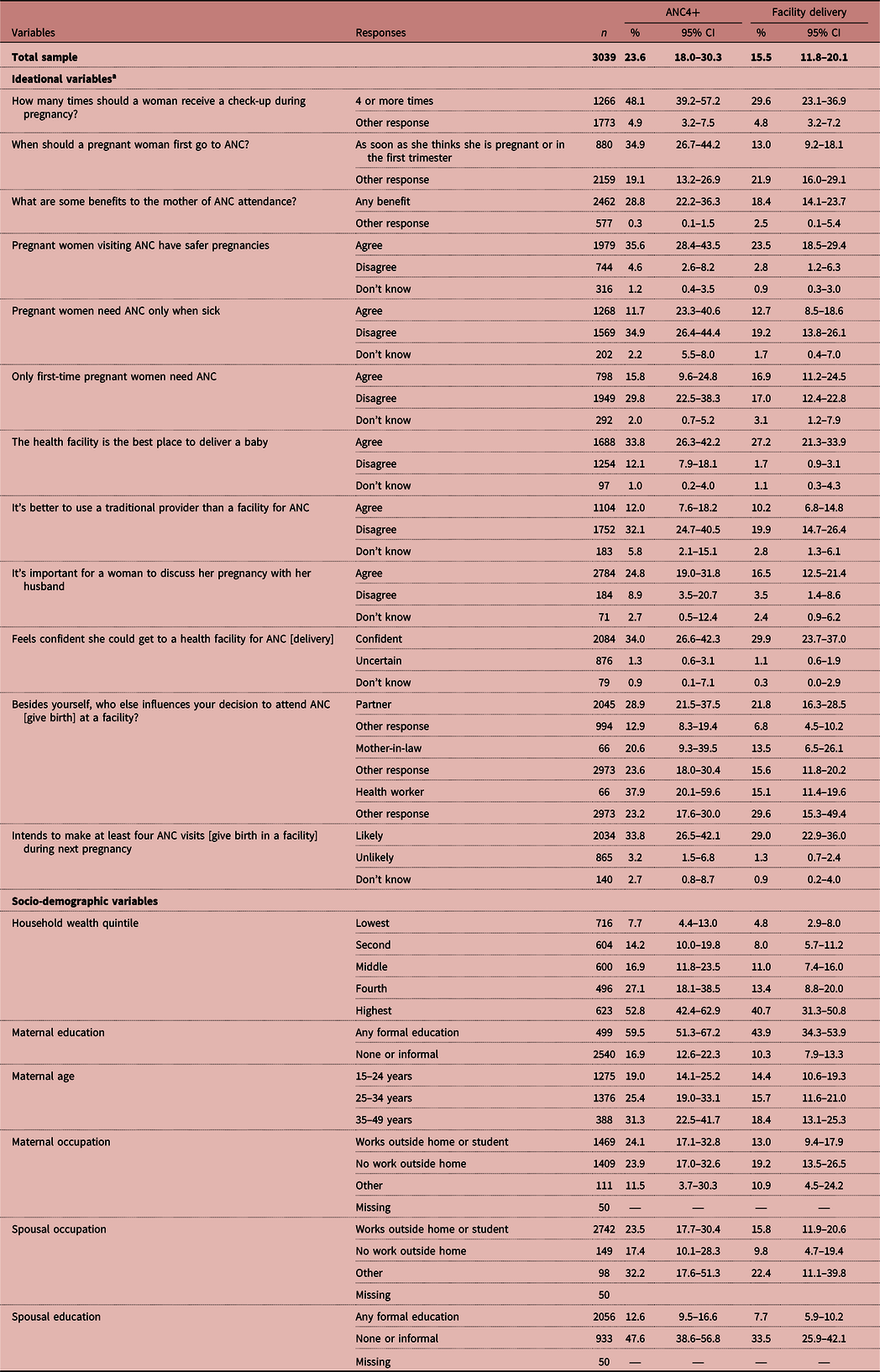
a Likert-scale statements with ‘Agree’ and ‘Confident’ and ‘Likely’ include ‘strongly or somewhat’ in the responses.
—: not applicable; variable not included in the regression model for that outcome.
Point estimates were derived using weights to account for unequal probabilities of selection in the survey sample. Confidence intervals accounted for clustering in the complex survey design.
A similar ideational pattern occurred among women who gave birth in a facility during her last pregnancy. Specifically, 29.6% (95% CI: 23.1%–36.9%) of respondents who gave birth in a facility knew that women should receive four or more check-ups during pregnancy compared with 4.8% (95% CI: 3.2%–7.2%) of respondents who did not know (knowledge). Similarly, 27.2% (95% CI: 21.3%–33.9%) of these same respondents believed that the health facility was the best place to deliver a baby compared with 1.7% (95% CI: 0.9%–3.1%) who disagreed (beliefs), while 29.9% (95% CI: 23.7%–37.0%) of these respondents were confident they could get to a health facility for delivery compared with 1.1% (95% CI: 0.6%–1.9%) who were uncertain (self-efficacy). Among respondents who gave birth at a facility during the last pregnancy, spouses/partners (21.8%, 95% CI: 16.3%–28.5%) were most commonly cited as influencing the woman’s decision to give birth in a facility.
Among women who did not attend ANC4+ times or give birth in a facility during her last pregnancy (Figure 1), 41.4% and 66.8% did not perceive it as necessary to go to ANC (95% CI: 33.0%–50.3%) or give birth in a facility (95% CI: 58.5%–74.3%), respectively. Spousal opposition was also a commonly cited reason for not attending ANC4+ times (25.2%, 95% CI: 18.3%–33.6%) or for giving birth in a facility (27.3%, 95% CI: 20.8%–34.9%).
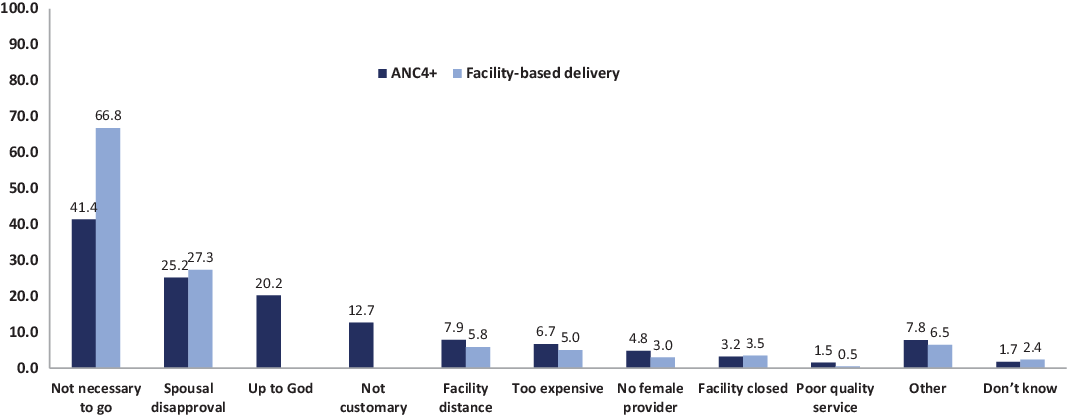
Figure 1. Women’s reported reasons for non-use of ANC and facility-based delivery services among women who did not attend ANC4+ or give birth in a facility during their last pregnancy. Percentages are those who cited specific reasons for non-use of services. Note that the percentages do not sum to 100 since multiple responses were allowed.
Ideational associations with ANC4+ visits
The psychosocial factors significantly associated with attending ANC4+ times in regression analyses included: ANC knowledge, beliefs about ANC efficacy and health services quality, self-efficacy and supportive spousal influence on decision-making (Table 4, Figure 2). In the adjusted analysis, the probability of attending ANC4+ times increased 16 percentage points (95% CI: 0.12–0.19, p<0.001) if the respondent knew that women should receive four or more check-ups during pregnancy compared with those who were not aware (knowledge); increased 5 percentage points (95% CI: 0.02–0.08, p=0.002) if she knew that women should initiate ANC in the first trimester or as soon as she thinks she is pregnant (knowledge); increased 16 percentage points (95% CI: 0.10–0.23, p<0.001) if she was able to report any ANC benefit for herself (knowledge); increased 5 percentage points (95% CI: 0.01–0.10, p=0.021) if she believed women who attend ANC4+ have safer pregnancies (beliefs); decreased 4 percentage points (95% CI: 0.00–0.08, p=0.037) if she believed only sick pregnant women needed ANC (beliefs); increased 4 percentage percentage points (95% CI: 0.01–0.08, p=0.006) if she believed that the health facility was the best place to deliver a baby (beliefs); increased 15 percentage points (95% CI: 0.11–0.20, p<0.001) if she felt confident that she could get to a health facility for ANC (self-efficacy); increased 4 percentage points (95% CI: 0.00–0.07, p=0.029) if she reported that her spouse/partner supported her decision to attend ANC4+ (social influence). The following socio-demographic variables were also significantly associated with ANC4+ attendance in the adjusted analysis: household wealth, maternal employment, maternal education and spousal education.
Table 4. Ideational and socio-demographic associations with ANC4+ and facility-based delivery for women aged 15–49 years with a live birth in the past 2 years
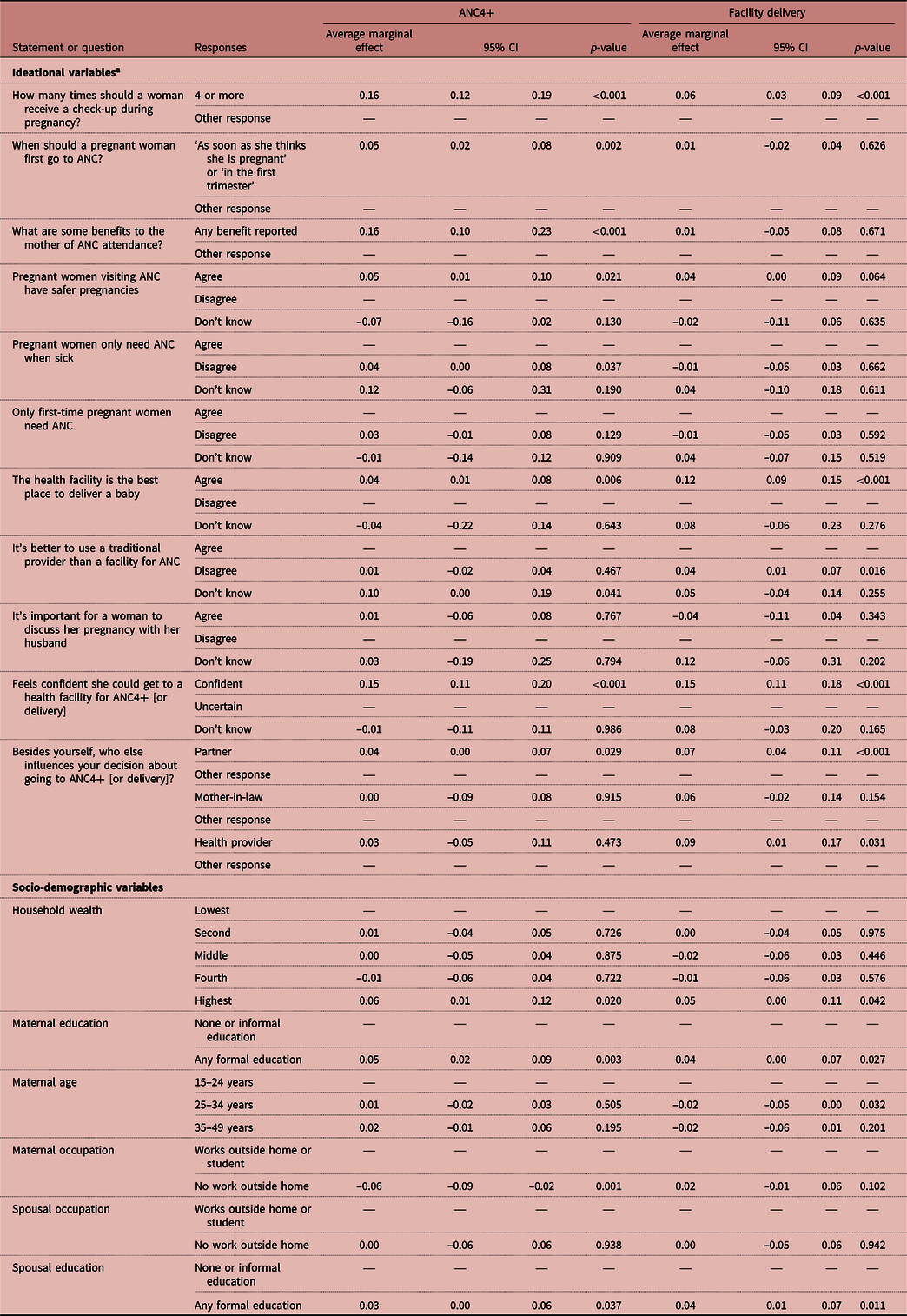
a ‘Likert-scale statements with ‘Agree’ and ‘Confident’ include ‘strongly or somewhat’ in the responses.
—: Reference category.
Average marginal effect estimates were derived from mixed-effects logistic regression models adjusted for ideational and socio-demographic variables. All variables were included as fixed effects nested within cluster identifiers. The level of statistical significance was set to p<0.05.

Figure 2. Predicted probabilities of a) ANC4+ and b) facility-based delivery among those with or without significant ideational characteristics. Note that the predicted probabilities were computed based on the average marginal effect estimates derived from mixed-effects logistic regression models adjusted for ideational and socio-demographic variables. All variables were included as fixed effects nested within cluster identifiers. Level of statistical significance was set to p<0.05.
Ideational associations with facility-based delivery
The psychosocial factors significantly associated with facility-based delivery were ANC knowledge, beliefs about health services quality, self-efficacy as well as spousal and health worker influence on decision-making (Table 4, Figure 2). After adjustment for other variables, the probability of giving birth in a facility increased 6 percentage points (95% CI: 0.03–0.09, p<0.001) if the respondent knew that women should receive four or more check-ups during pregnancy compared with those who were not aware (knowledge); increased 12 percentage points (95% CI: 0.09–0.15, p<0.001) if she believed that the health facility was the best place to deliver a baby (beliefs); decreased 4 percentage points (95% CI: 0.01–0.07, p=0.016) if she believed it was better to use a traditional provider than a health facility for ANC (beliefs); increased 15 percentage points (95% CI: 0.11–0.18, p<0.001) if she felt confident that she could get to a health facility for delivery (self-efficacy); increased 7 percentage points (95% CI: 0.04–0.11, p<0.001) if she reported that her spouse/partner supported her decision to give birth in a facility (social influence); increased 9 points (95% CI: 0.01–0.17, p=0.031) if she reported that a health provider supported her decision to give birth in a facility (social influence). The following socio-demographic variables were also significantly associated with facility-based delivery in the adjusted analysis: household wealth, maternal age, maternal education and spousal education.
Discussion
Across the study area, there were low levels of ANC4+ attendance and facility-based delivery among women aged 15–49 years during her last pregnancy in the past 2 years. The study findings suggest that cognitive, emotional and social psychosocial factors play an important role in the study women’s pregnancy and childbirth decisions, which are shaped by the broader socioeconomic, cultural and health system contexts of the north-west region (Galadanci et al., Reference Galadanci, Ejembi, Iliyasu, Alagh and Umar2007; Fagbamigbe & Idemudia, Reference Fagbamigbe and Idemudia2015; Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020). Specifically, ANC knowledge and beliefs, self-efficacy in accessing services, spousal support in pregnancy and childbirth decisions and positive perceptions of maternal health services quality were found to be among the most important ideations for SBC programmes to target in north-western Nigeria in relation to improving ANC4+ attendance and facility-based delivery. Such efforts must by complemented by health system strengthening efforts and other programmes that address entrenched gender and social norms that reduce women’s participation in health care decision-making.
Within the cognitive domain, knowledge of ANC timing and benefits was significantly associated with attending ANC4+ times and giving birth in a facility. This included knowing the recommended number of ANC check-ups and when to initiate the first ANC visit, as well as reporting at least one ANC benefit to herself. Indeed, it is well-recognized that raising knowledge about health behaviours, including pregnancy and childbirth, is an essential first step for health-promotion activities (Kincaid et al., Reference Kincaid, Delate, Storey and Figeroa2013). The present study results suggest that SBC programmes in north-western Nigeria may need to focus on increasing a woman’s basic ANC knowledge, as well as promoting the benefits to herself/child of ANC and facility-based delivery in these communities in order to increase service uptake.
At the same time, SBC programmes must also go beyond knowledge to address the cognitive beliefs that have been shown to further impede progress. In this study, women who believed that pregnant women attending ANC4+ times had safer pregnancies were 1.3 times more likely to attend ANC4+ times than those who did not, while women who thought ANC was only for sick pregnant women had 17% lower likelihood of ANC4+ attendance. The perception that ANC is only necessary if illness complications arise aligns with previous research suggesting that women often perceive pregnancy as a normal condition and place low value on antenatal care when feeling well (Finlayson & Downe, Reference Finlayson and Downe2013; Warri & George, Reference Warri and George2020). It also dovetails with the most common reason cited by women in the present study for non-use of ANC services – a lack of perceived need. The SBC programmes may therefore need to reinforce the importance of ANC to women and children even during healthy pregnancies without complications. Women’s beliefs about local health services quality were also associated with ANC4+ attendance and facility-based delivery, which underscores long-standing evidence that quality of health services is a main determinant of its use (Kruk et al., Reference Kruk, Hermosilla, Larson and Mbaruku2014; Larson et al., Reference Larson, Gage, Mbaruku, Mbatia, Haneuse and Kruk2019).
Within the emotional dimension, self-efficacy was a significant ideational domain associated with ANC4+ attendance and facility-based delivery. Women who felt confident that they could get to a facility for ANC or delivery were 2.5 and 3.4 times more likely to attend ANC4+ times or to give birth in a facility than women who lacked such confidence. Indeed, inability to access facilities due to transport or other issues is a common barrier to service uptake (Bohren et al., Reference Bohren, Hunter, Munthe-Kaas, Souza, Vogel and Gülmezoglu2014). Yet, women’s empowerment and confidence in their own ability to undertake the behaviour is an important behavioural influence itself (Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020) and further research should explore the complex reasons women may feel uncertain around accessing care for pregnancy and childbirth, including entrenched gender and cultural norms in this area, which reduce women’s participation in health care decision-making more broadly (Babalola et al., Reference Babalola, John, Ajao and Speizer2015; Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020).
Within the social dimension, supportive spousal influence on decision-making was significantly associated with both ANC4+ attendance and facility-based delivery, while health provider influence was only significantly related to giving birth in a facility. The important role of husbands in household decision-making in north-western Nigeria is well established (Oguntunde et al., Reference Oguntunde, Nyenwa, Yusuf, Dauda, Salihu and Sinai2019; Ntoimo et al., Reference Ntoimo, Okonofua, Aikpitanyi, Yaya, Johnson and Sombie2020) and this power dynamic is amplified by early marriage practices, polygyny and low female literacy and formal schooling (Wolf et al., Reference Wolf, Abubakar, Tsui and Williamson2008). Some research suggests that men in this area may consider pregnancy and childbirth a woman’s domain, and may not engage in decision-making, even if the wife is not empowered to make such decisions alone (Oguntunde et al., Reference Oguntunde, Nyenwa, Yusuf, Dauda, Salihu and Sinai2019). Nevertheless, shared health care decision-making and male engagement in pregnancy and childbirth decisions have been shown to improve pregnancy outcomes (Danforth et al., Reference Danforth, Kruk, Rockers, Mbaruku and Galea2009; Yargawa & Leonardi-Bee, Reference Yargawa and Leonardi-Bee2015). The current findings further underscore the important role of spousal support for uptake of maternal health services in this area. These results suggest that SBC programmes should place a high priority on male engagement in order to positively improve maternal health outcomes and must work within the context of gender and social norms that reduce women’s empowerment in health care decision-making more broadly. Finally, health worker support was also found to have a positive influence on women’s decision to give birth in a facility. Since providers are a conduit for positive health messaging through interpersonal communication with clients, encouraging providers to counsel women on the value of facility-based delivery during ANC visits may be an important channel for promoting behaviour change in the future. Such improvements in health care counselling must also be viewed in light of broader health system strengthening efforts that improve the availability and quality of maternal health care, which in turn improves community perceptions of, trust in and demand for these services.
The results presented in this paper should be viewed in light of some methodological limitations. First, associations found in cross-sectional studies do not imply causation, and importantly, there is potential for reverse causation such that performing a behaviour (e.g. giving birth in a facility) may create or reinforce an ideation (e.g. confidence in accessing a facility for delivery). Second, observational studies are prone to residual confounding from unmeasured variables, such as ideations that were not measured or facility-level variables that were not collected as part of this population-based survey. Third, self-reported attitudes may be affected by social desirability concerns or desires to please the interviewer, which could bias responses towards more agreeable ones. Respondents’ attitudes may also vary depending on the respondent’s disposition at the time of interview. Fourth, psychosocial metrics may not adequately capture the broadly defined ideational domain, which could lead to non-significant findings for an ideation despite its potential importance for pregnancy and childbirth decisions. Finally, the findings were derived from a community-based survey that aimed to gauge women’s perceptions and practices in relation to maternal health services in order to inform an SBC programme in the study wards. These findings do not provide evidence of health services quality, male perceptions or other broader cultural or societal contextual information, which also greatly influence service uptake.
Overall, the study results indicate that improving pregnancy and childbirth practices in north-western Nigeria will require SBC programmes to consider addressing a wide range of psychosocial factors, including raising knowledge and dispelling myths, building women’s confidence to access services, engaging spousal support in decision-making and improving perceived (and actual) maternal health services quality. These psychosocila factors are also heavily influenced by the broader socioeconomic, cultural and health system contexts of the north-west region. Such efforts must be complemented by broader health system strengthening efforts and other programmes that specifically address entrenched gender and social norms that reduce women’s participation in health care decision-making. Ideational metrics provide important insights for programmes that aim to change health behaviours, including pregnancy and childbirth, and should be explored for other health areas as well.
Acknowledgments
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Funding
The research was funded by the United States Agency for International Development (USAID) through the Breakthrough RESEARCH cooperative agreement AID-OAA-A-17-00018. The funders had no role in the study design, data collection and analysis, data interpretation, manuscript preparation or the decision to submit for publication.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
Ethical approval for this study was obtained from the National Health Research Ethics Committee in Nigeria [NHREC/01/01/2007-02/09/2019] and the Tulane University Institutional Review Board in Louisiana, USA [2019-1047]. Written informed consent to participate in the survey was obtained from all willing participants for the household and female questionnaires. Each participant signed or marked her thumbprint on the consent form to signify willingness to participate. All survey participants were married women and any respondent under 16 years was considered an emancipated minor not requiring parental consent.
Author Contributions
PLH and PCH designed and conceptualized the study. PLH and EWJ developed the study questionnaire, supervised fieldwork and data collection. EWJ, UA and PLH compiled, prepared and analysed data. EWJ, UA, DA, MO, SA-A, PCH and PLH contributed to interpretation of findings. EWJ wrote the first draft of the paper. EWJ, UA, DA, MO, SA-A, PCH and PLH reviewed, revised and contributed to writing the paper. All authors read and approved the final manuscript.








