Disasters have a significant impact on the affected communities’ well-being and mental health (MH) and may affect the utilization of health services. They cause injuries and loss of life, having a direct effect on MH conditions of people who experienced it. Reference Beaglehole, Mulder and Frampton1,Reference North, Ursano, Fullerton, Weisaeth and Raphael2 Furthermore, these events may also promote MH effects indirectly, through secondary stressors Reference Lock, Rubin and Murray3 such as the loss of social and familial bonds, loss of income, difficulties with compensations, loss of schooling and education, and through the preclusion of access to health and other essential services.
Even if the number of publications on the mental health consequences of disasters increased importantly in the last few decades, major challenges remain in this field of research. Reference North, Ursano, Fullerton, Weisaeth and Raphael2 First, since disastrous events are not reproducible and populations, health services, and the way they deal with such events differ a lot from region to region, Reference North4 it is hard to evaluate the external validity of the assumptions drawn from studies in this field of science. Second, disasters may prevent access to data, and data gathering tends to not be taken as a priority following disastrous events. Third, most of the research on the field were conducted in high-income countries, whereas the most affected populations tend to be in low- and middle-income countries. 5,Reference Rodriguez and Kohn6
On November 5, 2015, Fundão tailings dam suffered a failure in Mariana, Minas Gerais Region, southeastern Brazil. The event released 30 to 40 billion liters of sub-products of iron ore extraction, 7 the iron mud wave overcame another dam downstream and then flowed through the Gualaxo River and the Carmo River. It finally reached the Doce River and flowed to its mouth in the Atlantic Ocean, 663 km away from the original location of the accident, passing through 39 municipalities with riverside areas.
The drainage basin of Doce river covers an area of 84 000 km2 in 2 southeastern Brazilian states (86% in Minas Gerais and 14% in Espírito Santo), mostly within the Atlantic Forest biome. An important proportion of the region (59%) is used for pasture, and 27% is still covered by native vegetation, and the area was home to around 3.6 million inhabitants when the disaster struck. 8
The event caused the immediate death of 19 people and major destruction of natural resources, drastically changing landscapes and habitats of terrestrial and aquatic flora and fauna. Riparian, freshwater, and even marine environments were affected, impacting tourism, fishery, and water supply. 7,Reference Fernandes, Goulart and Ranieri9 Following the event, concerning levels of hazardous substances were found in the region’s freshwater sources, prompting the interruption of water supply in different municipalities with riverside areas. This interruption lasted for different periods and warranted different solutions for each municipality, ranging from the use of subterranean water sources to transport of water from elsewhere by trucks. Monitoring of the water quality from the end of 2016 until mid-2017 showed that mean turbidity, mean quantity of solids in suspension, and the concentration of iron and manganese in the water of Doce River Basin were still above legal limits in many monitoring stations, despite being lower than those recorded in the first year after the accident. 10
The long-term environmental impact of tailings dam failures has already been evidenced after the dam failure in Hajka, Hungary, in 2010. A study conducted 6 years after the failure of the dam used to contain byproducts of the aluminum manufacture found an increased salinity and increased concentration of trace elements in the soil. Reference Winkler, Bidló and Bolodár-Varga11 Another example of the environmental and socioeconomic impact of this type of event is the Los Frailles dam failure in Spain, in 1998, where €147 million was spent to mitigate environmental and agricultural damages. Reference Rico, Benito and Díez-Herrero12
The Brazilian public health system (Unified Health System—SUS) is universal and free of charge since the 1988 constitution defined health as a right of all citizens and duty of the state. The health service delivery is organized through integrated service networks arranged into health regions. Reference Paim, Travassos and Almeida13 The MH care network is composed of outpatient services which include municipal and regional psychosocial centers and inpatient psychiatric care services which may be present in general or psychiatric hospitals. The public health system in Brazil has been underfinanced from the beginning, a trend that tends to worsen with the financial crisis and the austerity measures implemented in 2016. Reference Castro, Massuda and Almeida14 Therefore, information on these services’ utilization during and following crisis is valuable, to help optimize the understanding of the health system and guiding an evidence-based allocation of limited resources.
In this study, we aim to assess the effects of water supply interruption following the Mariana dam failure on public mental health services (MHS) utilization. The importance of the water supply interruption following the disaster in Mariana is underlined by a report published by the government of Minas Gerais indicating that the impacts related to water were the most relevant environmental damages that followed the event, affecting agriculture, fishery, and other rural and urban economic activities. 15 Moreover, previous studies have identified water insecurity as a psychological stressor Reference Wutich and Ragsdale16 and linked it to an increase in the prevalence of specific MH conditions. Reference Aihara, Shrestha and Sharma17 We performed the study using secondary health data and defining MH utilization with 2 outcomes: the monthly rate of MH ambulatory care visits as primary outcome, and the monthly rate of MH hospital admissions (HA) as the secondary outcome.
Methods
We conducted an interrupted time-series analysis with control group, using monthly aggregated routine data from a federal public access database.
We considered the affected population (381 749 inhabitants) of the 9 municipalities of Minas Gerais that suffered interruption of water supply following the dam failure 8 : Belo Oriente, Periquito, Alpercata, Governador Valadares, Tumiritinga, Galiléia, Resplendor, Itueta, and Aimorés (Figure 1).
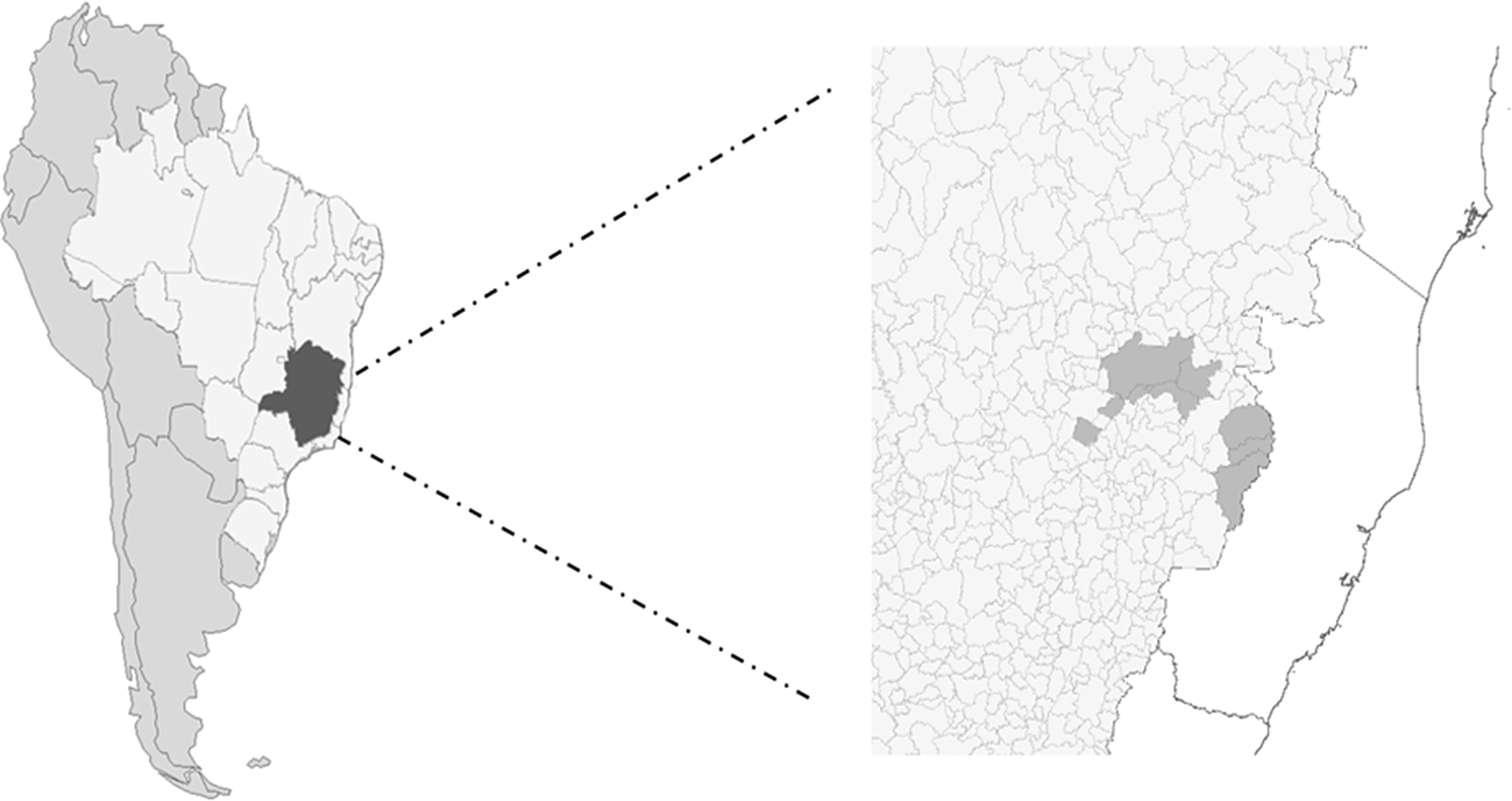
Figure 1. The right image shows a map of South America depicting Brazil in lighter gray and Minas Gerais state in darker, to the left a zoom-in showing the affected municipalities in darker gray.
We analyzed data only from municipalities in Minas Gerais, excluding 3 municipalities from Espírito Santo State (Baixo Guandu, Colatina, and Linhares) that also had interruption of water supply due to incompleteness and unreliability of data relative to these municipalities during the study period.
The comparison group (also referred to as unaffected in this paper) was the population living in the rest of the State of Minas Gerais (20 487 352 inhabitants).
To reduce potential bias due to displacement of subjects from affected areas following the disaster, we analyzed the visits and HA by municipality of residence instead of using the municipality where the visit or admission took place.
We imported data from Tabnet, 18 the Brazilian federal open access health information platform, which gives access to information from DATASUS (Informatic System of the Unified Health System—SUS). We extracted monthly aggregated routine data from January 2013 to October 2018 (34 months before and 36 months after the event), accessing the outpatient and inpatient services databases. Data were extracted for the whole state of Minas Gerais and for each of the 9 affected municipalities. Data on the ambulatory care and HA for the affected population and Minas Gerais state are provided as supplementary material.
Two investigators (MFDA and GECO) went separately through the whole list of procedures present on DATASUS and defined which were linked to mental health assistance, leading to a list with 65 MH procedures (see Supplementary material). Not all the selected procedures had entries in Minas Gerais during the study period.
For demographic information, we used open access information from IBGE’s (Brazilian Institute of Geography and Statistics) website. 19
The primary outcome of the study was the rate of mental health visits (MHV) and the secondary outcome was the rate of HA for mental health reasons. We present monthly aggregated data from both populations in the periods before and after the dam failure. Data are presented as means and standard deviation. We modeled the rates of MHV and hospitalizations using a negative binomial regression, allowing for possible overdispersion of data. The immediate effect of the disaster was modeled as a step function, using an indicator variable taking a value of 1 at the time of the event, whereas the gradual effects were investigated considering an interaction term between the dam failure and time. Reference Lopez Bernal, Cummins and Gasparrini20 As suggested in a previous publication, Reference Linden21 we first analyzed the affected and the unaffected groups separately (single-group analysis). Following that, we included the groups in the same model (multiple-group model) and evaluated whether the observed effects were different between the 2 groups. Since we used secondary data from a public open-access database with anonymized data, this study did not require an ethics committee approval.
We conducted the data analysis using Stata (Stata Statistical Software: Release 15; Stata Corp LLC, College Station, TX). Means were compared using an independent t-test and the ITS model used 2-sided tests and performed at the 5% level of statistical significance.
Results
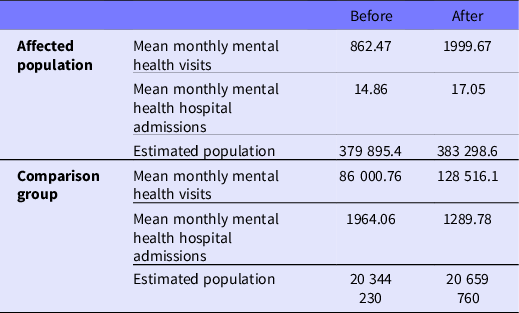
When comparing the whole analyzed period before the event with the period following the event, we evidenced an increase in the mean monthly MHV in the affected group from 862.47 to 1999.67, while in the comparison group it went from 86 000.76 to 128 516.1. When analyzing hospital admissions due to MH conditions, we observed an increase in the affected group from 14.86 to 17.05, whereas it decreased from 1964.06 to 1289.78 in the comparison group (Table 1).
Table 1. Descriptive statistics of the affected population and the comparison group
We observed a continuous discrete upward trend in the monthly rate of MHV overall throughout the study of the comparison group, with a neglectable change in level following the event. The affected population had a downward trend before the dam failure, which was followed by a significant positive change in level and a change in slope toward a growth on the rate of visits over time. The rate of MH visits was lower in the affected population when the event happened, and by the end of the series it tended to surpass the comparison group (Figure 2). In the regression model, we observed an 82% immediate increase in the rate of visits in the affected group (RR 1.82, 95% CI: 1.28 to 2.60), which was not evidenced in the unaffected population (RR 1.00, 95% CI: 0.93 to 1.07). When comparing the 2 groups, the increase in visits was 78% higher in the affected population than in the unaffected one (RR 1.78, 95% CI: 1.25 to 2.53). We also observed a 5% gradual increase (change in trend) in the monthly rate of visits in the affected group, whereas there was no change in slope in the unaffected group. The comparison between the 2 groups was statistically significant (P < 0.001) in this case as well (Table 2).
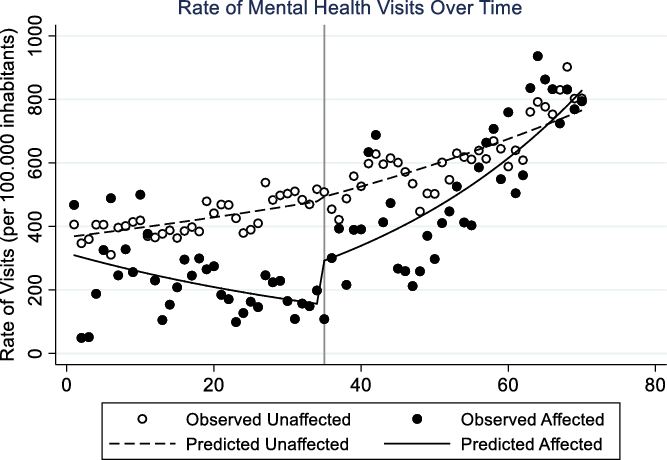
Figure 2. Rate of Mental Health Visits (per 100.000 inhabitants) over time in the affected and unaffected groups. The dots represent the observed data and the line the values predicted by the regression model. The black vertical line represents the time of the incident.
Table 2. Relative risk (RR) as predicted by the regression model showing immediate and gradual (monthly rate of change) effects of the Mariana dam failure on ambulatory mental health care visits and mental health hospital admissions in the affected and unaffected municipalities and the comparison between the 2 groups
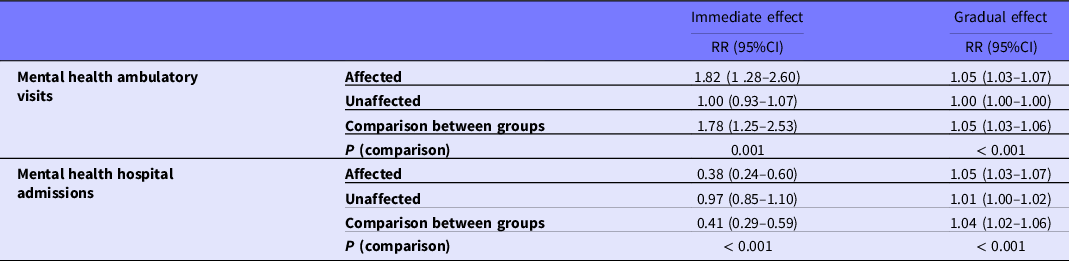
Regarding hospital admissions, our secondary outcome, observed was a 62% immediate decrease in the hospital visits due to mental health conditions in the affected group (RR: 0.38, 95% CI: 0.24 to 0.60), whereas there was no statistically significant change in the comparison group (RR: 0.97, 95% CI: 0.85 to 1.10) (this difference was statistically significant with a P < 0.001), whereas the monthly rate of change in hospital admissions was higher in the affected population (RR: 1.05, 95% CI: 1.03 to 1.07) than in the comparison group (RR: 1.01, 95% CI: 1.00 to 1.02), leading to a 4% higher increase in the affected population (RR: 1.04, 95% CI: 1.02 to 1.06) (Figure 3). The difference was statistically significant (P < 0.001) (see Table 2).
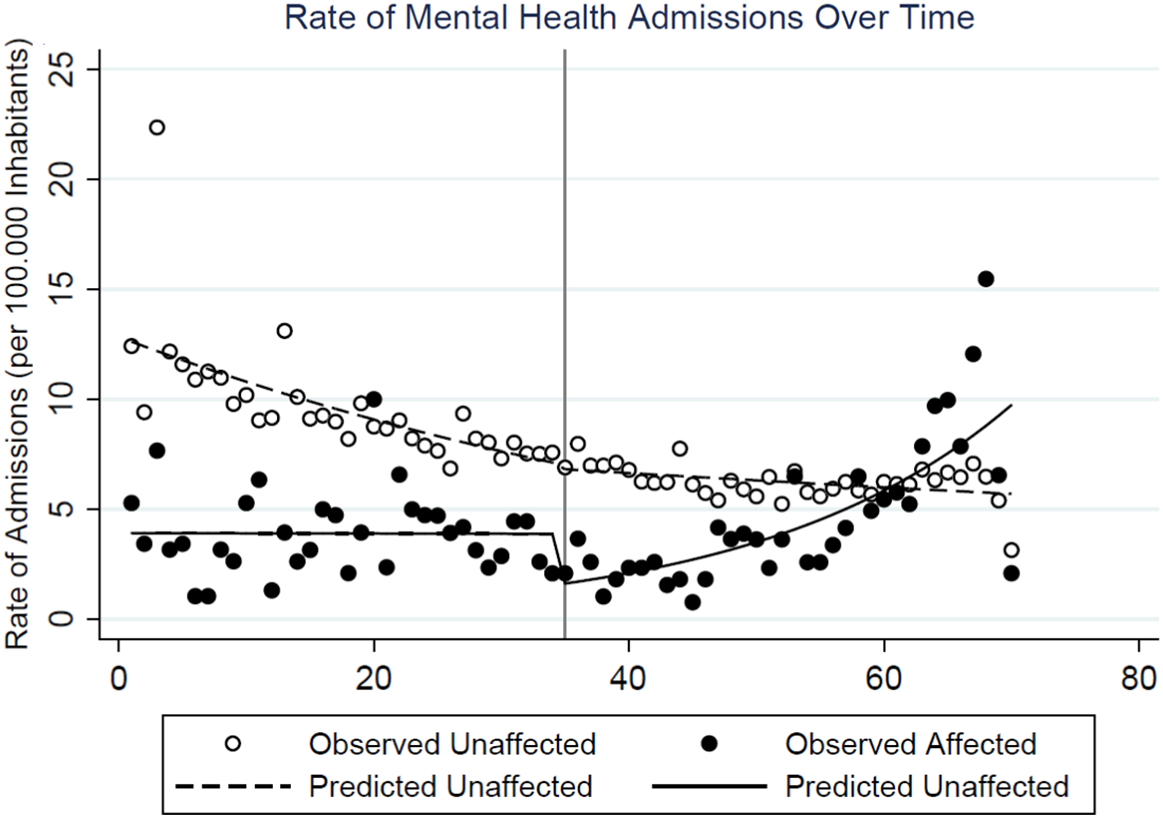
Figure 3. Rate of Mental Health Admissions (per 100.000 inhabitants) over time in the affected and unaffected groups. The dots represent the observed data and the line the values predicted by the regression model. The black vertical line represents the time of the incident.
Discussion
We identified a substantial increase in the rate of public MHV in the population of the municipalities that suffered water supply interruption after the Mariana dam failure, whereas no such an effect of MHV was observed in the comparison group. These results are in line with the findings of other studies. A study that evaluated MHS utilization before and after the landslides in Rio de Janeiro state mountainous region (Serrana Region) in 2011 Reference Dell’Aringa, Ranzani, Bierens and Murray22 reported an immediate increase in MHS utilization followed by a change of the underlying trend upward, and a study conducted after the 9/11 disaster Reference Boscarino, Adams and Figley23 suggests there was a long-term higher use of MHS following the event.
Our analysis of MH hospital admissions shows an important immediate decrease in the rate of MH admissions in the affected population. We hypothesize that this may be due to the acute allocation of hospital beds to other types of health emergencies following the event or difficulties in data registry in that period, whereas the positive trend in the monthly rate of MH admissions in the affected population following the event is probably due to the increase in the demand for MH services as seen in the ambulatory health data. Data on the comparison group show a steady decline in the rate of MH admissions. We believe this is probably linked to the Brazilian “anti-Asylum” movement and the “Psychiatric Reform,” which had its legal mark in 2001 with the approval of the 10.216 law, followed by a series of regulatory acts versing on the rights of MH patients and supporting less invasive and community-based ambulatory care. 24 The expansion of substitutive community-based services is illustrated by a report of the Ministry of Health showing that from 2002 to 2015 the number of community-based centers for psychosocial support (Centros de Atenção Psicossocial—CAPS) in Brazil increased from 424 to 2328, whereas the number of beds in psychiatric hospital decreased from 51.393 to 25.126. 25 This is the reason why we defined the changes in the rate of ambulatory care visits as our primary outcome.
Data from DATASUS 18 show that the affected region counted with 6 CAPS in the moment the disaster stroke and this number did not change until the end of the series. Even if the CAPS are not the only public health services where MH interventions take place, the increased number of MHV following the event may have led to an increased burden over these services if other strategies were not in place. To our knowledge, there are no publications discussing public mental health interventions focused on the studied population.
A survey performed 2 years after the Mariana dam failure (PRISMA) by authors from the Universidade Federal de Minas Gerais evidenced a high incidence of MH symptoms in the population of the districts of Mariana directly hit by the iron ore mud when the dam failed. They interviewed 271 victims (225 adults and 46 children), and their report shows that 28.9% of the studied population referred having diagnosis of depression, 32% of general anxiety disorder, 12% of posttraumatic stress disorder, and risk of suicide was identified in 16.4% of them. 26 Our study uses a broader population, aiming to address the potential impacts of secondary stressors—in our case, water supply interruption—which had their relevance highlighted in a recent publication that evidenced a threefold increase in depression symptoms in the United States following the emergence of the coronavirus disease (COVID-19) pandemic, pointing out that people who were more exposed to secondary stressors tended to report more severe depression symptoms. Reference Ettman, Abdalla and Cohen27
The Lancet Commission on Global Mental Health and Sustainable Development Reference Patel, Saxena and Lund28 suggested in 2018 that the global burden of diseases attributed to MH increased in the last years, especially in low- and middle-income countries. The Commission also mentioned that frequently the quality of MHS is lower than that of the services for other conditions and puts the reduction of the gap on the access to MHS as a priority. We hypothesized that disasters may increase this gap even more, worsening the burden on already insufficient services. This way, we believe that health services’ utilization studies may be a pragmatic way of evaluating a disaster’s consequence and analyzing the current health needs and gaps.
We defined the study affected population as the population of the municipalities that suffered water supply interruption as presented in the report from the Brazilian National Water Agency. 8 However, this does not mean that these municipalities were those only affected by the dam failure. Some of the municipalities that suffered the direct impact of the mud wave were not even included in the population we defined as affected; for this reason, our results should be regarded as conservative. Furthermore, the impact of the hereby studied event cannot be limited to the direct impact of the iron ore mud and the interruption of water supply. Many more secondary stressors played a part in the intricate chain of events that lead to the social and health impacts of the Mariana dam failure: The population directly affected by the event had difficulties with compensation Reference Fernandes, Goulart and Ranieri9 and in 2020, almost 5 years after the event, Brazilian prosecutors accused BHP and Vale S/A, the mining companies that hold Samarco (the joint venture that owned the Fundão Dam) of collusion to reduce the compensation for the victims. 29,30 In April 2021 the company filed for bankruptcy protection, which may make it even more difficult for the victims to receive compensation. 31 There are also reports of social conflict in the directly affected communities due to the search for compensation by some victims and the fear of not keeping their jobs if they fought for compensation for others. 26 A vast area of the states of Minas Gerais and Espírito Santo suffered major economic impact in tourism, agriculture, and fishing, and there was an important impact in the way of life and on the means of subsistence of indigenous populations and traditional communities. Reference Fernandes, Goulart and Ranieri9
Dam failures leading to loss of life have been reported for centuries. A report by the English Environmental Agency depicts such events in British soil from as far back as the 17th century. It also presents some important global events from the second half of the 20th century to 2009 leading to more than 6000 deaths in 14 different countries, including Brazil. 32 It is also important to highlight the relevance of the disaster risk and the social and environmental impacts related to mining in Brazil. The country holds 769 mining dams and the Fundão dam was one of the ones considered at low risk. In 2019, another disaster linked to tailing dams happened in Minas Gerais. The Córrego do Feijão dam, which was also considered low risk and belonged to Vale S/A, failed in Brumadinho killing more than 250 people and affecting more than 1 million. Reference Freitas, Barcellos and Asmus33,Reference Silva Rotta, Alcântara and Park34
Even though previous evidence 26 suggests that there was an important increase in the incidence of MH conditions in the population directly affected by the dam failure and the same has been observed after other disastrous events, such as a large MH survey conducted in England that reported an increase in common mental disorders and suicidal thoughts and attempts in the population who had their house damaged by the English floods from December 2013 to March 2014, Reference Graham, White, Cotton and McManus35 our study was not designed to access changes in incidence or severity of mental health disorders in the population. In this study, we aim to evaluate how the Mariana dam failure has influenced the utilization of public MHS in a pragmatic way, hoping to present information that can be useful for practitioners and managers of health services. Andersen’s Behavioral Model of Health Services utilization groups the factors that influence health services utilization in enabling, predisposing, and needs. Reference Kim and Lee36 Future studies focusing on the change in the MH disorders, social characteristics of the affected communities and their social support network, and more detailed and qualitative attributes of the local health services would help develop a more comprehensible view of the hereby presented phenomenon and further address the attributes of Andersen’s Behavioral Model.
Our study underlines the importance of routine health data to assess the effects of disastrous events, regarding health services’ utilization. While the use of this data trough is a robust methodology like the interrupted times series analysis is nowadays firmly established in some fields (eg, evaluation of public health interventions), its use in disaster medicine is still relatively new. At this extent, the role of open-access data on the development of evidence-based policies, a point stressed by the United Nation’s Office for Disaster Risk Reduction (UNDRR) in the Global Assessment of Risk 2019 (GAR2019), 5 cannot be overemphasized.
Limitations
One limitation of this study relies on the fact that we focused on public MHS not analyzing data on private services. However, data from the National Agency of Additional Health (Agencia Nacional de Saude Suplementar—ANS) indicates that just around 23.54% of the population of Minas Gerais has some sort of private health insurance and this proportion falls to around 22.30% when analyzing the whole country. 19,37 Moreover, the population on the lower socioeconomic quintile tends to rely exclusively on public health services. Reference Castro, Massuda and Almeida14 A second limitation of this study relies on the use of retrospective data, which may be also influenced by changes in the quality of acquisition following a disaster.
Conclusions
The municipalities that experienced water supply interruption following the Mariana dam failure had an increase in the utilization of public MHS when compared to the other municipalities of the state. Our findings draw attention to the effects disasters may have on the utilization on MHS, emphasizing the role of secondary stressors such as the preclusion of access to basic services.
Data availability statement
The list of the selected mental health procedures and the data used for this study are available as supplementary material at https://doi.org/10.6084/m9.figshare.16435248.
Funding statement
This manuscript is part of the joint PhD program in Global Health, Humanitarian Aid and Disaster Medicine of the University of Eastern Piedmont and The Free University of Brussels pursued by MFD with a scholarship.
Conflict(s) of interest
MFD is an associate editor of this journal but did not participate of the peer review process.







